Abstract
Despite modern medicine's incredible innovation and resulting accumulation of valuable knowledge, many of the world's most problematic diseases such as Alzheimer Disease (AD) still lack effective cures and treatments. Western medicine has revealed many genetic, cellular, and molecular processes that characterize AD such as protein aggregation and inflammation. As the need for novel and effective treatments increases, researchers have turned towards traditional medicine as a resource. Modern, evidence based research examining traditional and complementary remedies for AD has generated promising results within the last decade. Animal based products inhibiting cellular toxicity, anti-inflammatory nutraceuticals such as omega-3 fatty acids, and plant based compounds derived from herbal medicine demonstrate viability as neuroprotective treatments and possible application in developing pharmaceuticals. Analysis of antioxidant, anti-inflammatory, and neuroprotective phytochemicals used in various traditional medicines around the world reveal potential to ameliorate and prevent the devastating neurodegeneration observed in AD.
Keywords: TCM, eCAM, Alzheimer, Inflammation, Treatment
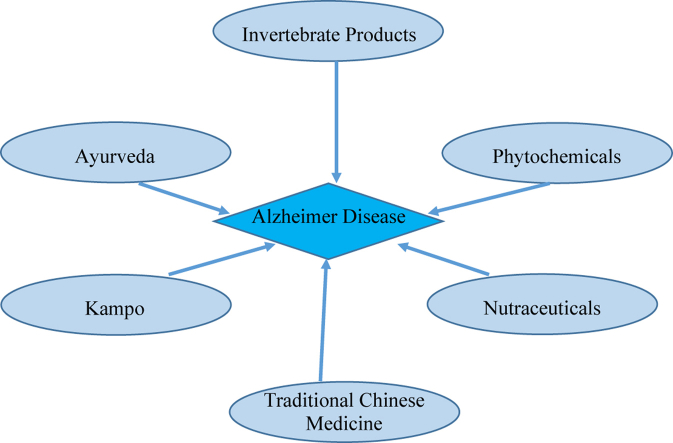
Graphical abstract
1. Alzheimer Disease (AD): general views
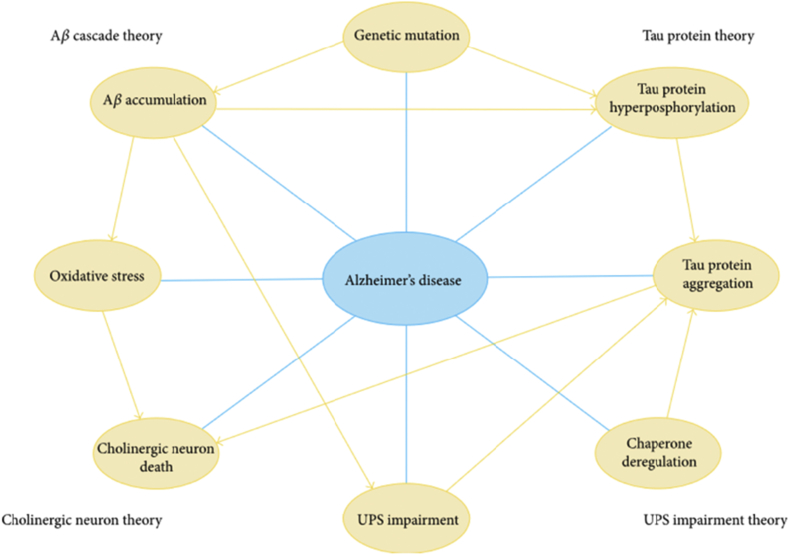
Alzheimer, a progressive neurodegenerative disease an affliction of the elderly, is the most common form of dementia, affecting over 150 million patients.1 Advances in research and technology have increased our quality of life and achieved increased longevity. Unfortunately, increased longevity is accompanied by elevated incidences of age-related diseases such as Alzheimer Disease (AD). AD is the sixth leading cause of death, and a leading cause of dementia amongst aged populations in the USA. It is a progressive neurodegenerative disorder, characterized by the prevalence of extracellular Aβ plaques and intracellular neurofibrillary tangles, derived from the proteolysis of amyloid precursor protein and hyperphosphorylation of microtubule-associated protein tau respectively. Multiple biological processes such as depletion or insufficient synthesis of neurotransmitters, oxidative stress, and abnormal ubiquitination are linked to neurodegenerative diseases.2 (Fig. 1) AD has received substantial attention as researchers seek to understand associated debilitating cognitive decline and dementia in patients. Despite mounting research, using simpler animal models such as the fruit fly, Drosophila, and the tiny round worm, Caenorhabditis elegans, molecular mechanisms that underlie pathology of AD still remain unclear.3 As one of the most complicated neurodegenerative diseases, AD is still an unsolved social and medical problem without effective treatment.3, 4, 5
Fig. 1.
