Abstract
Background
Previous meta‐analyses on meat intake and risk of stroke did not report the effect of white meat (poultry meat, excluding fish) and did not examine stroke incidence and mortality separately. We aimed to investigate the relationship of total (red and processed meat), red (unprocessed or fresh red meat), and processed (processed red meat) consumption along with white meat on risk of stroke incidence and mortality.
Methods and Results
Articles were identified from databases and reference lists of relevant studies up to October 28, 2016. We selected prospective cohort studies on meat consumption specified by types of meat and stroke incidence and mortality reporting relative risks and 95% confidence intervals. The pooled relative risk was estimated using the random‐effects model. Based on the inclusion criteria, 10 articles containing 15 studies (5 articles with 7 studies including 9522 cases of stroke incidence and 254 742 participants and 5 articles with 8 studies containing 12 999 cases of stroke mortality and 487 150 participants) were selected for quantitative synthesis. The pooled relative risks (95% confidence intervals) for total, red, processed and white meat consumption and total stroke incidence were 1.18 (1.09–1.28), 1.11 (1.03–1.20), 1.17 (1.08–1.25), and 0.87 (0.78–0.97), respectively. Total meat consumption (0.97 [0.85–1.11]) and red meat consumption 0.87 (0.64–1.18) were not significantly associated with stroke‐related death.
Conclusions
The relationship between meat intake and risk of stroke may differ by type of meat. Recommendations for replacing proportions of red and processed meats to white meat for the prevention of stroke may be considered in clinical practice.
Keywords: cerebrovascular accident, cerebrovascular infarction, cerebrovascular ischemia, meat consumption
Subject Categories: Diet and Nutrition, Epidemiology, Cardiovascular Disease, Lifestyle
Clinical Perspective
What Is New?
The association of meat consumption with risk of stroke varies by types of meat.
What Are the Clinical Implications?
Replacement of red and processed meats to white meat may be considered among patients at high risk for stroke, among the other lifestyle interventions.
Introduction
Cerebrovascular accidents are a serious health condition that causes disability and death among adults, with high disease burden in the world.1, 2 Although variation in stroke incidence and burden may exist between high‐ and low‐income countries, the prevalence of stroke (proportion of the population with history of stroke) and burden (disability‐adjusted life‐years lost) are increasing worldwide.3 Controlling for risk factors is needed to halt the increasing rates of stroke prevalence globally.4
Among the risk factors for stroke, dietary habit is one of the modifiable and self‐manageable factors that should be a focus of public health intervention. Previous meta‐analyses show that increased fruit and vegetable consumption is associated with a decreased risk of stroke,5, 6, 7 whereas high intake of red and processed meats is related to an increase in total stroke and ischemic stroke cases.8, 9, 10, 11 Despite a recent transition to a higher proportion of white meat (poultry) intake, consumption of red and processed meats still constitutes the largest proportion of overall meat consumption and has been increasing in the United States and other developed countries.12 One of the major problems currently with the recommendations for dietary protein in North America is that there is no clear distinction of fat content between red meat and white meat and fish.13 At present, evidence on the effects of meat consumption on risk of stroke accounting for nutritional properties of different types of meat is not entirely clear. Therefore, it is necessary to examine the association of consumption of different kinds of meat with incident stroke and stroke‐related death before establishing nutrition intervention strategies.
Some methodological inconsistencies and issues limit previous meta‐analyses of red meat and processed meat consumption that have reported a positive association with risk of stroke. Existing meta‐analyses considered stroke mortality as fatal stroke incidence and combined the results,8, 10, 11 synthesized both out‐of‐date14 and most recent15 results from the same cohort (ie, Health Professionals Follow‐Up Study) for analysis,11 and performed subgroup analysis only by stroke subtypes.8, 10 In addition, none of the previous meta‐analyses addressed the relationship between white meat intake and risk of stroke. This meta‐analysis aimed to update evidence on the association between total, red, and processed meat consumption, and white meat consumption on the risk of stroke and stroke‐related death.
Methods
Study Strategy and Literature Search
We followed the MOOSE (Meta‐Analysis of Observational Studies in Epidemiology) guideline for reporting the relevant items in this study.16, 17 We conducted a literature search of PubMed, Embase, and Cochrane Library databases to identify relevant articles published through October 2016. In accordance with one review,18 we used a broad search term for “total, red, processed and white meat” (meats, meat product, meat products, red meat, red meats, beef, veal, goat, lamb, pork, mutton, sausage, sausages, ham, hams, pastrami, bacon, bacons, salami, salamis, hot dog, hot dogs, animal food, animal foods, animal protein, animal proteins, diet, diets, dietary, white meat, poultry, chicken, duck, turkey, rabbit) in combination with “stroke” (stroke, ischemic stroke, hemorrhagic stroke, cerebrovascular disease, cerebrovascular attack, cerebral infarct, intracranial hemorrhage) to identify articles on total, processed, red and white meat consumption, and risk of stroke incidence and mortality. The full search strategy is shown in Table S1.
Two authors (K.K. and J.H.) independently conducted the selection procedure from the initial screening to select the articles included for this meta‐analysis. The two authors (K.K. and J.H.) reviewed articles eligible for a full‐text review and additional records were identified through the reference lists of relevant publications. Each article was evaluated based on the inclusion criteria. We conducted study selection procedures without any language restrictions. Any cases of disagreement between the 2 authors were resolved by consulting with the corresponding author (S.M.P.).
Study Selection
We selected prospective cohort studies with an assessment of meat intake and stroke incidence along with mortality comparing the highest versus the lowest categories. The following inclusion criteria were adopted for the final selection of studies used for this meta‐analysis: (1) prospective cohort design (2) assessment of total, red, processed, and white meat consumption (3) outcome of the study of stroke and its subtypes or stroke‐related death; and (4) reporting the outcome as relative risks (RRs) with 95% confidence intervals (CIs) in publication. In addition, we considered only the most recent publication eligible for inclusion if the studies were based on the same cohort.
Definition of the Types of Meat
The types of meat were assessed and classified by the following definition: (1) total meat: red meat and processed meat; (2) red meat: unprocessed or fresh red meat; (3) processed meat: processed meat or processed red meat; and (4) white meat: poultry meat only (fish excluded).
Definition of Stroke Incidence and Mortality
We defined stroke incidence as the first occurrence of stroke and stroke mortality as death caused by stroke.
Data Extraction and Quality Assessment
Two authors (K.K. and J.H.) independently reviewed selected articles and extracted the following information: last name of the author; study year; country; population size; follow‐up duration; amount of highest and lowest intake; type of meat consumption; number of stroke (and stroke subtypes) incidence and mortality; adjustment variables; and RRs and corresponding 95% CIs. The quality assessment of each study was performed using the Newcastle‐Ottawa Scale for cohort studies.19 Scores ranged from 0 to 9 based on the 8‐item instrument containing subject selection, comparability of subjects, and assessment of outcome/exposure. The quality assessment based on Newcastle‐Ottawa Scale for cohort studies is presented in Table S2.
Statistical Analysis
We transformed hazard ratios, RRs, and standard errors (calculated from corresponding 95% CIs) by taking their natural logarithms.20 The pooled RRs and 95% CIs were calculated from a random‐effects model based on the Der Simonian and Laird method21 to account for variation and statistical heterogeneity between the studies. Assessment of heterogeneity between the studies was based on Cochran Q test and Higgin I 2 statistic.22 Egger test was performed to check for a publication bias.23 P<0.1 from Q test and I 2 value >50% were determined as substantial heterogeneity. The significance cutoff P value for the Egger test was set to 0.1. We conducted subgroup analyses to assess the associations between types of meat consumption and stroke incidence and mortality by various characteristics of the studies (number of cases, follow‐up duration, sex, stroke subtypes, and adjustment variables ranging from sociodemographic status to health behavior and health status) to account for heterogeneity among the studies. All statistical analyses were conducted with Stata version 14.0 (StataCorp). Unless otherwise specified, P values were 2‐sided. P<0.05 was considered statistically significant.
