Abstract
Background
Despite decades of research and development, depression has risen from the 5th to the leading cause of disability in the U.S. Barriers to progress in the field are 1) Poor access to high quality care; 2) Limited mental health workforce; and 3) Few providers trained in the delivery of evidence-based treatments (EBTs). While mobile platforms are being developed to give consumers greater access to high quality care, too often these tools do not have empirical support for their effectiveness. In this study, we evaluated PRIME-D, a mobile app intervention that uses social networking, goal setting, and a mental health coach to deliver text-based, EBT’s to treat mood symptoms and functioning in adults with depression.
Methods
Thirty-six adults with depression remotely participated in PRIME-D over an 8-week period with a 4-week follow up, with 83% retained over the 12-week course of the study.
Results
On average, participants logged into the app 5 days/week. Depression scores (PHQ-9) significantly improved over time (over 50% reduction), with coach interactions enhancing these effects. Mood-related disability (SDS) also significantly decreased over time with participants no longer being impaired by their mood symptoms. Overall use of PRIME-D predicted greater gains in functioning. Improvements in mood and functioning were sustained over the 4-week follow-up.
Conclusions
Results suggest that PRIME-D is a feasible, acceptable, and effective intervention for adults with depression and that a mobile service delivery model may address the serious public health problem of poor access to high quality mental health care.
Keywords: Mobile app, Digital Health, Remote clinical trial, Pilot Study, Mental health coaching, Goal setting, Social networking
Introduction
Depression is one of the leading causes of disability and mortality around the world, resulting in significant personal, work place and health care costs (Lopez & Mathers, 2006; Papakostas & Ionescu, 2014). While there are many effective behavioral and pharmacological treatments available, many people do not have access to those treatments(Collins, Westra, Dozois, & Burns, 2004). Poor access to care is in part due to time demands that most traditional treatments place on consumers, the “bricks and mortar” delivery system, and the limited supply of treatment providers relative to those seeking care(Collins et al., 2004; Weil, 2015). Recent efforts to overcome poor access and to make care more efficient include using technology platforms to deliver evidence-based treatment (EBT), such as Internet-based and mobile app platforms. For instance, a recent systematic review of Internet-based, Cognitive Behavioral Therapy (CBT) treatments for depression found this method of care delivery overcomes access issues and improve outcomes to a similar degree as in-person care (Richards & Richardson, 2012). Delivering EBT’s, such as CBT for depression using online platforms, is a promising direction for the field and one that may help to improve access to care. Yet, while this is encouraging, an increasing number of individuals are opting for ownership of smartphone devices rather than laptop or desktop computers(Pew Research Center, 2013), thereby increasing the need for evidence-based mobile treatments. Further, using smartphones to deliver EBT’s may improve adherence and engagement by taking advantage of the convenience of on-the-go use as well as potentially optimize EBT’s by taking advantage of embedded sensors and other ecologically-valid information about individuals that may be used to inform more targeted care.
Although there is an emerging consensus that technology-based interventions for depression show great promise for improving mental health outcomes, existing mobile platforms developed by many commercial companies have not been adequately evaluated to determine their effectiveness(Donker et al., 2013; Huguet et al., 2016). Further, the degree to which these tools require guidance from a coach or treatment provider to optimize effectiveness and/or engagement is unclear. Many mobile platforms are entirely self-guided tools that require consumers to monitor their own symptoms and make use of suggestions to improve one’s mental health. Another approach is to provide users with a degree of human support, such as text-based interactions with coaches, to work with users to address their symptoms. For patients interested in these tools and for providers recommending these platforms, it is unclear what approach may be best suited for the individual. Yet, research on self-guided versus provider-supported Internet-based treatments suggests that human support significantly improves engagement by as much as 80% as well as leads to better outcomes(Andersson & Cuijpers, 2009; Mohr et al., 2013; Richards & Richardson, 2012). Further, treatments that include provider support lead to significantly more robust responses to treatment (d = 0.61) relative to those that are unsupported (d = 0.25) (Andersson & Cuijpers, 2009). While these findings suggest that including human support in technology-based interventions will lead to greater engagement and better outcomes, there is considerable variability in the qualifications of those delivering support (i.e. clinician, technician, research assistant), the modality it was given (i.e. phone, email, text, etc.), and “dose” (i.e. frequency, duration) of support offered in the various Internet-based treatments. As such, it is important that mobile health tools more explicitly define these features of support as well as examine the degree to which particular features and approaches may be tied to outcome of the treatments.
The purpose of this study was to evaluate the potential effectiveness of PRIME-D, a mobile app intervention that leverages EBT approaches, such as CBT and Behavioral Activation, to treat mood symptoms and functioning in adults with depression. We evaluated the feasibility, acceptability, and effectiveness of delivering PRIME-D entirely remotely with the support of a mental health coach, over an 8-week period with a 4-week follow up to 36 adults with depression. We hypothesized: 1) PRIME-D will be feasible and acceptable to adults with depression as measured by the degree of self-reported satisfaction, whether the app helped participants achieve their goals for using the app, retention rate, and use metrics; and 2) PRIME-D will significantly improve mood symptoms and functioning. We also hypothesized the degree to which different types of engagement in PRIME-D influence outcome: 3) The more active PRIME-D users were in the platform as well as the degree to which participants engaged with their assigned motivation coach will influence greater overall improvements in clinical outcome.