The multifaceted molecular pathology of AD. AD has been linked to many possible causes on genetic, molecular, and cellular levels. Each node in this figure represents a possible cause of AD. These causal events may work in concert and form an intricate cross-talking network, eventually resulting in neuronal death among patients.6
Understanding and modulating chronic activation of innate inflammatory responses could lead to new approaches for preventing and treating AD. Formation of neurofibrillary tangles and misfolding of amyloid-β peptides are reasonably clear as the devastating basis of neurodegeneration in AD.2, 3 However, the role of neuroinflammation has only been recently identified as an important component. Experimental, genetic, and epidemiological data have revealed the immune system's active role as a disease promoting factor.1 Binding of misfolded and aggregated proteins to receptors on microglia and astroglia may trigger an innate immune response, setting off a cascade of inflammation in the brain which in effect contributes to disease progression. Several genes associated with misfolding of proteins and inflammatory responses have been identified. External factors such as diabetes and obesity that exacerbate inflammatory processes may also contribute to disease progression. Thus, evidence indicates that the pathology of AD extends beyond its effects on neurons, and is closely related to immunological mechanisms and neuroinflammation.7
Immune reactions that may contribute to progression of AD however are not entirely clear. The immune system plays a complex role in progression of neurodegenerative disorders, exhibiting both neurodestructive and neuroprotective responses. The destructive or protective mechanisms are dependent on the relative numerical and functional dominance of effector or regulatory T cells. Immune responses may exhibit different migratory, regulatory, and effector functions after being triggered by misfolded and aggregated proteins and cell-specific stimuli. This in turn alters glial and neuronal behaviors that affect neuroinflammation and neuronal survival, altering the disease course. Consequently, the discovery of these destructive or protective immune mechanisms could lead to development of novel treatments by targeting therapeutic pathways that affect neuronal survival and slow disease progression.8
2. Utilizing animal models
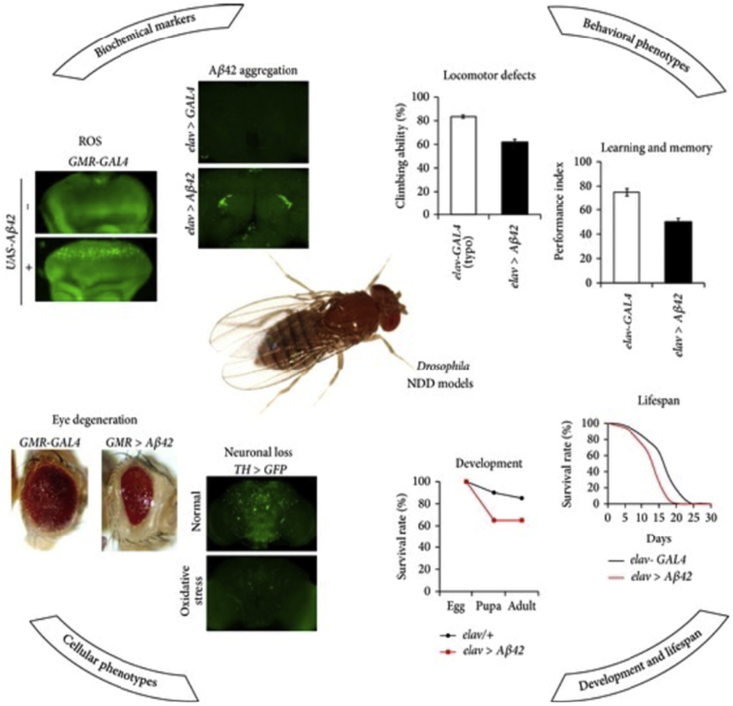
Our elderly population is rapidly growing, and as needs for novel therapeutics and methods of preventing AD escalate, analysis from an evolutionary perspective may prove valuable. In searching for answers and treatments, considering why AD exists and how it has evolved may expand our understanding of disease pathology.9 Due to the complex nature of immune and genetic mechanisms involved in AD, using certain animal models has advantages. Turning to a known model, Lee et al (2014) acknowledge that the fruit fly Drosophila is one of the oldest and most powerful genetic models, and a novel source of insights into numerous biological processes. Drosophila has emerged as a model system to analyze human diseases, which now include several that affect the nervous system. Due to genomic similarity between Drosophila and humans, neurodegenerative disease models that employ Drosophila exhibit various human-disease-like phenotypes (Fig. 2). As a result there is rapid and cost-effective in vivo genetic modifier for screening and drug evaluation. These models reveal many disease-associated genetic factors that facilitate the identification of potentially useful drugs.10
Fig. 2.
