Abstract
Background
In the United States, there are persistent racial and ethnic disparities in cardiovascular disease morbidity and mortality. National efforts have focused on reducing these disparities; however, little is known about the long‐term trends in racial/ethnic disparities in cardiovascular health (CVH).
Methods and Results
We included 11 285 adults aged ≥20 years from the National Health and Nutrition Examination Surveys survey cycles 1999/2000 through 2011/2012. CVH includes 7 health factors and behaviors—diet, physical activity, smoking status, body mass index, blood pressure, blood glucose, and total cholesterol—each scored as ideal (2 points), intermediate (1 point), or poor (0 points). Overall CVH is a summation of these scores (range, 0–14) points. Age‐adjusted mean CVH scores were calculated by race/ethnicity (non‐Hispanic black, non‐Hispanic white, or Mexican American) and sex for each survey cycle. Non‐Hispanic black women had significantly lower mean CVH scores as compared with non‐Hispanic white women at each survey cycle (difference=0.93; P=0.001 in 2011/2012) and Mexican‐American women had significantly lower mean score as compared with non‐Hispanic white women at almost all survey cycles (difference=0.71; P=0.02 in 2011/2012). Differences between racial/ethnic groups were smaller for men and were mostly nonsignificant.
Conclusions
From 1999/2000 to 2011/2012, there were enduring disparities in CVH for non‐Hispanic black and Mexican‐American women as compared with non‐Hispanic white women. Disparities that were present in 1999/2000 were present in 2011/2012, though no racial/ethnic differences became more pronounced over time. These findings provide US nationally representative data to evaluate health factors and behaviors of particular concern regarding racial/ethnic disparities in cardiovascular health.
Keywords: 2020 Strategic Impact Goals, cardiovascular health, race and ethnicity, sex, trends
Subject Categories: Race and Ethnicity, Women, Risk Factors, Primary Prevention, Epidemiology
Clinical Perspective
What Is New?
In a study that examined trends in cardiovascular health over time by race and sex, there were consistent disparities in cardiovascular health for non‐Hispanic black and Mexican‐American women as compared with non‐Hispanic white women.
What Are the Clinical Implications?
Cardiovascular health has been linked to lower risk of clinical cardiovascular disease. Clinician efforts to eliminate cardiovascular disease disparities must include culturally competent approaches to prevention aimed specifically at minority women.
Introduction
Despite declines in cardiovascular mortality over the past 50 years, cardiovascular disease (CVD) remains the leading cause of death in the United States across all racial and ethnic groups.1 There are significant racial and sex differences in the burden of CVD. Non‐Hispanic (NH) blacks have higher incidence of coronary heart disease, heart failure, stroke, and overall CVD mortality as compared with NH whites.1, 2 CVD burden in Hispanics as compared with NH whites is mixed; whereas Hispanics have lower overall CVD mortality, incidence rates for coronary heart disease and stroke appear to be higher.3 However, US Hispanics are an aggregated ethnicity that includes multiple heritage groups, and previous research has shown highly varying prevalence of CVD and CVD risk factor prevalence by Hispanic background.4 Within race/ethnicity groups, CVD rates are elevated in men compared with women. Eliminating health disparities is a core goal of public health efforts, including the Healthy People 2020 initiative and the current American Heart Association (AHA) Strategic Impact Goals.5, 6
In order to measure, monitor, and modify a positive construct associated with CVD‐free longevity, the AHA has defined cardiovascular health (CVH) according to 7 health factors and behaviors—diet, physical activity, smoking status, body mass index (BMI), blood pressure, blood glucose, and total cholesterol—each categorized into an ideal, intermediate, or poor status.6 Numerous studies have demonstrated that better CVH is associated greater longevity and lower cardiovascular incidence, cardiovascular mortality, and all‐cause mortality across racial/ethnic groups.7, 8, 9
Racial and ethnic disparities in CVH may be indicative of future disparities in CVD incidence. Past studies have consistently found that NH whites have higher mean number of ideal health factors and behaviors as compared with NH blacks and Hispanics in aggregate.10 As compared with NH whites, nonwhites (including Hispanics) are less likely to be in the ideal category for BMI, diet, physical activity, blood pressure, and blood glucose and more likely to be in the ideal category for total cholesterol and smoking status.11, 12 Further stratifying by sex yields additional variation. Little is known about how these racial/ethnic patterns may have changed over the past decade.
In this analysis, we sought to examine trends from 1999/2000 through 2011/2012 in racial/ethnic differences in overall CVH and the 7 behaviors and factors that comprise the CVH score. Therefore, using the US nationally representative National Health and Nutrition Examination Survey, we examined racial/ethnic differences in CVH overall and for each individual component from 1999 through 2012. We present age‐adjusted mean scores and multiple metrics assessing significant differences and trends by race/ethnicity and sex.
Methods
Data Source and Study Population
The National Health and Nutrition Examination Survey (NHANES) is a nationally representative cross‐sectional sample of the civilian, noninstitutionalized US population. Since 1999, NHANES data collection has occurred in 2‐year survey cycles; we used data from participants of 7 survey cycles (1999/2000 through 2011/2012). Because our primary outcome was the composite CVH measure, which includes laboratory measured health factors, we included participants from the NHANES fasting subsample, for a total of 13 249 Mexican‐American, NH black, and NH white adults aged ≥20 years. Other racial and ethnic groups were not appropriately sampled in each survey cycle to allow for reliable calculation of subpopulation estimates. We excluded participants who were pregnant or breastfeeding at the time of the exam (n=553). We further excluded from the sample persons who did not have reported values for all 7 of the risk factors and behaviors that comprise CVH (n=1401). The resulting combined analytical sample for 1999–2012 included 11 285 individuals. NHANES data collection was approved by the National Center for Health Statistics Research Ethics Review Board for each survey cycle, and all participants provided written informed consent.
Demographic Characteristics
Self‐reported race/ethnicity (Mexican American, NH black, and NH white), sex (male, female), age (in years), country of birth (US versus all other countries), educational attainment (high school diploma or less, some college or more), and household size and income were collected for each NHANES participant. We defined lower income as household incomes less than 185% of the US federal poverty level adjusted for household size and higher income as household incomes equal or greater than 185% of the US federal poverty level adjusted for household size.
CVH Factors
Anthropomorphic measures were obtained by trained health technicians in the NHANES mobile examination center. BMI was calculated as weight in kilograms/height in meters2. Measures of systolic and diastolic blood pressure were taken either in the mobile examination center or during home examinations using a mercury sphygmomanometer after 5 minutes of quiet sitting. Three consecutive readings were attempted; systolic blood pressure and diastolic blood pressure variables were averaged from all but the first reading if multiple readings were obtained, or the first reading if only one reading was obtained. Participants selected for venipuncture blood draw were requested to fast for at least 12 hours before the visit to the mobile examination center. Total cholesterol levels and plasma glucose were assessed from these blood samples in a central NHANES laboratory. Further protocol details regarding blood collection and processing are available in the NHANES Laboratory/Medical Technologists Procedures Manual (http://www.cdc.gov/nchs/nhanes/nhanes_questionnaires.htm). Current medication usage for hypertension, hypercholesterolemia, and diabetes mellitus was assessed during an in‐home interview.
CVH Behaviors
Dietary assessment utilized two 24‐hour recall interviews, 1 conducted in the mobile examination center and a second conducted 3 to 10 days later by telephone. A standardized set of measuring guides were provided to participants to assist in estimating portion sizes of all foods consumed. Using the MyPyramid Equivalents Database and methodology from the US Department of Agriculture,13 we calculated intake of 5 dietary components: cups of fruits and vegetables (daily); 3.5‐oz servings of fish (weekly); 1‐oz servings of whole grains (daily); milligrams of sodium intake (daily); and kilocalories from sugar‐sweetened beverages (weekly), scaling intake to a 2000‐kcal daily diet. Physical activity was assessed by a series of questions on the frequency and duration of leisure‐time activities done for at least 10 minutes continuously. Participants were queried as to whether activity was of vigorous intensity—characterized by heavy sweating or large increases in breathing or heart rate, or moderate intensity—characterized by light sweating or small increases in breathing or heart rate. Examples of vigorous‐ and moderate‐intensity activities were provided for guidance, but ultimately the participant determined and reported the intensity of their activity. Smoking status was self‐reported by questions about whether the participant was currently smoking or had formerly smoked cigarettes, cigars, or pipe tobacco.
Calculation of the CVH Score
CVH was defined as in previous publications.14, 15 Each health behavior and factor was assigned a score of 0, 1, or 2, based on the criteria outlined in Table 1, corresponding to poor, intermediate, or ideal health as outlined in the AHA Strategic Impact Goals.6 The scores for each component were summed for a composite CVH score (range, 0–14), with a higher score indicating better cardiovascular health.