Methods
Procedures
Recruitment, Screening, and Consent
Participants were recruited online by posting ads in the volunteer and jobs sections of Craigslist. Ads were posted nationally over a period of three days and remained active for a week and a half. Potential participants were directed to a website (www.brightenstudy.com) explaining the study purpose and procedures. Interested participants completed an online brief screening consisting of questions about mobile device ownership. We used a combination of a written consent and custom videos posted on YouTube to explain the study. Participants were required to pass a quiz that tested their understanding that the study was voluntary and was not a substitute for treatment. Each question had to be answered correctly before moving on to baseline assessment and assignment to the intervention. Eligibility was established after consent was obtained. For more details about this remote recruitment approach, see Anguera and colleagues (Anguera, Jordan, Castaneda, Gazzaley, & Areán, 2016). Participants in this study were asked to use PRIME-D every day with a minimum frequency of 1x/week over an 8-week period. Participants were informed that they would not be paid for using the PRIME-D intervention, but that they would be paid in Amazon e-gift cards $5/week for completing the week 1,2,3 assessments and $10 each for week 4,8, and 12 assessments with a bonus of $30 for completing all assessments (Total possible compensation for completion of all assessments was = $75).
Participant Eligibility
Participants were required to speak English, be 18 years old or older, and own a smartphone with iOS operating system (i.e., iPhone) with Wi-Fi or 3G/4G capabilities (PRIME-D, the study app intervention, was only available in iOS at the time of the study launch). A Patient Health Questionnaire (PHQ-9; Spitzer, Kroenke, & Williams, 1999)) score of 5 or greater, or a score of 2 or greater on PHQ item10 (indicating that they felt disabled in their life because of their mood), was also required for enrollment.
Study Sample
Of the participants who completed the eligibility survey (n=140), 90 were disqualified (no smartphone n= 7; Android device n = 81; PHQ-9 score too low n=2), which left 50 eligible, of which 36 successfully installed the PRIME-D app, set up their profile, and started the study. Clinical and demographic characteristics for the 36 participants may be found in Table 1.
Table 1.
Demographic and clinical characteristics of the final sample
| N = 36 Mean (SD) |
|
|---|---|
|
| |
| Age (years) | 31.33 (12.4) |
|
| |
| Male/Female | 8/28 |
|
| |
| Highest Level of Educational Attainment | |
| Graduate | 16.7% |
| University | 38.9% |
| Community College | 22.2% |
| High School | 22.2% |
|
| |
| % Employed | 75% |
|
| |
| Income Level | |
| Less than $20,000 | 50.0% |
| $20,000 – $40,000 | 22.2% |
| $40,000 – $60,000 | 22.2% |
| Greater than $60,000 | 5.6% |
|
| |
| Marital Status (%) | |
| Single/Never Married | 52.8% |
| Married/Partnered | 36.0% |
| Divorced | 5.6% |
| Separated | 5.6% |
|
| |
| Racial Background (%) | |
| Caucasian | 61.1% |
| African American | 19.5% |
| Asian American | 8.3% |
| Other | 11.1% |
|
| |
| Ethnicity | |
| Non-Hispanic | 83.3% |
| Hispanic | 16.7% |
|
| |
| % Seeing therapist/social worker | 27.8% |
|
| |
| % Seeing psychiatrist | 27.8% |
|
| |
| % Taking medication | 30.6% |
|
| |
| PHQ-9 Total | 13.23 (4.4) |
|
| |
| SDS | |
| Work | 4.97 (2.1) |
| Social | 5.13 (2.3) |
| Family/Home | 4.30 (2.6) |
| Total | 14.40 (5.7) |
|
| |
| GAD-7 Total | 9.33 (4.8) |
PHQ-9 = Patient Health Questionnaire; SDS = Sheehan Disability Scale; GAD-7 = Generalized Anxiety Scale
Personalized Real-Time Intervention for Motivational Enhancement for Depression (PRIME-D)
Participants in this study installed PRIME-D on their personal smartphones, a mobile app intervention that was originally developed for individuals with recent-onset schizophrenia that focused on improving motivation and quality of life(Schlosser et al., 2016). Our team worked in collaboration with IDEO, a global design and innovation firm, to implement a human-centered design process to make the platform appealing to users and address their needs. PRIME-D includes all of the features of the originally designed PRIME platform, but was modified to include symptoms particularly relevant to individuals with depression and the community of “peers” only included individuals with depression. For more information about the PRIME design process and coach training, please see Schlosser et al., 2016(Schlosser et al., 2016).
With PRIME-D, participants join a supportive on-line environment where they can select and document progress on small, self-determined goals in the domains of health/wellness, social relationships, creativity, and productivity. PRIME-D provides users with motivation coaches; masters-level clinicians who use evidence-based interventions drawn from CBT, behavioral activation, mindfulness, and psychoeducation to help participants overcome the daily obstacles that hinder goal progress and improve health outcomes. Additionally, the PRIME-D community provides a platform for users to interact with one another. Users may send messages directly to each other and can also capture and share positive, spontaneous moments in their daily life with the whole PRIME-D community.
The first time participants signed in to the app, they were guided through a process of creating a user profile. Participants created a user name, uploaded a profile picture, selected their interests, goals, symptoms, and wrote a short bio. Once the user was registered to the app, an assigned motivation coach sent the new participant a welcome message and an offer to support the user in achieving his/her goals. The coach informed his/her assigned users that the coach would be messaging with them “most days” per week, but would modify the frequency depending on the user’s preference, clinical issues, and overall progress towards goal achievement. The coach to participant ratio was approximately 1:10 and coaches spent on average less than 2 hours/week (i.e. 20 minutes/participant per week) delivering text-based coaching to their participants.
