Abstract
Personal listening devices (PLDs) have the potential to increase the risk of noise-induced hearing loss (NIHL) for users. The present study aimed to investigate the nature and extent of the risk posed, by describing the user profile of a PLD population, identifying listening habits of that population, and examining whether PLD risk status is associated with hearing damage. A sample of 4,185 Australian PLD users completed an online survey about listening behaviors and hearing health. Listeners were characterized as low, high, or very high-risk based on daily noise dose estimates calculated from self-reported listening volume and durations. Listening patterns and hearing difficulties were examined in relation to risk status. Results indicated differences in listening volumes and durations with respect to age, with higher listening volumes reported for environments with greater background noise. Fifteen percent of participants' usage was classified as posing a potential risk to hearing, with a significantly greater proportion of younger people in higher-risk categories. Forty-one percent of participants reported feeling they have a hearing loss, with ∼20% reporting difficulties with speech in noise. For 18- to 35-year-olds, higher-risk status was associated with a greater proportion of self-reported hearing difficulties, including perceived poorer speech perception. These results have implications for hearing health promotion activities and suggest that messages should focus on either volume levels or durations depending on the particular activity in which the PLD is used. In addition, the results underline the importance of placing PLD exposure in the context of individuals' wider noise exposure. Although PLD use alone is not placing the majority of users at risk, it may be increasing the likelihood that individuals' cumulative noise exposure will exceed safe levels.
Keywords: Personal listening devices, hearing health, noise-induced hearing loss, leisure noise exposure
Learning Outcomes: As a result of this activity, the participant will be able to (1) describe the use of personal listening devices (PLDs) in the general Australian population, (2) identify the user groups and listening behaviors that are considered risky for hearing loss, and (3) describe how hearing health messages may best be targeted to decrease PLD users' risk of hearing damage.
Noise-induced hearing loss (NIHL) results from exposure to high-intensity sounds for prolonged durations and is associated with the impairment of sensory hair cells of the inner ear. 1 2 Due to the insidious onset and progression of NIHL, the presence of a hearing deficit may go unnoticed until the loss is significant and irreversible. 3 Hearing damage is cumulative and continued exposure to noise leads to a risk of further hearing loss and communication difficulties. 4 Symptoms of NIHL include tinnitus, abnormal growth in the perception of loudness (loudness recruitment), decreased sound tolerance, and difficulty understanding speech in background noise. 5 In addition, hearing loss can adversely affect an individual's cognitive function, social well-being, and quality of life. 6 These can subsequently have negative consequences for academic performance and employment opportunities. 2 7
Occupational noise has long been considered a major source of NIHL and thus the focus of both hearing conservation programs and governmental noise standards. 5 8 Noise standards attempt to quantify noise exposure in relation to maximum workday exposure limits. For example, in Australia (and many other jurisdictions) the maximum daily workplace exposure limit is set at an A-weighted equivalent continuous noise level (L Aeq ) of 85 dB over 8 hours. However, there is increasing recognition that individuals' noise exposure may occur in multiple environments beyond the workplace, including recreational settings. 9
One such recreational noise source is the use of smartphones and personal listening devices (PLDs) for listening to music and other audio content. This activity is a pervasive feature of modern society, and it is not surprising that the possibility of NIHL arising from the use of such devices has attracted increasing media and research attention. Since 2006, at least 368.9 million iPods alone have been sold worldwide, 10 and in Australia it is estimated that 84% of the population own a smartphone, 15% of whom stream music on a daily basis. 11 PLDs are considered to be a substantial contributor to recreational noise exposure, 12 and much research has been published on PLD output levels highlighting their potential hazard to long-term hearing health. 13 14 15 16 The prevalence of noise exposure from PLDs is expected to have increased in line with technological advancements such as increased storage capacity, improved portability, and increased battery life of PLDs. 14 This, in addition to greater availability of online media content and increased mobile data speeds, have enabled PLD users to listen to a larger range of higher-quality content, for longer periods of time. 4 15 All of these factors may encourage increased and prolonged PLD listening behavior that may prove dangerous to hearing depending on the volumes selected.
Unlike participation in many other noisy leisure activities, PLD users can directly control both their volume level and their listening duration. Actual exposure levels, therefore, are dependent upon the individual, and their listening habits. Not everyone who uses a PLD is likely to be at risk, and there is likely to be considerable variation in risk levels between listeners. Williams investigated PLD listening levels and associated risk (based on workplace standards) across three data collection periods (total n = 139). 17 The study found a decrease in mean listening and exposure levels over time, with those considered to be listening at risky levels dropping from 25 to 17% between 2002 and 2008. These figures related to users age 14 to 59 years but are within the range reported for teenage users by Portnuff and colleagues, 18 who found 14% of the 29 teenage PLD users tested were listening at risky levels. Other studies suggest the risk from PLDs may be greater than this. A study of 189 college students by Levey et al found that 51.9% of PLD listeners exceeded the recommended exposure level. 4 The large variation in existing exposure estimates may, to some extent, be due to variations in sample sizes and age of participants. Collecting data from larger populations may provide more representative, and thus reliable, estimates of listening behaviors and risk.
Previous research has identified several factors that influence listening patterns for PLD users. Perhaps one of the most important is the user's listening environment, which has a significant impact on the volume level chosen. For example, Airo et al reported that greater ambient noise in the listening environment led to increases in the average chosen listening level (CLL). 19 Another study found that listeners seek a preferred signal-to-noise ratio, increasing their CLL proportionately to the levels of background noise. 20 Furthermore, a recent meta-analysis showed PLD use in listening environments with higher background level was associated with a greater proportion of users exceeding risk-dose thresholds. 21
Conversely, the same study showed earphones that provide greater isolation from ambient noise allow listeners to maintain their desired signal-to-noise ratio with a lower CLL. As sound isolation is not an issue in quiet environments, differences between earphone types were greatest in the noisy environments. These findings are supported by Portnuff et al, 15 who also found increased CLLs when listening in background noise and with poorer earphone isolation.
Another influential factor is the device-transducer pairing used by the listener. There are variations in the acoustic output level between device types, and different combinations of devices and transducers affect output performance and reliability. Williams and Purnell tested a range of such device-transducer combinations to provide mean and 95% confidence interval estimates of PLD outputs based on percentage volume settings. 16 Their results showed a between-earphone variation of 8.6 dB and a between-device variation of 6.6 dB, highlighting the difficulty of estimating individual exposures.