Table 1.
American Heart Association 2020 Strategic Impact Goal Definition Ideal, Intermediate, and Poor for Each Cardiovascular Risk Factor and Behavior, Adults Aged ≥20 Years
| Criteria | Ideal (Score=2) | Intermediate (Score=1) | Poor (Score=0) |
|---|---|---|---|
| Dieta | 4 to 5 dietary components | 2 to 3 dietary components | 0 to 1 dietary components |
| Physical activityb | ≥150 minutes moderate/vigorous activity per wk | 1 to 149 minutes moderate/vigorous activity per wk | No physical activity |
| Smoking | Never smoker or former smoker, quit >12 mo before | Former smoker, quit ≤12 mo before | Current smoker |
| Body mass index | <25 kg/m2 | 25 to 29.9 kg/m2 | ≥30 kg/m2 |
| Blood pressure | SBP <120 and DBP <80 mm Hg | SBP 120 to 139 or DBP 80 to 89, or treated to SBP <140/DBP <90 mm Hg | SBP ≥140 or DBP ≥90 mm Hg |
| Total cholesterol | <200 mg/dL | 200 to 239 or treated to <200 mg/dL | ≥240 mg/dL |
| Glucose | <100 mg/dL | 100 to 125 or treated to <100 mg/dL | ≥126 mg/dL |
DBP indicates diastolic blood pressure; SBP, systolic blood pressure.
The 5 dietary score components include ≥4.5 cups/day of fruits/vegetables, ≥2 servings of fish per week (3.5 oz), ≥3 servings of whole grains per day (1 oz), <1500 mg/day of sodium, and <450 kcal/week of sugar‐sweetened beverages. Dietary values are scaled to a 2000 kcal/day diet.
Vigorous physical activity minutes were doubled for combination with moderate activity minutes.
Statistical Analyses
All analyses were conducted in SAS software (version 9.4; SAS Institute Inc, Cary, NC) using survey analysis procedures (PROC SURVEYREG) to incorporate the complex, multistage survey sampling design of the NHANES, and using the smallest population subsample weight: the 2‐year fasting sample weight. Sex‐stratified and age‐adjusted means were calculated for each race/ethnicity group across NHANES survey cycles for the overall CVH score as well as the individual score components. We used the 2000 US Census population estimates for direct age adjustment using 4 age‐group strata (20–39, 35–49, 50–64, and ≥65 years).
Homogeneity in scores across race/ethnicity groups at each time point was estimated by an age‐adjusted Wald F test. In addition, pair‐wise comparisons of adjusted CVH scores were conducted to determine which race/ethnicity groups were significantly different from one another. We used Bonferroni adjustment in pair‐wise comparisons to account for multiple testing. Time trends from 1999/2000 to 2011/2012 were assessed by weighted linear regression models, first stratified by race/ethnicity and then including an interaction term time by race/ethnicity to test for differences in trends. Previous studies of CVH using NHANES data have indicated linear models as the appropriate functional form.15 Sensitivity analyses included further stratification by income and educational attainment category to determine whether socioeconomic status accounted for racial/ethnic differences.
Results
Unadjusted demographic characteristics of the sample are listed in Table 2 by race/ethnicity and sex. As compared with NH whites, NH black and Mexican‐American participants were younger with lower levels of educational attainment and income. More than half of Mexican Americans were born outside of the United States, a higher proportion than for NH blacks and NH whites.
Table 2.
Demographic Characteristics of US Adults Aged ≥20 Years by Race/Ethnicity and Sex: NHANES 1999–2012
| Characteristica | Non‐Hispanic White Mean or Percentage (95% CI) | Non‐Hispanic Black Mean or Percentage (95% CI) | Mexican American Mean or Percentage (95% CI) | |||
|---|---|---|---|---|---|---|
| Men (n=3280) | Women (n=3107) | Men (n=1172) | Women (n=1248) | Men (n=1300) | Women (n=1178) | |
| Age group, y, % | ||||||
| 20 to 34 | 25.4 (23.5–27.4) | 22.6 (20.9–24.3) | 36.8 (33.5–40.1) | 31.9 (28.9–34.8) | 46.9 (43.4–50.5) | 40.9 (36.8–45.1) |
| 35 to 49 | 31.7 (29.6–33.8) | 29.4 (27.2–31.6) | 31.9 (28.6–35.2) | 33.8 (31.1–36.5) | 33.4 (30.5–36.3) | 32.1 (28.6–35.5) |
| 50 to 64 | 25.6 (23.6–27.7) | 26.9 (25.1–28.8) | 21.8 (19.6–24.1) | 22.1 (20.1–24.2) | 14.0 (12.1–15.8) | 18.1 (15.3–20.8) |
| 65+ | 17.2 (16–18.5) | 21.1 (19.6–22.6) | 9.5 (8.0–10.9) | 12.2 (10.6–13.7) | 5.7 (4.7–6.7) | 8.9 (7.3–10.6) |
| Age, y, M | 47.3 (46.5–48.0) | 49.2 (48.5–50.0) | 42.1 (41.2–43.1) | 44.2 (43.0–45.3) | 38.2 (37.1–39.2) | 41.0 (39.6–42.3) |
| Country of birth | ||||||
| US born | 95.3 (94–96.5) | 95.9 (95–96.8) | 88.7 (85.9–91.5) | 91.9 (89.1–94.6) | 37.2 (32.2–42.1) | 43.7 (39.6–47.7) |
| Foreign born | 4.7 (3.5–6.0) | 4.1 (3.2–5.0) | 11.3 (8.5–14.1) | 8.1 (5.4–10.9) | 62.8 (57.9–67.8) | 56.3 (52.3–60.4) |
| Education | ||||||
| ≤High school | 38.7 (35.6–41.8) | 38.5 (35.6–41.4) | 56.1 (52.8–59.4) | 45.9 (42.8–49) | 74.9 (71.3–78.5) | 68.5 (64.9–72.1) |
| ≥Some college | 61.3 (58.2–64.4) | 61.5 (58.6–64.4) | 43.9 (40.6–47.2) | 54.1 (51–57.2) | 25.1 (21.5–28.7) | 31.5 (27.9–35.1) |
| Incomeb | ||||||
| Lower income | 22.1 (19.3–24.9) | 26.9 (24.4–29.4) | 42.2 (38.6–45.9) | 49.8 (46.1–53.5) | 56.4 (52.5–60.3) | 60.1 (55.4–64.7) |
| Higher income | 77.9 (75.1–80.7) | 73.1 (70.6–75.6) | 57.8 (54.1–61.4) | 50.2 (46.5–53.9) | 43.6 (39.7–47.5) | 39.9 (35.3–44.6) |
| Systolic blood pressure, M | 122.5 (121.8–123.3) | 119.5 (118.7–120.3) | 125.5 (124.2–126.6) | 123.5 (121.9–125.1) | 119.9 (118.8–121.1) | 116.5 (114.9–118.0) |
| Diastolic blood pressure, M | 71.8 (71.3–72.4) | 68.7 (68.0–69.3) | 73.2 (72.2–74.2) | 70.5 (69.5–71.4) | 70.5 (69.4–71.5) | 67.9 (67.1–68.7) |
| Total cholesterol, M | 196.4 (194.7–198.2) | 203.2 (201.6–204.8) | 190.8 (188.0–193.6) | 193.0 (190.5–195.6) | 198.1 (195.4–200.8) | 193.8 (190.7–196.9) |
| Fasting blood glucose, M | 104.7 (103.6–105.8) | 98.9 (97.9–99.9) | 105.3 (102.4–108.3) | 103.3 (101.2–105.5) | 108.4 (105.7–111.2) | 105.1 (102.0–108.2) |
| Taking BP‐lowering medication, % | 22.6 (20.6–24.6) | 22.9 (20.9–24.9) | 20.0 (17.3–22.8) | 32.9 (29.2–36.6) | 9.6 (7.2–12.0) | 12.8 (10.1–15.6) |
| Taking lipid‐lowering medication, % | 17.2 (15.7–18.8) | 15.0 (13.3–16.6) | 11.5 (9.1–13.9) | 12.4 (10.3–14.5) | 7.4 (5.5–9.3) | 10.1 (7.5–12.6) |
| Taking diabetes mellitus medication, % | 4.9 (4.0–5.9) | 3.8 (3.0–4.5) | 6.0 (4.5–7.5) | 8.4 (6.8–10.0) | 5.8 (4.3–7.4) | 6.3 (4.4–8.2) |
| Current smoker, % | 25.5 (23.3–27.7) | 21.4 (19.6–23.2) | 31.5 (28.2–34.8) | 19.1 (16.5–21.6) | 24.6 (21.6–27.6) | 11.8 (9.5–14.0) |
| Previously had CVD event, %c | 10.1 (8.9–11.3) | 6.7 (5.6–7.8) | 6.4 (5.1–7.8) | 7.7 (6.3–9.1) | 3.5 (2.5–4.6) | 4.0 (2.5–5.4) |
BP indicates blood pressure; CI, confidence interval; CVD, cardiovascular disease; NHANES, National Health and Nutrition Examination Surveys.
