Abstract
Background
Somatic complaints are often the presenting symptoms of major depressive disorder (MDD) in the outpatient context, because this may go unrecognized. It is well understood that MDD carries an increased risk of suicide. This study aimed to identify the risk factors and association with both MDD and suicidality among Han Chinese outpatients.
Methods
A multicenter study was carried out in 5189 outpatient adults (≥18 years old) in four general hospitals in Guangzhou, China. The 1392 patients who had the Patient Health Questionnaire-9 (PHQ-9) score ≥ 5, indicating depressive symptoms were offered an interview with a psychiatrist by the Mini International Neuropsychiatric Interview (MINI); 819 patients consented and completed the MINI interview. MINI module B was used to assess suicidality. Stepwise binary logistic models were used to estimate the relationship between a significant risk factor and suicide or MDD. According to with or without MDD, the secondary analysis was performed using the logistic regression model for the risk of suicidility.
Results
The current prevalence of MDD and the one month prevalence of suicidality were 3.7% and 2.3% respectively. The odds ratio of suicidality in women was more than twice that in men (OR = 2.62; 95% CI 1.45–4.76). Other risk factors which were significantly associated with suicidality were: living alone, higher education, self-reported depression, getting psychiatric diagnoses (MDD, anxiety disorders, and bipolar disorders). Significant risk factors for MDD were also noticed, such as comorbid anxiety disorders, self-reported anxiety, insomnia, suicidal ideation.
Limitation
It’s a cross-sectional study in outpatient clinics using self-report questionnaires.
Conclusion
This study provides valuable data about the risk factors and association of MDD and suicide risk in adult outpatients in Han Chinese. Those factors allow better the employment of preventative measures.
1. Introduction
Major depressive disorder (MDD) is the most prevalent psychiatric disease and is a major contributor to the global burden of disease [1]. This burden originates in two major sequelae of depression: declining physical health, and suicide. MDD is responsible for 11% of years lived with a disability, and up to 15% of individuals with recurrent MDD commit suicide [2,3]. Suicidality (ideation, plans, and attempts) is a significant cause of injury and mortality in the world, ranking as the 14th most common cause of death by the World Health Organization (WHO) [4,5].
However, the prevalence of suicide is not homogenous. In China, it is the fifth most common cause of death and is the most common cause of death amongst adolescents and young adults (15–34 years old) [6]. This is in contrast to the United States, where suicide is the tenth most common cause of death and second most common cause of death amongst 15–34 years old [7]. Traditionally, research on suicide risk has been conducted mainly in Europe and the United States; however, the ability of a given risk factor to provoke suicidality clearly varies by region. Moreover, the prevalence of suicide and its associated risk factors have been under-investigated in China [8]. The city of Guangzhou provides a relevant setting within China to study risk factors for suicidality, as it is home to more than 13 million people and is highly cosmopolitan.
Psychiatric disorders are a well-established risk factor for suicidility [9]. Affective disorders possess the greatest risk; it has been estimated that half of all individuals who complete suicide meet criteria for MDD. The association between MDD and suicidality is also very strong [10]. Thus, identifying MDD is a crucial component of any effective preventative screening for suicidality. However, given that half of patients who commit suicide do not meet MDD criteria, it is also important to screen for suicidality independently of an MDD diagnosis.
A nationwide study during 2004–2008 across China showed that 0.7% of Chinese adults had major depressive episode [11]. MDD has a point prevalence of 15% in the primary care setting, and 5% in the general population [12,13]. Major depression is a disabling mood disorder that is present in 5–10% of primary care patients, including 10–20% of patients with chronic medical conditions [14]. Although there are effective interventions to reduce the burden of depression, the majority is inadequately treated [15]. The presence of depression is reported to worsen medical prognosis, increase physical symptom burden, complicate self-care and treatment-adherence, the costs of care, and probably also increase mortality [16,17]. A number of population studies have shown an increased risk of associated with a range of specific physical illnesses [18,19]. The need for more effective screening in both physical and mental health is evident.
The aim of our study is to provide the risk factors which correlate with MDD and suicidality in a Han Chinese population.
2. Methods and materials
2.1 Setting and participants
In this multicenter, cross-sectional study, data was collected from outpatient divisions in four tertiary general hospitals in Guangzhou from March 15 to June 30, 2016. The survey starting date was randomly selected. Three hospitals recruited participants from the gastroenterology, cardiology, and gynecology clinics; and all four hospitals recruited from their neurology clinics. Participants were included if they were over 18 years old, consented to study participation, and were able to complete the PHQ-9 questionnaire. They were excluded if they did not or could not provide written informed consent, had previously received screening for depression, had a serious physical or mental condition, or had a language or hearing difficulty. In all, 5284 accepted the survey, but 5189 consecutive eligible adult outpatients completed the PHQ-9 questionnaire and were recruited for the statistics, finally, 819/1392 who got PHQ-9 scores≥5 received further psychiatric interview (see Fig 1). The authors had access to information that could identify individual participants during or after data collection.
Fig 1. Flowchart of the study on prevalence of major depressive disorders and suicide risk from general hospitals in Guangzhou.
All investigators participated in a two-day training session that described the clinical questionnaires, data collection methods, and goal of the study, as well as the ethical principles of human subject research. All questionnaires were administered by psychiatric postgraduates and senior students in clinical psychology. Three psychiatrists with more than 5 years of experience received four days of training on administering the Mini International Neuropsychiatric Interview (MINI) and used this tool to perform diagnostic interviews at each investigative site. These methods were approved by the Guangzhou Huiai Hospital Ethics Committee. China Clinical Trials Registration Center Registration No.: ChiCTR-INR-16008066.
2.2 Study procedures
First, the patients consented and filled out a written questionnaire containing demographic questions and the PHQ-9 scale. Only those which were completed were considered valid and included in the study; then, the investigators administered the other self-report questionnaire. If the PHQ-9 score was greater than 4, the investigators referred the patient to one of the three psychiatrists. If the participant consented, the psychiatrist performed the structured MINI to confirm the presence of MDD met the DSM-Ⅳ diagnostic criteria and suicidality.