Assessments
To assess the feasibility, acceptability, and impact of PRIME-D, we used a mixed-methods approach. We cross-validated learnings from data collected from gold-standard assessment tools, system analytics, and qualitative input.
Baseline
The baseline assessment was obtained from the study website (www.brightenstudy.com) and included the collection of demographics including age, race/ethnicity, martial and employment status, income, education, use of other health apps, and use of mental health services, including use of medications and psychotherapy. We collected information on mental health status using the Patient Health Questionnaire-9 (PHQ-9(Spitzer et al., 1999)) for depression, the Generalized Anxiety Disorder-7 (GAD-7(Löwe et al., 2008)), for generalized anxiety, and the Sheehan Disability Scale (SDS(Leon, Olfson, Portera, Farber, & Sheehan, 1997; Sheehan, Harnett-Sheehan, & Raj, 1996)), for mood-related disability. For the SDS, we examined functioning in the domains of work/school, social, and family life/home responsibilities.
Acceptability
We evaluated PRIME-D acceptability using a self-report satisfaction measure that was designed for the PRIME-D platform. Participants were surveyed about their satisfaction with the specific features of PRIME-D, such as the ability to interact with peers, coaches, and the different goal categories, on a 1 (not at all) to 10 (very much) scale and to provide optional qualitative feedback about the intervention. Participants were also surveyed on the extent to which PRIME-D helped them achieve their goals, and whether they would recommend PRIME-D to others. Participants answered these yes/no questions at the halfway point (4 weeks) and again at the end of the active phase of the trial (8 weeks). Retention in the trial was also used as a measure of acceptability.
Feasibility
To evaluate feasibility, we assessed the following use metrics: login frequency (average number of days logged in per week), average number of challenges completed (both overall and by individual challenge category), challenge completion percentage, and the average number of peer and coach interactions. Interactions included direct messaging on PRIME-D as well as commenting on and liking content posted to the community moments feed. To further understand how participants were engaging with the PRIME-D platform, we evaluated “active use rate”(Schlosser et al., 2016) (i.e., while logged in, any type of interaction with coaches and/or peers, posting spontaneous or goal achievement moments) vs. passive use (logging in, but not engaging with peers or coaches or posting content onto the moments feed), and the degree of social initiative (i.e., user initiated interactions relative to responsive interactions) from peer-to-peer and coach-to-peer interactions.
Primary Outcome Assessment
Changes in mood and functioning were evaluated using a survey app at 1-, 2-, 3-, 4-, 8- and 12-week (4 weeks post-trial) time points and included the PHQ-9 to measure changes in mood and the SDS for changes in mood-related disability.
Data Analysis Plan
We examined whether any demographic variables were related to baseline symptoms (PHQ-9, GAD-7) or functioning (SDS), and whether any demographic variables, baseline symptoms and functioning were related to PRIME-D use, using zero-order correlations. To determine PRIME-D acceptability, we examined the average ratings from the PRIME-D satisfaction survey for overall satisfaction as well as the most and least popular PRIME-D features. We also calculated the percentage of Y/N ratings participant made at the 4- and 8-week time points regarding whether PRIME-D was meeting their expectations. Furthermore, we also reviewed qualitative feedback from the PRIME-D exit interview.
To investigate PRIME-D feasibility, we examined descriptive statistics for the following PRIME-D metrics: login frequency, challenges completed, spontaneous and goal achievement moments, peer and coach interactions, and active use rate. To understand participants degree of engagement in PRIME-D, we computed a variable that represented how often participant’s actively utilized PRIME-D, which we called the active use rate. To do this, we added together the average number of challenges completed, peer, and coach interactions and divided this total by the number of weeks the participant had access to PRIME-D. Thus, a value of 2.3 would mean that a participant was active on PRIME-D 2.3 times/week. Passive use was defined as logging into the app, but not posting a moment, completing a challenge or interacting with peers or coaches. Thus, a participant may login to the app 4 days per week, but actively engage with the features of the app 2 times/week.
To investigate the effect that PRIME-D had on mood and mood-related disability, we assessed changes in PHQ-9 and SDS total scores. For the SDS, we also examined changes in the SDS domains of work, social, and family functioning. We modeled changes in these domains using linear mixed effects regression models. A mixed-effect regression model is able to accommodate the nesting that occurs in the repeated measurement of the same individuals over time by modeling the random distribution of individual differences in level (random effect for intercept) and change over time (random effect for slope). These random effects are thus mixed with standard fixed-effects: model predictors, which yield a single regression coefficient for the sample.
To explore the degree to which specific aspects of PRIME-D were associated with improvements in mood and functioning, we examined three different moderators of changes in PHQ-9 and SDS total scores: passive use of PRIME-D (PRIME-D login percentage), active use of PRIME-D (active use rate), and total number of coach interactions. Thus, we conducted three separate models investigating potential changes in mood and functioning. Model analyses were conducted using the lme4 package in R version 3.1.0 (R Core Team, 2013). For significant effects, we reported unstandardized beta coefficient estimates, standard errors, and effect sizes (Cohen’s d).