Sample sizes are unweighted numbers of each race/ethnicity and sex category; percentages are weighted to reflect NHANES complex, multistage survey sampling.
Lower income defined as household income <185% of the US federal poverty level adjusted for household size; higher income defined as household income ≥185% of the US federal poverty level adjusted for household size.
Previous CVD events include self‐reported congestive heart failure, coronary heart disease, heart attack, and stroke.
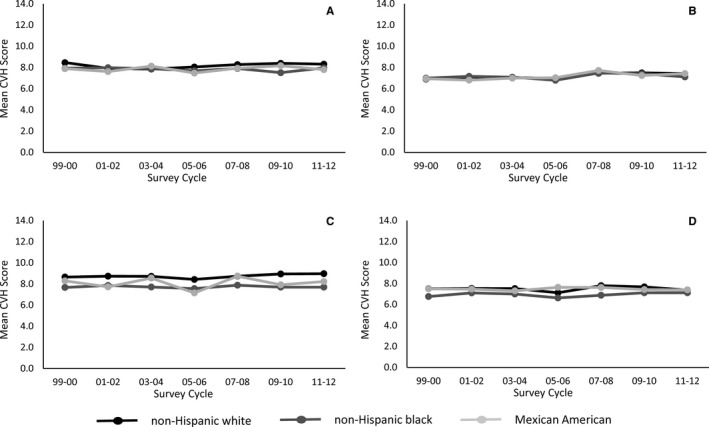
Across the NHANES survey cycles, the age‐adjusted mean CVH score remained nearly flat, from 7.9 (95% confidence interval, 7.6–8.3) in 1999/2000 to 8.1 (95% confidence interval, 7.8–8.3) in 2011/2012. CVH scores increased slightly from 1999/2000 to 2011/2012 within each sex and race/ethnicity category, but only Mexican‐American men and NH white men had significant increases over time (Figure 1; Table 3).
Figure 1.
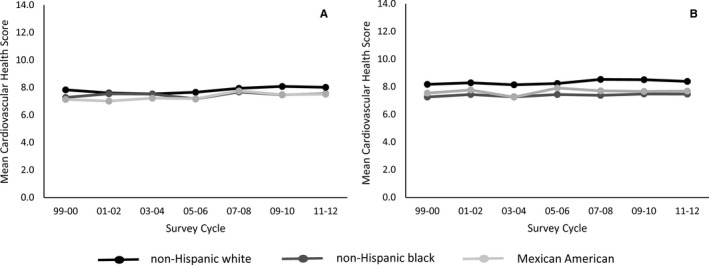
Trends in age‐adjusted mean cardiovascular health score for US adults aged ≥20 years by sex and race/ethnicity, National Health and Nutrition Examination Surveys 1999–2012. A, Men. B, Women.
Table 3.
Age‐Adjusted Mean Cardiovascular Health Score for US Adults Aged ≥20 Years by Sex, Race/Ethnicity, and NHANES Survey Cycle
| Age‐Adjusted Mean Score (95% CI) by NHANES Survey Cycle | P linear trend | P interaction | |||||||
|---|---|---|---|---|---|---|---|---|---|
| 1999–2000 | 2001–2002 | 2003–2004 | 2005–2006 | 2007–2008 | 2009–2010 | 2011–2012 | |||
| Men | |||||||||
| NH white | 7.83 (7.45–8.20) | 7.60 (7.37–7.84) | 7.53 (7.23–7.84) | 7.66 (7.39–7.93) | 7.94 (7.62–8.27) | 8.08 (7.90–8.26) | 8.02 (7.73–8.30) | 0.025 | 0.815 |
| NH black | 7.27 (6.89–7.66) | 7.54 (7.06–8.02) | 7.52 (7.05–8.00) | 7.17 (6.86–7.48) | 7.68 (7.38–7.98) | 7.48 (7.15–7.81) | 7.54 (7.17–7.91) | 0.353 | |
| Mexican American | 7.13 (6.82–7.44) | 7.02 (6.74–7.29) | 7.22 (7.01–7.44) | 7.18 (6.83–7.54) | 7.75 (7.44–8.06) | 7.49 (7.04–7.94) | 7.51 (6.91–8.11) | 0.018 | |
| P race effect | 0.036 | 0.012 | 0.421 | 0.146 | 0.532 | <0.001 | 0.074 | ||
| Women | |||||||||
| NH white | 8.18 (7.78–8.58) | 8.28 (8.11–8.46) | 8.14 (7.88–8.40) | 8.23 (7.89–8.58) | 8.53 (8.22–8.84) | 8.51 (8.25–8.77) | 8.39 (8.08–8.70) | 0.082 | 0.547 |
| NH black | 7.26 (6.96–7.56) | 7.44 (6.99–7.88) | 7.27 (6.96–7.58) | 7.44 (7.08–7.79) | 7.38 (7.10–7.65) | 7.48 (7.12–7.84) | 7.47 (7.09–7.84) | 0.397 | |
| Mexican American | 7.54 (7.11–7.97) | 7.77 (7.52–8.02) | 7.25 (6.99–7.51) | 7.91 (7.63–8.19) | 7.70 (7.15–8.26) | 7.66 (7.39–7.93) | 7.68 (7.36–8.00) | 0.480 | |
| P race effect | 0.002 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | 0.005 | ||
CI indicates confidence interval; NH, non‐Hispanic; NHANES, National Health and Nutrition Examination Surveys.
Black women had significantly lower mean CVH scores as compared with NH white women at each survey cycle (difference=0.93; P=0.001 in 2011/2012), and Mexican‐American women had significantly lower mean score as compared with NH white women at almost all survey cycles (difference=0.71; P=0.02 in 2011/2012). Differences between race/ethnicity categories were smaller for men and were mostly nonsignificant.
There were significant negative secular trends in BMI and fasting glucose scores among both women and men across race/ethnicities during the study period, indicating the rising prevalence of overweight/obesity and diabetes mellitus (Figures 2 and 3; Tables 4 and 5). Among men, there was little evidence of significant differences in BMI score by race/ethnicity; however, glucose scores were significantly worse in Mexican‐American men as compared with both NH white and NH black men. Among women, NH whites had significantly better BMI and glucose scores as compared with NH blacks and Mexican Americans at each survey cycle.
Figure 2.
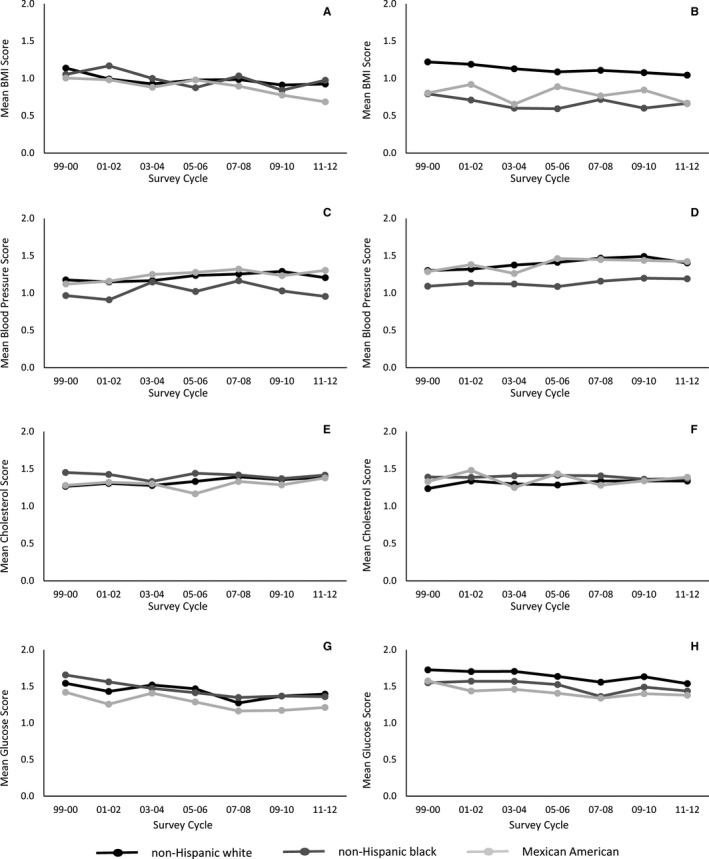
Trends in age‐adjusted means of cardiovascular health factors by sex and race/ethnicity, National Health and Nutrition Examination Surveys 1999–2012. A, Body mass index—men; B, Body mass index—women. C, Blood pressure—men. D, Blood pressure—women. E, Total cholesterol—men. F, Total cholesterol—women. G, Fasting blood glucose—men. H, Fasting blood glucose—women.