2.3 Research instruments
Patient Health Questionnaire-9(PHQ-9) [20,21] is a 9-item self-report questionnaire derived from the full PHQ. It assesses the presence of symptomatic criteria of a major depressive episode (MDE) and the severity of each symptom. It also evaluates frequency of each symptom via a 4-point Likert scale, from 0 (not at all) to 3 (nearly every day). Based upon the sum of these items, participants are categorized into 4 categories of depressive symptoms: minimal (0–4), mild (5–9), moderate (10–14), and severe (≥15).
Generalized Anxiety Disorder Scale-7(GAD-7) [22,23] is a 7 question self-report questionnaire which assesses the frequency of symptoms of general anxiety via a 4-point Likert scale, from 0 (not at all) to 3 (nearly every day).
The 15-symptom Patient Health Questionnaire (PHQ-15) [24,25] is 15-item self-report questionnaire derived from the full PHQ. It assesses the somatic symptoms and symptom clusters that account for more than 90% of physical complaints reported in the outpatient setting. Each item is scored on a 3-point Likert scale from 0 (not bothered at all) to 2 (bothered a lot) and the total is summed; a higher score indicates greater severity of somatic symptoms and physical complaints.
Medical Outcomes Study Short Form-12 (SF-12) [26,27] is a 12-question self-report measure of patient health. It has two domains: the physical component score (PCS) and the mental component score (MCS). Higher scores indicate a better quality of life (QOL).
Insomnia is not measured in the SF-12, but is highly relevant to our study of depression. We assessed insomnia with 3 questions validated for screening in previous studies [28]. The questions were as follows: “In the past month, do you have difficulty falling asleep?”, “…do you have difficulty in maintaining sleep and in waking up?”, and “…do you wake up in the middle of the night or in the early morning and have difficulty falling asleep again?”. If at least one answer was “often”, then the patient was deemed to have insomnia.
Mini International Neuropsychiatric Interview 6.0.0 (MINI) [29,30] is a psychiatrist-administered, structured interview assessing Diagnostic and Statistical Manual of Mental Diseases (DSM)-IV Axis I disorders. The MINI is robust and closely resembles the Structured Clinical Interview for the DSM-IV. The developer of the scale, Dr. David Sheehan, approved the use of the MINI 6.0.0 (Chinese version) for this investigation.
Mini International Neuropsychiatric Interview 6.0.0 module B (MINI module B) is a 15-question, yes-or-no interviewer-administered questionnaire used to evaluate suicidality and current risk of suicide. The first 3 questions screened for a recent suicide attempt in the past month, the next 14 for suicidal ideation, planning, or attempts in the past month, and the last question asks if the patient has ever attempted suicide in their life. The first 3 are excluded from the score, and the remainder are summed and categorized as low risk (<9), medium risk (9–16), or high risk (≥17) of future suicide attempts.
2.4 Statistical analysis
Demographic data were reported as frequency or percentage. If an item was not reported, it was counted as a missing value. A Receiver Operating Characteristic (ROC) curve was employed to identify a continuous variable threshold for dichotomization of each of the aforementioned scales into “low” and “high” score categories (“low”: PCS ≤39; MCS ≤47). Patients were classified in two ways for analysis: those with vs those without MDD, and those with vs those without suicidality. The Chi-square or Fischer’s exact test was used to determine the statistical significance of differences in distribution of categorical sociodemographic and clinical risk factors between groups for a given classification. The independent sample t-test was used for continuous variables with approximately normal distribution. The Chi-square test was used specifically for differences in groups based on marital status, living condition, and educational attainment. Comparison of the two groups’ rates with Bonferroni correction and the level of significance was 0.017.
Stepwise binary logistic regression analysis with the forward conditional method was used to determine the correlates of MDD and suicidality. When MDD was used as the dependent variable, the independent variables were those factors which proved significantly different between participants with vs those without MDD in the bivariate correlation analysis. When suicidality was used as the dependent variable, the independent variables were those factors which proved significantly different between participants with vs those without suicidality in the bivariate correlation analysis. The level of significance was set at 0.05 (two-tailed). All statistical analyses were performed using SPSS21.0 statistical software (SPSS Inc., Chicago, United States).
3. Results
3.1 Study population characteristics
Table 1 contains the summary of participant sociodemographic and clinical characteristics. The majority of the sample were women (66.2%), married (79.4%), and the plurality had medium educational attainment (7–12 years; 48.0%). 69.8% of participants reported low quality of life due to poor physical health and 45.3% reported low quality of life due to poor mental health on the SF-12 scale. 15.7% reported insomnia. The average scores on PHQ-9, GAD-7 and PHQ-15 scales were relatively 3.6±4.3, 3.2±4.2, and 5.0±4.5. There were 2.0% of participants with hopelessness. 89.2% of suicidal patients reported hopelessness, making it the most common symptom of suicidality. Suicide risk score stratification reported 1.6% of the sample at low, 0.5% at medium, and 0.2% at high risk of. The affective state evaluated by the MINI interview revealed a 3.5% current prevalence of anxiety spectrum disorders, a 1.6% current prevalence of bipolar disorder, a 3.7% MDD current prevalence, and a 2.9% MDD prevalence within the past two weeks.