Results
Study Selection and Characteristics of the Studies
An initial search identified a total of 2074 articles. In addition, we included 13 articles from the reference lists of relevant studies. After removing duplicates, a total of 1681 articles were remaining and 25 articles were eligible for a full‐text review after excluding articles with irrelevant titles and abstracts. After the full‐text review, we excluded 15 articles: 5 articles because they assessed overall dietary pattern instead of meat, 5 articles because they focused on the Mediterranean diet, 1 article because full text was not available, 2 articles because of a duplicate cohort, and 2 articles because of a case‐control design. Finally, a total of 10 articles containing 15 cohort studies published until October 2016 were included in this meta‐analysis. Five articles included 7 studies on total (6 comparisons), red (8 comparisons), processed (8 comparisons), and white meat (4 comparisons) consumption and stroke incidence and the other 5 articles contained 8 studies on total (5 comparisons) and red (4 comparisons) meat intake and stroke mortality. Data on 254 742 participants with 9522 stroke incidents and 487 150 participants with 12 999 cases of stroke mortality were quantitatively synthesized. A PRISMA16, 17 flow chart for the study selection is presented in Figure 1. Characteristics of the selected studies for this meta‐analysis are summarized in Table 1.15, 24, 25, 26, 27, 28, 29, 30, 31, 32
Figure 1.
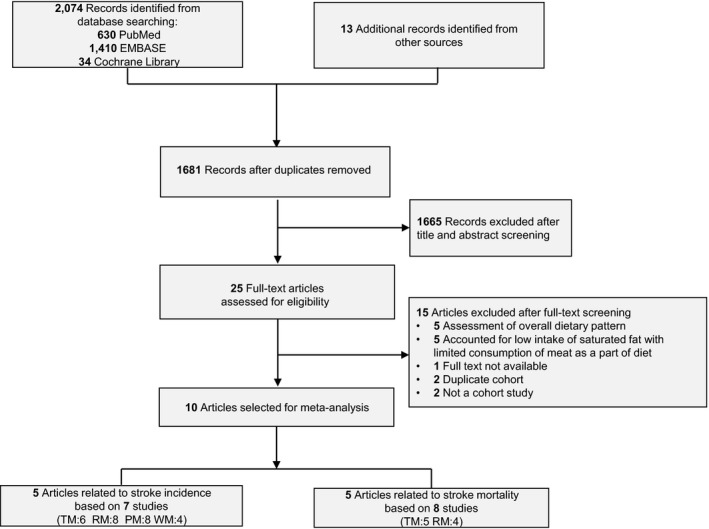
Flow diagram for identification and study selection. PM indicates processed meat; RM, red meat; TM, total meat; WM, white meat. The numbers in parentheses refer to the number of comparisons within the studies according to types of meat.
Table 1.
Characteristics of the Cohort Studies Included in the Quantitative Analysis of Total, Red, Processed, and White Meat Consumption and Risk of Stroke Incidence and Mortality
| Study | Country | Study Name | Follow‐Up Duration, y | Study Population (Baseline Age) | Type of Stroke and No. of Cases | Range of Meat Intake: Highest vs Lowest | Adjusted RR (95% CI) for Strokes | Adjustment | |
|---|---|---|---|---|---|---|---|---|---|
| Stroke incidence | |||||||||
| 1. | Larsson 201125 | Sweden | Swedish Mammography Cohort | 10.4 | 34 670 Women (49–83 y) | 1680 Total strokes, 1310 CIs, 154 ICHs, 79 SAHs 137 nonspecific |
Total red meat: ≥86.0 g/d vs <36.5 g/d Fresh red meat: ≥48.8 g/d vs <16.5 g/d Processed meat: ≥41.3 g/d vs 12.1 g/d |
TS: 1.12 (0.95–1.31) IS: 0.74 (0.45–1.12) TS: 1.07 (0.91–1.23) HS: 0.85 (0.54–1.34) TS: 1.18 (1.00–1.38) HS: 0.91 (0.60–1.39) |
Age, smoking, education, BMI, total physical activity, history of diabetes mellitus or hypertension, aspirin use, family history of MI, and intake of total energy, alcohol, coffee, fish, fruits, and vegetables |
| 2. | Larsson 201124 | Sweden | The Cohort of Swedish Men | 10.1 | 40 291 Men (45–79 y) | 2409 Total strokes, 1849 ISs, 350 HSs |
Total red meat: ≥136.2 g/d vs <62.5 g/d Fresh red meat: ≥83.1 g/d vs <33.5 g/d Processed meat: ≥57.1 g/d vs 20.1 g/d |
TS: 1.15 (1.00–1.33) HS: 1.57 (1.09–2.25) TS: 1.07 (0.93–1.24) HS: 1.27 (0.90–1.80) TS: 1.23 (1.07–1.40) HS: 1.39 (0.97–1.99) |
Age, smoking, education, BMI, total physical activity, history of diabetes mellitus or hypertension, aspirin use, family history of MI, and intake of total energy, alcohol, coffee, fish, fruits, and vegetables |
| 3. | Bernstein 201215 | United States | HFPS (Health Professionals Follow‐Up Study) | 22 | 43 150 Men (40–75 Years) | 1397 Total strokes, 829 ISs, 165 ICHs, 53 SAHs |
Total red meat: 2.29 servings/d vs 0.30 servings/d Fresh red meat: 1.11 servings/d vs 0.14 servings/d Processed red meat: 0.71 servings/d vs 0.03 servings/d White meat: 0.72 g/d vs 0.14 g/d |
TS: 1.28 (1.02–1.61) HS: 1.07 (0.55–2.08) IS: 1.31 (0.97–1.77) TS: 1.11 (0.88–1.39) HS: 0.70 (0.36–1.37) IS: 1.23 (0.91–1.67) TS: 1.27 (1.03–1.55) HS: 1.47 (0.80–2.72) IS: 1.31 (1.00–1.71) TS: 0.97 (0.81–1.17) HS: 0.66 (0.37–1.18) IS: 1.07 (0.84–1.37) |
Age, time period, BMI, smoking, physical exercise, parental history of early MI, menopausal status (including hormone replacement), multivitamin use, vitamin E supplement use, aspirin use, total energy, cereal fiber, alcohol, trans‐fat, fruit and vegetables, other protein sources, and history of MI, coronary artery bypass surgery, or percutaneous coronary intervention, angina, diabetes mellitus, hypertension, and hypercholesterolemia |
| 4. | Bernstein 201215 | United States | NHS (Nurses' Health Study) | 26 | 84 010 Women (30–55 y) | 2663 Total strokes, 1383 ISs, 235 ICHs, 240 SAHs |
Total red meat: 1.92 servings/d vs 0.44 servings/d Fresh red meat: 1.08 servings/d vs 0.28 servings/d Processed red meat: 0.64 servings/d vs 0.05 servings/d White meat: 0.54 g/d vs 0.14 g/d |
TS: 1.19 (1.00–1.41) HS: 1.30 (0.72–2.34) IS: 1.16 (0.92–1.48) TS: 1.19 (1.02–1.40) HS: 0.93 (0.54–1.60) IS: 1.30 (1.03–1.63) TS: 1.10 (0.95–1.27) HS: 0.94 (0.56–1.57) IS: 1.07 (0.87–1.31) TS: 0.82 (0.71–0.94) HS: 0.79 (0.51–1.24) IS: 0.78 (0.64–0.95) |
Age, time period, BMI, smoking, physical exercise, parental history of early MI, menopausal status (including hormone replacement), multivitamin use, vitamin E supplement use, aspirin use, total energy, cereal fiber, alcohol, trans‐fat, fruit and vegetables, other protein sources, and history of MI, coronary artery bypass surgery or percutaneous coronary intervention, angina, diabetes mellitus, hypertension, and hypercholesterolemia |
| 5. | Haring 201526 | United States | ARIC (Atherosclerosis Risk in Communities Study) | 22.7 | 11 601 Men and women (45–64 y) | 699 Total stroke |
Red and processed meats: 0.25 servings/d vs 1.90 servings/d Red meat: 0.14 servings/d vs 1.08 servings/d Processed meat: 0 servings/d vs 1.07 servings/d White meat 0.8 servings/d vs 0.07 servings/d |
Men TS: 1.62 (1.03–2.57) Women TS: 1.1 (0.75–1.89) Men and women: HS: 1.45 (0.66–3.17) IS: 1.35 (0.95–1.93) Men TS: 1.65 (1.06–2.56) Women TS: 1.22 (0.80–1.87) Men and women HS: 1.13 (.53–2.45) IS: 1.47 (1.06–2.05) Men TS: 1.20 (0.83–1.72) Women TS: 1.29 (0.85–1.97) Men and women HS 1.67 (0.80–3.51): IS: 1.20 (0.90–1.61) Men TS: 0.91 (0.61–1.36) Women TS: 0.79 (0.53–1.17) Men and women HS: 0.56 (0.26–1.20) IS: 0.94 (0.70–1.27) |
