Abstract
We report a case of a 7-year-old girl with atriofascicular Mahaim (AFM) pathway concomitant with Ebstein's anomaly. The QRS wave showed left bundle branch block pattern on electrocardiogram. Holter electrocardiogram showed prolongation of the PR interval and QRS morphological change during sinus tachycardia. An electrophysiological study demonstrated that the distal His potential appeared earlier than the proximal His potential, which suggested retrograde His conduction toward the atrioventricular node. Conduction from the Mahaim fiber to the His bundle was faster than that from the atrioventricular node towards the His bundle. The findings of this important case allowed a differential diagnosis between AFM and Wolff-Parkinson-White (WPW) syndrome.
Keywords: Atriofascicular Mahaim, Ebstein anomaly, Electrophysiology study, Radiofrequency catheter ablation
1. Introduction
Ebstein's anomaly is often accompanied by either Wolff-Parkinson-White (WPW) syndrome or atriofascicular Mahaim (AFM). Therefore, it is important to differentiate between them with regards to treatment and associated risks. AFM pathway indicates accessory pathway that demonstrate decremental conduction property without ventriculoatrial conduction [1]. AFM usually causes antidromic atrioventricular reciprocating tachycardia, although the risk of ventricular high-frequency reply at the time of the atrial fibrillation is lower than that in WPW syndrome. Because of shortened PR interval and prolonged QRS interval determined by electrocardiography, it is important to differentiate AFM from WPW syndrome. Here, we report our experiences with AFM complicated with Ebstein's anomaly in a 7-year-old patient.
2. Case report
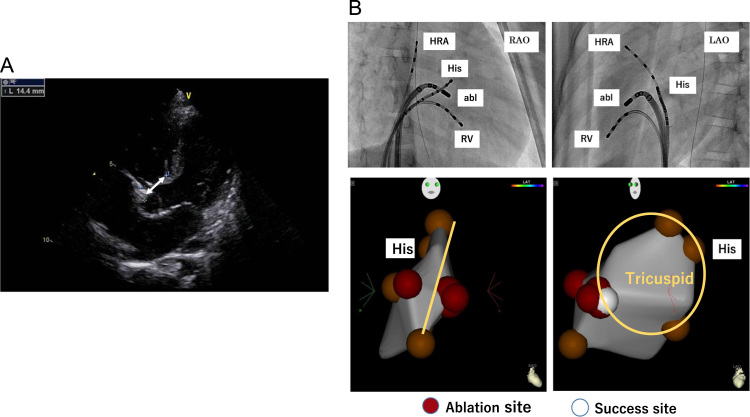
The patient was a 7-year-old girl. Delta waves were observed during a routine elementary school examination, which led to a diagnosis of WPW syndrome. She visited a nearby hospital, and an additional diagnosis of Ebstein's anomaly and atrial septal defect was made (Fig. 2A). Then, she was referred to our institution for radiofrequency catheter ablation.
Fig. 2.
(A) Echocardiography depicted the septal leaflet displaced towards the apex of the right ventricle, which led to the diagnosis of Ebstein's anomaly. (B) The successful ablation site was shown.
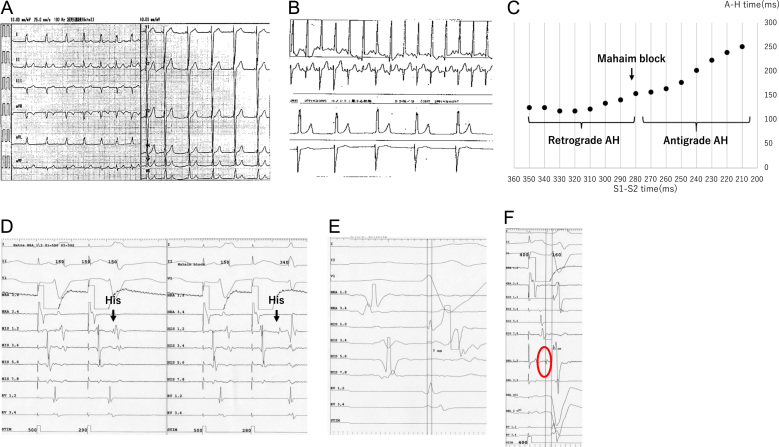
Electrocardiogram showed sinus rhythm, 79 bpm, PR interval of 0.11 s, and QRS interval of 0.12 s, and the QRS wave showed left bundle branch block pattern (Fig. 1A). Holter electrocardiogram indicated prolongation of PR interval and QRS morphological change during sinus tachycardia (Fig. 1B).
Fig. 1.
(A) These results are consistent with WPW syndrome with the right accessory pathway. (B) Normalization of both PR and QRS intervals during sinus tachycardia. (C) Both of the atrial-His and atrial-Mahaim by atrial extra pacing demonstrated decremental conduction property by atrial extra pacing. Atrial-Mahaim block was observed at 280 ms and A-His block was observed at 210 ms. (D) Mahaim block was observed at 280 ms. (E) The distal His potential appeared earlier than the proximal His potential. This suggested that the His bundle was excited retrogradely. (F) A sharp potential appeared earlier than the His potential. We diagnosed this potential as Mahaim potential.