Table 1. Characteristics of the demographic and clinical characteristics of the study population (N = 5189).
| Characteristics | N | % |
|---|---|---|
| Sex | ||
| Male | 1753 | 33.8 |
| Female | 3436 | 66.2 |
| Education | ||
| Illiterate or primary school (0–6) | 992 | 19.1 |
| Junior and senior high school(7–12) | 2490 | 48.0 |
| College and above(≥13) | 1707 | 32.9 |
| Marital status | ||
| Never married | 807 | 15.6 |
| Married | 4122 | 79.4 |
| Other(divorce/widowed) | 260 | 5.0 |
| Living condition | ||
| Alone | 468 | 9.0 |
| Live with families | 4354 | 83.9 |
| Othera | 367 | 7.1 |
| PCS | ||
| High(>39) | 1568 | 30.2 |
| Low(≤39) | 3621 | 69.8 |
| MCS | ||
| High(>47) | 2840 | 54.7 |
| Low(≤47) | 2349 | 45.3 |
| Smoking(yes) | 584 | 13.2 |
| Drinking(yes) | 970 | 21.6 |
| Any insomnia(yes) | 979 | 18.9 |
| Major depressive disorder(yes) | 190 | 3.7 |
| Anxiety disorders(yes) | 174 | 3.4 |
| Bipolar disorders(yes) | 85 | 1.6 |
| Hopelessness(yes) | 107 | 2.0 |
| Mean±SD b | ||
| Age(years) | 42.1±16.0 | |
| PHQ-9 total scores | 3.6±4.3 | |
| GAD-7 total scores | 3.2±4.2 | |
| PHQ-15 total scores | 5.0±4.5 |
a Other (living in a nursing home or dormitory)
b Continuous variables, Mean± standard deviation (SD)
120 patients had suicide risk, of which there are 84 low scores (1–8), moderate to 26 individuals (9–16), high score of 10 people (≥17).
PHQ-15: Patient Health Questionnaire somatic symptom severity scale-15.
PCS: physical component score of SF-12; MCS: mental component score of SF-12
PHQ-9: Patient Health Questionnaire-9; GAD-7: Generalized Anxiety Disorder Scale-7.
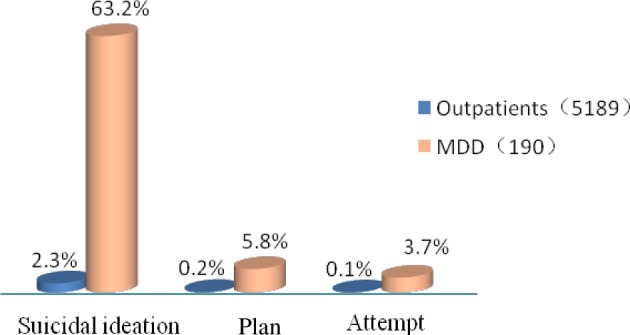
Suicidality was evaluated by suicide risk score on the MINI module B, with 2.3% of participants (120) reporting suicidal ideation within the past month and thus passing the screening phase. 0.2% (11) reported a suicide plan, and 0.1% (7) reported at least one prior suicide attempt; these are not mutually exclusive categories. Among the participants reporting suicidal ideation group, 55.8% had a current prevalence of MDD; conversely, of the proportion of the sample reporting current MDD symptoms, 63.2% reported suicidal ideation, 5.8% a suicide plan, and 3.7% at least one prior suicide attempt (see Fig 2).
Fig 2. The proportion of suicidal ideation, plan and attempt in all subjects and MDD.
3.2 Related factors associated with MDD and suicidality
Table 2 contains the results of bivariate correlation analysis of participant characteristics with either MDD or suicidality. We found 11 factors to be tentatively associated with current MDD based on preliminary bivariate analyses. Patients with current MDD were more likely to be women, younger, unmarried. They were also more likely to report hopelessness, anxiety, insomnia, and physical complaints with a corresponding poor PCS and MCS. Living condition had statistic difference (χ2 = 7.309, p = 0.026), but no significant difference between groups. There existed 14 factors associated with suicide risk. Patients with suicidality were more likely to be women, younger, unmarried, and to live alone and live in a nursing home or dormitory. They were also more likely to report depressed mood, anxiety, insomnia, and physical complaints with corresponding poor PCS and MCS. Both the suicidal group and MDD group were more likely to have comorbid psychiatric diagnoses. There was statistic difference in educational attainment (χ2 = 6.868, p = 0.032), but no significant difference between groups. However, no group differed based on smoking rates, alcohol use, income, occupation, or whether they lived in urban or rural areas. Using the Chi-square test for differences in groups based on marital status, living condition, and educational attainment. In MDD, Never married was significantly different compared to the married (χ2 = 10.193, p = 0.001). In suicide, Never married had significant difference, compared to the married (χ2 = 13.060, p<0.001); both living alone and living in a nursing home or dormitory were significantly different, compared to live with families (χ2 = 10.382, p = 0.001; χ2 = 7.211, p = 0.007). There were no significant differences between the other groups.
Table 2. Demographic and clinical characteristics of subjects according to major depressive disorder and suicide risk (N = 5189).