Age, sex, race, study center, total energy intake, smoking, cigarette years, education, systolic blood pressure, use of antihypertensive medication, high‐density lipoprotein cholesterol, total cholesterol, use of lipid‐lowering medication, BMI, waist to hip ratio, alcohol intake, sports‐related physical activity, leisure‐related physical activity, carbohydrate intake, fiber intake, fat intake, and magnesium intake |
| 6. | Amiano 201630 | Spain | EPIC (the Spanish cohort of the European Prospective Investigation into Cancer and Nutrition) | 12 | 15 490 Men (29–69 y) | 373 Stroke, 302 ISs, 42 HS, 17 SAHs, 12 mixed or unspecified |
Unprocessed red meat: <24.3 g/d vs ≥86 g/d Processed meat: <21.5 g/d vs 72.6 g/d |
TS: 0.81 (0.54–1.21) IS: 0.80 (0.51–1.25) TS: 0.92 (0.64–1.32) IS: 0.86 (0.57–1.29) |
Age, center, total energy, BMI, waist circumference, smoking status, smoking before age 20, recreational physical activity, educational level, alcohol consumption, use of vitamin supplements (ATC code A11), use of antithrombotic or antihemorrhagic agents (ATC code B01/B02), use of cardiovascular drugs (ATC code C01–C10), use of salicylic acid or derivatives (ATC code N02BA), incident acute myocardial infarction cases, diabetes mellitus, self‐reported diseases (hypertension, hyperlidemia), percentage of energy from carbohydrates, protein and fats, and intake of vegetables, fruit, dairy products, and fish |
| 7. | Amiano 201630 | Spain | EPIC (the Spanish cohort of the European Prospective Investigation into Cancer and Nutrition) | 12 | 25 530 Women (29–69 y) | 301 Stroke, 229 ISs, 37 HS, 25 SAHs, 10 mixed or unspecified |
Unprocessed red meat: 11.1 g/d vs ≥52.4 g/d Processed red meat: <12 g/d vs ≥46 g/d |
TS: 1.21 (0.79–1.85) IS: 1.24 (0.74–2.05) TS: 0.81 (0.51–1.27) IS: 0.82 (0.47–1.42) |
Age, center, total energy, BMI, waist circumference, smoking status, smoking before age 20, recreational physical activity, educational level, alcohol consumption, use of vitamin supplements (ATC code A11), use of antithrombotic or antihemorrhagic agents (ATC code B01/B02), use of cardiovascular drugs (ATC code C01–C10), use of salicylic acid or derivatives (ATC code N02BA), incident acute MI cases, diabetes mellitus, self‐reported diseases (hypertension, hyperlipidemia), menopausal status, hormone replacement therapy and oral contraceptives, percentage of energy from carbohydrates, protein, and fats, and intake of vegetables, fruit, dairy products, and fish |
| Stroke mortality | |||||||||
| 1. | Sauvaget 200331 | Japan | Life Spain Study | 16 | 37 130 Men and women (34–103 y) | 1462 Total stroke‐related deaths |
Red meat: never vs almost daily Processed meat: never vs almost daily |
TS: 1.01 (0.73–1.38) TS: 0.90 (0.61–1.33) |
Age, sex, city, radiation dose, BMI, smoking, alcohol, education, and history of diabetes mellitus or hypertension |
| 2. | Yaemsiri 201227 | United States | WHIO (Women's Health Initiative Observational Study) | 8 | 87 025 Women (50–79 y) | 1049 IS‐related deaths |
Total red meat: per 1 serving/d Red meat: per 1 serving/d |
IS: 0.94 (0.75–1.23) IS: 1.13 (0.95–1.34) |
Age, race, education, family income, years as a regular smoker, hormone replacement therapy use, total metabolic equivalent task h/wk, alcohol intake, history of coronary heart disease, history of atrial fibrillation, history of diabetes mellitus, aspirin use, use of antihypertensive medication, use of cholesterol‐lowering medication, BMI, systolic blood pressure, total energy intake, dietary vitamin E, fruits and vegetable intake, fiber intake |
| 3. | Nagano 201228 | Japan | JACC (the Japan Collaborative Cohort Study for Evaluation of Cancer Risk) | 18 | 20 466 men (40–79 y) | 1317 total stroke‐related death |
Total meat 77.6 g/d vs 10.4 g/d |
TS: 1.10 (0.84–1.43) | Age, BMI, ethanol intake, perceived mental stress, walking time, sports participation time, year of education, history of hypertension and diabetes mellitus, total energy, and energy‐adjusted food (rice, fish, soy, vegetables, and fruits) intakes |
| 4. | Nagano 201228 | Japan | JACC (the Japan Collaborative Cohort Study for Evaluation of Cancer Risk) | 18 | 31 217 Women (40–79 y) | 1368 Total stroke‐related death |
Total meat 59.9 g/d vs 7.5 g/d |
TS: 0.91 (0.70–1.19) | Age, BMI, ethanol intake, perceived mental stress, walking time, sports participation time, y of education, history of hypertension and diabetes mellitus, total energy and energy‐adjusted food (rice, fish, soy, vegetables, and fruits) intakes |
| 5. | Sharma 201329 | United States | The Multiethnic Cohort | 7.5 to | 78 844 Men (45–75 y) | 434 Total stroke‐related death | Total meat >7.3 servings/d vs 0 to 2.5 servings/d | TS: 0.87 (0.57–1.34) | Ethnicity, time in study, y of education, energy intake, smoking, BMI, physical activity, history of diabetes mellitus, and alcohol intake |
| 6. | Sharma 201329 | United States | The Multiethnic Cohort | 7.5 | 96 044 Women (45–75 y) | 426 total stroke‐related death | Total meat >7.3 servings/d vs 0 to 2.5 servings/d | TS: 1.06 (0.69–1.65) | Ethnicity, time on study, y of education, energy intake, smoking, BMI, physical activity, history of diabetes mellitus, and alcohol intake |
| 7. | Takata 201332 | China | SMHS (Shanghai Men's Health Study) | 5.5 | 61 483 Men (40–74 y) | 2733 Total stroke‐related deaths |
Red meat 126 g/d vs 21.4 g/d White meat 22.3 g/d vs 11.9 g/d |
HS: 0.71 (0.43–1.20) IS: 1.22 (0.69–2.15) HS: 0.89 (0.56–1.40) IS: 0.92 (0.54–1.57) |
Age, total caloric intake, income, occupation, education, comorbidity index, physical activity level, total vegetable intake, total fruit intake, fish intake, red meat or poultry intake where appropriate, smoking history, consumption of alcohol |
| 8. | Takata 201332 | China | SWHS (Shanghai Women's Health Study) | 11.2 | 74 941 Women (40–70 y) | 4210 Total stroke‐related deaths |
Red meat 103.4 g/d vs 16.5 g/d White meat: 19.9 g/d vs 11.9 g/d |
HS: 0.57 (0.37–0.87) IS: 0.84 (0.55–1.28) HS: 1.20 (0.79–1.80) IS: 1.04 (0.69–1.56) |
Age, total caloric intake, income, occupation, education, comorbidity index, physical activity level, total vegetable intake, total fruit intake, fish intake, red meat or poultry intake where appropriate, smoking history, consumption of alcohol |
ATC indicates anatomic therapeutic chemical; BMI, body mass index; CI, confidence intervals; HS, hemorrhagic stroke; ICH, intracerebral hemorrhage; IS, ischemic stroke; MI, myocardial infarction; RR, relative risk; SAH, subarachnoid hemorrhage; TS, total stroke.