Age and gender are also factors that affect PLD usage. 12 Smith et al reported that males had significantly greater exposure to social noise and set significantly higher CLLs than females. 22 Gender differences in preferred listening levels also have been observed in several other studies with males choosing higher PLD levels than female peers. 20 23 24 In contrast, Levey et al found no significant difference in PLD listening or exposure levels for males and females. 4 A recent study showed that age rather than gender was significantly associated with exposure, with younger users more likely to listen at higher levels. 3 Age differences also were noted by Williams, 17 who found that although exposure levels decreased with age, there was an increase in the mean age of PLD users between 2002 and 2008. This may reflect the use of PLDs continuing from adolescence into adulthood. Williams suggested that with greater accessibility to different types of media content, PLD use among older adults is increasingly considered more acceptable and convenient. 17
To better understand the factors that underlie patterns of use and levels of risk from PLDs (such as smartphones, portable music players, computers, and tablets), we need detailed data on usage from a wide range of users. Whereas previous studies have often focused on objective measures of output levels for smaller groups of PLD users, this study aimed to gather a large number of subjective reports. The aim was to compile a data set to better understand where and how PLDs are used, and the characteristics of users across the population. This information is important because it will assist hearing health professionals to identify PLD users at greatest risk and consequently design appropriately targeted reduction messages for the various types of PLD users.
Specifically, the purpose of the present study was to (1) characterize the user profile of the current Australian PLD population (in terms of age, gender, and education); (2) identify their listening habits (device and transducer type used, and listening volumes, durations and environments); (3) calculate the proportion of listeners whose PLD listening behavior could be considered high risk; and (4) determine if PLD risk status is associated with self-reported symptoms of hearing damage.
Methods
This project was part of a large online survey known as Sound Check Australia, which was approved by the Australian Hearing Human Research Ethics Committee.
Procedure
Sound Check Australia was a national noise and hearing survey accessible online and open to all Australian residents age 15 years or over. It was promoted through the Australian Broadcasting Corporation and was made available for a 5-week period from August to September 2012.
Materials
The full survey took ∼20 to 30 minutes to complete (although this varied between participants because the number of questions differed depending on individual responses) and included several modules. These covered a range of questions regarding participants' health, how often they listened to audio with headphones, participation in leisure activities and noisy work environments, and attitudes to noise and hearing loss. After demographic information was recorded, participants were asked how often “they used headphones or earbuds to listen to audio files on a PLD.” The response options were: regularly (>4 hours total during the past month), occasionally (<4 hours total during the past month), or not within the past month. All those who had used PLDs for more than 4 hours in the last month were later presented with further questions on PLD usage. Participants were asked to estimate the hours spent each month using a range of different PLD devices across different listening environments. For each usage estimated to be greater than 5 hours per month, additional questions were asked regarding estimated volume levels and transducer type. Participants were asked to estimate their usual listening volume as a percentage of the total maximum volume level for the device and to indicate from a selection of described transducer types (with example images) the headset/earphones generally used.
Participants also were asked (in a separate module) a series of questions about their hearing health including self-reports of hearing loss (question 1), changes in hearing (question 2), experience of tinnitus (question 3), hearing health (questions 4, 5), and speech perception ability in different contexts (questions 6, 7, 8; see Table 1 ).
Table 1. Hearing Health by Population and Risk Group Status*.
| Questions and Response Options | All PLD Users | Young Adult PLD Users (18–35 y) | ||
|---|---|---|---|---|
| Low Risk | High Risk | Very High Risk | ||
| n | 3,929 | 1,569 (82%) | 203 (10%) | 137 (7%) |
| Age, mean (SD) | 30 (14) | 25.2 (4.6) | 25.1 (4.6) | 25.2 (4.6) |
| % male | 53 | 54 | 60 | 49 |
| 1. Do you feel you have a hearing loss † ? | ||||
| No | 59 | 61 | 46 | 49 |
| Yes | 41 | 39 | 54 | 51 |
| 2. Over time, have you noticed any change in your hearing ability? | ||||
| No change | 46 | 50 | 38 | 45 |
| Yes, improved a little | 3 | 3 | 4 | 2 |
| Yes, Improved a lot | 1 | .4 | 1 | 0 |
| Yes, worsened a little | 48 | 46 | 55 | 47 |
| Yes, worsened a lot | 2 | 1 | 2 | 6 |
| 3. Have you ever experienced tinnitus? † | ||||
| Never/almost never | 29 | 28 | 22 | 25 |
| Occasionally | 29 | 32 | 33 | 28 |
| Sometimes | 23 | 26 | 25 | 30 |
| Frequently | 11 | 10 | 13 | 12 |
| Always/almost always | 8 | 5 | 8 | 5 |
| 4. In general, how would you describe your hearing ability? | ||||
| 1. Very poor/can hardly hear | 0 | 0 | 1 | 0 |
| 2. | 1 | 1 | 1 | 2 |
| 3. | 10 | 9 | 11 | 11 |
| 4. Neither good nor poor | 18 | 18 | 17 | 20 |
| 5. | 22 | 21 | 21 | 22 |
| 6. | 35 | 38 | 35 | 33 |
| 7. Perfect/near perfect | 15 | 14 | 16 | 12 |
| 5. Are you ever bothered by feelings that your hearing is poor? | ||||
| Never/almost never | 44 | 43 | 42 | 39 |
| Occasionally | 29 | 30 | 27 | 23 |
| Sometimes | 22 | 21 | 24 | 30 |
| Frequently | 6 | 5 | 6 | 8 |
| Always/almost always | 1 | 0.4 | 2 | 0 |
| 6. When several people are talking in a room, do you have difficulty hearing an individual conversation? | ||||
| 1. Never/almost never | 24 | 25 | 22 | 24 |
| 2. Occasionally | 31 | 34 | 29 | 25 |
| 3. Sometimes | 25 | 25 | 21 | 23 |
| 4. Frequently | 15 | 13 | 19 | 18 |
| 5. Always/almost always | 6 | 4 | 9 | 10 |
| 7. Can you follow the conversation when you are at a large dinner table? | ||||
| 1. Always/almost always | 42 | 43 | 34 | 36 |
| 2. Frequently | 35 | 38 | 40 | 37 |
| 3. Sometimes | 16 | 15 | 18 | 18 |
| 4. Occasionally | 5 | 4 | 6 | 7 |
| 5. Never/almost never | 2 | 1 | 2 | 3 |
| 8. Overall, I would judge my ability to make out speech or conversations to be: | ||||
| 1. Good | 48 | 50 | 41 | 46 |
| 2. Average | 33 | 34 | 37 | 30 |
| 3. Slightly below average | 16 | 14 | 17 | 18 |
| 4. Poor | 3 | 2 | 4 | 7 |
| 5. Very poor | 0 | 0 | 0 | 0 |
PLD, personal listening device; SD, standard deviation.
