Abstract
Background
Given high rates of obesity, hypertension, and diabetes mellitus, black persons are at risk to develop heart failure. The association of moderate to vigorous physical activity (MVPA) and heart failure in black adults is underresearched. The purpose of this study was to explore whether greater MVPA was associated with lower risk of heart failure hospitalizations (HFHs) among black adults with normal ejection fractions.
Methods and Results
We performed a prospective analysis of 4066 black adults who participated in the Jackson Heart Study and who had physical activity measured, had normal ejection fraction on 2‐dimensional echocardiograms, and were followed for 7 years for incident HFH. We used Cox proportional regression analyses adjusted for age, sex, body mass index, smoking status, hypertension, diabetes mellitus, chronic obstructive pulmonary disease, coronary heart disease, atrial fibrillation, and chronic kidney disease and examined effect modification by sex and body mass index. Of the eligible population, 1925 participants, according to the duration of MVPA, had poor health (0 minutes/week), 1332 had intermediate health (1–149 minutes/week), and 809 had ideal health (≥150 minutes/week). There were 168 incident HFHs. MVPA for intermediate and ideal health was associated with decreasing risk of incident HFH (hazard ratio: 0.70 [95% confidence interval, 49–1.00] and 0.35 [95% confidence interval, 0.19–0.64], respectively; P trend=0.003). The full model revealed hazard ratios of 0.74 [95% confidence interval, 0.52–1.07] and 0.41 [95% confidence interval, 0.22–0.74], respectively. There was no effect modification between MVPA and body mass index or sex on incident HFH.
Conclusions
A dose‐response relationship between increasing levels of MVPA and protection from incident HFH was found in black men and women with normal ejection fractions.
Keywords: epidemiology, exercise, heart failure, lifestyle, prevention
Subject Categories: Epidemiology, Exercise, Lifestyle
Clinical Perspective
What Is New?
Previous studies included only a small proportion of black adults and may have included participants with unrecognized left ventricular systolic dysfunction, a strong predictor of heart failure, and therefore been prone to confounding and reverse causation biases.
In this prospective analysis, a large cohort of community‐dwelling black adults with a broad age range and only preserved ejection fractions were studied. Increasing levels of moderate to vigorous physical activity were significantly associated with decreasing risk of incident heart failure hospitalization in a dose‐response fashion in this population.
What Are the Clinical Implications?
Given that black adults are at risk to develop heart failure due to a high prevalence of obesity, hypertension, and diabetes mellitus, encouragement of moderate to vigorous physical activity, in conjunction with careful management of comorbid conditions, should be considered for at‐risk black adults with normal ejection fractions.
Introduction
Approximately 5.1 million adults in the United States have heart failure (HF), which is associated with high morbidity and mortality.1 The economic burden of this disease imposed on the public is substantial, with an estimate total cost of $31 billion. It is predicted to increase to $70 billion by 2030.2 Especially for black adults, the majority of HF is HF with preserved ejection fraction (HFpEF), for which there is no effective treatment.3 Consequently, focusing on prevention is indicated. In contrast, asymptomatic left ventricular systolic dysfunction is associated with the development of HF with reduced ejection fraction, for which there is effective prevention and treatment with afterload reduction—angiotensin‐converting enzyme inhibitor, hydralazine, and nitrates.4
Physical activity is beneficial in preventing the development of many chronic diseases and may also improve control of these diseases if one were to have already acquired them. In patients with HF, exercise tolerance is limited. Nevertheless, exercise is still recommended because it improves exercise capacity and quality of life.5 Compared with the white population, physical activity may be more beneficial in the black population given the increased rate of disease,6 risk of earlier disease presentation,7 difference in response to physical activity,8 and lower levels of physical activity.9
Results from previous studies demonstrated that greater physical activity in middle‐aged and older participants was associated with reduced risk of HF.10, 11, 12, 13 These studies, however, incorporated only small proportions of black participants and may have included persons with unrecognized left ventricular systolic dysfunction, a strong predictor of HF, and therefore been prone to confounding and reverse causation biases. Our study included community‐dwelling black participants with a broad age range and only preserved ejection fractions—a population that has not been examined previously in such detail.
The association of moderate to vigorous physical activity (MVPA) with HF in black adults, an at‐risk population, is underresearched. The purpose of this study was to explore whether greater physical activity was associated with lower incidence of HF among black adults after accounting for age, sex, and other comorbidities in those with normal ejection fractions. The JHS (Jackson Heart Study) provides a large cohort of black participants and contains data to study HF incidence in this at‐risk population. We hypothesized that black adults who spent more time performing MVPA would have lower risk of HF compared with those who were sedentary.
Methods
Study Population
The JHS is an observational study of black participants from Hinds, Madison, and Rankin counties and Jackson, Mississippi. Because cardiovascular disease is prevalent among black adults, the primary focus of the JHS was to identify risk factors in this population and to seek ways to mitigate cardiovascular risk. The study design and the process of recruitment were described in detail elsewhere.14, 15 Briefly, the JHS cohort consisted of noninstitutionalized black adults aged 21 to 95 years at baseline. Between 2000 and 2004, 5301 participants were recruited. They completed questionnaires, physical examinations, and baseline echocardiographic and spirometric evaluations. We performed a prospective analysis to investigate the association of MVPA and HF hospitalizations (HFHs) among black adults. We excluded participants with a history of previous HFHs to define a disease‐free cohort for etiologic analysis. We also excluded participants who had missing MVPA data (n=5), covariate data (n=132), no follow‐up data to allow ascertainment of HF events (n=684), or reduced (<50%) or missing ejection fraction (n=414). Our analytic cohort comprised 4066 participants.
The JHS followed guidelines expressed by the Declaration of Helsinki, and all participants completed written informed consent. The institutional review boards at the participating institutions approved the study. The available data contained deidentified information.