Pooled Analysis and Heterogeneity
Figure 2, 15, 24, 25, 26, 30 demonstrates the adjusted RRs (95% CIs) for each study and the pooled RRs (95% CIs) comparing the highest versus the lowest category of each type of meat consumption. Cochran I 2 values are presented along with heterogeneity P value for the pooled analysis for each type of meat. Overall, the results of pooled analyses indicate that total (RR, 1.18; 95% CI, 1.09–1.28 [I 2=0.00]), red (RR, 1.11; 95% CI, 1.03–1.20 [I 2=0.00]), and processed (RR, 1.17, 95% CI, 1.08–1.25 [I 2=0.00]) meat intake is associated with an increase of stroke incidence, whereas white meat (RR, 0.87; 95% CI, 0.78–0.96 [I 2=0.00]) consumption is related to a reduction of stroke incidence. However, consumption of total (RR, 0.97; 95% CI, 0.85–1.11 [I 2=0.00]) and red meat (RR, 0.87; 95% CI, 0.64–1.18 [I 2=70.9]) were not significantly associated with stroke mortality. The association between total and red meat consumption and stroke mortality is shown in Figure 3.27, 28, 29, 31, 32
Figure 2.
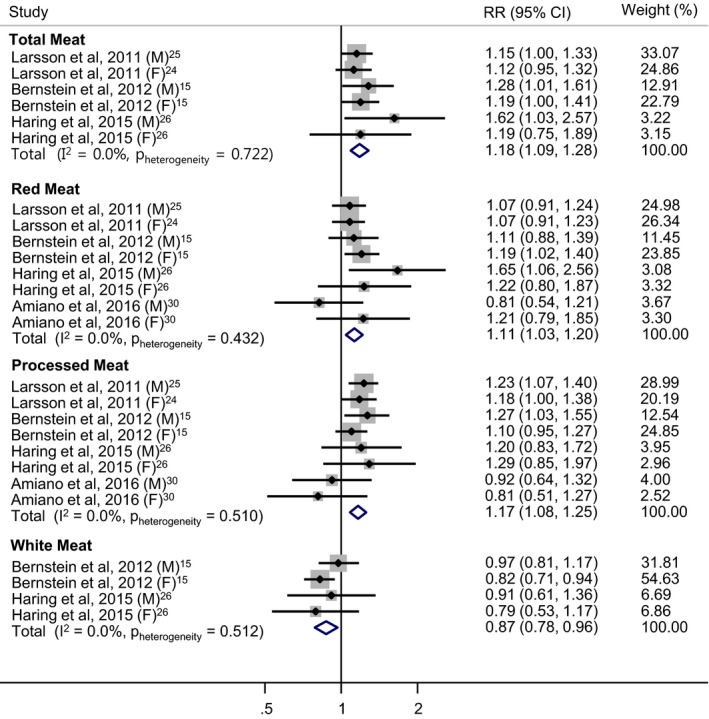
Relative risk (RR) ratios of total, red, processed, and white meat consumption and total incidence in stroke (highest vs lowest category). Weights are assigned from random‐effects model. CI indicates confidence interval; F, female; M, male.
Figure 3.
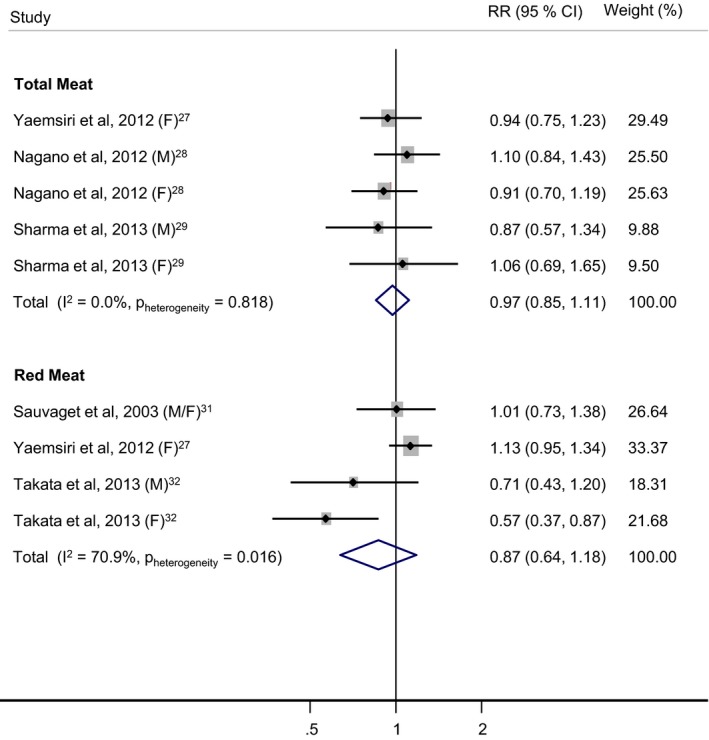
Total and red meat consumption and relative risk (RR) of stroke mortality (highest vs lowest category). Weights are assigned from random‐effects model. CI indicates confidence interval; F, female; M, male.
Total meat consumption and stroke incidence and mortality
Four articles containing 6 comparisons with reporting data on a total of 213 722 participants were included in the meta‐analysis of total meat consumption and stroke incidence.15, 24, 25, 26 The estimated RRs and 95% CIs of total meat intake and stroke incidence comparing the highest versus the lowest category is shown in Figure 2. The results suggest that consumption of total meat is significantly associated with a 9% to 28% increased risk of stroke. No heterogeneity was found among the 6 comparisons (I 2=0.00). The meta‐analysis of total meat consumption and mortality from stroke were based on 3 articles with 5 comparisons and a total of 313 596 participants.27, 28, 29 No evidence of an association between total meat intake and stroke morality was found (RR,0.97; 95% CI, 0.85–1.11 [I 2=0.00]).
Red meat consumption and stroke incidence and mortality
The combined results from 5 articles15, 24, 25, 26, 30 with 8 comparisons (254 742 participants) on red meat intake and stroke incidence comparing the highest versus the lowest category show that red meat consumption is linked to an increase of 3% to 20% stroke incidence. Among these 8 comparisons, we did not detect any heterogeneity (I 2=0.00). The association between red meat consumption and stroke‐related death was assessed based on 3 articles27, 31, 32 containing 4 comparisons (260 579 participants) comparing the highest versus the lowest categories. Although we found no association between red meat consumption and stroke mortality (RR, 0.87; 95% CI, 0.64–1.18 [I 2=70.9]), heterogeneity reached statistical significance.
Processed meat consumption and stroke incidence
The relationship between processed meat consumption and risk of stroke was investigated, with 5 articles consisting of 8 comparisons and a total of 254 742 participants.15, 24, 25, 26, 30 The meta‐analysis for processed meat intake and stroke incidence comparing the highest versus the lowest category showed that processed meat consumption is related to an 8% to 25% elevated stroke risk. There was no heterogeneity among the 8 studies (I 2=0.00).
White meat consumption and stroke incidence
For white meat, the pooled results from 2 articles15, 26 consisted of 4 comparisons (138 761 participants) comparing the highest versus the lowest categories and indicated that consumption of white meat is associated with a 4% to 22% decrease in stroke risk without any heterogeneity among studies (I 2=0.00).
Subgroup Analysis
The results from subgroup analyses for the studies on stroke incidence and mortality from stroke for each type of meat are presented in Tables 2, 3, 4, 5 through 6, respectively. Most of the results were consistent across the subgroups defined by factors described in the Methods section.
Table 2.