*Note: participants reporting a permanent hearing loss are not included in data set.
Where survey allowed for responses of “Unsure,” these were removed prior to analysis.
Participants
A total of 9,904 survey responses were obtained. Of these, 5,371 participants had used PLDs for more than 4 hours in the last month and were included in the study sample. These data were screened to remove responses from participants who failed to respond to large sections of the survey or those with suspect estimates of device usage (over 720 hours per month), inappropriate comments, or data-entry errors. The final sample consisted of 4,185 respondents (77.9% of the initial PLD user population).
Data Analysis
Data were analyzed using SPSS statistical software (version 23) (IBM Corp., Armonk, NY).
Listening Behaviors
Descriptive statistics were used to provide an overview of the PLD user cohort in relation to demographic details and listening habits (listening volumes, durations, and device-transducer use). Group differences in listening behaviors were investigated using t tests and one-way analyses of variance (ANOVAs) with Tukey post hoc comparisons.
Participants' PLD risk status was calculated using self-reported listening volume and duration information, in conjunction with transducer information. One-way ANOVAs with post hoc comparisons and Pearson chi-square tests were used to investigate risk-group differences in listening behavior for continuous and categorical data, respectively.
Hearing Health
Summary statistics were used to describe the self-reported hearing health of the overall sample of PLD users, after excluding participants with known permanent hearing loss. Risk-group comparisons were performed only on those age 18 to 35 years—a population of particular interest for several reasons: young adults are the most prolific users of PLDs and have had PLDs available to them for their entire adult life, many since childhood. Furthermore, this group is unlikely to be experiencing any age-related hearing loss that might confound the responses of older adults responding to self-report hearing health items.
Risk-group comparisons for the 18- to 35-year-old cohort were performed using ANOVA and chi-square analyses. Linear-by-linear association was used to compare risk status and hearing health for those questions with ordinal response options (i.e., questions 4 and 5) in which a linear relationship was predicted.
Results
Age, Gender, and Educational Characteristics
As shown in Table 2 , the study cohort consisted of PLD listeners age between 15 and 91 years (mean [M] = 31.4, standard deviation [SD] = 15.3). The majority (59%) of listeners were age 29 or younger; however, regular PLD use was prevalent among older individuals with 17% of users age 50 or over. There was a slightly higher proportion of males than females, and the majority of participants were highly educated, with 46% holding a university degree.
Table 2. Distribution of Age, Gender, and Highest Level of Education Attained in the PLD User Population.
| Variable | n | % of Sample | Mean Listening Duration (h/mo) | Mean Listening Volume (%) |
|---|---|---|---|---|
| Age | ||||
| 15–19 | 1,040 | 25 | 88 | 53 |
| 20–29 | 1,437 | 34 | 72 | 55 |
| 30–39 | 640 | 15 | 61 | 55 |
| 40–49 | 375 | 9 | 46 | 53 |
| 50+ | 693 | 17 | 47 | 48 |
| Sex | ||||
| Male | 2,233 | 53 | 68 | 53 |
| Female | 1,932 | 47 | 67 | 53 |
| Education | ||||
| No formal schooling | 3 | <1 | * | * |
| Primary | 21 | <1 | 73 | 58 |
| Some secondary | 848 | 20 | 89 | 54 |
| Completed secondary | 777 | 19 | 72 | 55 |
| Trade/technical qualification | 631 | 15 | 63 | 53 |
| University degree/postgrad | 1,904 | 45 | 58 | 52 |
PLD, personal listening device.
*Means not reported due to small group size.
Listening Volumes, Durations, Environments, Devices, and Transducers
Listening Volumes
The mean self-reported PLD listening volume was 53.3% of maximum volume setting (SD = 21.1). As shown in Table 2 , males and females reported listening volumes at similar levels, and listening volumes were similar across most age groups. However, those age 50 and above showed significantly lower listening volumes than all other age groups ( F [4, 3,525] = 12.95, p < 0.001).
Listening Durations
Listening duration data were analyzed to obtain an overview of how participants used PLDs. The total hours of listening per month were calculated, overall, and across different groups and activities to examine PLD usage profiles (see Table 2 ).
PLD mean listening durations differed significantly by age ( F [4, 4,048] = 35.83, p < 0.001). Mean monthly listening hours for 15- to 19-year-olds (M = 88, SD = 93) were significantly higher than that for 20- to 29-year-olds (M = 72, SD = 77) and 30- to 39-year-olds (M = 61, SD = 74), which were higher again than the mean monthly listening hours for those age 40 to 49 years (M = 46, SD = 53) and 50 to 59 years (M = 47, SD = 56). No significant differences were found in mean listening hours between 20- to 29- and 30- to 39-year-olds, or those age 40 to 49 and 50 or over. There was also no significant difference in mean listening durations for males and females ( t [4,001] = 0.36, p = 0.722).
Listening Environments
Across the sample, the highest proportion of listening time occurred during home-based leisure (23%), followed by working in quiet (18%) and commuting (16%; see Fig. 1 ). The percentage of individuals listening in each environment is shown in Fig. 2 ; PLD use during leisure time at home and commuting were most popular with 63% of individuals reporting participation. The next two most popular activities were working or studying in a quiet environment and exercising outdoors, which also showed participation rates of more than 50%.
Figure 1.
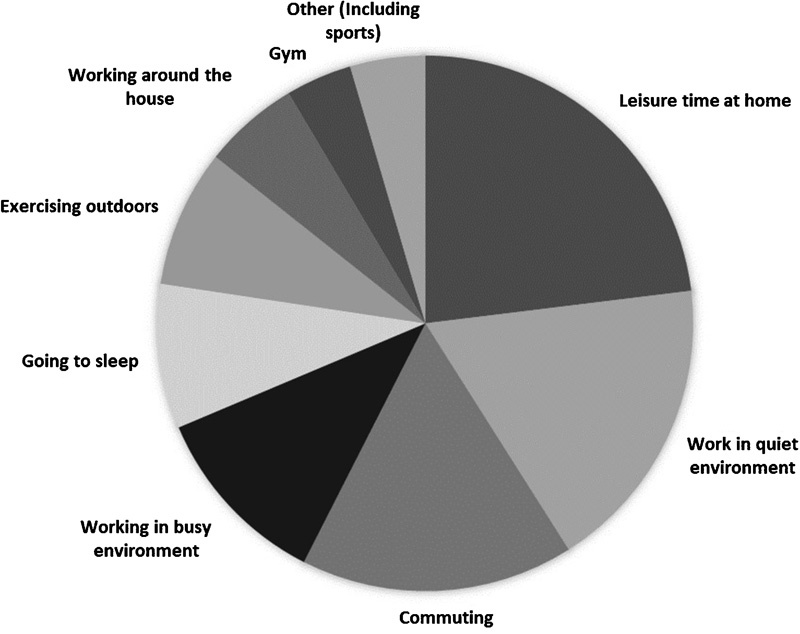
Percentage of total listening duration by listening environment.