Figure 3.
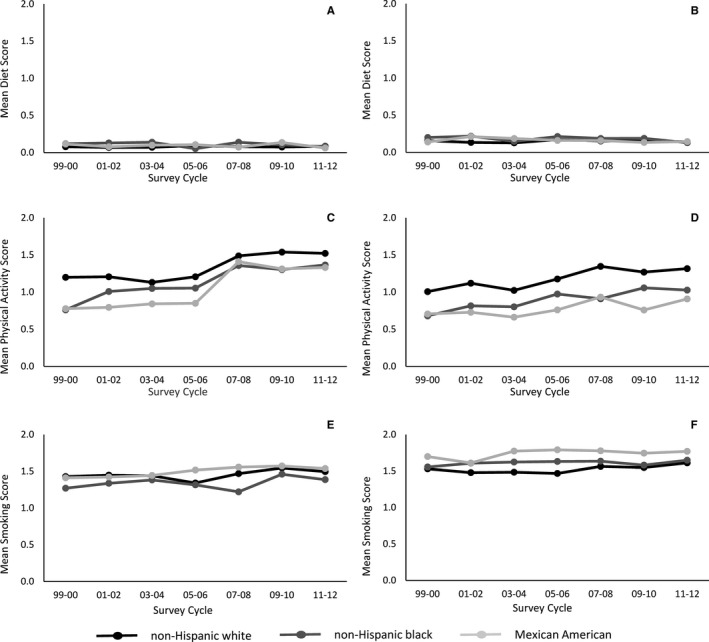
Trends in age‐adjusted means of cardiovascular health behaviors by sex and race/ethnicity, National Health and Nutrition Examination Surveys 1999–2012. A, Healthy diet index—men. B, Healthy diet index—women. C, Physical activity—men. D, Physical activity—women. E, Smoking—men. F, Smoking—women.
Table 4.
Age‐Adjusted Mean Score for Each Cardiovascular Health Factor/Behavior for US Men Aged ≥20 Years by Race/Ethnicity and NHANES Survey Cycle
| Age‐Adjusted Mean Score (95% CI) by NHANES Survey Cycle | P linear trend | P interaction | |||||||
|---|---|---|---|---|---|---|---|---|---|
| 1999–2000 | 2001–2002 | 2003–2004 | 2005–2006 | 2007–2008 | 2009–2010 | 2011–2012 | |||
| Body mass index | |||||||||
| NH white | 1.14 (1.06–1.21) | 0.99 (0.94–1.05) | 0.93 (0.85–1.00) | 0.98 (0.91–1.05) | 0.98 (0.91–1.06) | 0.91 (0.81–1.02) | 0.93 (0.87–0.98) | <0.001 | 0.199 |
| NH black | 1.05 (0.93–1.17) | 1.17 (1.05–1.29) | 1.00 (0.89–1.11) | 0.88 (0.73–1.03) | 1.03 (0.90–1.16) | 0.84 (0.67–1.02) | 0.98 (0.85–1.10) | 0.021 | |
| Mexican American | 1.01 (0.86–1.15) | 0.98 (0.89–1.07) | 0.88 (0.77–0.99) | 0.98 (0.82–1.13) | 0.90 (0.79–1.01) | 0.78 (0.66–0.89) | 0.69 (0.48–0.89) | 0.005 | |
| P race effect | 0.245 | 0.031 | 0.364 | 0.293 | 0.451 | 0.355 | 0.042 | ||
| Blood pressure | |||||||||
| NH white | 1.17 (1.10–1.25) | 1.15 (1.06–1.23) | 1.17 (1.07–1.26) | 1.24 (1.18–1.29) | 1.25 (1.20–1.31) | 1.29 (1.21–1.36) | 1.20 (1.14–1.27) | 0.034 | 0.923 |
| NH black | 0.96 (0.83–1.1) | 0.91 (0.76–1.06) | 1.15 (0.99–1.30) | 1.02 (0.89–1.15) | 1.16 (1.07–1.25) | 1.03 (0.95–1.11) | 0.96 (0.82–1.09) | 0.565 | |
| Mexican American | 1.12 (1.03–1.21) | 1.16 (1.02–1.30) | 1.25 (1.1–1.40) | 1.28 (1.19–1.36) | 1.32 (1.21–1.43) | 1.23 (1.14–1.32) | 1.30 (1.14–1.47) | 0.105 | |
| P race effect | 0.028 | 0.008 | 0.550 | 0.012 | 0.061 | <0.001 | 0.003 | ||
| Total cholesterol | |||||||||
| NH white | 1.27 (1.17–1.36) | 1.31 (1.22–1.39) | 1.28 (1.21–1.34) | 1.33 (1.28–1.39) | 1.39 (1.33–1.46) | 1.35 (1.29–1.42) | 1.39 (1.32–1.46) | 0.006 | 0.148 |
| NH black | 1.45 (1.33–1.57) | 1.43 (1.31–1.54) | 1.33 (1.22–1.44) | 1.44 (1.36–1.52) | 1.42 (1.32–1.52) | 1.37 (1.28–1.46) | 1.42 (1.32–1.52) | 0.988 | |
| Mexican American | 1.28 (1.23–1.33) | 1.32 (1.17–1.47) | 1.30 (1.17–1.43) | 1.17 (1.05–1.29) | 1.33 (1.23–1.44) | 1.29 (1.20–1.37) | 1.38 (1.28–1.48) | 0.759 | |
| P race effect | 0.010 | 0.173 | 0.684 | 0.001 | 0.086 | 0.574 | 0.630 | ||
| Fasting glucose | |||||||||
| NH white | 1.54 (1.46–1.63) | 1.43 (1.38–1.48) | 1.52 (1.45–1.59) | 1.47 (1.39–1.55) | 1.27 (1.20–1.34) | 1.37 (1.30–1.43) | 1.39 (1.33–1.46) | <0.001 | 0.087 |
| NH black | 1.66 (1.58–1.73) | 1.56 (1.44–1.69) | 1.47 (1.38–1.57) | 1.41 (1.32–1.51) | 1.35 (1.20–1.5) | 1.37 (1.24–1.50) | 1.36 (1.20–1.52) | <0.001 | |
| Mexican American | 1.42 (1.34–1.5) | 1.26 (1.20–1.32) | 1.41 (1.31–1.51) | 1.29 (1.14–1.43) | 1.16 (1.10–1.22) | 1.17 (1.10–1.25) | 1.21 (1.04–1.38) | <0.001 | |
| P race effect | <0.001 | 0.002 | 0.159 | 0.070 | 0.011 | <0.001 | 0.362 | ||
| Healthy diet index | |||||||||
| NH white | 0.08 (0.04–0.12) | 0.07 (0.04–0.09) | 0.07 (0.04–0.1) | 0.09 (0.06–0.13) | 0.08 (0.05–0.10) | 0.08 (0.05–0.10) | 0.09 (0.05–0.12) | 0.716 | 0.308 |
| NH black | 0.12 (0.01–0.22) | 0.13 (0.05–0.21) | 0.14 (0.05–0.23) | 0.05 (0.02–0.08) | 0.14 (0.08–0.20) | 0.11 (0.05–0.16) | 0.08 (0.03–0.13) | 0.392 | |
| Mexican American | 0.12 (0.09–0.15) | 0.08 (0.05–0.11) | 0.10 (0.07–0.13) | 0.11 (0.06–0.16) | 0.07 (0.04–0.11) | 0.14 (0.08–0.19) | 0.06 (0.03–0.1) | 0.458 | |
| P race effect | 0.248 | 0.330 | 0.227 | 0.004 | 0.006 | 0.207 | 0.553 | ||
| Physical activity | |||||||||
| NH white | 1.20 (1.10–1.30) | 1.21 (1.08–1.34) | 1.13 (1.05–1.21) | 1.21 (1.09–1.32) | 1.49 (1.39–1.58) | 1.54 (1.47–1.60) | 1.52 (1.42–1.63) | <0.001 | 0.005 |
| NH black | 0.76 (0.64–0.88) | 1.01 (0.86–1.16) | 1.05 (0.88–1.22) | 1.05 (0.91–1.20) | 1.36 (1.26–1.46) | 1.30 (1.24–1.36) | 1.37 (1.29–1.45) | <0.001 | |
| Mexican American | 0.78 (0.61–0.94) | 0.8 (0.71–0.88) | 0.84 (0.68–1.01) | 0.85 (0.71–0.99) | 1.41 (1.25–1.57) | 1.31 (1.21–1.41) | 1.33 (1.15–1.51) | <0.001 | |
| P race effect | <0.001 | <0.001 | <0.001 | 0.003 | 0.059 | <0.001 | 0.031 | ||
| Smoking | |||||||||
| NH white | 1.43 (1.29–1.57) | 1.45 (1.36–1.54) | 1.44 (1.34–1.54) | 1.34 (1.21–1.47) | 1.47 (1.37–1.57) | 1.55 (1.48–1.61) | 1.50 (1.38–1.61) | 0.230 | 0.268 |
| NH black | 1.27 (1.09–1.45) | 1.34 (1.13–1.55) | 1.38 (1.18–1.59) | 1.32 (1.19–1.44) | 1.22 (1.1–1.34) | 1.46 (1.38–1.54) | 1.39 (1.29–1.49) | 0.433 | |
| Mexican American | 1.41 (1.26–1.56) | 1.42 (1.31–1.54) | 1.44 (1.32–1.57) | 1.52 (1.38–1.65) | 1.56 (1.41–1.7) | 1.57 (1.49–1.66) | 1.54 (1.38–1.7) | 0.007 | |
| P race effect | 0.369 | 0.356 | 0.725 | 0.131 | 0.001 | 0.274 | 0.093 | ||
CI indicates confidence interval; NH, non‐Hispanic; NHANES, National Health and Nutrition Examination Surveys.