|
Characteristics |
MDD | Non-MDD | χ2 | Suicidality | Non-suicidality |
p-value |
||
|---|---|---|---|---|---|---|---|---|
| N = 190 | N = 4999 | p-value | N = 120 | N = 5069 | χ2 | |||
| n(%) | n(%) | n(%) | n(%) | |||||
| Sex | 5.642 | 0.019 | 19.809 | <0.001 | ||||
| Female | 141(4.1) | 3294(95.9) | 103(3.0) | 3332(97.0) | ||||
| Male | 49(2.8) | 1704(97.2) | 18(1.0%) | 1735(99.0) | ||||
| Education | 1.004 | 0.605 | 6.868 | 0.032 | ||||
| Illiterate or primary school | 31(3.1) | 961(96.9) | 16(1.6) | 976(98.4) | ||||
| Junior and senior high school | 94(3.8) | 2396(96.2) | 72(2.9) | 2418(97.1) | ||||
| College and above(≥13) | 65(3.8) | 1642(96.3) | 33(1.9) | 1674(98.1) | ||||
| Marital status | 13.342 | 0.001 | 13.076 | 0.001 | ||||
| Never married | 44(5.5) | 763(94.5) | 33(4.1) | 774(95.9) | ||||
| Married | 131(3.2) | 3991(96.8) | 82(2.0) | 4040(98.0) | ||||
| Other(divorce/widowed) | 15(5.8) | 245(94.2) | 6(2.3) | 254(97.7) | ||||
| Living condition | 7.309 | 0.026 | 15.144 | 0.001 | ||||
| Alone | 25(5.3) | 443(94.7) | 20(4.3) | 448(95.7) | ||||
| Live with families | 146(3.4) | 4208(96.6) | 86(2.0) | 4268(98.0) | ||||
| Other a | 19(5.2) | 348(94.8) | 15(4.1) | 352(95.9) | ||||
| PCS | 9.765 | 0.002 | 11.009 | 0.001 | ||||
| High(>39) | 38(2.4) | 1530(97.6) | 20(1.3) | 1548(98.7) | ||||
| Low(≤39) | 152(4.2) | 3469(95.8) | 101(2.8) | 3520(97.2) | ||||
| MCS | 82.020 | <0.001 | 44.816 | <0.001 | ||||
| High(>47) | 43(1.5) | 2797(98.5) | 30(1.1) | 2810(98.9) | ||||
| Low(≤47) | 147(6.3) | 2202(93.7) | 91(3.9) | 2258(96.1) | ||||
| Smoking(yes) | 18(3.1) | 566(96.9) | 1.219 | 0.303 | 11(1.9) | 573(98.1) | 0.810 | 0.368 |
| Drinking(yes) | 35(3.6) | 935(96.4) | 0.404 | 0.525 | 21(2.2) | 949(97.8) | 0.355 | 0.551 |
| Any insomnia(yes) | 99(10.1) | 880(89.9) | 142.344 | <0.001 | 60(6.1) | 919(93.9) | 76.379 | <0.001 |
| Anxiety disorders(yes) | 82(47.1) | 92(52.9) | 964.204 | <0.001 | 62(35.6) | 112(64.4) | 876.606 | <0.001 |
| Suicidal ideation(yes) | 67(55.4) | 54(44.6) | 939.112 | <0.001 | - | - | - | - |
| Bipolar disorders(yes) | - | - | - | - | 20(23.5) | 65(76.5) | 170.494 | <0.001 |
| Major depressive disorder(yes) | - | - | - | - | 67(35.3) | 123(64.7) | 939.112 | <0.001 |
| ±s | ±s | t | p-value | ±s | ±s | t | p-value | |
| Age(years) | 38.1±12.97 | 38.1±12.97 | -3.476 | 0.001 | 35.9±11.7 | 42.2±16.0 | -4.318 | <0.001 |
| PHQ-9 total scores | - | - | - | - | 13.0±5.9 | 3.4±4.0 | 25.877 | <0.001 |
| GAD-7 total scores | 10.9±5.8 | 2.9±3.9 | 27.245 | <0.001 | 11.3±5.8 | 3.0±4.0 | 22.285 | <0.001 |
| PHQ-15 total scores | 11.7±5.3 | 5.3±4.2 | 19.962 | <0.001 | 12.7±5.7 | 5.4±4.2 | 17.960 | <0.001 |
a Other (living in a nursing home or dormitory).
PHQ-9: Patient Health Questionnaire-9; GAD-7: Generalized Anxiety Disorder Scale-7
PCS: physical component score of SF-12; MCS: mental component score of SF-12
PHQ-15: Patient Health Questionnaire somatic symptom severity scale-15.
3.3 Binary logistic regression analysis
Table 3 reports the results of the logistic regression model for MDD. Significant risk factors were: GAD-7 total score (OR = 1.14 95% CI: 1.10–1.18), PHQ-15 total scores (OR = 1.07 95% CI: 1.03–1.11), insomnia (OR = 2.03 95% CI: 1.39–2.97), suicidal ideation (OR = 7.50 95% CI: 4.50–12.48), and the presence of an anxiety disorder (OR = 5.04 95% CI: 3.21–7.93). A high MCS score, reflective of quality of life in the mental realm, was protective against MDD (OR = 0.49 95% CI: 0.33–0.74). Another 5 factors were significantly different in bivariate analyses, however, were not entered into regression model, including age, sex, marital, living alone, and poor PCS.
Table 3. Logistic regression results for factors associated with major depressive disorder and suicide risk.
|
Variable |
Major depressive disorder | |||
| OR | 95%CI | p-value | ||
| Anxiety disorders(Yes vs. No) | 5.0 | 3.2–7.9 | <0.001 | |
| Insomnia(Yes vs. No) | 2.0 | 1.4–3.0 | <0.001 | |
| MCS(High vs. Low) | 0.5 | 0.3–0.7 | 0.001 | |
| Suicidal ideation (Yes vs. No) | 7.5 | 4.5–12.5 | <0.001 | |
| PHQ-15 total scores | 1.1 | 1.0–1.1 | <0.001 | |
| GAD-7 total scores | 1.1 | 1.1–1.2 | <0.001 | |
| Suicide risk | ||||
| OR | 95%CI | p-value | ||
| Sex(Female vs. Male) | 2.6 | 1.5–4.8 | 0.001 | |
| Major depressive disorder(Yes vs. No) | 11.9 | 6.6–21.5 | <0.001 | |
| Anxiety disorders(Yes vs. No) | 4.4 | 2.5–7.6 | <0.001 | |
| Bipolar disorders(Yes vs. No) | 7.9 | 3.7–16.9 | <0.001 | |
| PHQ-9 total scores | 1.2 | 1.1–1.2 | <0.001 | |
| Education(vs. College and above(≥13) | 0.005 | |||
| Illiterate or primary school(0–6) | 1.3 | 0.6–2.8 | 0.506 | |
| Junior and senior high school(7–12) | 2.3 | 1.4–3.9 | 0.002 | |
| Living condition(vs. Live with families) | 0.005 | |||
| Alone | 2.6 | 1.4–4.9 | 0.002 | |
| Others a | 1.9 | 0.9–3.9 | 0.095 | |
a Other (living in a nursing home or dormitory).
GAD-7: Generalized Anxiety Disorder Scale-7
PHQ-15: Patient Health Questionnaire somatic symptom severity scale-15.