Exposure
Physical activity
MVPA duration was obtained using the American Heart Association (AHA) Life's Simple 7 questionnaire.16 The categories of MVPA were defined by the US Department of Health and Human Services in 2008.17, 18 They have been used in studies as standards to define moderate and vigorous physical activity from metabolic equivalent data.9, 19 Participants were asked the question, “How much physical activity do you get in a week?” They were asked to provide the number of minutes of moderate and/or vigorous activity. Moderate‐intensity activity was defined as follows: “A person doing moderate‐intensity aerobic activity can usually talk, but not sing, during the activity.” Vigorous‐intensity activity was defined as follows: “A person doing vigorous‐intensity activity usually cannot say more than a few words without pausing for a breath.” Based on the number of minutes, MVPA was categorized into 3 groups: participants who performed 0 minutes of MVPA were classified as having poor health, those who performed 1 to 149 minutes were classified as having intermediate health, and those who performed ≥150 minutes were classified as having ideal health.
Outcome
Incident HFH
The primary outcome of interest in this study was incident HFH from January 1, 2005, to December 31, 2012. Trained interviewers conducted annual follow‐up telephone interviews to ascertain any significant health events since the last JHS contact, including diagnostic tests, hospitalizations, or death. HFH data were obtained from the annual follow‐up data and hospital discharge records from all catchment‐area hospitals. Data from non–catchment‐area hospitals were obtained after obtaining patient consent. HFH was adjudicated by trained medical personnel based on the relevant International Classification of Diseases, Ninth Revision, Clinical Modification codes. The self‐reported data from the annual follow‐up telephone interviews were reconciled with hospital discharge records.20, 21
Covariates
The following demographic, anthropometric, and disease variables were previously associated with HFpEF.22, 23 Baseline demographic characteristics included age and sex. Age was presented as a continuous variable, and self‐reported sex was presented as a binary variable. Body mass index (BMI) was based on weight and height obtained at the baseline visit and presented as a continuous variable. Smoking was derived based on self‐reported lifetime number of cigarettes smoked and current smoking status and categorized into 3 groups: never smoked, former smoker, and current smoker.
The presence of hypertension was defined as blood pressure ≥140/90 mm Hg per the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure24 or use of blood pressure–lowering medication. The presence of diabetes mellitus was defined based on the 2010 American Diabetes Association guidelines.25 Participants were classified as having diabetes mellitus if fasting glucose was ≥126 mg/dL, HbA1c level was ≥6.5%, or use diabetic medication was used within 2 weeks before the clinic visit.
Chronic obstructive lung disease (COPD) was defined per the GOLD (Global Initiative for Chronic Obstructive Lung Disease) guidelines as having a derived ratio of forced expiratory volume >1 second to forced vital capacity of <0.70.26 History of coronary heart disease (CHD) was defined as having a previous myocardial infarction that was self‐reported or noted from an ECG report. Chronic kidney disease was defined as having a glomerular filtration rate of <60 mL/min per 1.73 m2. Atrial fibrillation was defined based on the participant having Minnesota code 8‐3‐1 for electrocardiographic findings.
Statistical Analyses
Descriptive statistics were used to characterize the study sample. Continuous variables were presented as means and standard deviations. Categorical variables were presented as counts and percentages. ANOVA was used to test for difference of continuous variables, and the χ2 test was used to test for difference of categorical variables across the physical activity categories. We calculated person‐time, incident HF rates per 1000 person‐years for the eligible cohort and across levels of physical activity, and the respective confidence intervals.
We used Cox proportional hazards regression models to examine the relationship between MVPA and incident HFH and accounted for confounders that influenced this relationship. The proportional hazards assumption was examined and verified. Results were reported as hazard ratios (HRs) of the outcome for each level of MVPA compared with the referent group (poor health). We analyzed the association between MVPA and incident HFH with several models adjusting for age and sex and for age, sex, BMI, and covariates. Participants who died before the incident HF event were censored. To investigate whether censoring these participants significantly affected the estimates of incident HF, we conducted a sensitivity analysis by using a competing‐risk model, as described by Fine and Gray.27 The estimates from this analysis were presented as sub–hazard ratios.
Because development of HF may vary between men and women, as demonstrated in the NHANES I (first National Health and Nutrition Examination Survey) study, and obesity may increase HF risk,10, 28 we also examined effect modification by including interaction terms of sex and BMI in the model. P<0.10 for the interaction term was considered significant.
Of the 5301 participants, 253 did not have ejection fraction data. Because some of these participants may potentially have normal ejection fraction, we performed a sensitivity analysis to examine whether including them in the eligible cohort would substantially change the regression estimates compared with our original analysis.
Physical activity is associated with cardiovascular disease (CVD) risk, and CVD is associated with HF.29 To examine this relationship, we performed mediation and sensitivity analyses. We used a 4‐step approach for mediation analysis, as described by Baron and Kenny.30 We used logistic regression models to examine the relationships between (1) MVPA and incident HF, (2) MVPA and CVD, (3) CVD and incident HF, and (4) MVPA and incident HF controlling for CVD. If all 4 models showed a significant association, then the analyses suggest partial mediation. If the first 3 models showed a significant association but the last model did not, then they suggest complete mediation. In addition, we performed sensitivity analyses by either controlling for incident CHD or by excluding participants with incident CHD and compared those effect estimates to the one from the original analysis.
Given that this is an observational study, we attempted to address reverse causation. We excluded participants with ejection fraction <50% to obtain a study population with preserved ejection fractions. Besides just categorizing HFpEF based on ejection fraction, we performed sensitivity analyses examining comorbid conditions that are associated with HFpEF as well as physical activity. These conditions include COPD and atrial fibrillation, which could lead to the development of pulmonary hypertension and, by themselves, could limit functional capacity.31 We repeated the analyses by excluding participants with COPD or atrial fibrillation.
All statistical analyses were performed using STATA version 13.0 (StataCorp).
Results
Baseline Characteristics
Baseline characteristics and distribution of these characteristics by physical activity are presented in Table 1. Table S1 compares baseline variables of those in the analytic cohort with those of the excluded cohort, showing no difference between the 2 groups except for the prevalence of comorbid conditions. Some of this discrepancy may be explained by the presence of those with reduced ejection fractions in the excluded cohort.