Table 5.
Age‐Adjusted Mean Score by Cardiovascular Health CVH Factor/Behavior for US Women Aged ≥20 Years by Race/Ethnicity and NHANES Survey Cycle
| Age‐Adjusted Mean Score (95% CI) by NHANES Survey Cycle | P linear trend | P interaction | |||||||
|---|---|---|---|---|---|---|---|---|---|
| 1999–2000 | 2001–2002 | 2003–2004 | 2005–2006 | 2007–2008 | 2009–2010 | 2011–2012 | |||
| Body mass index | |||||||||
| NH white | 1.22 (1.07–1.37) | 1.19 (1.10–1.28) | 1.13 (1.01–1.25) | 1.09 (0.99–1.19) | 1.11 (1.02–1.20) | 1.08 (1.01–1.15) | 1.04 (0.91–1.17) | 0.027 | 0.254 |
| NH black | 0.79 (0.66–0.93) | 0.71 (0.59–0.83) | 0.60 (0.52–0.68) | 0.59 (0.44–0.75) | 0.72 (0.59–0.84) | 0.60 (0.48–0.72) | 0.66 (0.56–0.77) | 0.120 | |
| Mexican American | 0.81 (0.62–0.99) | 0.92 (0.76–1.08) | 0.65 (0.55–0.76) | 0.89 (0.80–0.98) | 0.77 (0.63–0.90) | 0.84 (0.78–0.90) | 0.67 (0.53–0.81) | 0.470 | |
| P race effect | 0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | ||
| Blood pressure | |||||||||
| NH white | 1.30 (1.25–1.35) | 1.32 (1.27–1.37) | 1.37 (1.32–1.43) | 1.41 (1.35–1.47) | 1.47 (1.42–1.52) | 1.49 (1.43–1.55) | 1.40 (1.34–1.46) | <0.001 | 0.161 |
| NH black | 1.09 (1.01–1.18) | 1.13 (1.04–1.22) | 1.12 (0.96–1.28) | 1.09 (0.93–1.24) | 1.16 (1.02–1.30) | 1.20 (1.10–1.29) | 1.19 (1.10–1.28) | 0.086 | |
| Mexican American | 1.29 (1.21–1.37) | 1.38 (1.29–1.47) | 1.26 (1.13–1.39) | 1.46 (1.32–1.61) | 1.45 (1.37–1.52) | 1.44 (1.39–1.49) | 1.42 (1.30–1.54) | 0.162 | |
| P race effect | 0.001 | 0.006 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | ||
| Total cholesterol | |||||||||
| NH white | 1.24 (1.19–1.28) | 1.34 (1.26–1.41) | 1.30 (1.26–1.34) | 1.28 (1.21–1.36) | 1.34 (1.29–1.38) | 1.34 (1.25–1.43) | 1.34 (1.29–1.39) | 0.1154 | 0.077 |
| NH black | 1.39 (1.29–1.49) | 1.39 (1.28–1.50) | 1.41 (1.31–1.50) | 1.41 (1.34–1.48) | 1.41 (1.32–1.50) | 1.36 (1.26–1.47) | 1.37 (1.26–1.48) | 0.5397 | |
| Mexican American | 1.33 (1.27–1.39) | 1.48 (1.34–1.63) | 1.25 (1.15–1.35) | 1.44 (1.34–1.53) | 1.28 (1.20–1.36) | 1.34 (1.25–1.43) | 1.39 (1.27–1.51) | 0.5397 | |
| P race effect | <0.001 | 0.097 | 0.041 | 0.021 | 0.296 | 0.821 | 0.354 | ||
| Fasting glucose | |||||||||
| NH white | 1.73 (1.68–1.78) | 1.70 (1.66–1.75) | 1.71 (1.64–1.78) | 1.64 (1.57–1.71) | 1.56 (1.49–1.63) | 1.63 (1.56–1.71) | 1.54 (1.50–1.57) | <0.001 | 0.615 |
| NH black | 1.55 (1.44–1.66) | 1.57 (1.48–1.66) | 1.57 (1.50–1.64) | 1.53 (1.44–1.61) | 1.36 (1.28–1.45) | 1.49 (1.41–1.57) | 1.44 (1.35–1.52) | 0.005 | |
| Mexican American | 1.58 (1.46–1.69) | 1.44 (1.34–1.53) | 1.46 (1.25–1.67) | 1.41 (1.27–1.54) | 1.34 (1.22–1.45) | 1.40 (1.30–1.50) | 1.38 (1.22–1.54) | 0.050 | |
| P race effect | 0.003 | <0.001 | 0.003 | 0.002 | 0.001 | 0.005 | 0.062 | ||
| Healthy diet index | |||||||||
| NH white | 0.16 (0.11–0.21) | 0.13 (0.10–0.17) | 0.13 (0.08–0.18) | 0.17 (0.13–0.22) | 0.15 (0.12–0.19) | 0.15 (0.12–0.18) | 0.14 (0.10–0.19) | 0.823 | 0.479 |
| NH black | 0.20 (0.10–0.30) | 0.22 (0.14–0.3) | 0.15 (0.08–0.21) | 0.21 (0.16–0.26) | 0.19 (0.12–0.25) | 0.19 (0.12–0.26) | 0.13 (0.09–0.17) | 0.450 | |
| Mexican American | 0.14 (0.10–0.18) | 0.21 (0.19–0.24) | 0.19 (0.10–0.27) | 0.16 (0.12–0.20) | 0.16 (0.11–0.21) | 0.13 (0.07–0.20) | 0.15 (0.06–0.23) | 0.657 | |
| P race effect | 0.552 | 0.009 | 0.591 | 0.289 | 0.508 | 0.389 | 0.948 | ||
| Physical activity | |||||||||
| NH white | 1.01 (0.85–1.16) | 1.12 (1.00–1.24) | 1.02 (0.94–1.11) | 1.18 (1.05–1.30) | 1.35 (1.22–1.47) | 1.27 (1.20–1.34) | 1.32 (1.23–1.40) | <0.001 | 0.711 |
| NH black | 0.68 (0.57–0.79) | 0.82 (0.62–1.01) | 0.80 (0.66–0.94) | 0.97 (0.85–1.10) | 0.91 (0.76–1.06) | 1.06 (0.91–1.20) | 1.03 (0.88–1.18) | <0.001 | |
| Mexican American | 0.71 (0.60–0.81) | 0.73 (0.57–0.88) | 0.66 (0.54–0.79) | 0.76 (0.60–0.92) | 0.93 (0.63–1.24) | 0.76 (0.67–0.85) | 0.91 (0.68–1.14) | 0.025 | |
| P race effect | 0.002 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | ||
| Smoking | |||||||||
| NH white | 1.53 (1.4–1.66) | 1.48 (1.38–1.57) | 1.48 (1.4–1.56) | 1.47 (1.35–1.59) | 1.56 (1.48–1.65) | 1.55 (1.46–1.64) | 1.61 (1.53–1.7) | 0.067 | 0.449 |
| NH black | 1.55 (1.41–1.70) | 1.61 (1.49–1.73) | 1.62 (1.52–1.72) | 1.63 (1.47–1.79) | 1.63 (1.51–1.76) | 1.58 (1.42–1.74) | 1.65 (1.53–1.76) | 0.637 | |
| Mexican American | 1.70 (1.56–1.83) | 1.61 (1.49–1.73) | 1.77 (1.7–1.85) | 1.79 (1.72–1.86) | 1.78 (1.62–1.94) | 1.74 (1.66–1.82) | 1.77 (1.59–1.94) | 0.182 | |
| P race effect | <0.001 | 0.140 | <0.001 | <0.001 | 0.024 | 0.011 | 0.637 | ||
CI indicates confidence interval; NH, non‐Hispanic; NHANES, National Health and Nutrition Examination Surveys.