Figure 2.
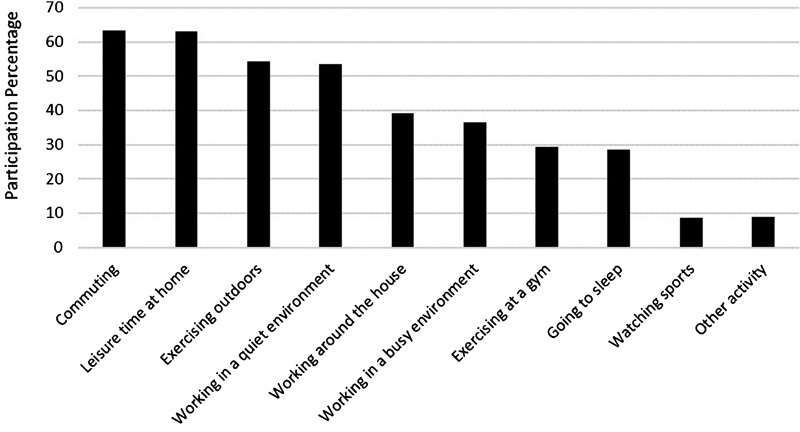
Percentage of participants who reported using PLDs at least once in each listening environment.
Participants' mean reported listening volumes for each listening environment are shown in Fig. 3 . Reported listening volumes were generally higher for environments with greater background noise (such as exercising, commuting, working in busy environment) than quieter environments.
Figure 3.
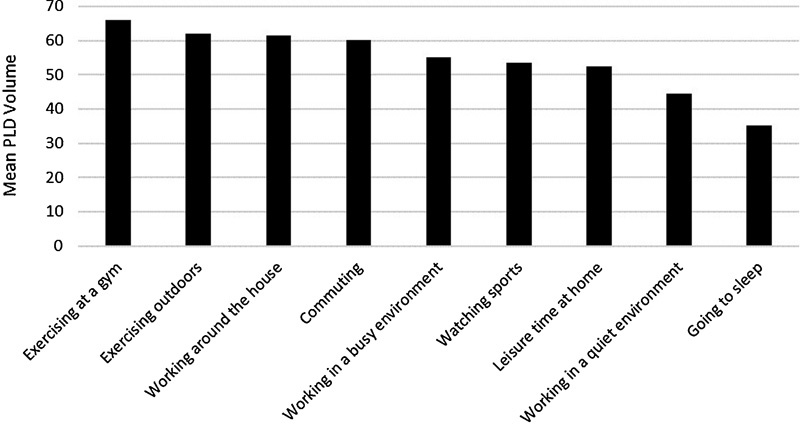
Mean volume (as percent of maximum PLD volume), by listening environment. PLD, personal listening device.
Devices and Transducer Types
MP3 devices, computers, and phones were the most commonly used devices, making up a combined 88% of total listening duration across the sample ( Fig. 4 ). Transducer use was recorded in relation to individual listening activities, with many participants using different transducers for different listening environments and/or devices. As shown in Fig. 5 , more than a quarter of participants' overall listening time was undertaken using the default earbuds or headsets that came with their nominated device. For the remaining listening hours, earbuds, which were generally reported to be used more for phones/MP3 devices for commuting and exercising, were more popular than headphones, which were predominantly used with computers or while spending leisure time at home. Only a small percentage of listening time was undertaken with noise-canceling devices (7.5%).
Figure 4.
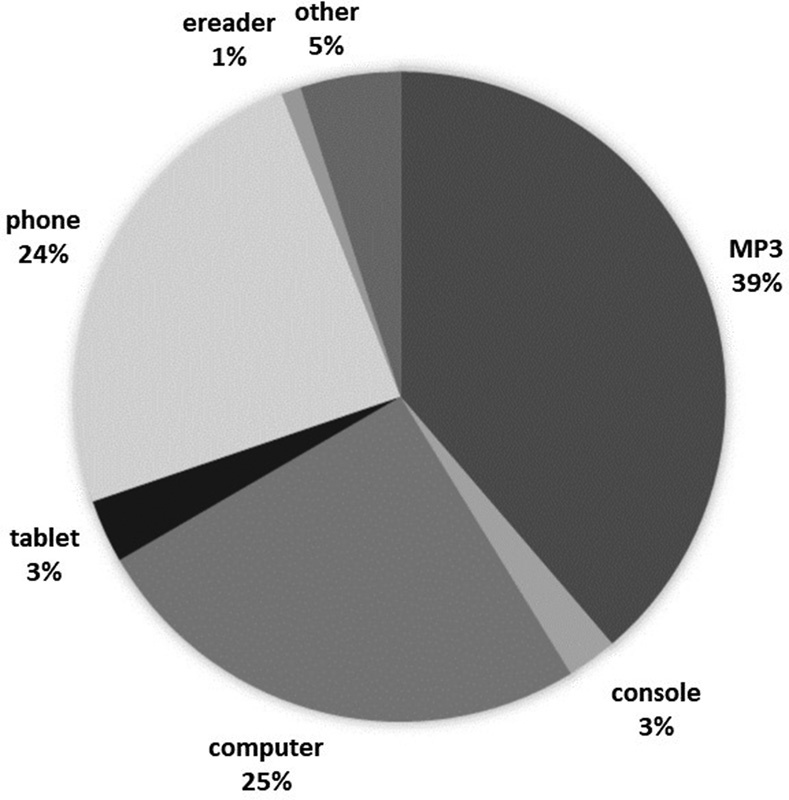
Percentage of total listening duration by device type.
Figure 5.