Results
Participants in this study were more likely to be female, college educated, single, Caucasian, at a lower-to-middle income level, and about 1/3 were receiving some form of mental health treatment. Participant demographics were not related to clinical symptoms. However, being a female participant was associated with a greater PRIME-D login percentage, r(30) = 0.36, p = 0.05. No other demographic variables were related to any PRIME-D use metrics.
We also assessed participant digital health use (e.g. health related mobile app usage) over the past month. In terms of digital health resource utilization, participants reported moderate levels of digital health utilization, with the most utilized applications falling in the categories of improving sleep (57%), increasing exercise and fitness (53%), increasing relaxation (50%), weight loss (40%), improving concentration (30%), and managing mood (27%). The rates reported by participants are consistent with a trend reported by the Pew Research Center, which suggests that at least 50% of smartphone owners use their phones to access health information and track their health(Smith, n.d.; Street, NW, Washington, & Inquiries, n.d.). The percentage of participants using mental health services, including use of medications and psychotherapy, are presented in Table 1.
PRIME Acceptability
Mean overall satisfaction with PRIME-D for the entire sample, as rated during the exit interview administered at the 12-week post-assessment, was 7.23 (SD: 2.8). Some of the comments made by participants when asked about how PRIME-D impacted their lives included: “Prime has helped me identify some stress triggers in my life. With the insight of my coach, Charlie I have some great resources and tools to help manage my stress and anxiety”, “The interaction with peers and coaches was great! The challenges were just that, challenging, but some were also fun. Being able to see the achievements of my peers was encouraging”, and “Awesome idea that can help change lives. Helped my depression and anxiety”. The most popular PRIME-D feature was the ability to like other user’s posts (M: 8.38, SD: 2.0) and the least popular PRIME feature were the challenges (mean: 6.83, SD: 3.0).
To further assess PRIME-D acceptability, we compared the ratings made at the 4- and 8-week time points regarding the extent to which PRIME was helping them achieve their goals, whether they planned to continue using PRIME-D, and whether they would recommend PRIME-D to others. At the 4-week time point, 79% of participants stated that PRIME-D was helping them achieve their goals, 79% stated that they planned to continue using PRIME-D, and 83% stated that they would recommend PRIME-D to others. At the 8-week time point, the percentage of participants stating that PRIME-D helped them achieve their goals increased to 93% (t(29) = 1.68, p = .10, d = .31), as did the percentage of participants stating that they would continue using PRIME-D (79% to 83%, p = .72). Examples of participants goals included “To help me better understand myself and to work with others in achieving certain goals”, “help me feel more calm and centered. Help me focus on my wellness”, and “Find patterns and trends in my emotions and depression and help regulate those trends.” The percentage of participants stating that they would recommend PRIME-D to others did not change between the 4- and 8-week time points, remaining at 83%. Of the thirty-six participants enrolled, 6 participants dropped out (five after the first week, one after the second week of the trial), for an overall retention rate of 83%, suggesting that the sample found the intervention acceptable.
PRIME Feasibility
PRIME-D use data (login frequency, challenge completion, moments, and interactions) can be found in Table 2. Although participants were asked to use the app at least 1x/week, on average, participants logged in 4.5 days/week and engaged in approximately 2 features each time they used PRIME-D. While using the platform, participants were most likely to engage with their assigned coach, with participants interacting with a coach, on average, 3.5 days/week. Over an 8-week period, participants were highly engaged in the platform, with 720 direct messages sent from participants to coaches. In terms of peer-to-peer interactions, participants initiated interactions with each other a total of 63 times. Participants had about three interactions with coaches and two interactions with peers each week. Twenty-nine of the 36 participants (81%) initiated at least one message to a coach and 16 (45%) initiated more than the average of 27.8 coach interactions. Working on challenges was the least popular feature of the app, relative to posting moments and interacting with peers and coaches, however, the challenge completion rate was at around 80%, which suggests that, while participants may not have been as satisfied with this feature as others, they were highly likely to achieve their goals once they were set.
Table 2.
PRIME-D utilization characteristics
| Mean (SD) | ||
|---|---|---|
|
| ||
| Login Frequency (average days per week) | 4.56 (1.7) | |
|
| ||
| Challenge completion rate (%) | 77.6% | |
|
| ||
| Average Weekly | Average Overall | |
|
| ||
| Total Peer Interactions | 2.01 (2.7) | 16.10 (16.6) |
|
| ||
| Total Coach Interactions | 3.48 (2.4) | 27.80 (19.5) |
|
| ||
| Moments | ||
| Spontaneous | 1.00 (1.5) | 7.70 (12.0) |
| Achievement | 1.57 (1.5) | 12.53 (12.2) |
|
| ||
| Comments | 1.85 (1.8) | 14.87 (14.5) |
|
| ||
| Likes | 1.73 (2.0) | 13.87 (16.3) |
|
| ||
| Challenges Completed | ||
| Overall | 1.93 (1.7) | 15.40 (13.6) |
| Health/wellness | 1.24 (1.2) | 9.97 (9.9) |
| Social | .38 (.47) | 3.00 (3.8) |
| Creativity | .32 (.35) | 3.13 (2.9) |
| Productivity | .39 (.36) | 2.53 (2.8) |
|
| ||
| Active Use Rate | 7.28 (4.49) | 58.25 (36.0) |
Participants completed an average of about 2 challenges per week. Health/wellness challenges were the most popular at a little over one challenge completed per week, followed by creativity challenges, social challenges, and productivity challenges of which participants completed approximately 1 every two to three weeks. Challenge completion percentage was high (78%), suggesting that participants had little difficulty completing the challenges that they set.