There were significant positive secular trends in physical activity for both women and men across race/ethnicities during the study period. Among men, the rate of increase was higher for NH blacks and Mexican Americans (P interaction=0.005); the differing rates narrowed, but did not eliminate, significant gaps in physical activity scores between NH white men and both NH black and Mexican‐American men (P=0.031 in 2011/2012). Women experienced similar rates of increase across race/ethnicities, continuing trends where NH white women had better physical activity scores as compared with NH black and Mexican‐American women.
Small and mostly nonsignificant increases occurred in blood pressure, cholesterol, and smoking scores for both women and men across race/ethnicities during the study period. Among both men and women, NH blacks had significantly worse blood pressure scores at each survey cycle as compared with NH whites and Mexican Americans, who had similar blood pressure scores. Persistent significant differences across race/ethnicity groups for cholesterol scores were not observed for men or women. Little difference in smoking scores by race/ethnicity was observed among men at each survey cycle, whereas Mexican‐American women had better smoking scores as compared with NH white and NH black women.
Few Americans met the AHA guidelines for ideal diet in any of the survey cycles, and thus healthy diet index scores had little change over survey cycles nor were there significant differences between race/ethnicity groups.
In sensitivity analyses that further stratified the analyses by income and educational attainment, socioeconomic status did not fully account for the significant differences in CVH among women and disparities tended to be more pronounced at higher levels of socioeconomic status (Figures 4 and 5).
Figure 4.
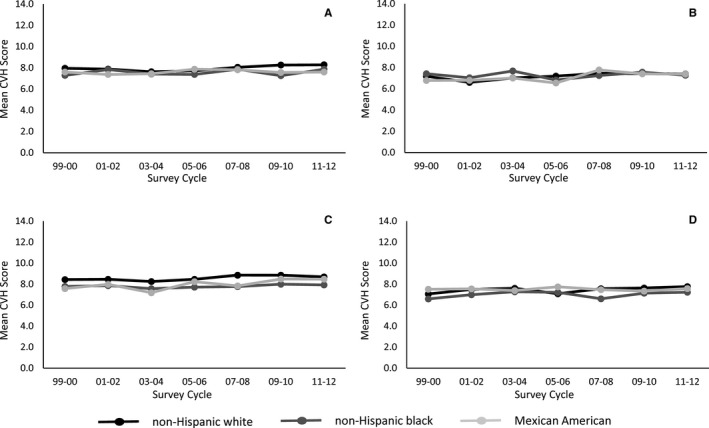
Trends in age‐adjusted mean cardiovascular health score for US adults aged ≥20 years by sex, race/ethnicity, and income level, National Health and Nutrition Examination Surveys 1999–2012. A, Higher income—men. B, Lower income—men. C, Higher income—women. D, Lower income—women. Lower income defined as household income <185% of the US federal poverty level adjusted for household size; higher income defined as household income ≥185% of the US federal poverty level adjusted for household size. CVH indicates cardiovascular health.
Figure 5.
Trends in age‐adjusted mean cardiovascular health score for US adults aged ≥20 years by sex, race/ethnicity, and educational attainment, National Health and Nutrition Examination Surveys 1999–2012. A, Higher education—men. B, Lower education—men. C, Higher education—women. D, Lower education—women. Lower education defined as high school diploma or less educational attainment; higher education defined as least some college education. CVH indicates cardiovascular health.
Discussion
We observed that, despite greater public health focus on reducing racial/ethnic disparities, there has been little change in overall CVH scores from 1999/2000 through 2011/2012. As a result, racial/ethnic differences in CVH have persisted over the past decade and there is little evidence of narrowing disparities. Racial/ethnic disparities were generally larger among women.
There were also racial/ethnic differences within individual CVH factors and behaviors. Among men, there were significant differences in physical activity, blood pressure, and fasting glucose across race/ethnicity groups. Among women, there were significant differences in BMI, fasting glucose, physical activity, blood pressure, and smoking, in addition to overall CVH. Although there was change over time within the specific factors and behaviors, there were almost no significant differences in this change over time by race/ethnicity, thus disparities within these factors and behaviors persisted over time.
Previous studies also have noted cross‐sectional differences in CVH by race/ethnicity with NH whites having higher mean number of ideal health factors and behaviors compared with NH blacks and Hispanics in aggregate.10, 11, 12, 14 One article looking at US trends over time in mean number of ideal factors and behaviors by racial/ethnic category showed persistent gaps between NH whites and both NH blacks and Hispanics.12 Our study adds to the understanding of CVH trends over time by presenting racial/ethnic differences by sex, and by examining the full spectrum of CVH, utilizing the 14 point CVH score that assesses ideal, intermediate, and poor CVH. We found significant differences between racial/ethnic groups among women only.
For most of the differences observed in this study, NH whites had higher scores than NH blacks or Mexican Americans. Historical policies of social exclusion as well as documented discrimination in access to health‐enhancing resources experienced by racial/ethnic minority groups in the United States are likely contributors to racial/ethnic differences in CVH.16, 17, 18 For example, neighborhoods with a higher percentage of racial/ethnic minority residents—regardless of income—have fewer grocery stores,19 fewer recreation facilities,20 and less walkability21; these neighborhood resources have been linked to preservation of ideal CVH.22 Previous research has shown that individuals who have multiple forms of social disadvantage—such as low income, low education, and nonwhite race—are even less likely to have ideal CVH.11 In our study, the racial/ethnic disparities in CVH factors and behaviors were not fully explained by differing distributions of income and education across race/ethnicities. Factors beyond socioeconomic status may contribute to these disparities.
Yet, there were CVH differences that did not fit this pattern. For example, there were significantly higher smoking scores (ie, fewer smokers) among Mexican‐American women. Indeed, the lower rates of CVD mortality among Hispanics as compared with NH whites—known as the Hispanic Paradox—are contrary to the generally higher risk factor burden and CVD incidence among Hispanics.3 It has been posited that cultural context may contribute to this particular CVH resiliency, despite disparate access to some health resources.23 However, US Hispanics are an aggregated ethnicity from multiple heritage backgrounds, and risk factor patterning may be different among Hispanic subgroups. For example, a previous study found similarly low levels of smoking among Mexican‐American women, but much higher levels of smoking in Puerto Rican and Cuban women.4 Our findings are generalizable only to Mexican Americans.
A strength of this study is the use of NHANES, a US nationally representative survey that was conducted at regular intervals during the study period. Each of the factors/behaviors was measured using detailed assessments that allow for analysis according to AHA criteria for ideal, intermediate, and poor levels of CVH. Because the NHANES measures correspond to the AHA criteria, we were able to use the full 14‐point CVH scale and analyze scores as continuous variables. This allowed for identification of linear trends as well as isolation of smaller differences between racial/ethnic and sex subpopulations.
Despite these strengths, there were several limitations. We included participants from the fasting subsample, who were the only NHANES participants who had a fasting glucose measurement. This subsample is designed to be nationally representative, but does include fewer NHANES participants. For our analysis sample, we excluded participants who had missing data for any of the 7 factors and behaviors included in the CVH score, around 11% of the fasting subsample. As shown in Table 6, the demographic composition without exclusion for missing risk factor data is nearly identical to the analysis sample (Table 2). Furthermore, because of the NHANES sampling strategy, we were unable to include persons who reported any race or ethnicity other than NH black, NH white, or Mexican American. There is evidence of disparities in levels of CVH for other racial/ethnic groups in the United States,10, 12 and characterization and evaluation of CVH trends is equally important for those subpopulations. Additionally, in sensitivity analyses, we stratified by income and educational attainment. Because of sample‐size issues, it was not possible to calculate estimates for more‐precise educational categories for each race‐sex group, and thus we may miss nuances in educational differences between racial/ethnic groups. Because of differing age distributions by race/ethnicity, we age‐adjusted our estimates using the US population in 2000. Smaller sample sizes coupled with age adjustment may have led to some sampling variability in estimates over time. Therefore, we focused on long‐term, linear trends over the study period. Our results were less robust for small changes within the study period, such as dietary shifts that occurred during the Great Recession of 2007–2009.24 Last, the scores for the 3 heath behaviors—smoking, diet, and physical activity—were self‐reported and thus potentially disposed to misclassification.