Subgroup Analyses of the Studies on Total Meat Consumption and Stroke Incidence
| Total Meat | Stroke Incidence | |||
|---|---|---|---|---|
| No. | RR (95% CI) | I 2, % | P h Value | |
| Stroke subtype | ||||
| Ischemic | 4 | 1.16 (0.94–1.43) | 40.6 | 0.168 |
| Hemorrhagic | 4 | 1.41 (1.08–1.84) | 0.00 | 0.783 |
| Sex | ||||
| Male | 3 | 1.22 (1.07–1.40) | 12.5 | 0.319 |
| Female | 3 | 1.16 (1.03–1.30) | 0.00 | 0.875 |
| No. of cases | ||||
| <2000 | 4 | 1.19 (1.06–1.35) | 0.00 | 0.424 |
| ≥2000 | 2 | 1.17 (1.04–1.30) | 0.00 | 0.764 |
| Follow‐up duration | ||||
| <20 y | 2 | 1.14 (1.02–1.26) | 0.00 | 0.809 |
| ≥20 y | 4 | 1.24 (1.09–1.41) | 0.00 | 0.601 |
| Adjustment variable | ||||
| Education | ||||
| Yes | 4 | 1.15 (1.04–1.28) | 0.00 | 0.514 |
| No | 2 | 1.22 (1.07–1.40) | 0.00 | 0.706 |
| Family history of MI | ||||
| Yes | 4 | 1.17 (1.07–1.27) | 0.00 | 0.808 |
| No | 2 | 1.34 (0.91–1.95) | 26.6 | 0.243 |
| Fruit and vegetable intake | ||||
| Yes | 4 | 1.17 (1.07–1.27) | 0.00 | 0.808 |
| No | 2 | 1.34 (0.91–1.95) | 26.6 | 0.243 |
| Fish intake | ||||
| Yes | 2 | 1.14 (1.02–1.26) | 0.00 | 0.809 |
| No | 4 | 1.24 (1.09–1.41) | 0.00 | 0.601 |
| Use of aspirin | ||||
| Yes | 4 | 1.17 (1.07–1.27) | 0.00 | 0.808 |
| No | 2 | 1.34 (0.91–1.95) | 26.6 | 0.243 |
| Use of vitamin supplements | ||||
| Yes | 2 | 1.22 (1.07–1.40) | 0.00 | 0.617 |
| No | 4 | 1.15 (1.04–1.28) | 0.00 | 0.514 |
CI indicates confidence interval; P h, P value for heterogeneity; RR, relative risk.
Table 3.
Subgroup Analyses of the Studies on Red Meat Consumption and Stroke Incidence
| Red Meat | Stroke Incidence | |||
|---|---|---|---|---|
| No. | RR (95% CI) | I 2, % | P h Value | |
| Stroke subtype | ||||
| Ischemic | 5 | 1.24 (1.05–1.46) | 17.7 | 0.302 |
| Hemorrhagic | 5 | 1.11 (0.89–1.38) | 0.00 | 0.530 |
| Sex | ||||
| Male | 4 | 1.10 (0.91–1.32) | 46.0 | 0.135 |
| Female | 4 | 1.14 (1.02–1.26) | 0.00 | 0.770 |
| No. of cases | ||||
| <2000 | 4 | 1.14 (0.99–1.30) | 13.7 | 0.324 |
| ≥2000 | 4 | 1.10 (0.98–1.24) | 13.9 | 0.323 |
| Follow‐up duration | ||||
| <20 y | 4 | 1.06 (0.96–1.17) | 0.00 | 0.550 |
| ≥20 y | 4 | 1.20 (1.06–1.53) | 0.00 | 0.481 |
| Adjustment variable | ||||
| Education | ||||
| Yes | 6 | 1.10 (0.98–1.23) | 18.0 | 0.297 |
| No | 2 | 1.16 (1.02–1.33) | 0.00 | 0.624 |
| Family history of MI | ||||
| Yes | 4 | 1.11 (1.02–1.20) | 0.00 | 0.750 |
| No | 4 | 1.18 (0.88–1.57) | 46.3 | 0.133 |
| Fruit and vegetable intake | ||||
| Yes | 6 | 1.10 (1.01–1.19) | 0.00 | 0.605 |
| No | 2 | 1.41 (1.04–1.92) | 0.00 | 0.334 |
| Fish intake | ||||
| Yes | 4 | 1.06 (0.96–1.17) | 0.00 | 0.550 |
| No | 4 | 1.20 (1.06–1.35) | 0.00 | 0.481 |
| Use of aspirin | ||||
| Yes | 4 | 1.11 (1.02–1.20) | 0.00 | 0.750 |
| No | 4 | 1.18 (0.88–1.57) | 46.3 | 0.133 |
| Use of vitamin supplements | ||||
| Yes | 4 | 1.13 (1.00–1.28) | 4.70 | 0.369 |
| No | 4 | 1.11 (0.99–1.26) | 20.0 | 0.290 |
CI indicates confidence interval; MI, myocardial infarction; P h, P value for heterogeneity; RR, relative risk.
Table 4.
Subgroup Analyses of the Studies on Processed Meat Consumption and Stroke Incidence
| Processed Meat | Stroke Incidence | |||
|---|---|---|---|---|
| No. | RR (95% CI) | I 2, % | P h Value | |
| Stroke subtype | ||||
| Ischemic | 5 | 1.10 (0.96–1.27) | 11.4 | 0.341 |
| Hemorrhagic | 5 | 1.19 (0.95–1.49) | 8.10 | 0.360 |
| Sex | ||||
| Male | 4 | 1.21 (1.09–1.34) | 0.00 | 0.480 |
| Female | 4 | 1.12 (1.01–1.24) | 0.00 | 0.476 |
| No. of cases | ||||
| <2000 | 4 | 1.22 (1.09–1.37) | 0.00 | 0.943 |
| ≥2000 | 4 | 1.10 (0.96–1.26) | 39.3 | 0.176 |
| Follow‐up duration | ||||
| <20 y | 4 | 1.12 (0.95–1.31) | 36.6 | 0.193 |
| ≥20 y | 4 | 1.17 (1.05–1.30) | 0.00 | 0.674 |
| Adjustment variable | ||||
| Education | ||||
| Yes | 6 | 1.16 (1.04–1.29) | 0.60 | 0.412 |
| No | 2 | 1.16 (1.01–1.33) | 20.8 | 0.261 |
| Family history of MI | ||||
| Yes | 4 | 1.18 (1.08–1.29) | 0.00 | 0.595 |
| No | 4 | 1.05 (0.85–1.28) | 6.00 | 0.363 |
| Fruit and vegetable intake | ||||
| Yes | 6 | 1.15 (1.05–1.26) | 16.6 | 0.307 |
| No | 2 | 1.24 (0.94–1.63) | 0.00 | 0.799 |
| Fish intake | ||||
| Yes | 4 | 1.12 (0.95–1.31) | 36.6 | 0.193 |
| No | 4 | 1.17 (1.05–1.30) | 0.00 | 0.674 |
| Use of aspirin | ||||
| Yes | 4 | 1.18 (1.08–1.29) | 0.00 | 0.595 |
| No | 4 | 1.05 (0.85–1.28) | 6.00 | 0.363 |
| Use of vitamin supplements | ||||
| Yes | 4 | 1.09 (0.94–1.27) | 34.0 | 0.208 |
| No | 4 | 1.22 (1.09–1.37) | 0.00 | 0.943 |
CI indicates confidence interval; MI, myocardial infarction; P h indicates P value for heterogeneity; RR, relative risk.
Table 5.
Subgroup Analyses of the Studies on Total Meat Consumption and Stroke Mortality
| Total Meat | Stroke Mortality | |||
|---|---|---|---|---|
| No. | RR (95% CI) | I 2, % | P h Value | |
| No. of cases | ||||
| <1000 | 2 | 0.96 (0.71–1.30) | 0.00 | 0.526 |
| ≥1000 | 3 | 0.98 (0.84–1.14) | 0.00 | 0.568 |
| Follow‐up duration | ||||
| <10 y | 3 | 0.95 (0.78–1.15) | 0.00 | 0.814 |
| ≥10 y | 2 | 1.00 (0.83–1.21) | 0.00 | 0.323 |
| Adjustment variable | ||||
| Socioeconomic status | ||||
| Yes | 1 | 0.94 (0.75–1.23) | NC | NC |
| No | 4 | 0.99 (0.84–1.16) | 0.00 | 0.697 |
| History of hypertension | ||||
| Yes | 2 | 1.00 (0.83–1.21) | 0.00 | 0.323 |
| No | 3 | 0.95 (0.78–1.15) | 0.00 | 0.814 |
| Smoking | ||||
| Yes | 2 | 0.96 (0.71–1.30) | 0.00 | 0.526 |
| No | 3 | 0.98 (0.84–1.14) | 0.00 | 0.568 |
| Fruit and vegetable intake | ||||
| Yes | 3 | 0.98 (0.84–1.14) | 0.00 | 0.568 |
| No | 2 | 0.96 (0.71–1.30) | 0.00 | 0.526 |
CI indicates confidence interval; NC, not calculable; P h, heterogeneity P value; RR, relative risk.