Table 1.
Characteristics of the JHS Population at Baseline Visit by Physical Activity, 2000–2004
| AHA Physical Activity Categories | |||||
|---|---|---|---|---|---|
| Variable | Overall (n=4066) | Poor Healtha (n=1925) | Intermediate Healthb (n=1332) | Ideal Healthc (n=809) | P Value |
| Age, y | 55.01±12.43 | 57.30±12.09 | 53.50±12.14 | 52.05±12.70 | <0.001 |
| Sex | <0.001 | ||||
| Female | 2621 (64.46) | 1277 (66.34) | 881 (66.14) | 463 (57.23) | |
| Male | 1445 (35.54) | 648 (33.66) | 451 (33.86) | 346 (42.77) | |
| Body mass index, kg/m2 | 31.69±7.06 | 32.23±7.51 | 31.54±6.85 | 30.63±6.11 | <0.001 |
| Smoking status | <0.001 | ||||
| Never | 2821 (69.38) | 1300 (67.53) | 952 (71.48) | 569 (70.33) | |
| Current | 473 (11.63) | 285 (14.81) | 117 (8.78) | 71 (8.78) | |
| Former | 772 (18.99) | 340 (17.66) | 263 (19.74) | 169 (20.89) | |
| Hypertension | 2351 (57.82) | 1217 (63.22) | 729 (54.73) | 405 (50.06) | <0.001 |
| Diabetes mellitus | 805 (19.80) | 453 (23.53) | 236 (17.72) | 116 (14.34) | <0.001 |
| Chronic obstructive pulmonary disease | 322 (7.92) | 187 (9.71) | 90 (6.76) | 45 (5.56) | <0.001 |
| Coronary heart disease | 190 (4.67) | 107 (5.56) | 50 (3.75) | 33 (4.08) | 0.038 |
| Atrial fibrillation | 7 (0.17) | 4 (0.21) | 1 (0.08) | 2 (0.25) | <0.001 |
| Chronic kidney disease | 186 (4.57) | 103 (5.35) | 57 (4.28) | 26 (3.21) | 0.042 |
| Incident coronary heart diseased | 127 (3.29) | 77 (4.25) | 31 (2.43) | 19 (2.45) | 0.007 |
Data are presented as mean±SD or n (%). Physical activity is based on the American Heart Association Life's Simple 7.
Poor health is defined as 0 min of moderate and vigorous physical activity.
Intermediate health is defined as 1 to 149 min of moderate physical activity, 1 to 75 min of vigorous activity, or 1 to 149 min of combined moderate and vigorous physical activity.
Ideal health is defined as ≥150 min of moderate physical activity, ≥75 min of vigorous physical activity, or ≥150 min of combined moderate and vigorous physical activity.
Incident coronary heart disease excluding missing values (n=3862).
AHA indicates American Heart Association; JHS, Jackson Heart Study.
According to the duration of MVPA, 1925 of the 4066 participants had poor health (0 min/week), 1332 had intermediate health (1–149 min/week), and 809 had ideal health (≥150 min/week). Younger participants had higher minutes of MVPA. More smokers were in the poor health group compared with the intermediate and ideal health groups. The ideal health group had the fewest smokers.
The poor health group had the highest proportion of participants with hypertension; however, the proportion of those with hypertension in the intermediate and ideal health groups was substantial (>50%). Like hypertension, the proportion of diabetic participants was highest in the poor health group. About 14% of the participants in the ideal health group had diabetes mellitus. More participants with COPD, CHD, atrial fibrillation, and chronic kidney disease were in the poor health group compared with the intermediate and ideal health groups.
Person‐Time and Incidence Rates
The highest proportion of participants with HFH was found in the poor health group, followed by the intermediate and ideal health groups, as shown in Table 2. There were 168 HFHs. The incidence rates for those with poor, intermediate, and ideal health were 10.75, 5.72, and 2.69 HFHs per 1000 person‐years, respectively, demonstrating a monotonically decreasing trend.
Table 2.
Incidence Rates Per 1000 Person‐Years of Incident HFH Across Physical Activity Levels
| Physical Activity | Person‐Years | Events | Incidence Rate | 95% CI |
|---|---|---|---|---|
| Eligible cohort | 22 398 | 168 | 7.50 | 6.45–8.73 |
| Poor health | 10 604 | 114 | 10.75 | 8.95–12.92 |
| Intermediate health | 7338 | 42 | 5.72 | 4.23–7.75 |
| Ideal health | 4457 | 12 | 2.69 | 1.53–4.74 |
HFH indicates Heart Failure Hospitalization.
Association of Physical Activity and HFH
The cumulative hazard function curves are depicted in Figure. The slope for poor health was steeper than the slopes for intermediate and ideal health at all times. The cumulative hazard for intermediate and ideal health were similar until approximately year 4, when the slope became steeper in the intermediate health group compared with the ideal health group.
Figure 1.
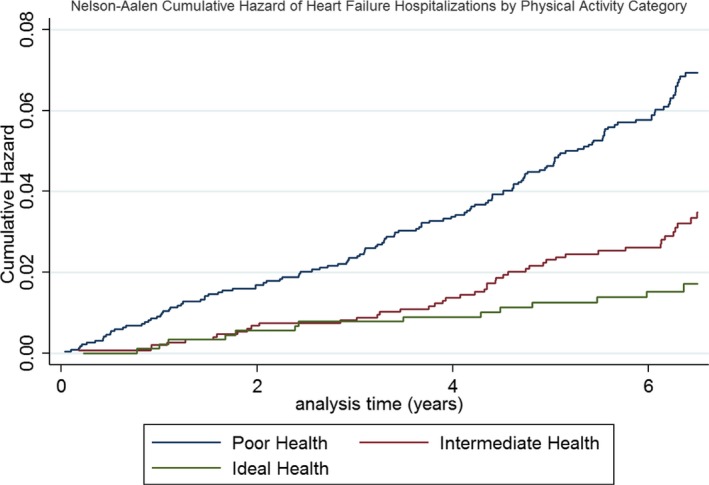
Depiction of the cumulative hazard (Nelson–Aalen estimator) of incident heart failure hospitalization by poor, intermediate, and ideal health. The difference in the survival functions across the 3 groups was statistically significant (log‐rank P<0.001). Incident heart failure hospitalization hazard decreased from poor to intermediate to ideal health (P trend<0.001).