Representative neurological phenotypes of the Drosophila neurodegenerative disease models.10
Despite numerous advantages of Drosophila, its usage in evaluating traditional medicines is relatively new. Thus Drosophila can now be introduced for analyzing neurodegenerative diseases modeled after examples that demonstrate successful application of Drosophila models in evaluating traditional medicines.10 Development of new genomic technologies has potential to advance animal model research even further.10, 11 When viewing animal models of disease and treatment, the fruit fly is often the first species to be examined. However, an even simpler model is becoming equally popular.3 Model organisms, such as the nematode, C. elegans, offer a complementary approach to numerous questions. C. elegans is advantageous for several reasons to analyze AD and other neurodegenerative diseases in depth. Like their mammalian counterparts, these nematode worms possess complex conserved biochemical pathways. Gene mutations that correlate with AD possess worm counterparts in C. elegans. These include an amyloid precursor protein related gene, apl-1, a tau homolog, ptl-1, and presenilin homologs, such as sel-12 and hop-1. With neuronal connectivity in C. elegans established, it is now advantageous as a model for learning and memory impairments that occur during AD.3
Earthworms, an emerging model, have been widely used as sources of food and medicine in the practice of traditional medicine. Forging a new research direction recently has resulted from analyses of innate immunity. While interest in and recognition of earthworms' beneficial properties stems from ancient cultures, earthworms are now being examined in modern medicine for their biomedical potential, advancing how we understand innate immunity. In fact, one of the first studies devoted to the histopathology of senescence revealed characteristics in earthworms with uniform amyloid deposits.12 This may be an important path and prove useful in analyzing and understanding AD, revealing even more undiscovered insights into immunity and medicinal properties.13
We recognize that AD is a complex and progressive neurodegenerative disorder. Available therapy is limited to treating symptoms, thus its efficacy remains somewhat unsatisfactory. Aware of the prevalence and predicted increase in incidence of AD, is it essential to develop effective therapy so crucial for public health? Following this lead and due to multifactorial etiology of AD, the multi-target-directed ligand approach is promising as we augment our search for new anti-AD drugs. Guzior et al (2015) review current development of multifunctional potential of anti-AD agents, most of which are acetylcholinesterase inhibitors that extend the pharmacological profile. Thus compounds that offer hope are symptomatic and suggest causal treatment of AD.
