Abstract
.
Keywords: Premature ventricular complexes, Atrioventricular block
1. Case presentation
A 46-year-old man with no significant medical history or personal history of syncope was seen in clinic for palpitations. A 12-lead electrocardiogram (ECG) at rest showed sinus rhythm with four premature ventricular complexes (PVCs) (Fig. 1). His exercise stress echocardiography was negative for ischemia at 13 metabolic equivalents of task (METs), with a normal ejection fraction of 60%, no regional wall motion abnormalities, and normal valves. PVCs were suppressed during peak stress. He also underwent a 24-h Holter that showed frequent PVCs, mainly bigeminy and couplets, with a PVC burden of 19%.
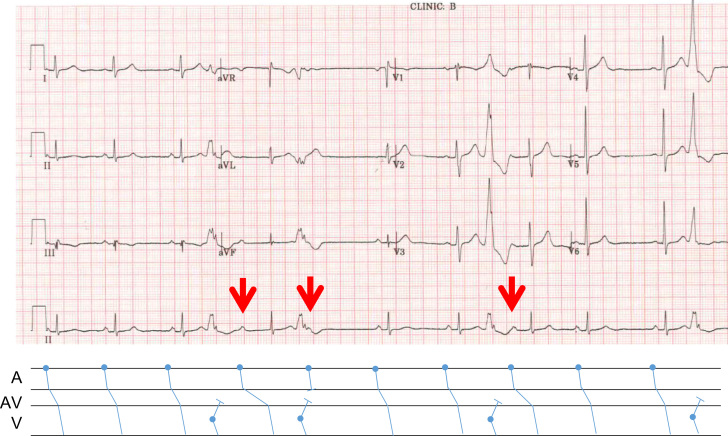
Fig. 1.
ECG of the patient at rest with corresponding ladder diagram.
2. Comments
An interpolated PVC is one that occurs between two sinus beats without a compensatory pause, where the P-P interval remains approximately constant.
Fig. 1 shows an interesting observation where the third sinus beat was followed by an interpolated PVC, after which the PR interval of the subsequent sinus beat was prolonged (first red arrow). A second interpolated PVC was observed, followed by a non-conducted sinus beat (second red arrow). After the dropped beat, two sinus beats were conducted with normal PR intervals. The earlier conduction pattern was then repeated with a third interpolated PVC preceding another sinus beat with a prolonged PR interval (third red arrow). The ECG ended with yet another PVC.
At this point, possible considerations for the arrhythmia may include 1) concealed conduction; 2) second degree atrioventricular (AV) nodal block of the Wenckebach type; 3) infranodal block; or 4) intermittent atrioventricular dissociation.
Concealed conduction occurs when electrical stimulation of cardiac tissue occurs without a direct manifestation of effects on ECG, hence the term “concealed”. However, conduction characteristics may be altered and this may become apparent upon observing subsequent conduction patterns [1], [2], as in this example.
In the ECG above, an interpolated PVC was retrogradely conducted to the AV node (AVN) but was not able to completely penetrate it. This “concealed” conduction increased the refractoriness of the AVN, causing a subsequent AV nodal conduction delay. This is evident in the post-PVC sinus beat (first red arrow), where delayed conduction through the incompletely recovered AVN resulted in prolongation of the PR interval. This is not a second-degree AV nodal block of the Wenckebach type.
Interestingly, when a second interpolated, retrogradely conducted PVC in succession perturbed the first post-PVC sinus beat, a non-conducted sinus beat was observed (second red arrow). The observation can be explained by the further increased refractoriness of the AVN due to concealed conduction, such that the P wave was unable to conduct through the AVN at all, resulting in a dropped beat. This is elucidated in the ladder diagram. The non-conducted P wave hidden within the terminal portion of the PVC (second red arrow) originated from the sinus node, as suggested by its positivity in lead II and also by its timing, given that an approximately constant P-P interval is expected. It was not a retrogradely conducted atrial beat secondary to the preceding PVC.
The AVN then recovered and two subsequent sinus beats with normal PR intervals were observed. The phenomenon was repeated with concealed conduction of a third interpolated PVC and resultant prolongation of the post-PVC sinus beat (third red arrow). The level of the block is at the AVN rather than an infranodal block.
Interestingly, the PR interval of the beat corresponding to the first red arrow measured about 440 milliseconds, approximately 160 milliseconds longer than the PR interval of the beat corresponding to the third red arrow (280 milliseconds). On closer inspection, it is revealed that the P-P intervals are variable. Specifically, the P-P interval preceding the first interpolated PVC is 880 ms, while that preceding the third interpolated PVC measures 1080 ms, which may be attributable to varying vagal tone. The coupling intervals of the interpolated PVCs are similar. It was also observed that the P wave immediately after the third interpolated PVC arrives earlier than the P wave following the first PVC, which should result in greater decrementation (i.e., a longer PR interval) when compared to the first; however, the converse was actually observed here.
The unexpectedly shorter PR interval in the third arrow beat can be explained by a lesser degree of AVN penetration by the retrogradely conducted PVC. Given that the P–P interval preceding the third interpolated PVC is longer, there could be a greater degree of infrahisian conduction delay and hence a “shallower” extent of penetration by the retrogradely conducted PVC with a correspondingly lesser extent of resultant AVN refractoriness compared to that caused by the first interpolated PVC [3]. The marked difference in PR intervals might also be explained by conduction down the slow pathway following the first PVC in the first red arrow beat, due to greater retrograde concealment resulting in an antegrade fast pathway block.
There is no convincing evidence of atrioventricular dissociation here. Rather, the observation is more consistent with concealed conduction resulting in AV nodal block.
This case study is presented here to showcase the manifestation of AV nodal block due to concealed conduction of interpolated PVCs, which is uncommonly observed on surface ECGs. Knowledge of the above concept will enable appropriate treatment to be implemented in patients. It would be inappropriate to hold off beta blockade if it is mistakenly thought that doing so would alleviate the AV nodal block. Conversely, beta blockade should be prescribed to suppress symptomatic PVCs. The patient above was treated with propranolol with relief of symptoms.
Conflicts of interest
All authors declare no conflict of interest related to this study.
Acknowledgements
Dr. Kelvin Wong provided the patient’s details and ECG. Both Dr. Kelvin Wong and Dr. Tan Vern Hsen proofread and edited the initial manuscript. We would like to thank Dr. Colin Yeo for providing technical advice on manuscript submission. We would also like to thank the Cardiology Department of Changi General Hospital for taking care of the above patient.
Contributor Information
Ying Zi Oh, Email: ohyingzi@gmail.com.
Vern Hsen Tan, Email: vern_hsen_tan@cgh.com.sg.
Kelvin CK Wong, Email: kelvin_wong@cgh.com.sg.
References
- 1.Langendorf R., Pick A. Concealed conduction. Further evaluation of a fundamental aspect of propagation of the cardiac impulse. Circulation. 1956;13:381–399. doi: 10.1161/01.cir.13.3.381. [DOI] [PubMed] [Google Scholar]
- 2.Ari H., Ari S., Koca V. Misleading ECG appearance of AV block due to concealed AV nodal conduction. Arch Turk Soc Cardiol. 2009;37:197–200. [PubMed] [Google Scholar]
- 3.Lehmann M.H., Mahmud R., Denker S. Retrograde concealed conduction in the atrioventricular node: differential manifestations related to level of intranodal penetration. Circulation. 1984;70:392–401. doi: 10.1161/01.cir.70.3.392. [DOI] [PubMed] [Google Scholar]