PHQ-9: Patient Health Questionnaire-9; MCS: mental component score of SF-12
Table 3 also reports the results of the logistic regression model for suicidality. A diagnosis of MDD (OR = 11.91 95% CI: 6.60–21.49), anxiety disorder (OR = 4.39 95% CI: 2.53–7.61) and bipolar disorder (OR = 7.94 95% CI 3.74–16.85) were significant risk factors. In addition, PHQ-9 total score was significant risk factor (OR = 1.16 95% CI: 1.12–1.20). Three sociodemographic factors also proved significant: being female (OR = 2.62 95% CI: 1.45–4.76), having medium educational attainment (7–12 years: OR = 2.31 95% CI: 1.36–3.91), and living alone (OR = 2.61 95% CI: 1.40–4.85). Another 7 factors proved not to be significant in the logistic regression model, including age, marital, insomnia, poor PCS & MCS, and PHQ-15 scores.
3.4 The secondary logistic regression analysis
Furthermore, a secondary analysis was performed using the logistic regression model for the risk of suicidality in patients diagnosed with MDD. Significant risk factors in Table 4 were: female (OR = 2.28 95% CI: 0.97–6.54), anxiety disorder (OR = 2.24 95% CI: 1.17–4.28), other (living in a nursing home or dormitory; OR = 3.45 95% CI: 1.18–10.14), and high PCS that was protective against MDD (OR = 0.23 95% CI: 0.09–0.62).
Table 4. The secondary logistic regression results for factors associated with suicide risk.
|
Variable |
With major depressive disorder | |||
| OR | 95%CI | p-value | ||
| Sex(Female vs. Male) | 2.3 | 1.0–5.1 | 0.042 | |
| Anxiety disorders(Yes vs. No) | 2.2 | 1.2–4.3 | 0.015 | |
| PCS(High vs. Low) | 0.2 | 0.1–0.6 | 0.004 | |
| Living condition(vs. Live with families) | 0.027 | |||
| Alone | 2.5 | 1.0–6.5 | 0.057 | |
| Others a | 3.5 | 1.2–10.1 | 0.024 | |
| Without major depressive disorder | ||||
| OR | 95%CI | p-value | ||
| Sex(Female vs. Male) | 4.0 | 1.6–9.9 | 0.003 | |
| Anxiety disorders(Yes vs. No) | 8.5 | 3.8–19.0 | <0.001 | |
| Bipolar disorders(Yes vs. No) | 4.4 | 1.9–10.2 | <0.001 | |
| GAD-7 total scores | 1.2 | 1.1–1.2 | <0.001 | |
| PHQ-15 total scores | 1.1 | 1.0–1.2 | 0.004 | |
| Living condition(vs. Live with families) | 0.041 | |||
| Alone | 2.9 | 1.3–6.6 | 0.012 | |
| Others a | 1.4 | 0.5–4.1 | 0.557 | |
a Other (living in a nursing home or dormitory).
PHQ-15: Patient Health Questionnaire somatic symptom severity scale-15.
PCS: physical component score of SF-12; GAD-7: Generalized Anxiety Disorder Scale-7
Table 4 also performed using the logistic regression model for the risk of suicidality in patients who did not receive a diagnosis of MDD. Significant risk factors were: Sex (OR = 3.97 95% CI: 1.60–9.87), living alone(OR = 2.89 95% CI: 1.27–6.57), Anxiety disorders (OR = 8.45 95% CI: 3.76–18.99), Bipolar disorders (OR = 4.42 95% CI: 1.93–10.16), GAD-7 total scores (OR = 1.15 95% CI: 1.09–1.22) and PHQ-15 total scores (OR = 1.09 95% CI: 1.03–1.15).
4. Discussion
The global 12-month prevalence of MDD has recently been estimated at 4.7–6.7% [4,31]. Several recent epidemiological studies of mental disorders in China (1.2–8.6%), and a survey of 50 general hospital internal medicine clinics in China reported lower levels of MDD prevalence (3.95%) as compared to the global average [32]. Our study found a 3.7% current prevalence of MDD, which is in keeping with reported levels in. We did not evaluate lifetime prevalence; instead, we found a 2.3% past-month prevalence rate which is surprisingly high, given that this is equivalent to the lifetime prevalence found in the aforementioned study in Beijing. Another study showed 4.8% of inpatients with suicidal ideation in past one month were higher than ours [33].
Our evaluation of the risk factors for MDD was consistent with literature both within China and globally: being female, being unmarried, and being younger [2,34]. Our report of significant risk factors for suicidality was in line with many other cross-national studies in China: being female, unmarried, living alone, being younger, not attaining college education [4,35,36]. A most recent Ethiopian study showed that women had 63% higher odds of endorsing suicidal risk than men at general hospital (OR = 1.63 95%CI: 1.13–2.36) [9]. The Hong Kong survey also showed that female gender was associated with a higher risk of suicidal ideation [37]. The Chinese national reports on suicide showed a strong reversal of the international trend: in those younger than 60 years, female rates exceed male rates by an average of 26% [8]. While women also reported significantly higher rates of MDD than men in our study, this is consistent both within China and globally, and does not explain the difference in suicidality. Women may report MDD more commonly than men for multiple reasons: social inequality and oppression, higher rates of sexual and physical abuse, higher healthcare utilization and willingness to report symptoms, and the presence of female-specific affective disorders due to fluctuation in estrogen and progesterone levels such as premenstrual dysphoric disorder [8,38,39].
MDD is well-known as a primary risk factor for suicidality, and this was borne out in our study (OR = 11.91; 95% CI: 6.60–21.49). The prevalence of suicidal ideation among our participants with MDD (55.4%) was consistent with the literature, which reports rates from 47% to 69% [40,41]. A nationwide study showed that 15% of 0.5 million Chinese adults with major depressive episode had suicidal ideation [11]. Hopelessness is another major risk factor for suicidality, as described by Britton et al.; we found that 89.2% of patients reporting suicidality also reported hopelessness and this was significantly more common than patients without suicidility [42]. There is a sequence of suicidality; as the situation persists, a person moves from suicidal ideation, to developing a plan, and then to attempting suicide within the first year after onset of suicidal ideation [10]. There is a limited window in which to prevent this outcome; this fact encourages the employment of more sensitive and more rigorous screening and more intense intervention in order to reduce suffering and death. This is particularly true within China, where rates of utilization of psychiatric services for suicidal ideation are low. One study found that, in Beijing, 36.2% of suicidal subjects sought medical help for their suicidality, and only 20.7% consulted a psychiatrist [43].