The electrophysiological study demonstrated prolongation of both the atrial-His and atrial-Mahaim intervals during atrial extra pacing (Fig. 1C). Atrial-Mahaim interval demonstrated decremental conduction property with the effective refractory period of 280 ms (Fig. 1D). The distal His (His 1.2) potential appeared earlier than the proximal His (His 3.4) potential, which indicated retrograde His conduction towards the atrioventricular node (Fig. 1E). Atrial extra pacing during the administration of isoproterenol caused narrowing of the QRS complex with anterograde conduction in the His bundle. When an ablation catheter was placed in the tricuspid valve ring, a sharp potential appeared before the His potential (Fig. 1F). This potential was diagnosed as Mahaim potential, and catheter ablation was conducted at the site. The QRS narrowed to an interval of 3.3 s after delivery of radiofrequency energy, and disconnection of the AFM was made (Fig. 2B). Tachycardia could not be induced before and after the ablation.
3. Discussion
AFM has been reported to account for approximately 3% of all the accessory pathways. Differential diagnosis between AFM and WPW syndrome is very important because both of them cause antidromic atrioventricular reciprocating tachycardia.
One of the points to consider differentiating AFM from WPW syndrome is the change of PR interval. In WPW syndrome, PR interval during sinus rhythm is stable because accessory pathways do not exhibit decremental conduction property. Meanwhile in AFM, both PR interval and QRS waveform often change due to decremental conduction property in the Mahaim fiber. In this case, the Holter electrocardiogram demonstrated a change in the PR interval and narrowing of the QRS complex, which supported the diagnosis of AFM rather than WPW syndrome.
A previous study reported that 61% of AFM patients showed rS pattern QRS waveforms in lead III in contrast with only 6% of normal heart patients with palpitations [2]. The present case also had rS pattern QRS waveforms in lead III, which supported the diagnosis of AFM.
It has been reported that left bundle branch block causes remarkable left ventricular dyssynchrony, which could lead to future development of congestive heart failure [3]. In this case, the electrophysiological study confirmed anterograde and retrograde conduction of the atrioventricular node by atrial and ventricular pacing. We decided to perform catheter ablation, considering the risk of future development of congestive heart failure with congenital cardiac anomaly and preventing antidromic atrioventricular tachycardia.
It has been reported that the most common site on the atrium edge of AFM fibers was 8:00–10:00 on the tricuspid valve ring (87%). Of those, 67% demonstrated Mahaim potential on tricuspid valve ring, which was considered the preferred ablation site [4]. In this case, Mahaim potential was demonstrated by placing the ablation catheter around 8:00–9:00 on the tricuspid valve ring. Radiofrequency energy was delivered at this site and disconnection of AFM fibers was accomplished.
Generally, due to slow conduction velocity in the Mahaim fiber, dual anterograde atrioventricular conduction causes fusion beats. However, in this rare case, retrograde His conduction from the Mahaim fiber was faster than anterograde conduction from the atrioventricular node; therefore, in this difficult and important case, the diagnosis of AFM rather than WPW syndrome was made.
4. Conclusion
The prevalence of WPW syndrome in patients with Ebstein's anomaly is high, while that of AFM in these patients is also common. Usually AFM demonstrates normal PR interval with incomplete left bundle block. However, in the present case, 12-leads electrocardiograms before the catheter ablation demonstrated shorter PR interval with wide QRS complex, which made it difficult to differentiate from WPW syndrome.
Conflict of interest
All authors declare no conflict of interest related to this study.
References
- 1.Tchou P., Lehmann M.H., Jazayeri M. Atriofascicular connection or a nodoventricular Mahaim fiber? Electrophysiologic elucidation of the pathway and associated reentrant circuit. Circulation. 1988;77:837–848. doi: 10.1161/01.cir.77.4.837. [DOI] [PubMed] [Google Scholar]
- 2.Sternick E.B., Timmermans C., Sosa E. The electrocardiogram during sinus rhythm and tachycardia in patients with Mahaim fibers: the importance of an "rS" pattern in lead III. J Am Coll Cardiol. 2004;44:1626–1635. doi: 10.1016/j.jacc.2004.07.035. [DOI] [PubMed] [Google Scholar]
- 3.Baldasseroni S., Opasich C., Gorini M. Left bundle-branch block is associated with increased 1-year sudden and total mortality rate in 5517 outpatients with congestive heart failure: a report from the Italian network on congestive heart failure. Am Heart J. 2002;143:398–405. doi: 10.1067/mhj.2002.121264. [DOI] [PubMed] [Google Scholar]
- 4.Bohora S., Dora S.K., Namboodiri N. Electrophysiology study and radiofrequency catheter ablation of atriofascicular tracts with decremental properties (Mahaim fibre) at the tricuspid annulus. Europace. 2008;10:1428–1433. doi: 10.1093/europace/eun283. [DOI] [PubMed] [Google Scholar]