The Effect of PRIME-D on Mood and Functioning and Moderators of Outcome
To investigate the effects of PRIME-D on participant mood and functioning, we modeled changes in PHQ-9 and SDS scores from baseline through the post-PRIME-D assessment (4 weeks after the trial ended) using linear mixed effect regression models. We conducted three different models for each of our outcomes in order to investigate which specific aspects of PRIME-D moderated potential improvements in mood and functioning.
Across all three of our models examining changes in PHQ-9 scores, we found significant main effects of time, suggesting that PHQ-9 scores decreased over the course of the trial (see Table 3). For the model looking at passive PRIME-D use, as captured by PRIME-D login percentage, we did not find a main effect of passive PRIME-D use. However, the interaction between changes in PHQ-9 scores over time and passive PRIME-D use was not significant (p = .07). For the model looking at active use of PRIME-D, we found a significant main effect of active use of PRIME-D on PHQ-9 scores. Similar to the passive use findings, the Time X Active Use interaction was not significant (p = .07). Thus, active use of PRIME-D, appears to have contributed to improvements in mood symptoms over the course of the trial. Finally, for the model looking at the effect of coach interactions, we did not find a significant main effect, but did find a significant Time X Coach Interaction effect. Taken together, participants who used PRIME-D, and specifically had greater interaction with PRIME-D coaches, were likely to have a greater improvement in mood symptoms at the post-PRIME-D assessment.
Table 3.
Linear Mixed Effect Regression Model Results
| PHQ-9 | |||||
|---|---|---|---|---|---|
| B | SE | t | p | d | |
| Intercept | 13.95 | 2.91 | −7.09 | <.001 | – |
| Time | −1.99 | 0.54 | −3.68 | .001 | −.67 |
| Passive Use | −3.68 | 4.31 | −0.85 | .40 | −.16 |
| Time X Passive Use | 1.49 | .79 | 1.88 | .07 | .34 |
| Intercept | 13.83 | 1.35 | 10.26 | <.001 | – |
| Time | −1.44 | 0.26 | −5.43 | <.001 | −.99 |
| Active Use | −0.31 | 0.16 | −1.99 | .05 | −.36 |
| Time X Active Use | 0.06 | 0.03 | 1.90 | .07 | .35 |
| Intercept | 12.14 | 1.28 | 9.46 | <.001 | – |
| Time | −1.41 | 0.24 | −5.99 | <.001 | −1.09 |
| Coach Interactions | −0.02 | 0.04 | −0.57 | .57 | −.10 |
| Time X Coach Interactions | 0.01 | 0.01 | 2.10 | .04 | .38 |
| SDS Total | |||||
|---|---|---|---|---|---|
| B | SE | t | p | d | |
| Intercept | 13.92 | 3.71 | 3.75 | <.001 | – |
| Time | −2.66 | 0.68 | −3.88 | <.001 | −.71 |
| Passive Use | 1.01 | 5.50 | 0.18 | .86 | .03 |
| Time X Passive Use | 2.49 | 1.00 | 2.48 | .02 | .45 |
| Intercept | 16.17 | 1.78 | 9.07 | <.001 | – |
| Time | −1.62 | 0.35 | −4.67 | <.001 | −.85 |
| Active Use | −0.22 | 0.21 | −1.05 | .30 | −.19 |
| Time X Active Use | 0.08 | 0.04 | 2.02 | .05 | .37 |
| Intercept | 13.90 | 1.62 | 8.56 | <.001 | – |
| Time | −1.46 | 0.32 | −4.61 | <.001 | −.84 |
| Coach Interactions | 0.02 | 0.05 | 0.50 | .62 | .09 |
| Time X Coach Interactions | 0.02 | 0.01 | 1.72 | .10 | .31 |
| B | SE | t | p | d | |
|---|---|---|---|---|---|
| SDS Social | |||||
| Intercept | 5.04 | 0.37 | 13.50 | <.001 | – |
| Time | −0.37 | 0.07 | −4.90 | <.001 | −.89 |
| SDS Work | |||||
| Intercept | 4.86 | 0.31 | 15.06 | <.001 | – |
| Time | −0.37 | 0.07 | −5.10 | <.001 | −.93 |
| SDS Family | |||||
| Intercept | 4.63 | 0.36 | 12.79 | <.001 | – |
| Time | −0.28 | 0.08 | −3.57 | <.001 | −.65 |
We found significant main effects of time for the models looking at changes in SDS total scores as well as changes in the domains of work, social, and family functioning. This suggests that mood-related disability decreased and functioning in work, social, and family domains improved over the course of the trial (see Table 3). Next, we explored moderators of total mood-related disability (SDS total score). For the model looking at passive PRIME-D use, we did not find a main effect of passive PRIME-D use, but did find a significant Time X Passive Use interaction, suggesting that logging in to the app was predictive of improved functioning over time. We found a similar pattern of findings for the model looking at active use, with a non-significant main effect, but significant Time X Active Use interaction. Thus, reported improvements in functioning appear to be moderated by PRIME-D use, regardless of whether participants were more or less actively engaging in the various features of the app. For the model looking at coaching interactions, we did not find a significant main effect or Time X Coaching Interaction effect. Despite not being significant, the effect size for the Time X Coaching Interaction effect was in the moderate range.