Anxiety and depression are commonly comorbid and may represent different facets of a single underlying mental phenomena; they are more commonly comorbid than separate [44]. Anxiety in the context of MDD increases the likelihood of suicidal ideation [45]. This has been demonstrated in Chinese patients as well [46]. Indeed, anxiety has been found as an independent risk factor for suicidal ideation and suicide attempts [47]. Our study corroborates this; the presence of anxiety in patients with MDD was a significant risk factor for suicidality (OR = 2.24 95% CI: 1.17–4.28), as well as in all patients reporting suicidality (OR = 4.39 95% CI: 2.53–7.61).
The secondary logistic regression analysis suggested us that one patient with MDD had some characteristics such as female, living in a nursing home or dormitory, and combine anxiety disorders, so they will increase her suicide risk. When we see the patients without MDD in general hospitals, however, they are female and live alone, self-report anxious mood and somatic complaints, getting anxiety disorders and bipolar disorders, we should be alert her who are more likely to have suicide risk.
5. Limitations
The major strengths of our study were the large sample size, the use of reliable and cross-validated clinical diagnostic assessments, and the significant results it produced. However, there are several limitations to this study. First, because it is cross-sectional, no causality can be assumed between the significant risk factors and MDD or suicidality. Second, because all data was reliant upon self-report, it is subject to recall bias, response bias, and a desire for non-disclosure because of the sensitive nature of the material at hand. Third, the clinical context of non-psychiatric outpatient clinics within urban general hospitals may have induced some selection bias, and limits generalizability to the broader Chinese population. However, the results of this study are in keeping with the scientific literature on this subject, and provide ample data to enhance the understanding of the epidemiology of these disorders.
6. Conclusions
Our results demonstrate that MDD and suicidality are both common among adult outpatients with somatic complaints. Chinese-specific risk factors for suicide were verified and expounded upon, with women who are unmarried, of higher education, living alone, self-report depression or anxiety, and have psychiatric diagnoses being at much greater risk of suicidal ideation. Significant risk factors for MDD were also detailed, such as comorbid anxiety, self-reported anxiety, insomnia, suicidal ideation. Given the low utilization of psychiatric services in China, our data provides a strong impetus for non-psychiatric clinicians consulting a patient with somatic complaints to screen for, elaborate upon, and treat or refer depression and suicidality to a psychiatrist. Improving health may resolve depression in some patients, but others may require appropriate referral and direct psychiatric care [48]. Our data also displays the need for strengthening mental health promotion, anti-stigma campaigns, prevention programs, public education about the availability of treatment for depression, anxiety, and suicidality, and early intervention at populations at high risk of MDD and suicide [8].
Supporting information
(DOCX)
(DOC)
(SAV)
Flowchart of the study on prevalence of major depressive disorders and suicide risk from general hospitals in Guangzhou.
(TIF)
(TIF)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(PDF)
(DOCX)
(DOC)
Acknowledgments
It was conducted in and supported by these participating hospitals (The First Affiliated Hospital of Guangzhou University of Traditional Chinese Medicine, Guangzhou Panyu Central Hospital, Southern Medical University, The Third Affiliated Hospital of Sun Yet-Sen University). The authors would also like to thank Bin Sun and Prof. Robert A. Rosenheck.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This study was funded through National Key Research and Development Plan "Precision Medical Research" 2016 Project (2016YFC0906302) to YPN; Guangzhou Medical and Health Science and Technology Major Projects (20151A031003) to YPN; the National Science and Technologic Program of China(2015BAI13B02) to YPN. The funders had a role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.World Health Organization (WHO) WOoNC. (2016) Available at:http://wwwwhoint/mediacentre/factsheets/fs369/en/.
- 2.Kessler RC, Bromet EJ. (2013) The epidemiology of depression across cultures. Annu Rev Public Health 34: 119–138. https://doi.org/.10.1146/annurev-publhealth-031912-114409 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Whiteford HA, Degenhardt L, Rehm J, Baxter AJ, Ferrari AJ, Erskine HE, et al. (2013) Global burden of disease attributable to mental and substance use disorders: findings from the Global Burden of Disease Study 2010. Lancet 382: 1575–1586. doi: 10.1016/S0140-6736(13)61611-6 . [DOI] [PubMed] [Google Scholar]
- 4.Nock MK, Borges G, Bromet EJ, Cha CB, Kessler RC, Lee S. (2008) Suicide and suicidal behavior. Epidemiol Rev 30: 133–154. https://doi.org/.10.1093/epirev/mxn002 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.(WHO) WHO. (2014) Preventing Suicide:a Global Imperative. Available at: http://wwwwhoint/mental_health/suicide-prevention/en/.