Table 6.
Demographic Characteristics of the NHANES Fasting Subsample 1999–2012, Including Missing Risk Factor Data (N=12 696)
| Characteristic* | Total No. (Percent) of Missing Data | Non‐Hispanic White Mean or Percentage (95% CI) | Non‐Hispanic Black Mean or Percentage (95% CI) | Mexican American Mean or Percentage (95% CI) | |||
|---|---|---|---|---|---|---|---|
| Men (n=3592) | Women (n=3487) | Men (n=1351) | Women (n=1488) | Men (n=1422) | Women (n=1356) | ||
| Age group, y, % | |||||||
| 20 to 34 | Missing=0 (0%) | 25.7 (23.8–27.5) | 21.9 (20.3–23.5) | 35.3 (32.1–38.4) | 30.3 (27.6–32.9) | 47.1 (43.6–50.5) | 40.1 (36.2–44.0) |
| 35 to 49 | 31.6 (29.6–33.6) | 29.8 (27.7–31.9) | 32.1 (28.9–35.2) | 34.7 (31.9–37.5) | 32.6 (29.8–35.4) | 32.9 (29.5–36.3) | |
| 50 to 64 | 25.6 (23.6–27.5) | 26.7 (25–28.5) | 22.3 (20.1–24.6) | 22.3 (20.2–24.4) | 14.4 (12.5–16.3) | 18.0 (15.7–20.3) | |
| 65+ | 17.2 (16–18.4) | 21.6 (20.2–23) | 10.3 (8.8–11.8) | 12.7 (11.1–14.3) | 5.9 (4.9–6.9) | 9.0 (7.3–10.6) | |
| Age, y, M | Missing=0 (0%) | 47.3 (46.6–48) | 49.6 (48.9–50.3) | 42.9 (42–43.8) | 44.7 (43.8–45.7) | 38.3 (37.4–39.3) | 41.3 (40.2–42.4) |
| Country of birth | Missing=5 (<0.1%) | ||||||
| US born | 95.1 (93.9–96.3) | 95.8 (94.9–96.7) | 88.4 (85.7–91.2) | 91.4 (88.5–94.3) | 36.8 (32.1–41.5) | 42.5 (38.6–46.5) | |
| Foreign born | 4.9 (3.7–6.1) | 4.2 (3.3–5.1) | 11.6 (8.8–14.3) | 8.6 (5.7–11.5) | 63.2 (58.5–67.9) | 57.5 (53.5–61.4) | |
| Education | Missing=18 (0.1%) | ||||||
| ≤High school | 38.9 (35.9–41.8) | 38.6 (35.9–41.4) | 56.5 (53.4–59.7) | 47.1 (44–50.1) | 75.4 (72.1–78.7) | 69.8 (66.3–73.3) | |
| ≥Some college | 61.1 (58.2–64.1) | 61.4 (58.6–64.1) | 43.5 (40.3–46.6) | 52.9 (49.9–56) | 24.6 (21.3–27.9) | 30.2 (26.7–33.7) | |
| Income† | Missing=922 (7.3%) | ||||||
| Lower income | 22.2 (19.6–24.8) | 27.3 (24.7–29.8) | 43.1 (39.9–46.4) | 51.0 (47.6–54.3) | 57.4 (53.6–61.2) | 61.4 (57–65.8) | |
| Higher income | 77.8 (75.2–80.4) | 72.7 (70.2–75.3) | 56.9 (53.6–60.1) | 49.0 (45.7–52.4) | 42.6 (38.8–46.4) | 38.6 (34.2–43.0) | |
| Body mass index, M | Missing=219 (1.7%) | 28.5 (28.2–28.7) | 28.0 (27.7–28.3) | 28.5 (28.0–28.9) | 32.0 (31.5–32.4) | 28.6 (28.1–29.0) | 29.7 (29.2–30.1) |
| Systolic blood pressure, M | Missing=451 (3.6%) | 122.5 (121.9–123.1) | 119.7 (119.0–120.4) | 126.5 (125.3–127.6) | 124.0 (122.7–125.3) | 120.5 (119.6–121.5) | 116.6 (115.3–118) |
| Diastolic blood pressure, M | Missing=451 (3.6%) | 71.7 (71.1–72.2) | 68.6 (68–69.2) | 73.5 (72.7–74.4) | 70.8 (69.9–71.7) | 70.7 (69.6–71.7) | 67.8 (67–68.6) |
| Total cholesterol, M | Missing=144 (1.1%) | 195.3 (193.6–197) | 202.9 (201.4–204.5) | 190.5 (188.2–192.9) | 192.9 (190.6–195.2) | 198.2 (195.8–200.6) | 192.6 (189.7–195.4) |
| Fasting blood glucose, M | Missing=21 (0.2%) | 105.2 (104.1–106.2) | 99.4 (98.5–100.4) | 104.9 (102.5–107.2) | 104.3 (102–106.6) | 109.6 (107.3–112) | 106.0 (103.4–108.6) |
| Taking BP‐lowering medication, % | Missing=0 (0%) | 23.0 (21.0–25.0) | 24.2 (22.2–26.2) | 22.2 (19.7–24.6) | 33.9 (30.8–37) | 9.8 (7.8–11.9) | 13.2 (10.8–15.6) |
| Taking lipid‐lowering medication, % | Missing=0 (0%) | 17.2 (15.7–18.7) | 15.5 (13.8–17.1) | 12.1 (10.1–14.1) | 12.7 (11–14.5) | 7.5 (5.9–9.1) | 9.7 (7.7–11.7) |
| Taking diabetes mellitus medication, % | Missing=0 (0%) | 5.3 (4.4–6.2) | 4.0 (3.3–4.7) | 6.3 (5–7.7) | 9.0 (7.4–10.5) | 5.7 (4.4–7) | 6.6 (5.1–8.1) |
| Current smoker, % | Missing=0 (0%) | 25.4 (23.4–27.5) | 20.7 (19–22.4) | 32.6 (29.8–35.5) | 19.2 (16.7–21.8) | 24.5 (21.8–27.2) | 11.6 (9.5–13.8) |
| Previously had CVD event, %‡ | Missing=0 (0%) | 10.2 (9.2–11.3) | 7.2 (6.2–8.1) | 7.4 (6.1–8.7) | 8.3 (6.9–9.7) | 3.7 (2.9–4.6) | 3.9 (2.7–5.1) |
BP indicates blood pressure; CI, confidence interval; CVD, cardiovascular disease; NHANES, National Health and Nutrition Examination Surveys.
*Sample sizes are unweighted numbers of each race/ethnicity and sex category; percentages are weighted to reflect NHANES complex, multistage survey sampling.
Lower income defined as household income <185% of the US federal poverty level adjusted for household size; higher income defined as household income ≥185% of the US federal poverty level adjusted for household size.
Previous CVD events include self‐reported congestive heart failure, coronary heart disease, heart attack, and stroke.
In summary, we found enduring disparities in overall CVH for NH black and Mexican‐American women as compared with NH white women. The nearly 1‐point difference in CVH score would be expected to translate into disparities in incident CVD in the future. Each 1 point greater on the 14‐point CVH scale has been associated with 18% lower risk of developing stroke or myocardial infarction in a multiracial sample.25 As previous studies have noted, if CVH trends continue without rapid improvement, prevention goals will go unmet.15, 26 Likewise, if the racial/ethnic trends in CVH persist, goals to eliminate health disparities will also go unmet. Efforts to eliminate cardiovascular disparities must include community‐based primordial prevention aimed specifically at minority women. Multifaceted approaches to prevention that acknowledge and integrate both community and healthcare interventions using culturally tailored approaches may have more success in reducing disparities.27
Sources of Funding
This study was supported, in part, by a grant from the American Heart Association (15SFDRN25080331).
Disclosures
None.