Advantageous properties include the amyloid-β antiaggregation activity, inhibition of β-secretase and monoamine oxidase, an antioxidant and metal chelating activity, NO releasing ability and interaction with cannabinoid, NMDA or histamine H3 receptors. These unusual molecules possess heterodimeric structures that interact with multiple targets which in turn might combine different pharmacophores, original or derived from natural products or existing therapeutics (tacrine, donepezil, galantamine, memantine). There is minimal reaction to these findings since several described compounds may be promising drug candidates. Others may be valuable inspirations as we continue to search for new effective AD therapies.14
3. CAM and AD
Various natural animal and plant based products have enormous potential. We can therefore expect improved treatment and creation of drugs for certain diseases: cancer, diabetes, and heart disease, and expect that AD will be added. Natural products from invertebrates have already begun to be integrated into modern biomedicine, e.g. leeches are employed for plastic surgery or snail venom is used as an alternative to opioids for humans.15 For example, alterations in uptake and release of glutamate, predominant excitatory neurotransmitter in the central nervous system, have been observed in various neurodegenerative diseases, including AD. Bee venom, which has been used in Traditional Korean Medicine, exerts anti-inflammatory effects, and has been assessed for its inhibition of glutamate as related to neurotoxicity. Protecting against cell death and inhibiting cellular toxicity, bee venom is a promising compound that may be helpful as a treatment against glutamatergic neurotoxicity for neurodegenerative diseases.16 Moreover, compounds isolated from marine invertebrates have shown equally promising leads. Acetylcholinesterase (AChE) inhibition seems relevant for treating AD. Marine natural products may be effective as AChE inhibitors with curative potential.17
4. Application of phytochemicals and nutraceuticals
Synthetic drugs are useful for managing AD and many other chronic illnesses; still there are side effects. Consequently, attention of researchers has inclined toward phytochemicals as promising therapeutic agents. Many are anti-inflammatory, antioxidative and possess anticholinesterase activities with minimal side effects.2 Approaches to Traditional Chinese Medicine (TCM) remedies reveal first that traditional herbs and phytochemicals may delay AD onset and slow its progression but also allow recovery by targeting multiple pathological causes that possess antioxidative, anti-inflammatory, and antiamyloidogenic properties.4 Furthermore herbs regulate mitochondrial stress, apoptotic factors, free radical scavenging systems, and neurotrophic factors. Neurotrophins such as BDNF, NGF, NT3, and NT4/5 may also participate in neuronal and nonneuronal responses to AD.
Neurotrophin depletion accelerates progression of AD and therefore, replacing such neurotrophins could serve as a potential treatment for certain neurodegenerative diseases. Emphasis concerning mechanisms rests on phytochemicals that mediate signaling pathways involved in neuroprotection specifically neurotrophin-mediated activation of Trk receptors and members of the p75(NTR) superfamily. Research conducted by Venkatesan et al (2015) focused on representative phenolic derivatives, iridoid glycosides, terpenoids, alkaloids, and steroidal saponins as regulators of neurotrophin-mediated neuroprotection. There is evidence derived from encouraging advances, since these phytochemicals have attracted attention due to their in vitro neurotrophin potentiating activity, yet there is still a need for in vivo and clinical efficacy trials. Currently, proof of neuroprotective effects in certain preclinical models and in humans is unclear.4