- 6.Phillips MR, Li X, Zhang Y. (2002) Suicide rates in China, 1995–99. Lancet 359: 835–840. doi: 10.1016/S0140-6736(02)07954-0 . [DOI] [PubMed] [Google Scholar]
- 7.Agarwal A, Sharma R, Harlev A, Esteves SC. (2016) Effect of varicocele on semen characteristics according to the new 2010 World Health Organization criteria: a systematic review and meta-analysis. Asian J Androl 18: 163–170. https://doi.org/.10.4103/1008-682X.172638 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Law S, Liu P. (2008) Suicide in China: unique demographic patterns and relationship to depressive disorder. Curr Psychiatry Rep 10: 80–86. . [DOI] [PubMed] [Google Scholar]
- 9.Whittier AB, Gelaye B, Deyessa N, Bahretibeb Y, Kelkile TS, Berhane Y, et al. (2016) Major depressive disorder and suicidal behavior among urban dwelling Ethiopian adult outpatients at a general hospital. J Affect Disord 197: 58–65. https://doi.org/.10.1016/j.jad.2016.02.052 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kessler RC, Borges G, Walters EE. (1999) Prevalence of and risk factors for lifetime suicide attempts in the National Comorbidity Survey. Arch Gen Psychiatry 56: 617–626. . [DOI] [PubMed] [Google Scholar]
- 11.Chen Y, Bennett D, Clarke R, Guo Y, Yu C, Bian Z, et al. (2017) Patterns and correlates of major depression in Chinese adults: a cross-sectional study of 0.5 million men and women. Psychol Med 47: 958–970. https://doi.org/.10.1017/S0033291716002889 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sartorius N, Ustun TB, Lecrubier Y, Wittchen HU. (1996) Depression comorbid with anxiety: results from the WHO study on psychological disorders in primary health care. Br J Psychiatry Suppl: 38–43. . [PubMed] [Google Scholar]
- 13.Ayuso-Mateos JL, Vazquez-Barquero JL, Dowrick C, Lehtinen V, Dalgard OS, Casey P, et al. (2001) Depressive disorders in Europe: prevalence figures from the ODIN study. Br J Psychiatry 179: 308–316. . [DOI] [PubMed] [Google Scholar]
- 14.Siu AL, Force USPST, Bibbins-Domingo K, Grossman DC, Baumann LC, Davidson KW, et al. (2016) Screening for Depression in Adults: US Preventive Services Task Force Recommendation Statement. JAMA 315: 380–387. https://doi.org/.10.1001/jama.2015.18392 . [DOI] [PubMed] [Google Scholar]
- 15.Duhoux A, Fournier L, Gauvin L, Roberge P. (2013) What is the association between quality of treatment for depression and patient outcomes? A cohort study of adults consulting in primary care. J Affect Disord 151: 265–274. https://doi.org/.10.1016/j.jad.2013.05.097 . [DOI] [PubMed] [Google Scholar]
- 16.Katon WJ. (2011) Epidemiology and treatment of depression in patients with chronic medical illness. Dialogues Clin Neurosci 13: 7–23. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Olver JS, Hopwood MJ. (2013) Depression and physical illness. Med J Aust 199: S9–12. . [DOI] [PubMed] [Google Scholar]
- 18.Webb RT, Kontopantelis E, Doran T, Qin P, Creed F, Kapur N. (2012) Suicide risk in primary care patients with major physical diseases: a case-control study. Arch Gen Psychiatry 69: 256–264. https://doi.org/.10.1001/archgenpsychiatry.2011.1561 . [DOI] [PubMed] [Google Scholar]
- 19.Qin P, Webb R, Kapur N, Sorensen HT. (2013) Hospitalization for physical illness and risk of subsequent suicide: a population study. J Intern Med 273: 48–58. https://doi.org/.10.1111/j.1365-2796.2012.02572.x . [DOI] [PubMed] [Google Scholar]
- 20.Kroenke K, Spitzer RL, Williams JB. (2001) The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med 16: 606–613. doi: 10.1046/j.1525-1497.2001.016009606.x . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chen S, Chiu H, Xu B, Ma Y, Jin T, Wu M, et al. (2010) Reliability and validity of the PHQ-9 for screening late-life depression in Chinese primary care. Int J Geriatr Psychiatry 25: 1127–1133. https://doi.org/.10.1002/gps.2442 . [DOI] [PubMed] [Google Scholar]
- 22.Spitzer RL, Kroenke K, Williams JB, Lowe B. (2006) A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med 166: 1092–1097. https://doi.org/.10.1001/archinte.166.10.1092 . [DOI] [PubMed] [Google Scholar]
- 23.Tong X, An D, McGonigal A, Park SP, Zhou D. (2016) Validation of the Generalized Anxiety Disorder-7 (GAD-7) among Chinese people with epilepsy. Epilepsy Res 120: 31–36. https://doi.org/.10.1016/j.eplepsyres.2015.11.019 . [DOI] [PubMed] [Google Scholar]
- 24.Kroenke K, Spitzer RL, Williams JB. (2002) The PHQ-15: validity of a new measure for evaluating the severity of somatic symptoms. Psychosom Med 64: 258–266. . [DOI] [PubMed] [Google Scholar]
- 25.Zhang L, Fritzsche K, Liu Y, Wang J, Huang M, Wang Y, et al. (2016) Validation of the Chinese version of the PHQ-15 in a tertiary hospital. BMC Psychiatry 16: 89 https://doi.org/.10.1186/s12888-016-0798-5 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jenkinson C, Layte R. (1997) Development and testing of the UK SF-12 (short form health survey). J Health Serv Res Policy 2: 14–18. . [DOI] [PubMed] [Google Scholar]
- 27.Lam CL, Tse EY, Gandek B. (2005) Is the standard SF-12 health survey valid and equivalent for a Chinese population? Qual Life Res 14: 539–547. . [DOI] [PubMed] [Google Scholar]
- 28.Liu X, Uchiyama M, Okawa M, Kurita H. (2000) Prevalence and correlates of self-reported sleep problems among Chinese adolescents. Sleep 23: 27–34. . [PubMed] [Google Scholar]
- 29.Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, et al. (1998) The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry 59 Suppl 20: 22–33;quiz 34–57. . [PubMed] [Google Scholar]