The unadjusted, age and sex adjusted, and fully adjusted HRs of HFH are presented in Table 3. For all models, there was a significant (P trend) dose response in risk reduction across levels of physical activity. The inverse relationship between minutes of MVPA and incident HFH was greatest for the ideal health group (unadjusted HR: 0.24; age and sex adjusted HR: 0.35; fully adjusted HR: 0.41) and remained statistically significant despite confounding adjustments. For the intermediate health MVPA group, the relationship was more modest (unadjusted HR: 0.52; age and sex adjusted HR: 0.70; fully adjusted HR: 0.74) and demonstrated statistical significance only in the unadjusted model compared with the poor health MVPA category. The HRs in the unadjusted and adjusted models did not appear to differ after accounting for competing risk of death (Table S2). We did not find significant effect modification between MVPA and BMI or sex on incident HFH.
Table 3.
Unadjusted and Adjusted HRs of Incident HFH Across Physical Activity Levels
| Models | HR (95% CI) | P trend |
|---|---|---|
| Physical activity, crude | <0.001 | |
| Poor health | 1.00 (Referent) | |
| Intermediate health | 0.52 (0.36–0.73) | |
| Ideal health | 0.24 (0.13–0.44) | |
| Physical activity, age, and sex | <0.001 | |
| Poor health | 1.00 (Referent) | |
| Intermediate health | 0.70 (0.49–1.00) | |
| Ideal health | 0.35 (0.19–0.64) | |
| Physical activity, age, sex, BMI, smoking status, hypertension, COPD, CHD, atrial fibrillation, diabetes mellitus, and CKD | 0.003 | |
| Poor health | 1.00 (Referent) | |
| Intermediate health | 0.74 (0.52–1.07) | |
| Ideal health | 0.41 (0.22–0.74) |
BMI indicates body mass index; CHD, coronary heart disease; CI, confidence interval; CKD, chronic kidney disease; COPD, chronic obstructive pulmonary disease; HFH, heart failure hospitalization; HR, hazard ratio.
Sensitivity Analyses and Mediation
Because of concerns about selection bias, we performed a sensitivity analysis including participants with both known and unknown ejection fractions, excluding those with reduced ejection fractions (n=161). The unadjusted and adjusted models with the inclusion of participants with unknown ejection fractions are presented in Table 4. Similar to the primary analysis, we saw an inverse dose‐response relationship between minutes of MVPA and incident HFH.
Table 4.
Sensitivity Analysis: Unadjusted and Adjusted HR of Incident HFH Across Physical Activity Levels in Participants With Normal and Unknown Ejection Fraction
| Models | HR (95% CI) | P trend |
|---|---|---|
| Physical activity, crude | <0.001 | |
| Poor health | 1.00 (Referent) | |
| Intermediate health | 0.50 (0.37–0.72) | |
| Ideal health | 0.27 (0.16–0.48) | |
| Physical activity, age, and sex | 0.001 | |
| Poor health | 1.00 (Referent) | |
| Intermediate health | 0.70 (0.49–0.99) | |
| Ideal health | 0.40 (0.23–0.69) | |
| Physical activity, age, sex, BMI, smoking status, hypertension, COPD, CHD, atrial fibrillation, diabetes mellitus, CKD | 0.005 | |
| Poor health | 1.00 (Referent) | |
| Intermediate health | 0.73 (0.51–1.05) | |
| Ideal health | 0.45 (0.26–0.79) |
BMI indicates body mass index; CHD, coronary heart disease; CI, confidence interval; CKD, chronic kidney disease; COPD, chronic obstructive pulmonary disease; HFH, heart failure hospitalization; HR, hazard ratio.
The associations of intermediate and ideal health compared with poor health MVPA and incident HF were statistically significant (P<0.001 for both). Their associations with incident CHD was also significant (P=0.012 and P=0.004, respectively). The association of incident CHD and incident HF was significant (P<0.001). Finally, the association of intermediate and ideal health compared with poor health MVPA and incident HF adjusting for incident CHD remained significant (P<0.001 for both). These findings suggest that the association of physical activity with incident HF may be partially mediated by incident CHD. In addition, adjusting for or excluding incident CHD attenuated the association between intermediate health MVPA and incident HF. However, for ideal health MVPA, the effect estimate decreased after adjusting for incident CHD, and it remained similar compared with the original analysis after excluding incident CHD (Table S3).
In comparison with the effect estimates from the original analysis, excluding COPD or atrial fibrillation attenuated the association of intermediate health MVPA and incident HF. In the ideal health MVPA group, excluding COPD showed a modest decrease in the effect estimate, whereas excluding atrial fibrillation showed a larger reduction. (Table S4)
Discussion
This study of black men and women with normal ejection fractions and self‐reported HF demonstrated a dose response inverse relationship between minutes of moderate to vigorous physical activity and incident HFHs. The strongest association was found for the group that met national guidelines of ≥150 minutes of MVPA. The association of physical activity with incident HF was demonstrated to be partially mediated by incident CHD.
Our findings confirmed previous studies that higher physical activity level is associated with reducing the risk of presenting with HF. A recent meta‐analysis of 10 cohort studies (282 889 participants) found 28% risk reduction in the most physically active group compared with the least physically active group.32 There was no difference in risk between men and women. These effect estimates were similar to our findings.