Here is where we are with respect to therapeutic approaches. According to Frautschy and Cole (2010), AD involves a complex pathological cascade perhaps triggered initially by accumulation of beta-amyloid peptide aggregates or aberrant amyloid precursor protein processing. Moreover, there is credible information concerning factors initiating AD process significantly before onset of cognitive deficits. However, there is an unclear understanding of any events that immediately precede and precipitate cognitive decline. Without these events defined or at least clarified more adequately we are left with a major limiting factor that hinders rapid development of adequate prevention and treatment strategies. If we agree with the hypothesis of inhibiting certain pathways, clearly efforts have focused on pleiotropic activities of omega-3 fatty acids and anti-inflammatory, antioxidant, and anti-amyloid activity of curcumin in multiple models that consider many steps in the AD pathogenic cascade.18
AD reveals that inflammation contributes to neurodegenerative disease. Knowing this it is therefore suggested that early prevention and management of inflammation might conceivably delay onset or reduce symptoms of AD, but what is a likely target? With aging, normal physiological changes in the brain include depletion of long chain omega-3 fatty acids. Analyses have shown that brains of AD patients possess lower levels of docosahexaenoic acid (DHA). In agreement, Thomas et al (2015) report that DHA supplementation reduces markers of inflammation. Research devoted to epidemiological, dietary intervention, and supplementation support roles of long chain omega-3 fatty acids in preventing or delaying cognitive decline in AD during its early stages. These results support further investigation of long chain omega-3 supplementation in early stage AD, and maintains the importance of overall quality and composition of diet to protect against AD and dementia.19
Complementary and alternative medicine reveals nutraceuticals whose properties are both anti-inflammatory and anti-cancer. For example, mangosteen, the fruit from a tropical evergreen tree native to Southeast Asia, has nutraceuticals which possess multiple beneficial properties, especially neuroprotective, anti-oxidative, and anti-inflammatory effects. Treatment with mangosteen based nutraceuticals decreased cell death and increased brain-derived levels of neurotrophic factor. Moreover, mice fed a mangosteen supplemented diet showed improved inflammation related cognitive function, demonstrating its promise in treating AD.20 Another nutraceutical that has garnered interest as an antioxidant is quercetin. Oxidative stress plays a role in the progression of various diseases and conditions including AD. Thus quercetin has received attention as a food derived antioxidant for its promising biological effects and ability to prevent oxidative damage.21
5. Traditional medicine and AD
Despite increasing prevalence of AD worldwide, in addition to extensive research efforts to find a cure, we still have no long term solution. Effective therapeutic and preventative treatments are urgently needed to combat the devastating cognitive decline observed in patients with AD. This is especially pertinent as many potential remedies and medications for neurodegenerative diseases have been derived from traditional medicine.
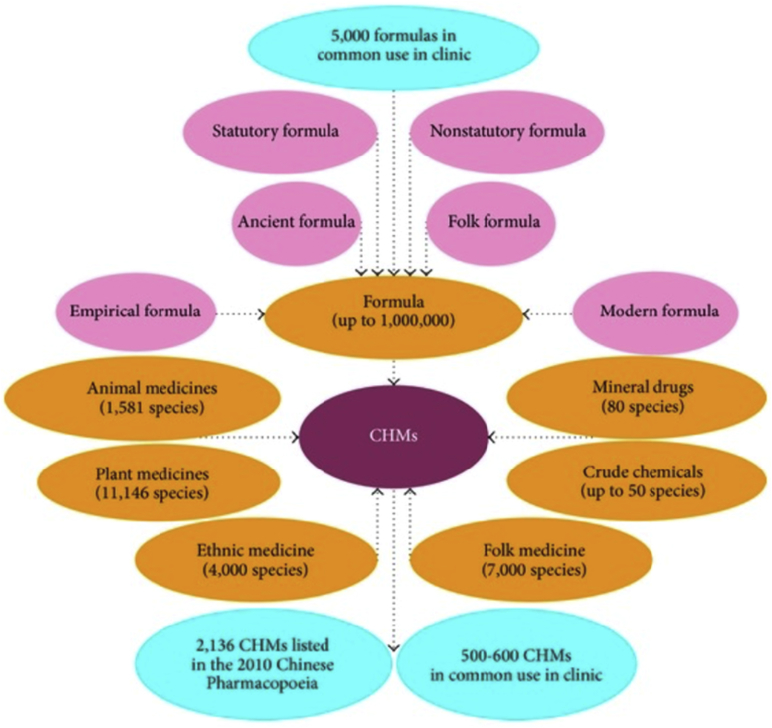
According to Liu et al (2014) Traditional Chinese Medicine (TCM) has been in use for more than 2,000 years. Recently herbal medicines employed to treat AD in China are based on TCM or modern pharmacological theories; this approach has resonated with respect to etiology and pathogenesis of AD, TCM therapy, and herbal extracts useful in treating AD. Evidence suggests that TCM therapy may offer certain complementary cognitive benefits for treating AD. Moreover, Chinese herbs may be advantageous if we consider multiple target regulation especially compared with single-target antagonist.22 (Fig. 3).
Fig. 3.