- 30.Si Tian-Mei SL, Wei-Min Dang, Yun-Ai Se, Jing-Xu Chen, Wen-Tian Dong. (2009) Evaluation of the Reliability and Validity of Chinese Version of the Mini-international Neuropsychiatric Interview in Patients with Mental Disorders. Chinese Mental Health Journal (in Chinese) 23: 493–497. https://doi.org/.10.3969/j.issn.1000-6729.2009.07.011. [Google Scholar]
- 31.Ferrari AJ, Charlson FJ, Norman RE, Flaxman AD, Patten SB, Vos T, et al. (2013) The epidemiological modelling of major depressive disorder: application for the Global Burden of Disease Study 2010. PLoS One 8: e69637 https://doi.org/.10.1371/journal.pone.0069637 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Li X.Y. ZYP, Wang Z.Q., Yang S.J., Michael R., Phillips. (2010) Prevalence of depressive disorders among patients treated in general hospitals in Beijing. Chinese Journal of Nervous and Mental Diseases (in Chinese) 36(2): 65–69. https://doi.org/.10.3969/j.issn.1002-0152.2010.02.001. [Google Scholar]
- 33.Chan WS, Law CK, Liu KY, Wong PW, Law YW, Yip PS. (2009) Suicidality in Chinese adolescents in Hong Kong: the role of family and cultural influences. Soc Psychiatry Psychiatr Epidemiol 44: 278–284. https://doi.org/.10.1007/s00127-008-0434-x . [DOI] [PubMed] [Google Scholar]
- 34.Wang J, Williams J, Lavorato D, Schmitz N, Dewa C, Patten SB. (2010) The incidence of major depression in Canada: the National Population Health Survey. J Affect Disord 123: 158–163. https://doi.org/.10.1016/j.jad.2009.07.016 . [DOI] [PubMed] [Google Scholar]
- 35.Liu KY, Chen EY, Chan CL, Lee DT, Law YW, Conwell Y, et al. (2006) Socio-economic and psychological correlates of suicidality among Hong Kong working-age adults: results from a population-based survey. Psychol Med 36: 1759–1767. https://doi.org/.10.1017/S0033291706009032 . [DOI] [PubMed] [Google Scholar]
- 36.Ribeiro JD, Franklin JC, Fox KR, Bentley KH, Kleiman EM, Chang BP, et al. (2016) Self-injurious thoughts and behaviors as risk factors for future suicide ideation, attempts, and death: a meta-analysis of longitudinal studies. Psychol Med 46: 225–236. https://doi.org/.10.1017/S0033291715001804 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cheung YB, Law CK, Chan B, Liu KY, Yip PS. (2006) Suicidal ideation and suicidal attempts in a population-based study of Chinese people: risk attributable to hopelessness, depression, and social factors. J Affect Disord 90: 193–199. https://doi.org/.10.1016/j.jad.2005.11.018 . [DOI] [PubMed] [Google Scholar]
- 38.Seeman MV. (1997) Psychopathology in women and men: focus on female hormones. Am J Psychiatry 154: 1641–1647. https://doi.org/.10.1176/ajp.154.12.1641 . [DOI] [PubMed] [Google Scholar]
- 39.Cyranowski JM, Frank E, Young E, Shear MK. (2000) Adolescent onset of the gender difference in lifetime rates of major depression: a theoretical model. Arch Gen Psychiatry 57: 21–27. . [DOI] [PubMed] [Google Scholar]
- 40.Asnis GM, Friedman TA, Sanderson WC, Kaplan ML, van Praag HM, Harkavy-Friedman JM. (1993) Suicidal behaviors in adult psychiatric outpatients, I: Description and prevalence. Am J Psychiatry 150: 108–112. https://doi.org/.10.1176/ajp.150.1.108 . [DOI] [PubMed] [Google Scholar]
- 41.Sokero TP, Melartin TK, Rytsala HJ, Leskela US, Lestela-Mielonen PS, Isometsa ET. (2003) Suicidal ideation and attempts among psychiatric patients with major depressive disorder. J Clin Psychiatry 64: 1094–1100. . [DOI] [PubMed] [Google Scholar]
- 42.Britton PC, Duberstein PR, Conner KR, Heisel MJ, Hirsch JK, Conwell Y. (2008) Reasons for living, hopelessness, and suicide ideation among depressed adults 50 years or older. Am J Geriatr Psychiatry 16: 736–741. https://doi.org/.10.1097/JGP.0b013e31817b609a . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ma X, Xiang YT, Cai ZJ, Li SR, Xiang YQ, Guo HL, et al. (2009) Lifetime prevalence of suicidal ideation, suicide plans and attempts in rural and urban regions of Beijing, China. Aust N Z J Psychiatry 43: 158–166. https://doi.org/.10.1080/00048670802607170 . [DOI] [PubMed] [Google Scholar]
- 44.Baldwin DS, Evans DL, Hirschfeld RM, Kasper S. (2002) Can we distinguish anxiety from depression? Psychopharmacol Bull 36 Suppl 2: 158–165. . [PubMed] [Google Scholar]
- 45.Fava M, Rush AJ, Alpert JE, Carmin CN, Balasubramani GK, Wisniewski SR, et al. (2006) What clinical and symptom features and comorbid disorders characterize outpatients with anxious major depressive disorder: a replication and extension. Can J Psychiatry 51: 823–835. https://doi.org/.10.1177/070674370605101304 . [DOI] [PubMed] [Google Scholar]
- 46.Cohen AD, Ofek-Shlomai A, Vardy DA, Weiner Z, Shvartzman P. (2006) Depression in dermatological patients identified by the Mini International Neuropsychiatric Interview questionnaire. J Am Acad Dermatol 54: 94–99. https://doi.org/.10.1016/j.jaad.2005.09.019 . [DOI] [PubMed] [Google Scholar]
- 47.Eikelenboom M, Smit JH, Beekman AT, Penninx BW. (2012) Do depression and anxiety converge or diverge in their association with suicidality? J Psychiatr Res 46: 608–615. https://doi.org/.10.1016/j.jpsychires.2012.01.025 . [DOI] [PubMed] [Google Scholar]
- 48.Cigognini MA, Furlanetto LM. (2006) Diagnosis and pharmacological treatment of depressive disorders in a general hospital. Rev Bras Psiquiatr 28: 97–103. https://doi.org/./S1516-44462006000200005 . [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
(DOC)
(SAV)
Flowchart of the study on prevalence of major depressive disorders and suicide risk from general hospitals in Guangzhou.
(TIF)
(TIF)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(PDF)
(DOCX)
(DOC)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.