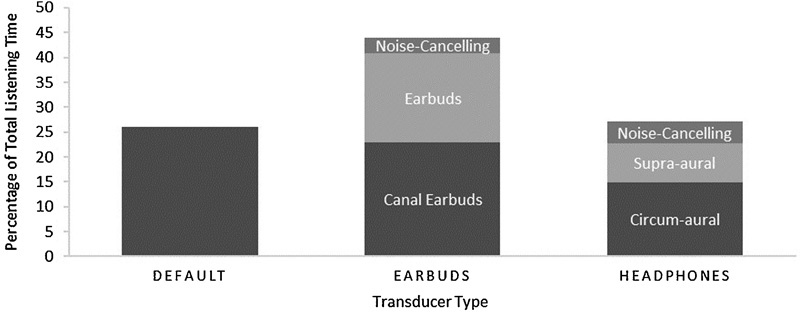
Percentage of total listening duration by transducer type. ( Default refers to the transducer that came with the device, and may include either earbuds or headphones.)
Risk Categorization
Participant risk status was calculated based on participants' self-reported PLD listening volumes and durations with respect to reported transducer type used.
To determine the relevant decibel level corresponding to participants' reported listening levels, we used three regression equations provided by the authors of an earlier publication that examined PLD listening habits. 15 Table 3 shows the equations provided by Portnuff (written communication, April 2017) across three common transducer types.
Table 3. Regression Equations for Converting Reported Percentage Volumes to Decibel Equivalents, by Transducer Type*.
| Transducer Type | Regression Equation | Corresponding Transducer Types (Current Study) |
|---|---|---|
| Earbuds | 0.6143 x + 39.395 | Default earbuds/earbuds |
| Isolator | 0.6159 x + 42.561 | Canal/noise-canceling earbuds |
| Supra-aural | 0.6147 x + 34.939 | Supra-aural/circumaural/noise-canceling headphone |
*Where x represents reported device volume as a percentage of maximum (based on data presented in Portnuff et al 15 ).
For each listening event, participants' reported listening level was converted to a decibel estimate by selecting the regression equation most appropriate for the transducer type used. Listening durations were then converted from the reported hours per month to daily duration based on a 30-day month. This duration information, along with the decibel values previously described were used to calculate exposure estimates for each activity, as a percentage of the daily recommended workplace exposure limit (where 100% = 8-hour 85 dB L Aeq ). Activity exposure estimates were summed to give a PLD daily noise dose (DND) for each participant.
Of the 4,185 PLD users, 3,578 participants provided suitable volume and duration details to calculate their risk status (see Table 4 ). Participants receiving less than 0.5 PLD DND from all their listening activities were classified as low risk. Participants whose PLD DND was greater than 0.5 were categorized as high risk, and those with a PLD DND over 3 as very high risk. A total of 401 participants (over 10% of all PLD users) had exposures of greater than 1 PLD DND—that is, they were receiving exposure levels from PLDs alone that exceeded the maximum recommended daily workplace exposure guidelines.
Table 4. Risk Classification and Related PLD DNDs*.
| Risk Status | PLD DND Criteria | n (%) | Mean PLD DND (SD) |
|---|---|---|---|
| Low risk | <0.5 | 3,017 (84.8) | 0.05 (0.10) |
| High risk | 0.5–3 | 338 (9.4) | 1.24 (0.65) |
| Very high risk | >3 | 223 (6.2) | 11.26 (11.6) |
DND, daily noise dose; PLD, personal listening device; SD, standard deviation.
*1 PLD DND = DND.
A significant difference was found across the three risk groups with respect to age ( F [2, 3,577] = 30.35, p < 0.001). Post hoc tests showed that the age of low-risk participants (M = 32, SD = 15) was significantly higher than that of high-risk and very-high-risk participants (M = 28, SD = 12 and M = 25, SD = 10, respectively); however, the mean age of the latter two risk groups did not differ from each other ( p = 0.210).
Pearson chi-square showed a significant difference in the proportion of males and females in the three risk groups (χ 2 [2, N = 3,562] = 7.13, p = 0.028), with a slightly higher percentage of females (54%) than males in the very-high-risk group.
There were significant variations in total hours per month of PLD listening across the three risk groups ( F [2, 3,551] = 155.59, p < 0.001). Tukey post hoc tests showed significant increases from low- (M = 65, SD = 68) to high-risk groups (M = 103, SD = 92), and from high- to very-high-risk groups (M = 148, SD = 124; p < 0.001).
The durations of PLD usage for individual activities also varied significantly across the three risk groups, with the exception of going to sleep. Activity durations were generally greatest for the very-high-risk group, followed by the high- and then low-risk groups (see Fig. 6 ). However, there was no difference between the high- and very-high-risk groups for leisure time at home or working in a busy environment or between the low- and high-risk group for working in quiet or busy environments, or working around the house. Furthermore, only the low- and very-high-risk groups differed significantly in the hours spent using PLDs while watching sport.
Figure 6.
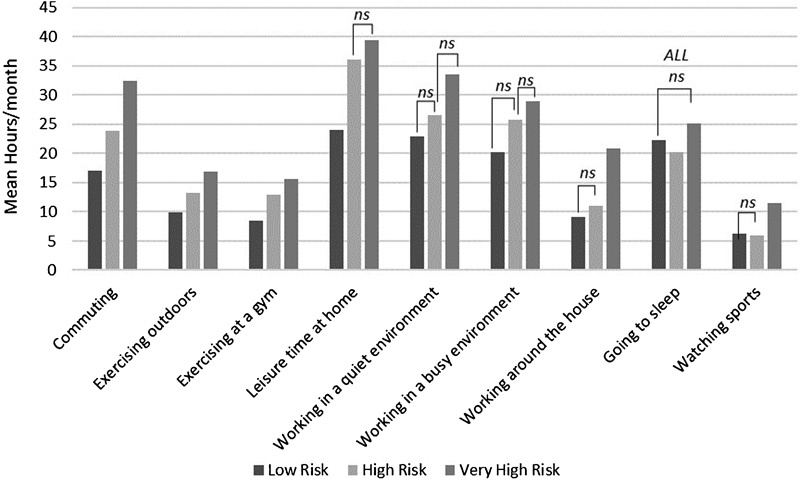
Mean monthly activity duration participation, by risk group. ns, not significant.
There was a significant difference in mean listening volumes across the three risk groups ( F [2, 3,518] = 662.81, p < 0.001). Post hoc tests showed that very-high-risk participants listened at significantly higher volumes (M = 84, SD = 14) than high-risk participants (M = 75, SD = 13), who in turn listened at significantly higher volumes than low-risk participants (M = 49, SD = 19).
Significant effects for risk groups also were seen for mean listening volumes in the various listening activities (see Fig. 7 ). Participants in the high-risk status group reported listening at significantly higher levels than participants in the low-risk status group for all activities. The very-high-risk group showed significantly higher mean listening levels than the high-risk group for each activity except watching sports (where participation numbers were low). Furthermore, the very-high-risk group was most likely to report mean listening levels above the critical 80% volume level.