Chinese herbal medicine (CHM) in China.23
One neuroprotective plant that is widely used in TCM as herbal medicine is Evodia rutaecarpa Bentham. Evodiamine (Evo), an extract of E. rutaecarpa Bentham, presents an extensive array of beneficial properties. First, Evo exhibits anti-AD and anti-inflammatory functions. Second, a surfeit exists. There are anticancer, antiobesity, antinomic, antinociceptive, and antimetastatic functions. These results are enormously positive for treating neurodegenerative disorders.24 Moreover, TCM has also given us compounds that require improvement or alternative substitutes for existing AD. Retinoid X Receptor (RXR) agonist, Targetin, is an effective treatment for AD in mouse models. The TCM compounds β -lipoic acid and sulfanilic acid are also strong candidates as RXR agonists. Forming viable bonds with the RXR protein receptors, these TCM compounds exhibit potential to be developed into anti-dementia drugs.25
Research on the promising compound Nobiletin employed in Traditional Japanese Medicine (Kampo) has yielded promising results. Nobiletin, a citrus flavonoid, exhibited memory improving functions when tested in several animal models. Demonstrating beneficial effects against oxidative stress, cholinergic neurodegeneration, dysfunction of synaptic plasticity-related signaling, and formation of plaques, nobiletin shows potential as a natural anti-dementia compound. In addition, nobiletin exerts certain possible novel pharmaceutical and preventative applications. When tested in mice, Nobiletin enhanced learning and memory, reversing the impairment inflicted on short-term memory and recognition memory.26, 27 Further investigation of Kampo treatments has revealed another herbal medicine ninjin'yoeito (NYT). NYT has been analyzed in clinical trials for its long term effects on cognitive function and mood. Twenty-three patients at varying stages of disease progression who had all shown insufficient responses to treatment with donzepil alone were tested. Eleven patients were treated with donzepil alone, whereas twelve received a combined combination of donzepil supplemented with NYT for two years. After this period, patients receiving donzepil and NYT showed both cognitive improvement and a reduction of AD related depression.28
Ayurveda, Traditional Indian Medicine, has also contributed to the growing list of valuable compounds. Results have validated ancient remedies for nervous system disorders, including memory related conditions such as dementia. Efforts have been made to analyze Ayurvedic medicine experimentally and to understand its effects on geriatric diseases such as Alzhiemer Disease.29 Traditionally used as Ayurvedic brain tonic medicine, the plant Centella asiatica (L.) Urban, native to Southeast Asia, exerts various neuroprotective effects. Reducing oxidative stress, inhibiting enzymes, and preventing the formation of amyloid plaques in AD, C. asiatica exhibits comprehensive neuroprotection, a potential phytopharmaceutical.30
6. Application of integrative approaches
Modern biomedicine mostly utilizes a Western approach towards solving current medical problems, and has revealed many of the genetic, cellular, and molecular processes that characterize AD such as protein aggregation and inflammation. The unmistakable influence and value of primitive animal models in advancing our understanding of neurodegenerative disease is evident in studies that continue to analyze Drosophila and C. elegans. Animal models serve as cost-effective genetic sources for evaluating treatments, enhancing our understanding of conserved biochemical pathways. However, in spite recent insights into mechanisms that underlie AD pathology, current treatments lack efficacy and adequacy, and a significant cure is yet to be found—still, we persevere!
As the need for novel and effective treatments increases, researchers have turned towards ancient knowledge and alternative practices. Using a rigorous, evidence based approach to analyze compounds attributed in CAM and various traditional medicines, researchers revealed viable alternate treatments that show promising anti-inflammatory, memory improving, and neuroprotective effects. They utilize similar animal models to evaluate their potency and value, a confirmation of their still largely untapped utility. Most products are animal or plant based, and their compounds have possible applications whose development into pharmaceuticals reveal promising cures and potential prevention. Acceptance and practice of theory based medicines in Western biomedicine may require significant time to first become integrated or even totally accepted. However, utilizing Western methodology and approaches to medicine to investigate Traditional Medicine and CAM is a more pragmatic approach to integration. Evidence based research and successful application of alternative and traditional compounds have shed light on potential methods and cures for preventing AD, yielding encouraging results that point towards progress and even beyond.
Conflict of interest
There are no conflicts of interest.
Acknowledgements
Expressions of appreciation to Hillary Brown for assistance in preparing the manuscript and to Melody Ma for assistance in the revision process.
Footnotes
Peer review under responsibility of The Center for Food and Biomolecules, National Taiwan University.