Table 6.
Subgroup Analyses of the Studies on Red Meat Consumption and Stroke Mortality
| Red Meat | Stroke Mortality | |||
|---|---|---|---|---|
| No. | RR (95% CI) | I 2, % | P h Value | |
| Follow‐up duration | ||||
| <10 y | 2 | 0.96 (0.62–1.48) | 64.7 | 0.092 |
| ≥10 y | 2 | 0.77 (0.44–1.35) | 77.4 | 0.035 |
| Adjustment variable | ||||
| Socioeconomic status | ||||
| Yes | 3 | 0.80 (0.50–1.28) | 80.6 | 0.006 |
| No | 1 | 1.01 (0.73–1.38) | NC | NC |
| History of hypertension | ||||
| Yes | 1 | 1.01 (0.73–1.38) | NC | NC |
| No | 3 | 0.80 (0.50–1.28) | 80.6 | 0.006 |
| Smoking | ||||
| Yes | 3 | 0.76 (0.53–1.10) | 57.3 | 0.096 |
| No | 1 | 1.13 (0.95–1.34) | NC | NC |
| Fruit and vegetable intake | ||||
| Yes | 3 | 0.80 (0.50–1.28) | 80.6 | 0.006 |
| No | 1 | 1.01 (0.73–1.38) | NC | NC |
CI indicates confidence interval; NC, not calculable; P h, heterogeneity P value; RR, relative risk.
Total, red, and processed meat consumption and stroke incidence
Studies containing a small number of cases (<2000 cases) and longer follow‐up duration (≥20 years) showed a stronger association of total, processed, and red meat consumption and stroke incidence compared with other studies. In general, studies with male participants showed a stronger association of total and processed meat intake and risk of stroke. Total meat consumption was associated with hemorrhagic stroke (RR, 1.41; 95% CI, 1.08–1.84 [I 2=0.00]), but no significant association was found between total meat consumption and ischemic stroke (RR, 1.16; 95% CI, 0.94–1.43 [I 2=40.6]). A positive association between total meat consumption and stroke incidence was found regardless of sex, number of cases, and follow‐up duration. When we stratified the analysis by adjustment variables, studies that adjusted for family history of myocardial infarction, fruit and vegetable intake, and use of aspirin showed a statistically significant relationship between total meat intake and risk of stroke compared with other studies that did not include those as adjustment variables.
Red meat consumption was associated with ischemic stroke (RR, 1.24; 95% CI, 1.05–1.46 [I 2=17.7]) but not with hemorrhagic stroke (RR, 1.11; 95% CI, 0.89–1.38 [I 2=0.00]). Studies adjusted for family history of myocardial infarction and use of aspirin and vitamin supplements showed a statistically significant association between consumption of red meat and risk of stroke. Processed meat consumption was linked to neither ischemic (RR, 1.10; 95% CI, 0.96–1.27 [I 2=11.4]) nor hemorrhagic stroke (RR, 1.19; 95% CI, 0.95–1.49 [I 2=8.10]). Studies adjusted for family history of MI, fruit and vegetable intake, and use of aspirin showed a statistically significant association between processed meat intake and stroke incidence compared with other studies.
Total and red meat consumption and stroke mortality
No statistically significant association between total and red meat consumption and stroke mortality was found in subgroup analysis by number of cases, follow‐up duration, and adjustment variables.
Publication Bias and Quality Assessment
We did not detect any significant publication bias based on the Egger test except that the evaluation of total meat with stroke incidence reached the significance threshold. The P values from the Egger test for the articles related to meat consumption and stroke incidence were 0.10 for total meat, 0.59 for red meat, 0.30 for processed meat, and 0.903 for white meat. For the articles concerning meat consumption and stroke mortality, the P values from the Egger test were 0.95 for total meat and 0.11 for red meat. The average score for study quality assessed by the Newcastle‐Ottawa Scale was 7.29 (range 7–8) for studies on meat consumption and stroke incidence and 6.87 (range 6–8) for those on stroke mortality (Table S2).
Discussion
The findings from this meta‐analysis of prospective cohort studies suggest that higher consumption of total, red, and processed meats is associated with an 18%, 11%, and 17% increase in the risk of stroke, while higher intake of white meat is related to a 13% reduction in stroke incidence. We observed no association between total and red meat intake and mortality from stroke. In terms of stroke subtype, we found a significant association between red meat consumption and risk of ischemic stroke.
The underlying mechanisms for the increased risk of stroke associated with high red and processed meat consumption may relate to the nutritional content of meat. Red meat contains a large amount of saturated fats that can raise the level of plasma cholesterol,33 low‐density lipoprotein cholesterol,34 and triglycerides.35 The artery‐clogging effects of cholesterol and triglycerides may contribute to an interruption in blood flow to the brain and lead to stroke incidence. In addition, red meat is high in heme iron, which can catalyze oxidative reactions in biological systems.36 Oxidative reactions can damage lipids, proteins, and DNA, increasing the risk of metabolic, neurologic, and cardiovascular diseases.37, 38 According to one epidemiological study,39 heme iron intake was related to a 16% increased risk of stroke (hazard ratio, 1.16; 95% CI, 1.03–1.31) when comparing the highest (≥2.34 mg/d) category with the lowest (<1.28 mg/d) category.
Furthermore, processed meat is often manufactured with the preservative sodium nitrate,40 which elevates the risk of hypertension and consequently exerts negative effects on the cardiovascular systems.41, 42, 43 According to reviews, high blood pressure is a major risk factor for stroke; thus, lowering blood pressure can contribute to a reduction in stroke risk across different geographic regions and population groups.44, 45 High blood pressure may contribute to an increased risk of stroke risk because of the elevated force placed on the walls of arteries, which facilitates damage and the accumulation of circulating particles.46 However, regarding the possibility of the imprecision and variability of sodium nitrate concentration in processed meat, the extent to which sodium nitrate in processed meat could induce high blood pressure and stroke needs to be examined in future studies.
In contrast to red and processed meats, white meat contains less heme iron and is high in polyunsaturated fat. A previous study showed that a diet consisting of polyunsaturated fats as the primary source of fatty acids can lower low‐density lipoprotein cholesterol (LDL‐C).47 Compared with no change or an increase in low‐density lipoprotein cholesterol, the lowering of low‐density lipoprotein cholesterol was related to a decreased risk of stroke and coronary heart disease.48 Despite this plausible mechanism, further studies are required to investigate the biological mechanism that can explain the protective effect of poultry meat consumption on stroke risk.
In our study, red meat consumption was associated with stroke incidence, not mortality. More than two thirds of stroke cases are ischemic strokes49, 50 and ischemic strokes are generally associated with lower mortality compared with hemorrhagic stroke because of the nature of their pathogenesis.51 The former occurs from a clotting in blood vessels, whereas the latter occurs as a result of a rupture of blood vessels, which is fatal and may need additional clinical attention. In addition, considerable heterogeneity was found in the evaluation of red meat consumption and stroke mortality in this study. Given the limited number of published studies on meat consumption and stroke mortality, more studies are warranted to make a definite conclusion on this relationship.