Figure 7.
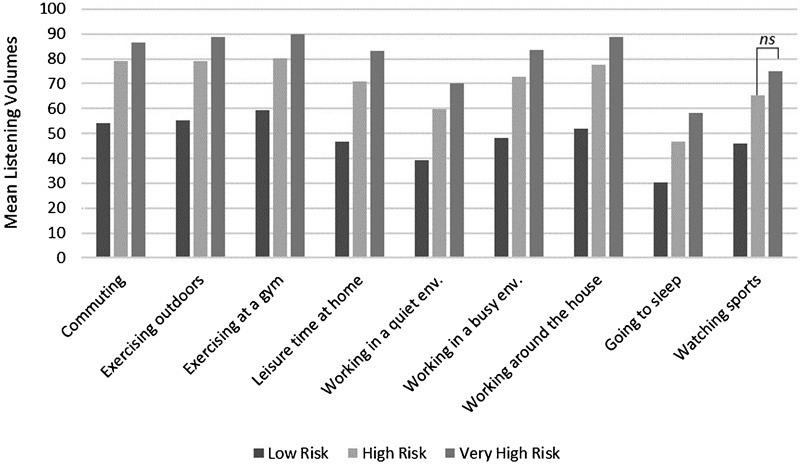
Mean activity listening volume (by risk group). ns, not significant.
Hearing Health
An overview of PLD users' responses to questions regarding their hearing health is shown in Table 1 . Overall, 41% of participants reported feeling that they had a hearing loss.
Half of the participants reported that their hearing ability had worsened over time. Nearly three-quarters of participants had experienced tinnitus, with 19% reporting they experience it frequently or always. Although only 11% of participants described their hearing ability as poor, a further 18% rated it as neither good nor poor, suggesting a lack of confidence in their hearing ability.
Just under one-fifth of participants judged themselves as having poorer than average overall speech perception abilities with 21% of participants reporting frequently or always experiencing difficulties hearing a conversation in a room full of people talking. A similar proportion of participants reported that they could infrequently follow conversations at a large dinner table. Although 60% of participants reported being at least occasionally bothered by feelings of poor hearing, this occurred frequently or always for only 6%.
Hearing Health and Personal Listening Device Risk Status (Younger Cohort: 18 to 35 Years)
As previously discussed, the age range and makeup of the overall participant sample meant that a variety of causes could account for any self-reported hearing health difficulties. Thus, our investigation of the relationship between hearing health and PLD usage (based on risk status) was restricted to those participants 18 to 35 years of age.
Risk group membership for 18- to 35-year-olds showed a similar pattern to that of the overall group. Only 17% of younger participants' PLD DNDs placed them in the high-risk category, with approximately half of these classified as very high risk. A summary of the younger cohort's responses to hearing health items, by risk group, is shown in Table 1 .
The low-risk group reported a significantly smaller proportion of self-reported hearing loss than the high- and very-high-risk groups, and this difference was significant (χ 2 [2, N = 1,346] = 15.96, p = 0.001). Furthermore, significantly greater proportions of participants in higher-risk groups reported experiencing a negative change in hearing than those in the low-risk group (χ 2 [8, N = 1,907] = 30.55, p <0.001).
Frequent tinnitus was reported by a greater proportion of those in the high-risk groups than in the low-risk group. However, participants' experience of tinnitus showed no overall significant difference in relation to risk-group membership (χ 2 [8, N = 1,839] = 7.69, p = 0.46). Similarly, although participants' self-rated hearing ability decreased in relation to risk-group status, this was not significant (χ 2 [12, N = 1,908] = 13.85, p = 0.311).
Items focusing on the impacts of hearing loss also were investigated in relation to risk status. Linear-by-linear associations showed that increased risk was significantly associated with higher likelihood of being bothered by feelings that hearing was poor (χ 2 [1, N = 1,906] = 3.95, p = 0.047). In relation to reported speech perception ability, participants' responses across the three relevant items (questions 6 to 8) were significantly and highly correlated ( r = 0.509 to 0.563, p < 0.001). A single composite score was therefore calculated based on the mean of participants' responses (coded on a scale 1 to 5) across these items and used for group comparison. There was a significant effect for group membership ( F [2, 1,906] = 10.28, p < 0.001), with post hoc tests showing the low-risk group reporting significantly fewer speech perception difficulties (1.96, SD = 0.77) than the high- and very-high-risk groups (M = 2.17, SD = 0.88; M = 2.18, SD = 0.80, respectively).
Discussion
This study aimed to profile PLD users in Australia, identify their listening habits, calculate the proportion potentially at risk for NIHL from their listening behaviors, and examine whether risk is associated with self-reported hearing difficulties.
The profile of PLD participation rates showed a disproportionately high level of use by younger listeners compared with older age groups. Listening durations and volumes also showed an association with age, with listening durations decreasing with age and those age 50 and over listening at significantly lower volume levels than younger users. Age was also a significant factor overall in relation to risk status, with higher-risk groups having a younger average age overall. On the other hand, there was no significant difference in gender between the risk groups. These findings are consistent with several other studies that have found PLD usage is associated with age but not gender. 3 4 25
Listening volumes were highest for activities associated with higher levels of background noise, such as exercising and commuting. Activities associated with less ambient noise, such as working in a quiet environment and going to sleep, showed the lowest listening volumes. These results support previous findings that background noise affects listening levels. 18 19 20 It should be noted, however, that those activities associated with the highest listening levels (e.g., exercise-related activities) were among those with the lowest levels of participation (hours per month). Providing hearing health education to PLD users, therefore, needs to reference not only activities with high listening volumes but also those with a high listening durations . PLD hearing health messages should avoid focusing only on volume reduction as a single solution. Rather, hearing health messages may be more effective if a flexible approach is taken that promotes decreasing listening volumes and/or decreasing durations, whichever is most relevant on an activity-by-activity basis. For example, users may be encouraged to find ways to decrease their PLD volumes while exercising, while for at-home activities, the focus may be to encourage listeners to decrease the amount of time spent using PLDs. For activities with high listening volumes and duration, participants should be encouraged to be more aware of their usage and decrease either or both volume and duration.
In general, earbud and canal earbuds (where earbuds are inserted into the ear) were the most commonly reported transducer type used, particularly preferred for phones and MP3 devices. This is most probably due to their ease of portability, convenience, and availability, because this style is also generally the transducer provided with PLDs. Thus, it is likely that many of the participants reporting using these were in fact using the default transducers. Furthermore, although the current survey did not differentiate between styles within the default option provided, it is likely that a large proportion of those participants reporting using these transducers were using earbuds. Headphones were most often used with the computer or while spending leisure time at home where less portability is required.