Contributor Information
Edwin L. Cooper, Email: cooper@mednet.ucla.edu.
Melissa J. Ma, Email: melissajma@gmail.com.
References
- 1.Heneka M.T., Golenbock D.T., Latz E. Innate immunity in Alzheimer's disease. Nat Immunol. 2015;16(3):229–236. doi: 10.1038/ni.3102. [DOI] [PubMed] [Google Scholar]
- 2.Rasool M., Malik A., Qureshi M.S. Recent updates in the treatment of neurodegenerative disorders using natural compounds. Evid Based Complement Altern Med. 2014;2014:979730. doi: 10.1155/2014/979730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Alexander A.G., Marfil V., Li C. Use of Caenorhabditis elegans as a model to study Alzheimer's disease and other neurodegenerative diseases. Front Genet. 2014;5 doi: 10.3389/fgene.2014.00279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Venkatesan R., Ji E., Kim S.Y. Phytochemicals that regulate neurodegenerative disease by targeting neurotrophins: a comprehensive review. BioMed Res Int. 2015;2015:814068. doi: 10.1155/2015/814068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cooper E.L., Baculi B.S. Degenerative changes in the annelid Lumbricus terrestis. J Gerontol. 1968;23:375–381. doi: 10.1093/geronj/23.3.375. [DOI] [PubMed] [Google Scholar]
- 6.Sulistio Y.A., Heese K. Proteomics in traditional chinese medicine with an emphasis on Alzheimer's disease. Evidence Based Complement Altern Med. 2015;2015:1–17. doi: 10.1155/2015/393510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Heneka M.T., Carson M.J., El Khoury J. Neuroinflammation in Alzheimer's disease. Lancet Neurol. 2015;14(4):388–405. doi: 10.1016/S1474-4422(15)70016-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Anderson K.M., Olson K.E., Estes K.A., Flanagan K., Gendelman H.E., Mosley R.L. Dual destructive and protective roles of adaptive immunity in neurodegenerative disorders. Transl Neurodegener. 2014;3(1):25. doi: 10.1186/2047-9158-3-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Glass D.J., Arnold S.E. Some evolutionary perspectives on Alzheimer's disease pathogenesis and pathology. Alzheimers Dement. 2012;8(4):343–351. doi: 10.1016/j.jalz.2011.05.2408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lee S., Bang S.M., Lee J.W., Cho K.S. Evaluation of traditional medicines for neurodegenerative diseases using Drosophila models. Evid Based Complement Altern Med. 2014;967462:2014. doi: 10.1155/2014/967462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bouleau S., Tricoire H. Drosophila models of Alzheimer's disease: advances, limits, and perspectives. J Alzheimers Dis. 2015;45(4):1015–1038. doi: 10.3233/JAD-142802. http://www.ncbi.nlm.nih.gov/pubmed/25697708 [DOI] [PubMed] [Google Scholar]
- 12.Cooper E.L. Invertebrates can tell us something about senescence. Aging Clin Exp Res. 1994;6(1):5–23. doi: 10.1007/BF03324208. http://www.ncbi.nlm.nih.gov/pubmed/8043627 [DOI] [PubMed] [Google Scholar]
- 13.Cooper E.L., Balamurugan M., Huang C.Y. Earthworms dilong: ancient, inexpensive, noncontroversial models may help clarify approaches to integrated medicine emphasizing neuroimmune systems. Evid Based Complement Altern Med. 2012;164152:2012. doi: 10.1155/2012/164152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Guzior N., Wieckowska A.W., Panek D., Malawska B. Recent development of multifunctional agents as potential drug candidates for the treatment of Alzheimer's disease. Curr Med Chem. 2015;22(3):373–404. doi: 10.2174/0929867321666141106122628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cherniack E.P. Bugs as drugs, part two: worms, leeches, scorpions, snails, ticks, centipedes, and spiders. Altern Med Rev. 2011;16(1):50–58. http://www.ncbi.nlm.nih.gov/pubmed/21438646 [PubMed] [Google Scholar]