The amount of improvement in physical activity required to reduce incident HF risk is unknown. However, an increase in activity level is likely to increase functional capacity, and higher functional status is associated with improved survival even in the presence of cardiovascular risk factors.33 From this we can speculate that improvement in physical activity may be associated with reduced risk of incident HF. Furthermore, other studies have shown an inverse dose‐response relationship between physical activity and risk of CHD and HF. Sattelmair et al observed that some physical activity was better than none and higher physical activity conferred more benefits in terms of reducing the risk of CHD.34 Pandey et al examined the quantitative dose‐response relationship between physical activity and HF risk. They also found an inverse linear dose‐response relationship, but a higher dose of physical activity above the minimum amount (500 min/week metabolic equivalent) recommended by guideline may be needed to significantly reduce the risk of incident HF compared with incident CHD.35 We also found a linear association between physical activity and incident HF, and findings from Pandey et al may explain our observation that ideal health MVPA was significantly associated with reduced risk of incident HF.
In terms of the difference in developing HFpEF compared with HFrEF with varying physical activity levels, studies in other populations have suggested that increased physical activity is associated with lower HFpEF and not HFrEF risk. Based on multivariable results from the Framingham Heart Study, higher physical activity index was associated with lower HF and HFpEF risk in older adults, whereas this association was attenuated in those with HFrEF.11 In a more recent study, which included participants from 3 cohort studies (Women's Health Initiative, Multi‐Ethnic Study of Atherosclerosis, and CHS [Cardiovascular Health Study]), any physical activity was not associated with HFrEF risk. Two times higher than the recommended minimum amount of physical activity was needed to demonstrate a reduction in HFpEF risk.9 These findings suggest that the management considerations are different for both types of HF. In addition, although HFpEF is associated with comorbid conditions that affect the heart such as obesity, hypertension, and diabetes mellitus, the benefits of physical activity for these conditions may possibly explain, in part, the effect of physical activity on HFpEF risk.
Several risk factors have been demonstrated to be associated with HF. He et al demonstrated in the NHANES I cohort of 13 643 men and women without history of HF that HF was associated with physical inactivity, male sex, less education, smoking, obesity, diabetes mellitus, hypertension, valvular heart disease, and CHD10; however, that study included only a small proportion (13–15%) of black participants.
A few studies have examined sex‐specific association of physical activity and HF risk. Kenchaiah et al evaluated the association of vigorous physical activity and HF risk in men who participated in the Physicians' Health Study.13 Vigorous physical activity was associated with an 18% reduction in HF risk. Like our study, interaction was not found among BMI, vigorous physical activity, and HF risk. Rahman et al examined the association between physical activity and HF in women.36 A cohort of 27 895 women was followed for 13 years. Moderate to high levels of physical activity were associated with 27% to 35% HF risk, depending on the type of activity. Agha et al demonstrated in the Women's Health Initiative that the health lifestyle score was associated with the risk of HF in postmenopausal women.37 The score incorporated several components that resemble good health, and a criterion was being physically active. Women who were somewhat active and highly active had a 23% and 31% decrease in HF risk, respectively, compared with those who were inactive. We did not find that sex confounded the relationship between physical activity and HF in our study.
Approximately 23% of the eligible participants in our study were ≥65 years old. Previous studies have demonstrated the protective effect of physical activity on HF risk in the elderly. Patel et al evaluated older adults aged ≥65 years in the CHS and their need for higher levels of physical activity to reduce incident HF risk.38 The CHS cohort was composed mainly of women, and 15% of the 5503 participants were black. After adjusting for age, sex, and race, medium and high physical activity compared with no physical activity were associated with significant reductions in incident HF risk (32% and 40%, respectively). The amount of risk reduction in the medium physical activity group was similar to our intermediate health group. In a more recent study, Kraigher‐Krainer et al evaluated 1142 older community participants in the Framingham Heart Study and found that physical activity was associated with reduced risk of incident HF. Their estimated HF risk in the age‐ and sex‐adjusted models of physical activity ranged from 0.68 to 0.57 for those who performed MVPA compared with those who were sedentary.11
As discussed, only a few studies included black participants. The study that included the largest proportion of black participants was the one performed by Bell et al39 They investigated the relationship between physical activity and incident CVD defined as incident HF, stroke, or CHD. They included 10 018 white and 3707 black participants and followed this cohort for 21 years. After adjusting for confounders, they found 35% CVD risk reduction in the intermediate physical activity group and 41% reduction in the recommended physical activity group compared with the poor physical activity group among black participants. Similar risk reduction was found when examining HF incidence. There was no apparent difference in effect estimates between black and white participants. Two‐dimensional echocardiography was not available, and the study may have been confounded with participants having HFrEF.
The abovementioned studies used total duration of MVPA (work plus leisure time physical activity) as a measurement of activity intensity. Some studies have used other definitions of physical activity such as sedentary time and leisure time physical activity, which may better represent activity that provides cardiovascular protection. Andersen et al compared total and leisure time physical activity with regard to risk of HF.40 They included 39 805 Swedish participants. Both total and leisure time physical activity lowered HF risk, but leisure time activity had a greater effect compared with total physical activity level. With total physical activity, there was a ≈20% reduction in HF risk in those who were most active. With leisure time physical activity, there was about a 50% reduction in HF risk in those who were most active. Using the Copenhagen City Heart Study, Saevereid et al expanded on findings of leisure time activity to include speed and duration of walking and examined their association with subsequent hospitalization or death from HF.41 They found that light and moderate to high leisure time physical activity was associated with lowering HF risk by 25% and 20%, respectively. Walking speed was associated with greater reduction in HF risk compared with walking duration. In contrast with physical activity time, Young et al examined the association of sedentary time and HF risk in 82 695 men from the California Men's Health Study.42 The cohort was followed for 10 years. In addition to medium and low physical activity time, medium and high sedentary time increased HF risk. These studies also lack 2‐dimensional echocardiography data.
Limitations and Strengths
An association between MVPA and HFH in black adults was present, but our study had a few limitations. Because HFH was adjudicated in 2005, left truncation of the data was present. This may be a limitation and a strength of our study. As a strength, assessment of MVPA and HFH at different time points provided temporal separation between the exposure and the outcome and made reverse causality highly unlikely.