Perhaps the most important finding to emerge from this study was that ∼15% of the PLD users surveyed appear to be at risk of hearing damage from high listening volumes coupled with excessive listening duration. Although this finding is on the lower end of previous estimates of prevalence, which range from 16.7 to 51.9%, 4 17 18 it is nonetheless a substantial proportion of listeners when considering the overall popularity of PLD use. The significant differences in listening duration and volume across the three risk status groups indicate that both volume and duration are significant contributors to exposure levels.
Of particular concern are the 400 participants (over 10% of PLD users) whose exposure exceeded 1 PLD DND. These individuals are exceeding, from PLD usage alone, the total DND recommended by workplace noise exposure guidelines. As such, these listening behaviors place individuals at considerable risk of NIHL particularly when considering that PLD use is unlikely to be the only source of noise exposure for this group. 25
It is also important not to dismiss the potential impact of PLDs for those whose exposure may appear relatively low. A listener with even just 0.5 PLD DND may only be receiving 50% of an acceptable noise dose from their PLD usage—an amount unlikely to be enough to directly risk hearing damage—but they are at risk of more quickly reaching their daily exposure limit if they participate in any other noisy activities during work or leisure time. For many of these users, PLD exposure may be taking up any safety net they may have had, leaving them more vulnerable to other noise exposures (one-off or otherwise) putting them over the limit. The difficulties of devising a meaningful acceptable noise exposure guideline now that many people are exposed to multiple uncontrolled noise sources has previously been discussed. 9 The development of hearing health advice, particularly that which is aimed at PLD users, should take these issues into account.
This study also provides insight into the extent to which hearing difficulties may be present for PLD users. Tinnitus was reported by nearly three-quarters of all PLD users, which is comparable to that reported elsewhere. 26 The absence of a significant difference in tinnitus experience between the 18- to 35-year-old risk groups may be explained in several ways. Tinnitus prevalence is known to increase with age, 27 and it may be that for this younger group there is insufficient variation in age to see differences in tinnitus experience. Alternatively, it has been proposed that the presence of tinnitus can act as a motivator for reducing noise exposure. 25 28 In this case, many participants who have experienced tinnitus may have already reduced their exposure. A potential alternative explanation is that lower-intensity exposure from PLDs may be less likely to trigger hearing damage symptoms such as tinnitus, an outcome with potential implications for education. Short-term hearing difficulties, such as temporary threshold shifts and tinnitus (often considered warning signs of longer-term damage), are generally associated with higher-intensity exposures (e.g., nightclub attendance). As PLD usage is often associated with lower intensity of exposure, albeit often for longer durations, there may be fewer “red flags” that exposure doses are being exceeded. As such, many PLD users may be more likely to remain unaware of potential damage following exposure events. Hearing health messages should perhaps warn PLD users that the possibility of NIHL from low-volume PLD exposures is all the more insidious, requiring greater vigilance and monitoring of their exposure.
Interestingly, we did find differences between risk groups in relation to self-reported difficulty listening to speech in noise. The significant, albeit small, differences between risk groups were consistent across multiple items; that is, high-risk users were more likely to report hearing difficulties, particularly in relation to speech and conversation, compared with those with lower levels of risk. Although this study did not include objective measurement of hearing, these results suggest a potential relationship between PLD use and speech-in-noise difficulties. Such difficulties often precede clinical hearing loss as measured by pure tone audiometry and could therefore be considered an early warning sign for PLD users at risk of NIHL.
Limitations
Given the voluntary nature of the survey, limitations to be considered when interpreting the results include the possibility of bias in the self-selection of participants. In particular, the sample characteristics showed a skew toward participants with higher levels of education, which was also evident in the overall sample of 9,904 participants. This is potentially the result of the online nature of the study and its mode of promotion. Participants were most likely to complete the survey because of promotion through the many media arms of the national broadcaster and only if they had access to the necessary technology and were reasonably comfortable using it.
Although previous research has shown high correlations between self-reported noise exposure and objective noise dosimetry measures (suggesting that self-report can capture actual listening behavior with reasonable accuracy), clearly reliability limitations do exist. 18 The calculation of exposure estimates was based on several assumptions, each of which may limit the accuracy of the findings. Participants' volume estimates were converted to noise dose estimates via regression equations originally derived specifically for MP3 devices. The current study broadened the range of devices examined to include computers, tablets, and smartphones. It is acknowledged that these devices may have different outputs, and therefore the conversion from listening level to decibels may over- or underestimate an individual's true listening volume. Furthermore, the equations themselves contain a degree of uncertainty because they were devised by taking into account differences in the output capabilities of the PLDs originally assessed. Thus, due to inherent uncertainty in both the device outputs and the equations themselves, our volume calculations should be regarded as our best estimate of each individual's listening volume.
Another limiting factor was the reliance on participants' ability to recall past events accurately and provide an estimated average regarding their own behaviors over a month. Participants were required to report volume levels and estimate listening durations for multiple devices and activities. To minimize variations in the interpretation of questions and response items, definitions and examples were provided where necessary. Nevertheless, responses may have been impacted by participants' recall accuracy.
Conclusions
This study showed that the population of Australian PLD users is both large and diverse. A selection of hearing health indicators suggested that several high-risk users may be experiencing early warning signs of hearing damage. These findings highlight the importance of engaging with PLD users about their hearing health and encouraging them to monitor their exposure. In particular, this study suggests that to encourage safe listening behaviors in frequent PLD users, messages that are framed according to individual PLD listening patterns may be most effective. For example, for those using PLDs in higher noise environments, a major concern is corresponding increases in listening volumes. Encouraging lower volume settings or the use of transducers that provide greater attenuation (negating the need for high volumes) may be the most relevant strategies for these users. For those in lower volume environments, strategies that encourage users to monitor and limit their listening duration may be more appropriate.
Although the vast majority of those surveyed were listening at levels many would consider to be relatively safe, we would strongly argue that this does not negate the need for targeted and sustained hearing health messages for PLD users. The widespread use of, and related noise exposure from, PLDs means that a large proportion of the community is receiving consistent noise exposure, even at low levels, that may be increasing their risk of exceeding exposure guidelines once other noise sources are considered. According to the data, it would be disingenuous to suggest that PLD use alone places the majority of users at greater risk of NIHL. However, messages that position PLD exposure within the greater context of daily noise exposure guidelines may allow users to better manage their risk. Furthermore, the widespread usage of PLDs across all age groups means that hearing health campaigns incorporating PLD messages are likely to be relevant to a large cross section of the community. By targeting PLD use as a starting point for promotional activities, general awareness of hearing health could be increased, paving the way for more specific messages aimed at target groups engaged in other high-risk activities.