Acknowledgments
All data used in this study were collected by the National Center for Health Statistics, Centers for Disease Control and Prevention. The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
(J Am Heart Assoc. 2017;6:e006027 DOI: 10.1161/JAHA.117.006027.)28939713
References
- 1. Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, Das SR, de Ferranti S, Després JP, Fullerton HJ, Howard VJ, Huffman MD, Isasi CR, Jiménez MC, Judd SE, Kissela BM, Lichtman JH, Lisabeth LD, Liu S, Mackey RH, Magid DJ, McGuire DK, Mohler ER III, Moy CS, Muntner P, Mussolino ME, Nasir K, Neumar RW, Nichol G, Palaniappan L, Pandey DK, Reeves MJ, Rodriguez CJ, Rosamond W, Sorlie PD, Stein J, Towfighi A, Turan TN, Virani SS, Woo D, Yeh RW, Turner MB; on behalf of the American Heart Association Statistics Committee and Stroke Statistics Subcommittee . Heart disease and stroke statistics—2016 update: a report from the American Heart Association. Circulation. 2016;133:e38–e60. [DOI] [PubMed] [Google Scholar]
- 2. Pearson‐Stuttard J, Guzman‐Castillo M, Penalvo JL, Rehm CD, Afshin A, Danaei G, Kypridemos C, Gaziano T, Mozaffarian D, Capewell S, O'Flaherty M. Modeling future cardiovascular disease mortality in the United States: national trends and racial and ethnic disparities. Circulation. 2016;133:967–978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Rodriguez CJ, Allison M, Daviglus ML, Isasi CR, Keller C, Leira EC, Palaniappan L, Piña IL, Ramirez SM, Rodriguez B, Sims M; on behalf of the American Heart Association Council on Epidemiology and Prevention; American Heart Association Council on Clinical Cardiology; and American Heart Association Council on Cardiovascular and Stroke Nursing . Status of cardiovascular disease and stroke in Hispanics/Latinos in the United States: a science advisory from the American Heart Association. Circulation. 2014;130:593–625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Daviglus ML, Talavera GA, Avilés‐Santa ML, Allison M, Cai J, Criqui MH, Gellman M, Giachello AL, Gouskova N, Kaplan RC, LaVange L, Penedo F, Perreira K, Pirzada A, Schneiderman N, Wassertheil‐Smoller S, Sorlie PD, Stamler J. Prevalence of major cardiovascular risk factors and cardiovascular diseases among Hispanic/Latino individuals of diverse backgrounds in the United States. JAMA. 2012;308:1775–1784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. US Department of Health and Human Services . Healthy People 2020: Improving the Health of Americans. Washington, DC: Government Printing Office; 2010. [Google Scholar]
- 6. Lloyd‐Jones DM, Hong Y, Labarthe D, Mozaffarian D, Appel LJ, Van Horn L, Greenlund K, Daniels S, Nichol G, Tomaselli GF, Arnett DK, Fonarow GC, Ho PM, Lauer MS, Masoudi FA, Robertson RM, Roger V, Schwamm LH, Sorlie P, Yancy CW, Rosamond WD; on behalf of the American Heart Association Strategic Planning Task Force and Statistics Committee . Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association's Strategic Impact Goal through 2020 and beyond. Circulation. 2010;121:586–613. [DOI] [PubMed] [Google Scholar]
- 7. Folsom AR, Yatsuya H, Nettleton JA, Lutsey PL, Cushman M, Rosamond WD; ARIC Study Investigators . Community prevalence of ideal cardiovascular health, by the American Heart Association definition, and relationship with cardiovascular disease incidence. J Am Coll Cardiol. 2011;57:1690–1696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Dong C, Rundek T, Wright CB, Anwar Z, Elkind MS, Sacco RL. Ideal cardiovascular health predicts lower risks of myocardial infarction, stroke, and vascular death across whites, blacks, and Hispanics: the northern Manhattan study. Circulation. 2012;125:2975–2984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Kulshreshtha A, Vaccarino V, Judd SE, Howard VJ, McClellan WM, Muntner P, Hong Y, Safford MM, Goyal A, Cushman M. Life's Simple 7 and risk of incident stroke: the reasons for geographic and racial differences in stroke study. Stroke. 2013;44:1909–1914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Pilkerton CS, Singh SS, Bias TK, Frisbee SJ. Changes in cardiovascular health in the United States, 2003–2011. J Am Heart Assoc. 2015;4:e001650. doi: 10.1161/JAHA.114.001650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Caleyachetty R, Echouffo‐Tcheugui JB, Muennig P, Zhu W, Muntner P, Shimbo D. Association between cumulative social risk and ideal cardiovascular health in US adults: NHANES 1999–2006. Int J Cardiol. 2015;191:296–300. [DOI] [PubMed] [Google Scholar]
- 12. Fang J, Yang Q, Hong Y, Loustalot F. Status of cardiovascular health among adult Americans in the 50 States and the District of Columbia, 2009. J Am Heart Assoc. 2012;1:e005371. doi: 10.1161/JAHA.112.005371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Britten P, Marcoe K, Yamini S, Davis C. Development of food intake patterns for the MyPyramid Food Guidance System. J Nutr Educ Behav. 2006;38:S78–S92. [DOI] [PubMed] [Google Scholar]
- 14. Shay CM, Ning H, Allen NB, Carnethon MR, Chiuve SE, Greenlund KJ, Daviglus ML, Lloyd‐Jones DM. Status of cardiovascular health in US adults: prevalence estimates from the National Health and Nutrition Examination Surveys (NHANES) 2003–2008. Circulation. 2012;125:45–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Huffman MD, Capewell S, Ning H, Shay CM, Ford ES, Lloyd‐Jones DM. Cardiovascular health behavior and health factor changes (1988–2008) and projections to 2020: results from the National Health and Nutrition Examination Surveys. Circulation. 2012;125:2595–2602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Braveman PA, Kumanyika S, Fielding J, Laveist T, Borrell LN, Manderscheid R, Troutman A. Health disparities and health equity: the issue is justice. Am J Public Health. 2011;101:S149–S155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Mensah GA, Mokdad AH, Ford ES, Greenlund KJ, Croft JB. State of disparities in cardiovascular health in the United States. Circulation. 2005;111:1233–1241. [DOI] [PubMed] [Google Scholar]
- 18. Kurian AK, Cardarelli KM. Racial and ethnic differences in cardiovascular disease risk factors: a systematic review. Ethn Dis. 2007;17:143–152. [PubMed] [Google Scholar]
- 19. Franco M, Diez‐Roux AV, Nettleton JA, Lazo M, Brancati F, Caballero B, Glass T, Moore LV. Availability of healthy foods and dietary patterns: the Multi‐Ethnic Study of Atherosclerosis. Am J Clin Nutr. 2009;89:897–904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Kelly CM, Schootman M, Baker EA, Barnidge EK, Lemes A. The association of sidewalk walkability and physical disorder with area‐level race and poverty. J Epidemiol Community Health. 2007;61:978–983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Moore LV, Diez Roux AV, Evenson KR, McGinn AP, Brines SJ. Availability of recreational resources in minority and low socioeconomic status areas. Am J Prev Med. 2008;34:16–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Unger E, Diez‐Roux AV, Lloyd‐Jones DM, Mujahid MS, Nettleton JA, Bertoni A, Badon SE, Ning H, Allen NB. Association of neighborhood characteristics with cardiovascular health in the Multi‐Ethnic Study of Atherosclerosis. Circ Cardiovasc Qual Outcomes. 2014;7:524–531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Gallo LC, Penedo FJ, Espinosa de los Monteros K, Arguelles W. Resiliency in the face of disadvantage: do Hispanic cultural characteristics protect health outcomes? J Pers. 2009;77:1707–1746. [DOI] [PubMed] [Google Scholar]
- 24. Ng SW, Slining MM, Popkin BM. Turning point for US diets? Recessionary effects or behavioral shifts in foods purchased and consumed. Am J Clin Nutr. 2014;99:609–616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Miao C, Bao M, Xing A, Chen S, Wu Y, Cai J, Chen Y, Yang X. Cardiovascular health score and the risk of cardiovascular diseases. PLoS One. 2015;10:e0131537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Huffman MD, Lloyd‐Jones DM, Ning H, Labarthe DR, Guzman Castillo M, O'Flaherty M, Ford ES, Capewell S. Quantifying options for reducing coronary heart disease mortality by 2020. Circulation. 2013;127:2477–2484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Havranek EP, Mujahid MS, Barr DA, Blair IV, Cohen MS, Cruz‐Flores S, Davey‐Smith G, Dennison‐Himmelfarb CR, Lauer MS, Lockwood DW, Rosal M, Yancy CW; on behalf of the American Heart Association Council on Quality of Care and Outcomes Research, Council on Epidemiology and Prevention, Council on Cardiovascular and Stroke Nursing, Council on Lifestyle and Cardiometabolic Health, and Stroke Council . Social determinants of risk and outcomes for cardiovascular disease: a scientific statement from the American Heart Association. Circulation. 2015;132:873–898. [DOI] [PubMed] [Google Scholar]