In particular, those who had a sedentary lifestyle at baseline were at risk of developing HFpEF in the future. However, we were unable to determine whether those at baseline already had diastolic dysfunction due to unavailable tissue Doppler measurements, which, in turn, may restrict physical activity. In addition, pulmonary dysfunction, such as COPD, may also limit exercise capacity. We attempted to address reverse causation by performing sensitivity analyses accounting for incident CHD, COPD, or atrial fibrillation. We found that these risk factors attenuated the association of intermediate health MVPA and incident HF. In contrast, ideal health MVPA was associated with lower risk of incident HF. Consequently, incident CHD, COPD, and atrial fibrillation may be associated with incident HF and may limit the impact of the estimates, but our findings provided a notion that greater physical activity may be a potential early intervention in preventing HF in the black population.
The JHS cohort was recruited from a limited geographical area of Jackson, Mississippi. Black participants in that location may not represent black adults in other parts of the country, and our findings may not be generalizable.
MVPA was categorized based on self‐reported duration of activity over a week. Self‐report of physical activity has been shown to be prone to recall bias and may be a source of misclassification.43 AHA categories of poor and ideal health may be less prone to misclassification due to the extreme values for MVPA (0 minutes for poor health and ≥150 minutes of moderate physical activity, ≥75 minutes of vigorous physical activity, or ≥150 minutes of combined moderate and vigorous physical activity for ideal health). In contrast, because of a wide range of activity duration with a minimum value of 1 minute, the intermediate health group may contain some participants who were misclassified. Those who were sedentary may overestimate their activity level and be classified in the intermediate health group.
Last, other types of physical activity measurement such as type, speed, and duration of physical activity, leisure time, or sedentary time were not available. Consequently, we were not able to determine which type of activity was beneficial in the black population. Nonetheless, we defined physical activity based on a widely accepted method designed by the AHA.
Our study had several strengths. It is the first study to examine the relationship between MVPA and HFH in black participants with normal ejection fraction at the time of assessment of self‐reported physical activity. The JHS included a large cohort of black participants and collected multiple relevant variables for confounder adjustment. In addition, it acquired 2‐dimensional echocardiograms at the time of physical activity evaluation, assessed MVPA using a validated questionnaire (AHA Life's Simple 7), and adjudicated HFH events over several years.
Conclusion
Black adults are at risk to develop HF because they have a higher prevalence of associated risk factors, such as obesity, hypertension, and diabetes mellitus. Besides careful management of comorbid conditions, strategies for preventing HF are limited. Physical activity has been demonstrated to be beneficial in many chronic diseases. Its relationship to HF in the black population is understudied. In our study, we found that ideal and, to an extent, intermediate health MVPA was associated with reducing the risk of incident HF events in black adults with normal ejection fractions. Encouragement of MVPA for at‐risk black adults should be considered.
Sources of Funding
The Jackson Heart Study (JHS) is supported and conducted in collaboration with Jackson State University (HHSN268201300049C and HHSN268201300050C), Tougaloo College (HHSN268201300048C), and the University of Mississippi Medical Center (HHSN268201300046C and HHSN268201300047C) contracts from the National Heart, Lung, and Blood Institute (NHLBI) and the National Institute for Minority Health and Health Disparities (NIMHD). The efforts for this project were also supported by NHLBI T32 contract.
Disclosures
None.
Supporting information
Table S1. Characteristics of the Excluded Cohort at Baseline Visit by Physical Activity, 2000–2004
Table S2. Unadjusted and Adjusted Hazard Ratios of Incident Heart Failure Hospitalization
Table S3. Unadjusted and Adjusted Hazard Ratios of Incident Heart Failure Hospitalization Across Physical Activity Levels With Full Model Adjusting for Incident Coronary Heart Disease or Excluding Participants With Incident Coronary Heart Disease
Table S4. Unadjusted and Adjusted Hazard Ratios of Incident Heart Failure Hospitalization Across Physical Activity Levels With Full Model Excluding Participants With Incident Coronary Heart Disease, Chronic Obstructive Pulmonary Disease, or Atrial Fibrillation
Acknowledgments
The authors wish to thank the staff and participants of the Jackson Heart Study. The views expressed in this article are those of the authors and do not necessarily represent the views of the National Heart, Lung, and Blood Institute; the National Institutes of Health; or the US Department of Health and Human Services.