Study Strengths and Limitations
There are several strengths in our study. By including only prospective cohort studies, we were able to minimize the effects from possible recall and selection. To our knowledge, our study is the first to examine stroke incidence and mortality separately and to include white meat, which were not considered in previous meta‐analyses.8, 9, 10, 11 Limitations of this meta‐analysis also need to be addressed when interpreting the results. Because our meta‐analysis was based on observational studies, we could not entirely eliminate the effect of confounding from unadjusted risk factors. Several previous researches reported that stroke incidence is greater among participants with a higher consumption of red and processed meats because they tend to have unhealthy behaviors and conditions.15, 24, 25 Although studies included in this meta‐analysis adjusted for major stroke risk factors such as hypertension, diabetes mellitus, smoking, obesity, and alcohol use, the effect of unadjusted risk factors still remain. Quantification of meat consumption through a self‐reported survey in the selected studies may have led to a misclassification of the different types of meat caused by a measurement error. Because categorization of high versus low meat intake used to assess RR reflects characteristics of the population in each study, quantity of meat intake dividing high versus low consumption groups were not entirely consistent in the studies included in this meta‐analysis. Therefore, further investigation should standardize the comparison between highest and lowest meat consumption and risk of stroke incidence and mortality to account for this variability.
In addition, the tendency to publish only positive results may have influenced the results of this meta‐analysis. However, we found no evidence of publication bias in this study except for the results of total meat consumption and stroke incidence that met the threshold. Possible sources of this publication bias is the existence of unpublished studies in other continents since all of the data available for the evaluation of total meat consumption and stroke incidence were from Europe and North America. Further evaluation of publication bias on this result is required when more studies become available. In this study, we were not able to perform analyses on the associations between processed and white meat consumption and stroke mortality because of limitation of data. It is necessary to examine these relationships when relevant data are published in the future.
In our study, we separately examined the association between consumption of total, red, processed, and white meats and risk of stroke and deaths from stroke. Previous meta‐analyses that showed a positive association between total, red, and processed meat intake and risk of stroke have not distinguished stroke incidence from stroke mortality and synthesized the results from all studies. In our meta‐analysis, we found no significant association between consumption of total and red meat and deaths from stroke. In terms of stroke subtype, previous meta‐analyses indicated that there was no association between total, red, and processed meat intake and hemorrhagic stroke.8, 10 However, the present meta‐analysis shows that total meat consumption is significantly related to hemorrhagic stroke. Since more studies are included in our meta‐analysis, our analysis had higher statistical power to assess the relationship between total meat intake and risk of hemorrhagic stroke.
Although our findings on the association between the high consumption of total, red, and processed meats and an increase in the risk of stroke events are consistent with previous studies, our meta‐analysis has some additions to the current topic that may have clinical importance. We found evidence that the consumption of white meat is related to a lower risk of stroke. Individuals who are at a higher risk of stroke who habitually consume red and processed meats should consider substituting a source of their protein intake to white meat.
Conclusions
High meat consumption, particularly red and processed meats, is associated with increased risk of stroke. In contrast, white meat consumption is associated with reduced risk of stroke. While no association was found between any meat consumption and stroke mortality, more studies are warranted to confirm this finding.
Author Contributions
K.K. conducted the systematic review, selected the studies for meta‐analysis (cross‐checked by J.H. and under the supervision of S.M.P.), and wrote the first draft of the article. J.H., S.A.L, S.O.K., H.L., N.K., J.K.L., and S.M.P. provided the important intellectual content for the draft. S.A.L., S.O.K, H.J.L., N.K., J.K.L., and S.M.P. supervised the meta‐analysis and draft and critically revised the article.
Sources of Funding
This research was supported by a research grant (16162MFDS590) provided from the Ministry of Food and Drug Safety in the Republic of Korea in 2016. Kim received a scholarship from the BK21‐plus education program provided by the National Research Foundation of Korea.
Disclosures
None.
Supporting information
Table S1. Search Strategy
Table S2. Quality Assessment of Studies Selected for Final Meta‐Analysis Based on the Newcastle‐Ottawa Scale
Acknowledgments
We would like to thank Brenda Beck, DO (University Hospitals Cleveland Medical Center) for providing the English proofreading.
(J Am Heart Assoc. 2017;6:e005983 DOI: 10.1161/JAHA.117.005983.)28855166
Part of this study was presented at the 3rd European Stroke Organization Conference, May 16—18, 2017, in Prague, Czech Republic.
References
- 1. Bonita R, Mendis S, Truelsen T, Bogousslavsky J, Toole J, Yatsu F. The global stroke initiative. Lancet Neurol. 2004;3:391–393. [DOI] [PubMed] [Google Scholar]
- 2. Adamson J, Beswick A, Ebrahim S. Is stroke the most common cause of disability? J Stroke Cerebrovasc Dis. 2004;13:171–177. [DOI] [PubMed] [Google Scholar]
- 3. Feigin VL, Forouzanfar MH, Krishnamurthi R, Mensah GA, Connor M, Bennett DA, Moran AE, Sacco RL, Anderson L, Truelsen T. Global and regional burden of stroke during 1990–2010: findings from the Global Burden of Disease Study 2010. Lancet. 2014;383:245–255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Johnston SC, Mendis S, Mathers CD. Global variation in stroke burden and mortality: estimates from monitoring, surveillance, and modelling. Lancet Neurol. 2009;8:345–354. [DOI] [PubMed] [Google Scholar]
- 5. He FJ, Nowson CA, MacGregor GA. Fruit and vegetable consumption and stroke: meta‐analysis of cohort studies. Lancet. 2006;367:320–326. [DOI] [PubMed] [Google Scholar]
- 6. Dauchet L, Amouyel P, Dallongeville J. Fruit and vegetable consumption and risk of stroke a meta‐analysis of cohort studies. Neurology. 2005;65:1193–1197. [DOI] [PubMed] [Google Scholar]
- 7. Joshipura KJ, Ascherio A, Manson JE, Stampfer MJ, Rimm EB, Speizer FE, Hennekens CH, Spiegelman D, Willett WC. Fruit and vegetable intake in relation to risk of ischemic stroke. JAMA. 1999;282:1233–1239. [DOI] [PubMed] [Google Scholar]
- 8. Kaluza J, Wolk A, Larsson SC. Red meat consumption and risk of stroke a meta‐analysis of prospective studies. Stroke. 2012;43:2556–2560. [DOI] [PubMed] [Google Scholar]
- 9. Micha R, Wallace SK, Mozaffarian D. Red and processed meat consumption and risk of incident coronary heart disease, stroke, and diabetes mellitus a systematic review and meta‐analysis. Circulation. 2010;121:2271–2283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Chen G, Lv D, Pang Z, Liu Q. Red and processed meat consumption and risk of stroke: a meta‐analysis of prospective cohort studies. Eur J Clin Nutr. 2013;67:91–95. [DOI] [PubMed] [Google Scholar]
- 11. Yang C, Pan L, Sun C, Xi Y, Wang L, Li D. Red meat consumption and the risk of stroke: a dose–response meta‐analysis of prospective cohort studies. J Stroke Cerebrovasc Dis. 2016;25:1177–1186. [DOI] [PubMed] [Google Scholar]
- 12. Daniel CR, Cross AJ, Koebnick C, Sinha R. Trends in meat consumption in the USA. Public Health Nutr. 2011;14:575–583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Fisher M, Lees K, Spence JD. Nutrition and stroke prevention. Stroke. 2006;37:2430–2435. [DOI] [PubMed] [Google Scholar]
- 14. He K, Merchant A, Rimm EB, Rosner BA, Stampfer MJ, Willett WC, Ascherio A. Dietary fat intake and risk of stroke in male US healthcare professionals: 14 year prospective cohort study. BMJ. 2003;327:777–782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Bernstein AM, Pan A, Rexrode KM, Stampfer M, Hu FB, Mozaffarian D, Willett WC. Dietary protein sources and the risk of stroke in men and women. Stroke. 2012;43:637–644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta‐analyses: the PRISMA statement. Ann Intern Med. 2009;151:264–269. [DOI] [PubMed] [Google Scholar]
- 17. Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, Moher D, Becker BJ, Sipe TA, Thacker SB. Meta‐analysis of observational studies in epidemiology: a proposal for reporting. JAMA. 2000;283:2008–2012. [DOI] [PubMed] [Google Scholar]
- 18. Lippi G, Mattiuzzi C, Cervellin G. Meat consumption and cancer risk: a critical review of published meta‐analyses. Crit Rev Oncol Hematol. 2016;97:1–14. [DOI] [PubMed] [Google Scholar]
- 19. Wells G, Shea B, O'connell D, Peterson J, Welch V, Losos M, Tugwell P. The Newcastle‐Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta‐analyses. 2000.