Discussion
The results from the study supported our hypotheses that PRIME-D was feasible, acceptable, and effective at improving mood and functioning in adults with depression. Participants who joined the trial were moderately depressed, as self-reported using the PHQ-9, and were disabled by their mood symptoms to a moderate degree in the domains of work, social functioning and family relationships. Typically, individuals who report this degree of mood symptom severity and subsequent disruption to functioning; the treatment recommendations are to initiate psychotherapy or antidepressant medication(Spitzer et al., 1999). Overall, participants reported over a 50% reduction in mood symptoms over the course of using PRIME-D. Participants went from moderately depressed to the mild range, which is a clinically significant reduction in symptoms (Spitzer et al., 1999). The improvement in mood symptoms was observed relatively quickly (within the first week) and was sustained over the four-week, post evaluation period, suggesting a relatively brief course of PRIME-D was sufficient for sustained improvements. While improvements in mood were observed whether participants were more actively or passively engaged in the app, those who interacted more with their coaches, experienced greater improvements in mood symptoms. This finding is consistent with Internet-delivered treatments, which show stronger effects of improving clinical outcomes with the addition of coach-support(Mohr et al., 2013; Richards & Richardson, 2012). Participants also experienced significant improvements in mood-related disability, such that participants went from experiencing moderate disruptions to work, social, and family life to no longer experiencing disruptions to their functioning. Further, the overall retention rate of 83% is very good, relative to other Internet-based and mobile interventions that range from 10%–70%(Richards & Richardson, 2012; Titov et al., 2010), and is consistent with the trend in the literature, which suggests that including human support improves engagement in digital health platforms(Richards & Richardson, 2012).
In addition to demonstrating the benefits of PRIME-D, we were able to highlight the feasibility and effectiveness of a potential model for screening and delivering remote care directly to individuals with depression, independent from a healthcare system. A digital system of care may help circumvent the challenges of limited access to high quality mental health care in the U.S. For instance, in this study, when participants endorsed experiences with depression, they were directly given access to a mobile treatment, whereas in traditional care settings, initial appointments may take up to three months(Kaplan, Lopez, McGinnis, & Institute of Medicine (U.S.), 2015). Another challenge we are seeing in the U.S. healthcare system pertains to the limited supply of mental health care providers relative to those seeking care(Collins et al., 2004; Weil, 2015). In this study, mental health coaches spent on average, 2 hours per week, delivering treatment to 10 individuals with depression. In comparison to traditional psychotherapy models, in which individuals attend in-person, 1-hour long weekly therapy sessions with their care provider, this delivery model represents a more efficient model of care that was also effective. Most evidence-based treatments also typically require about a 12-week course of weekly sessions, whereas we observed significant symptomatic relief within 1 week and functional improvements within 2 weeks(Beck, 1995). While PRIME-D provided a “high-touch” experience, such that users had nearly continuous access to mental health coaches and their peers, interactions were, for the most part, brief and highly effective in a short amount of time.
There are several limitations of the study, including the open label design and absence of a control condition, thereby limiting the conclusiveness of the findings. The results of this study should be replicated in a larger randomized controlled trial with a direct comparison to standard models of care. Yet, by examining the guidelines of successful treatment outcome, a 50% reduction in PHQ-9 scores and an average score of less than 9, represents clinically significant improvements, suggesting that PRIME-D is likely to produce meaningful improvements in mood(McMillan, Gilbody, & Richards, 2010; Spitzer et al., 1999).
The findings in this study add to a growing body of literature that is supporting a new, digital service delivery model to treat mental health conditions. Coach-supported mobile mental health treatments that deliver evidence-based approaches have the potential to address the serious public health problem of poor access to high quality care. In this study, we were able to demonstrate the feasibility and effectiveness of PRIME-D to produce a rapid and robust improvement in depression and mood-related disability using an efficient model of care. While evaluation of existing and new mobile treatments is necessary, those that do demonstrate empirical support should be made available to meet the growing demand for services. This is especially important given the limited supply of treatment providers trained to deliver EBTs, the long waiting lists to access care in healthcare systems around the country, and the stigma-related concerns by consumers to access care in traditional healthcare settings. Providing consumers with the choice to access care remotely, delivering a flexible, on-the-go service with qualified coaches trained to deliver EBTs has tremendous potential to improve mental health outcomes and promote better quality of life for consumers worldwide.
Supplementary Material
Figure 1.
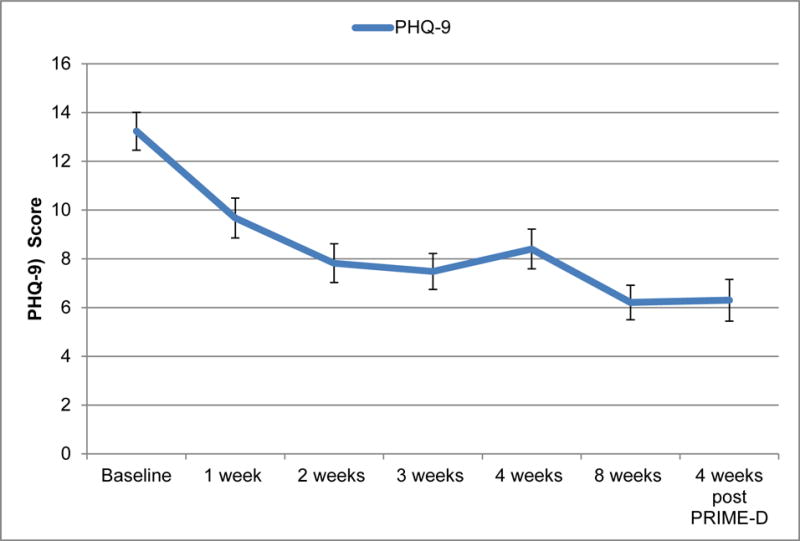
Changes in self-reported depression (PHQ-9 scores) as a function of PRIME-D use from baseline to 4-weeks post trial.