- 16.Lee S.M., Yang E.J., Choi S.M., Kim S.H., Baek M.G., Jiang J.H. Effects of bee venom on glutamate-induced toxicity in neuronal and glial cells. Evid Based Complement Altern Med. 2012;368196:2012. doi: 10.1155/2012/368196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Farrokhnia M., Nabipour I. Marine natural products as acetylcholinesterase inhibitor: comparative quantum mechanics and molecular docking study. Curr Comput Aided Drug Des. 2014;10(1):83–95. doi: 10.2174/1573409910666140408155615. http://www.ncbi.nlm.nih.gov/pubmed/24712383 [DOI] [PubMed] [Google Scholar]
- 18.Frautschy S.A., Cole G.M. Why pleiotropic interventions are needed for Alzheimer's disease. Mol Neurobiol. 2010;41(2–3):392–409. doi: 10.1007/s12035-010-8137-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Thomas J., Thomas C.J., Radcliffe J., Itsiopoulos C. Omega-3 fatty acids in early prevention of inflammatory neurodegenerative disease: a focus on Alzheimer's disease. BioMed Res Int. 2015;2015:1–13. doi: 10.1155/2015/172801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Huang H.J., Chen W.L., Hsieh R.H., Hsieh-Li H.M. Multifunctional effects of mangosteen pericarp on cognition in C57BL/6J and triple transgenic Alzheimer's mice. Evid Based Complement Altern Med. 2014;2014:813672. doi: 10.1155/2014/813672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gibellini L., Pinti M., Nasi M. Quercetin and cancer chemoprevention. Evidence Based Complement Altern Med. 2011;2011:591356. doi: 10.1093/ecam/neq053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Liu P., Kong M., Yuan S., Liu J., Wang P. History and experience: a survey of traditional chinese medicine treatment for Alzheimer's disease. Evidence Based Complement Altern Med. 2014;2014:1–5. doi: 10.1155/2014/642128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pan S.Y., Litscher G., Gao S.H. Historical perspective of traditional indigenous medical practices: the current renaissance and conservation of herbal resources. Evidence Based Complement Altern Med. 2014;2014:525340. doi: 10.1155/2014/525340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Liu A.J., Wang S.H., Hou S.Y. Evodiamine induces transient receptor potential vanilloid-1-mediated protective autophagy in U87-MG astrocytes. Evid Based Complement Altern Med. 2013;2013:354840. doi: 10.1155/2013/354840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chen K.C., Liu Y.C., Lee C.C., Chen C.Y. Potential retinoid x receptor agonists for treating Alzheimer's disease from traditional Chinese medicine. Evid Based Complement Altern Med. 2014;2014:278493. doi: 10.1155/2014/278493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nakajima A., Ohizumi Y., Yamada K. Anti-dementia activity of nobiletin, a citrus flavonoid: a review of animal studies. Clin Psychopharmacol Neurosci. 2014;12(2):75–82. doi: 10.9758/cpn.2014.12.2.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nakajima A., Aoyama Y., Shin E.J. Nobiletin, a citrus flavonoid, improves cognitive impairment and reduces soluble Aβ levels in a triple transgenic mouse model of Alzheimer's disease (3XTg-AD) Behav Brain Res. 2015;289:69–77. doi: 10.1016/j.bbr.2015.04.028. [DOI] [PubMed] [Google Scholar]
- 28.Kudoh C., Arita R., Honda M. Effect of ninjin'yoeito, a Kampo (traditional Japanese) medicine, on cognitive impairment and depression in patients with Alzheimer's disease: 2 years of observation. Psychogeriatrics. 2015:85–92. doi: 10.1111/psyg.12125. http://www.ncbi.nlm.nih.gov/pubmed/25918972 [DOI] [PubMed] [Google Scholar]
- 29.Orhan I.E. Centella asiatica (L.) urban: from traditional medicine to modern medicine with neuroprotective potential. Evid Based Complement Altern Med. 2012;2012:946259. doi: 10.1155/2012/946259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nishteswar K., Joshi H., Karra R.D. Role of indigenous herbs in the management of Alzheimer's disease. Anc Sci Life. 2014;34(1):3–7. doi: 10.4103/0257-7941.150763. [DOI] [PMC free article] [PubMed] [Google Scholar]