- 20. Altman DG, Bland JM. Interaction revisited: the difference between two estimates. BMJ. 2003;326:219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. DerSimonian R, Laird N. Meta‐analysis in clinical trials. Control Clin Trials. 1986;7:177–188. [DOI] [PubMed] [Google Scholar]
- 22. Higgins J, Thompson SG. Quantifying heterogeneity in a meta‐analysis. Stat Med. 2002;21:1539–1558. [DOI] [PubMed] [Google Scholar]
- 23. Egger M, Smith GD, Schneider M, Minder C. Bias in meta‐analysis detected by a simple, graphical test. BMJ. 1997;315:629–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Larsson SC, Virtamo J, Wolk A. Red meat consumption and risk of stroke in Swedish men. Am J Clin Nutr. 2011;94:417–421. [DOI] [PubMed] [Google Scholar]
- 25. Larsson SC, Virtamo J, Wolk A. Red meat consumption and risk of stroke in Swedish women. Stroke. 2011;42:324–329. [DOI] [PubMed] [Google Scholar]
- 26. Haring B, Misialek JR, Rebholz CM, Petruski‐Ivleva N, Gottesman RF, Mosley TH, Alonso A. Association of dietary protein consumption with incident silent cerebral infarcts and stroke the Atherosclerosis Risk in Communities (ARIC) study. Stroke. 2015;46:3443–3450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Yaemsiri S, Sen S, Tinker L, Rosamond W, Wassertheil‐Smoller S, He K. Trans fat, aspirin, and ischemic stroke in postmenopausal women. Ann Neurol. 2012;72:704–715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Nagao M, Iso H, Yamagishi K, Date C, Tamakoshi A. Meat consumption in relation to mortality from cardiovascular disease among Japanese men and women. Eur J Clin Nutr. 2012;66:687–693. [DOI] [PubMed] [Google Scholar]
- 29. Sharma S, Cruickshank JK, Green DM, Vik S, Tome A, Kolonel LN. Impact of diet on mortality from stroke: results from the US multiethnic cohort study. J Am Coll Nutr. 2013;32:151–159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Amiano P, Chamosa S, Etxezarreta N, Arriola L, Sánchez M, Ardanaz E, Molina‐Montes E, Chirlaque M, Moreno‐Iribas C, Huerta J. Unprocessed red meat and processed meat consumption and risk of stroke in the Spanish cohort of the European Prospective Investigation into Cancer and Nutrition (EPIC). Eur J Clin Nutr. 2016;70:313–319. [DOI] [PubMed] [Google Scholar]
- 31. Sauvaget C, Nagano J, Allen N, Grant EJ, Beral V. Intake of animal products and stroke mortality in the Hiroshima/Nagasaki Life Span Study. Int J Epidemiol. 2003;32:536–543. [DOI] [PubMed] [Google Scholar]
- 32. Takata Y, Shu XO, Gao YT, Li H, Zhang X, Gao J, Cai H, Yang G, Xiang YB, Zheng W. Red meat and poultry intakes and risk of total and cause‐specific mortality: results from cohort studies of Chinese adults in Shanghai. PLoS One. 2013;8:e56963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Mensink RP, Zock PL, Kester AD, Katan MB. Effects of dietary fatty acids and carbohydrates on the ratio of serum total to HDL cholesterol and on serum lipids and apolipoproteins: a meta‐analysis of 60 controlled trials. Am J Clin Nutr. 2003;77:1146–1155. [DOI] [PubMed] [Google Scholar]
- 34. Mensink RP, Katan MB. Effect of dietary trans fatty acids on high‐density and low‐density lipoprotein cholesterol levels in healthy subjects. N Engl J Med. 1990;323:439–445. [DOI] [PubMed] [Google Scholar]
- 35. Shepherd J, Packard CJ, Grundy SM, Yeshurun D, Gotto A, Taunton O. Effects of saturated and polyunsaturated fat diets on the chemical composition and metabolism of low density lipoproteins in man. J Lipid Res. 1980;21:91–99. [PubMed] [Google Scholar]
- 36. Carlsen CU, Møller JK, Skibsted LH. Heme‐iron in lipid oxidation. Coord Chem Rev. 2005;249:485–498. [Google Scholar]
- 37. Tappel A. Heme of consumed red meat can act as a catalyst of oxidative damage and could initiate colon, breast and prostate cancers, heart disease and other diseases. Med Hypotheses. 2007;68:562–564. [DOI] [PubMed] [Google Scholar]
- 38. Meneghini R. Iron homeostasis, oxidative stress, and DNA damage. Free Radic Biol Med. 1997;23:783–792. [DOI] [PubMed] [Google Scholar]
- 39. Kaluza J, Wolk A, Larsson SC. Heme iron intake and risk of stroke a prospective study of men. Stroke. 2013;44:334–339. [DOI] [PubMed] [Google Scholar]
- 40. Honikel KO. The use and control of nitrate and nitrite for the processing of meat products. Meat Sci. 2008;78:68–76. [DOI] [PubMed] [Google Scholar]
- 41. Alderman MH. Evidence relating dietary sodium to cardiovascular disease. J Am Coll Nutr. 2006;25:256S–261S. [DOI] [PubMed] [Google Scholar]
- 42. Micha R, Michas G, Lajous M, Mozaffarian D. Processing of meats and cardiovascular risk: time to focus on preservatives. BMC Med. 2013;11:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Farquhar WB, Edwards DG, Jurkovitz CT, Weintraub WS. Dietary sodium and health: more than just blood pressure. J Am Coll Cardiol. 2015;65:1042–1050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Lawes CM, Bennett DA, Feigin VL, Rodgers A. Blood pressure and stroke an overview of published reviews. Stroke. 2004;35:776–785. [DOI] [PubMed] [Google Scholar]
- 45. Willmot M, Leonardi‐Bee J, Bath PM. High blood pressure in acute stroke and subsequent outcome a systematic review. Hypertension. 2004;43:18–24. [DOI] [PubMed] [Google Scholar]
- 46. Leonardi‐Bee J, Bath PM, Phillips SJ, Sandercock PA. Blood pressure and clinical outcomes in the International Stroke Trial. Stroke. 2002;33:1315–1320. [DOI] [PubMed] [Google Scholar]
- 47. Mattson FH, Grundy SM. Comparison of effects of dietary saturated, monounsaturated, and polyunsaturated fatty acids on plasma lipids and lipoproteins in man. J Lipid Res. 1985;26:194–202. [PubMed] [Google Scholar]
- 48. Amarenco P, Goldstein LB, Szarek M, Sillesen H, Rudolph AE, Callahan A, Hennerici M, Simunovic L, Zivin JA, Welch KMA. Effects of intense low‐density lipoprotein cholesterol reduction in patients with stroke or transient ischemic attack the Stroke Prevention by Aggressive Reduction in Cholesterol Levels (SPARCL) trial. Stroke. 2007;38:3198–3204. [DOI] [PubMed] [Google Scholar]
- 49. Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, Das SR, de Ferranti S, Després JP, Fullerton HJ. Executive summary: heart disease and stroke statistics—2016 update: a report from the American Heart Association. Circulation. 2016;133:447. [DOI] [PubMed] [Google Scholar]
- 50. Koton S, Schneider AL, Rosamond WD, Shahar E, Sang Y, Gottesman RF, Coresh J. Stroke incidence and mortality trends in us communities, 1987 to 2011. JAMA. 2014;312:259–268. [DOI] [PubMed] [Google Scholar]
- 51. Andersen KK, Olsen TS, Dehlendorff C, Kammersgaard LP. Hemorrhagic and ischemic strokes compared stroke severity, mortality, and risk factors. Stroke. 2009;40:2068–2072. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Search Strategy
Table S2. Quality Assessment of Studies Selected for Final Meta‐Analysis Based on the Newcastle‐Ottawa Scale