Figure 2.
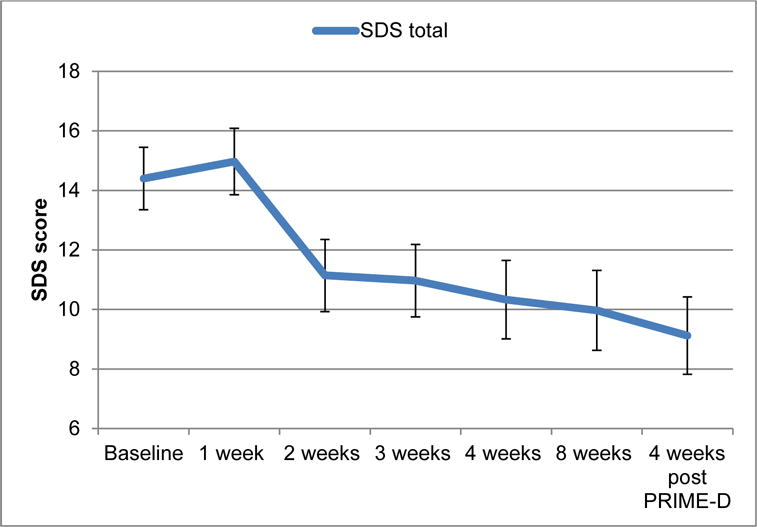
Changes in total self-reported disability (SDS scores) as a function of PRIME-D use from baseline to 4-weeks post trial.
Figure 3.
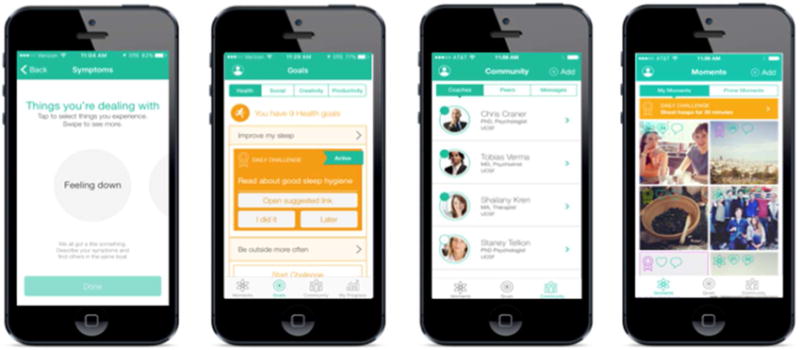
Screenshots of PRIME-D
PRIME screenshots (from left to right): Personalized profile set-up; Goal setting; Community (access to coaching and social networking); Moments (community feed).
Acknowledgments
The PRIME-product was developed from NIH funding and is owned by UCSF. None of the study authors have a financial interest in the PRIME-D product
Footnotes
The authors report no conflict of interests or financial disclosures related to this work.
Literature Cited
- 2013, T. chart shows global P. shipments from 2006 through 2013 I., worldwide, 316 million PCs were shipped, & Earlier, A. 10 P. D. from a Y. (n.d.). Infographic: Global PC Industry Continues Downward Trend. Retrieved June 17, 2016, from https://www.statista.com/chart/1766/global-pc-industry-continues-downward-trend/
- Andersson G, Cuijpers P. Internet-Based and Other Computerized Psychological Treatments for Adult Depression: A Meta-Analysis. Cognitive Behaviour Therapy. 2009;38(4):196–205. doi: 10.1080/16506070903318960. http://doi.org/10.1080/16506070903318960. [DOI] [PubMed] [Google Scholar]
- Anguera JA, Jordan JT, Castaneda D, Gazzaley A, Areán PA. Conducting a fully mobile and randomised clinical trial for depression: access, engagement and expense. BMJ Innovations. 2016;2(1):14–21. doi: 10.1136/bmjinnov-2015-000098. http://doi.org/10.1136/bmjinnov-2015-000098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck JS. Cognitive therapy: basics and beyond. New York: Guilford Press; 1995. [Google Scholar]
- Collins KA, Westra HA, Dozois DJA, Burns DD. Gaps in accessing treatment for anxiety and depression: challenges for the delivery of care. Clinical Psychology Review. 2004;24(5):583–616. doi: 10.1016/j.cpr.2004.06.001. http://doi.org/10.1016/j.cpr.2004.06.001. [DOI] [PubMed] [Google Scholar]
- Donker T, Petrie K, Proudfoot J, Clarke J, Birch MR, Christensen H. Smartphones for smarter delivery of mental health programs: a systematic review. Journal of Medical Internet Research. 2013;15(11):e247. doi: 10.2196/jmir.2791. http://doi.org/10.2196/jmir.2791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Emerging Nations Embrace Internet, Mobile Technology | Pew Research Center. (n.d.). Retrieved June 17, 2016, from http://www.pewglobal.org/2014/02/13/emerging-nations-embrace-internet-mobile-technology/
- Huguet A, Rao S, McGrath PJ, Wozney L, Wheaton M, Conrod J, Rozario S. A Systematic Review of Cognitive Behavioral Therapy and Behavioral Activation Apps for Depression. PloS One. 2016;11(5):e0154248. doi: 10.1371/journal.pone.0154248. http://doi.org/10.1371/journal.pone.0154248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaplan G, Lopez MH, McGinnis JM, Institute of Medicine (U.S.), editors. Transforming health care scheduling and access: getting to now. Washington, DC: National Academies Press; 2015. [PubMed] [Google Scholar]
- Leon AC, Olfson M, Portera L, Farber L, Sheehan DV. Assessing psychiatric impairment in primary care with the Sheehan Disability Scale. International Journal of Psychiatry in Medicine. 1997;27(2):93–105. doi: 10.2190/T8EM-C8YH-373N-1UWD. [DOI] [PubMed] [Google Scholar]
- Lopez AD, Mathers CD. Measuring the global burden of disease and epidemiological transitions: 2002–2030. Annals of Tropical Medicine and Parasitology. 2006;100(5–6):481–499. doi: 10.1179/136485906X97417. http://doi.org/10.1179/136485906X97417. [DOI] [PubMed] [Google Scholar]