(J Am Heart Assoc. 2017;6:e006107 DOI: 10.1161/JAHA.117.006107.)28882818
References
- 1. Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Blaha MJ, Dai S, Ford ES, Fox CS, Franco S, Fullerton HJ, Gillespie C, Hailpern SM, Heir JA, Howard VJ, Huffman MD, Judd SE, Kissela BM, Kittner SJ, Lackland DT, Lichtman JH, Lisabeth LD, Mackey RH, Magid DJ, Marcus GM, Marelli A, Matchar DB, McGuire DK, III Mohler ER, Moy CS, Mussolino ME, Neumar RW, Nichol G, Pandey DK, Paynter NP, Reeves MJ, Sorlie PD, Stein J, Towfighi A, Turan RN, Virani SS, Wong ND, Woo D, Turner MB; American Heart Association Statistics Committee and Stroke Statistics Subcommittee . Executive summary: heart disease and stroke statistics—2014 update: a report from the American Heart Association. Circulation. 2014;129:399–410. [DOI] [PubMed] [Google Scholar]
- 2. Heidenreich PA, Albert NM, Allen LA, Bluemke DA, Butler J, Fonarow GC, Ikonomidis JS, Khavjou O, Konstam MA, Maddox TM, Nichol G, Pham M, Piña IL, Trogdon JG; American Heart Association Advocacy Coordinating Committee; Council on Arteriosclerosis, Thrombosis and Vascular Biology; Council on Cardiovascular Radiology and Intervention; Council on Clinical Cardiology; Council on Epidemiology and Prevention; Stroke Council . Forecasting the impact of heart failure in the United States: a policy statement from the American Heart Association. Circ Heart Fail. 2013;6:606–619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Gupta DK, Shah AM, Castagno D, Takeuchi M, Loehr LR, Fox ER, Butler KR, Mosley TH, Kitzman DW, Solomon SD. Heart failure with preserved ejection fraction in African Americans: the ARIC (Atherosclerosis Risk in Communities) study. JACC Heart Fail. 2013;1:156–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Reed BN, Sueta CA. A practical guide for the treatment of symptomatic heart failure with reduced ejection fraction (HFrEF). Curr Cardiol Rev. 2015;11:23–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Nolte K, Herrmann‐Lingen C, Wachter R, Gelbrich G, Düngen HD, Duvinage A, Hoischen N, von Oehsen K, Schwarz S, Hasenfuss G, Halle M, Pieske B, Edelmann F. Effects of exercise training on different quality of life dimensions in heart failure with preserved ejection fraction: the Ex‐DHF‐P trial. Eur J Prev Cardiol. 2015;22:582–593. [DOI] [PubMed] [Google Scholar]
- 6. Flack JM, Ferdinand KC, Nasser SA. Epidemiology of hypertension and cardiovascular disease in African Americans. J Clin Hypertens (Greenwich). 2003;5:5–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Jolly S, Vittinghoff E, Chattopadhyay A, Bibbins‐Domingo K. Higher cardiovascular disease prevalence and mortality among younger blacks compared to whites. Am J Med. 2010;123:811–818. [DOI] [PubMed] [Google Scholar]
- 8. Yan H, Behun MA, Cook MD, Ranadive SM, Lane‐Cordova AD, Kappus RM, Woods JA, Wilund KR, Baynard T, Halliwill JR, Fernhall B. Differential post‐exercise blood pressure responses between Blacks and Caucasians. PLoS One. 2016;11:e0153445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Pandey A, LaMonte M, Klein L, Ayers C, Psaty BM, Eaton CB, Allen NB, de Lemos JA, Carnethon M, Greenland P, Berry JD. Relationship between physical activity, body mass index, and risk of heart failure. J Am Coll Cardiol. 2017;69:1129–1142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. He J, Ogden LG, Bazzano LA, Vupputuri S, Loria C, Whelton PK. Risk factors for congestive heart failure in US men and women: NHANES I epidemiologic follow‐up study. Arch Intern Med. 2001;161:996–1002. [DOI] [PubMed] [Google Scholar]
- 11. Kraigher‐Krainer E, Lyass A, Massaro JM, Lee DS, Ho JE, Levy D, Kannel WB, Vasan RS. Association of physical activity and heart failure with preserved vs. reduced ejection fraction in the elderly: the Framingham Heart Study. Eur J Fail. 2013;15:742–746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Hu G, Jousilahti P, Antikainen R, Katzmarzyk PT, Tuomilehto K. Joint effects of physical activity, body mass index, waist circumference, and waist‐to‐hip ratio on the risk of heart failure. Circulation. 2010;121:237–244. [DOI] [PubMed] [Google Scholar]
- 13. Kenchaiah S, Sesso HD, Gaziano JM. Body mass index and vigorous physical activity and the risk of heart failure among men. Circulation. 2009;119:44–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Taylor HA Jr, Wilson JG, Jones DW, Sarpong DF, Srinivasan A, Garrison RJ, Nelson C, Wyatt SB. Toward resolution of cardiovascular health disparities in African Americans: design and methods of the Jackson Heart Study. Ethn Dis. 2005;15:S6–4‐17. [PubMed] [Google Scholar]
- 15. Fuqua SR, Wyatt SB, Andrew ME, Sarpong DF, Henderson FR, Cunningham MF, Taylor HA Jr. Recruiting African‐American research participation in the Jackson Heart Study: methods, response rates, and sample description. Ethn Dis. 2005;15:S6–S18. [PubMed] [Google Scholar]
- 16. Lloyd‐Jones DM, Hong Y, Labarthe D, Mozaffarian D, Appel LJ, Van Horn L, Greenlund K, Daniels S, Nichol G, Tomaselli GF, Arnett DK, Fonarow GC, Ho PM, Lauer MS, Masoudi FA, Robertson RM, Roger V, Schwamm LH, Sorlie P, Yancy CW, Rosamond WD; American Heart Association Strategic Planning Task Force and Statistics Committee . Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association's strategic Impact Goal through 2020 and beyond. Circulation. 2010;121:586–613. [DOI] [PubMed] [Google Scholar]
- 17. Physical Activity Guidelines Advisory Committee . Physical Activity Guidelines Advisory Report. Washington, DC: US Dept of Health and Human Services; 2008. [Google Scholar]
- 18. US Department of Health and Human Services . 2008 Physical Activity Guidelines for Americans. Washington, DC: US Dept of Health and Human Services; 2008. [Google Scholar]
- 19. Janssen I, Carson V, Lee IM, Katzmarzyk PT, Blair SN. Years of life gained due to leisure‐time physical activity in the U.S. Am J Prev Med. 2013;44:23–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Keku E, Rosamond W, Taylor HA Jr, Garrison R, Wyatt SB, Richard M, Jenkins B, Reeves L, Sarpong D. Cardiovascular disease event classification in the Jackson Heart Study: methods and procedures. Ethn Dis. 2005;15:S6–S62. [PubMed] [Google Scholar]
- 21. Mentz RJ, Greiner MA, DeVore AD, Dunlay SM, Choudhary G, Ahmad T, Khazanie P, Randolph TC, Griswold ME, Eapen ZJ, O'Brien EC, Thomas KL, Curtis LH, Hernandez AF. Ventricular conduction and long‐term heart failure outcomes and mortality in African Americans: insights from the Jackson Heart Study. Circ Heart Fail. 2015;8:243–251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Lam CS, Donal E, Kraigher‐Krainer E, Vasan RS. Epidemiology and clinical course of heart failure with preserved ejection fraction. Eur J Heart Fail. 2011;13:18–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Wu CK, Lee JK, Chiang FT, Lin LY, Lin JW, Hwang JJ, Tseng CD, Tsai CT. Prognostic factors of heart failure with preserved ejection fraction: a 12‐year prospective cohort follow‐up study. Int J Cardiol. 2014;171:331–337. [DOI] [PubMed] [Google Scholar]
- 24. Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, Jones DW, Materson BJ, Oparil S, Wright JT Jr, Roccella EJ; National Heart, Lung, and Blood Institute Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; National High Blood Pressure Education Program Coordinating Committee . The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289:2560–2572. [DOI] [PubMed] [Google Scholar]
- 25. American Diabetes Association . Diagnosis and classification of diabetes mellitus. Diabetes Care. 2010;33:S62–S69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Vestbo J, Hurd SS, Agusti AG, Jones PW, Vogelmeier C, Anzueto A, Barnes PJ, Fibbri LM, Martinez FJ, Nishimura M, Stockley RA, Sin DD, Rodriguez‐Roisin R. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med. 2013;187:347–365. [DOI] [PubMed] [Google Scholar]
- 27. Fine JP, Gray RJ. A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc. 1999;94:496–509. [Google Scholar]
- 28. Kenchaiah S, Evans JC, Levy D, Wilson PW, Benjamin EJ, Larson MG, Kannel WB, Vasan RS. Obesity and the risk of heart failure. N Engl J Med. 2002;347:305–313. [DOI] [PubMed] [Google Scholar]
- 29. Shiroma EJ, Lee IM. Physical activity and cardiovascular health: lessons learned from epidemiological studies across age, gender, and race/ethnicity. Circulation. 2010;122:743–752. [DOI] [PubMed] [Google Scholar]
- 30. Baron RM, Kenny DA. The moderator‐mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51:1173–1182. [DOI] [PubMed] [Google Scholar]
- 31. Lam CS, Roger VL, Rodeheffer RJ, Borlaug BA, Enders FT, Redfield MM. Pulmonary hypertension in heart failure with preserved ejection fraction: a community‐based study. J Am Coll Cardiol. 2009;53:1119–1126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Echouffo‐Tcheugui JB, Butler J, Yancy CW, Fonarow GC. Association of physical activity or fitness with incident heart failure: a systematic review and meta‐analysis. Circ Heart Fail. 2015;8:853–861. [DOI] [PubMed] [Google Scholar]
- 33. Myers J, Prakash M, Froelicher V, Do D, Partington S, Atwood JE. Exercise capacity and mortality among men referred for exercise testing. N Engl J Med. 2002;346:793–801. [DOI] [PubMed] [Google Scholar]
- 34. Sattelmair J, Pertman J, Ding EL, Kohl HW III, Haskell W, Lee IM. Dose response between physical activity and risk of coronary heart disease: a meta‐analysis. Circulation. 2011;124:789–795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Pandey A, Garg S, Khunger M, Darden D, Ayers C, Kumbhani DJ, Mayo HG, de Lemos JA, Berry JD. Dose‐response relationship between physical activity and risk of heart failure: a meta‐analysis. Circulation. 2015;132:1786–1794. [DOI] [PubMed] [Google Scholar]
- 36. Rahman I, Bellavia A, Wolk A. Relationship between physical activity and heart failure risk in women. Circ Heart Fail. 2014;7:877–881. [DOI] [PubMed] [Google Scholar]
- 37. Agha G, Loucks EB, Tinker LF, Waring ME, Michaud DS, Foraker RE, Li W, Martin LW, Greenland P, Manson JE, Eaton CB. Health lifestyle and decreasing risk of heart failure in women: the Women's Health Initiative observational study. J Am Coll Cardiol. 2014;64:1777–1785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Patel K, Sui X, Zhang Y, Fonarow GC, Aban IB, Brown CJ, Bittner V, Kitzman DW, Allman RM, Banach M, Aronow WS, Anker SD, Blair SN, Ahmed A. Prevention of heart failure in older adults may require higher levels of physical activity than needed for other cardiovascular events. Int J Cardiol. 2013;168:1905–1909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Bell EJ, Lutsey PL, Windham BG, Folsom AR. Physical activity and cardiovascular disease in African Americans in Atherosclerosis Risk in Communities. Med Sci Sports Exerc. 2013;45:901–907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Andersen K, Mariosa D, Adami HO, Held C, Ingelsson E, Lagerros YT, Nyren O, Ye W, Bellocco R, Sundström J. Dose‐response relationship of total and leisure time physical activity to risk of heart failure: a prospective cohort study. Circ Heart Fail. 2014;7:701–708. [DOI] [PubMed] [Google Scholar]
- 41. Saevereid HA, Schnohr P, Prescott E. Speed and duration of walking and other leisure time physical activity and the risk of heart failure: a prospective cohort study from the Copenhagen City Heart Study. PLoS One. 2014;9:e89909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Young DR, Reynolds K, Sidell M, Brar S, Ghai NR, Sternfeld B, Jacobsen SJ, Slezak JM, Caan B, Quinn VP. Effects of physical activity and sedentary time on the risk of heart failure. Circ Heart Fail. 2014;7:21–27. [DOI] [PubMed] [Google Scholar]
- 43. Shephard RJ. Limits to the measurement of habitual physical activity by questionnaires. Br J Sports Med. 2003;37:197–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Characteristics of the Excluded Cohort at Baseline Visit by Physical Activity, 2000–2004
Table S2. Unadjusted and Adjusted Hazard Ratios of Incident Heart Failure Hospitalization
Table S3. Unadjusted and Adjusted Hazard Ratios of Incident Heart Failure Hospitalization Across Physical Activity Levels With Full Model Adjusting for Incident Coronary Heart Disease or Excluding Participants With Incident Coronary Heart Disease
Table S4. Unadjusted and Adjusted Hazard Ratios of Incident Heart Failure Hospitalization Across Physical Activity Levels With Full Model Excluding Participants With Incident Coronary Heart Disease, Chronic Obstructive Pulmonary Disease, or Atrial Fibrillation