- Löwe B, Decker O, Müller S, Brähler E, Schellberg D, Herzog W, Herzberg PY. Validation and standardization of the Generalized Anxiety Disorder Screener (GAD-7) in the general population. Medical Care. 2008;46(3):266–274. doi: 10.1097/MLR.0b013e318160d093. http://doi.org/10.1097/MLR.0b013e318160d093. [DOI] [PubMed] [Google Scholar]
- McMillan D, Gilbody S, Richards D. Defining successful treatment outcome in depression using the PHQ-9: A comparison of methods. Journal of Affective Disorders. 2010;127(1–3):122–129. doi: 10.1016/j.jad.2010.04.030. http://doi.org/10.1016/j.jad.2010.04.030. [DOI] [PubMed] [Google Scholar]
- Mohr DC, Duffecy J, Ho J, Kwasny M, Cai X, Burns MN, Begale M. A randomized controlled trial evaluating a manualized TeleCoaching protocol for improving adherence to a web-based intervention for the treatment of depression. PloS One. 2013;8(8):e70086. doi: 10.1371/journal.pone.0070086. http://doi.org/10.1371/journal.pone.0070086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Papakostas GI, Ionescu DF. Updates and Trends in the Treatment of Major Depressive Disorder: (ASCP Corner) The Journal of Clinical Psychiatry. 2014:1419–1421. doi: 10.4088/JCP.14ac09610. http://doi.org/10.4088/JCP.14ac09610. [DOI] [PubMed]
- Richards D, Richardson T. Computer-based psychological treatments for depression: a systematic review and meta-analysis. Clinical Psychology Review. 2012;32(4):329–342. doi: 10.1016/j.cpr.2012.02.004. http://doi.org/10.1016/j.cpr.2012.02.004. [DOI] [PubMed] [Google Scholar]
- Schlosser D, Campellone T, Kim D, Truong B, Vergani S, Ward C, Vinogradov S. Feasibility of PRIME: A Cognitive Neuroscience-Informed Mobile App Intervention to Enhance Motivated Behavior and Improve Quality of Life in Recent Onset Schizophrenia. JMIR Research Protocols. 2016;5(2):e77. doi: 10.2196/resprot.5450. http://doi.org/10.2196/resprot.5450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheehan DV, Harnett-Sheehan K, Raj BA. The measurement of disability. International Clinical Psychopharmacology. 1996;11(Suppl 3):89–95. doi: 10.1097/00004850-199606003-00015. [DOI] [PubMed] [Google Scholar]
- Smartphone penetration in the US (share of population) 2010–2019 | Statistic. (n.d.). Retrieved June 17, 2016, from http://www.statista.com/statistics/201183/forecast-of-smartphone-penetration-in-the-us/
- Smith A. US Smartphone Use in 2015. (n.d.) Retrieved from http://www.pewinternet.org/2015/04/01/us-smartphone-use-in-2015/
- Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA. 1999;282(18):1737–1744. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- Street, 1615 L., NW, Washington, S. 800, & Inquiries, D. 20036 202 419 4300 | M. 202 419 4349 | F. 202 419 4372 | M. (n.d.). Health Fact Sheet. Retrieved from http://www.pewinternet.org/fact-sheets/health-fact-sheet/
- Titov N, Andrews G, Schwencke G, Robinson E, Peters L, Spence J. Randomized controlled trial of Internet cognitive behavioural treatment for social phobia with and without motivational enhancement strategies. The Australian and New Zealand Journal of Psychiatry. 2010;44(10):938–945. doi: 10.3109/00048674.2010.493859. http://doi.org/10.3109/00048674.2010.493859. [DOI] [PubMed] [Google Scholar]
- Weil TP. Insufficient Dollars and Qualified Personnel to Meet United States Mental Health Needs: The Journal of Nervous and Mental Disease. 2015;203(4):233–240. doi: 10.1097/NMD.0000000000000271. http://doi.org/10.1097/NMD.0000000000000271. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