Acknowledgments
This study was part of Sound Check Australia a citizen science and research project undertaken by ABC Science in conjunction with the National Acoustic Laboratories, Sydney, the research division of Australian Hearing, and part of The HEARing Cooperative Research Centre (CRC) ( http://www.hearingcrc.org/ ), a Commonwealth Government funded research consortium dedicated to hearing research.
Funds for this project were provided by the Australian Government Department of Health and the Department of Industry and Science.
The authors thank Kylie Andrews, the producer from ABC Science who led this project, Ryan Sabir, for technical and IT production, and all of the citizen scientists who participated in the study. We also gratefully acknowledge the constructive assistance from Cory Portnuff during the review process, particularly in relation to exposure estimate calculations.
References
- 1.Daniel E. Noise and hearing loss: a review. J Sch Health. 2007;77(05):225–231. doi: 10.1111/j.1746-1561.2007.00197.x. [DOI] [PubMed] [Google Scholar]
- 2.Sliwinska-Kowalska M, Davis A. Noise-induced hearing loss. Noise Health. 2012;14(61):274–280. doi: 10.4103/1463-1741.104893. [DOI] [PubMed] [Google Scholar]
- 3.Fligor B J, Levey S, Levey T. Cultural and demographic factors influencing noise exposure estimates from use of portable listening devices in an urban environment. J Speech Lang Hear Res. 2014;57(04):1535–1547. doi: 10.1044/2014_JSLHR-H-12-0420. [DOI] [PubMed] [Google Scholar]
- 4.Levey S, Levey T, Fligor B J. Noise exposure estimates of urban MP3 player users. J Speech Lang Hear Res. 2011;54(01):263–277. doi: 10.1044/1092-4388(2010/09-0283). [DOI] [PubMed] [Google Scholar]
- 5.Moller A R. Burlington, MA: Academic Press; 2006. Hearing: Anatomy, Physiology, and Disorders of the Auditory System. [Google Scholar]
- 6.Arlinger S. Negative consequences of uncorrected hearing loss—a review. Int J Audiol. 2003;42 02:S17–S20. [PubMed] [Google Scholar]
- 7.Serra M R, Biassoni E C, Richter U et al. Recreational noise exposure and its effects on the hearing of adolescents. Part I: an interdisciplinary long-term study. Int J Audiol. 2005;44(02):65–73. doi: 10.1080/14992020400030010. [DOI] [PubMed] [Google Scholar]
- 8.Nelson D I, Nelson R Y, Concha-Barrientos M, Fingeruhut M. The global burden of occupational noise induced hearing loss. Am J Ind Med. 2005;48:446–458. doi: 10.1002/ajim.20223. [DOI] [PubMed] [Google Scholar]
- 9.Gilliver M, Williams W, Beach E F. Noise exposure in the balance: Managing occupational and leisure risks to hearing health. Journal of Health, Safety, and Environment. 2014;30(01):203–208. [Google Scholar]
- 10.Statista.Global Apple iPod sales from 2006 to 2014 (in million units)Available at:https://www.statista.com/statistics/263405/global-apple-ipod-sales-since-1st-quarter-2006/. Accessed February 27, 2017
- 11.Drumm J, White N, Swiegers M.Mobile Consumer Survey 2016—The Australian Cut Hyper Connectivity: Clever Consumption. Deloitte Touche Tohmatsu 2016Available at:https://www2.deloitte.com/content/dam/Deloitte/au/Documents/technology-media-telecommunications/deloitte-au-tmt-mobile-consumer-survey-2016-smartphone-091116.pdf. Accessed January 23, 2017
- 12.Dehnert K, Raab U, Perez-Alvarez C et al. Total leisure noise exposure and its association with hearing loss among adolescents. Int J Audiol. 2015;54(10):665–673. doi: 10.3109/14992027.2015.1030510. [DOI] [PubMed] [Google Scholar]
- 13.Fligor B J, Cox L C. Output levels of commercially available portable compact disc players and the potential risk to hearing. Ear Hear. 2004;25(06):513–527. doi: 10.1097/00003446-200412000-00001. [DOI] [PubMed] [Google Scholar]
- 14.Keith S E, Michaud D S, Chiu V. Evaluating the maximum playback sound levels from portable digital audio players. J Acoust Soc Am. 2008;123(06):4227–4237. doi: 10.1121/1.2904465. [DOI] [PubMed] [Google Scholar]
- 15.Portnuff C DF, Fligor B J, Arehart K H. Teenage use of portable listening devices: a hazard to hearing? J Am Acad Audiol. 2011;22(10):663–677. doi: 10.3766/jaaa.22.10.5. [DOI] [PubMed] [Google Scholar]
- 16.Williams W, Purnell J. The statistical distribution of expected noise level output from commonly available personal stereo players. Acoust Aust. 2010;38(03):119–122. [Google Scholar]
- 17.Williams W. Trends in listening to personal stereos. Int J Audiol. 2009;48(11):784–788. doi: 10.3109/14992020903037769. [DOI] [PubMed] [Google Scholar]
- 18.Portnuff C DF, Fligor B J, Arehart K H. Self-report and long-term field measures of MP3 player use: how accurate is self-report? Int J Audiol. 2013;52 01:S33–S40. doi: 10.3109/14992027.2012.745649. [DOI] [PubMed] [Google Scholar]
- 19.Airo E, Pekkarinen J, Olkinuora P. Listening to music with earphones: an assessment of noise exposure. Acta Acust United Acust. 1996;82(06):885–894. [Google Scholar]
- 20.Fligor B J, Ives T. Does earphone type affect risk for recreational noise-induced hearing loss? Available at:https://www.etymotic.com/media/publications/erl-0136-2006.pdf. Accessed January 1, 2017
- 21.Jiang W, Zhao F, Guderley N, Manchaiah V. Daily music exposure dose and hearing problems using personal listening devices in adolescents and young adults: a systematic review. Int J Audiol. 2016;55(04):197–205. doi: 10.3109/14992027.2015.1122237. [DOI] [PubMed] [Google Scholar]
- 22.Smith P A, Davis A, Ferguson M, Lutman M E. The prevalence and type of social noise exposure in young adults in England. Noise Health. 2000;2(06):41–56. [PubMed] [Google Scholar]
- 23.Torre P., III Young adults' use and output level settings of personal music systems. Ear Hear. 2008;29(05):791–799. doi: 10.1097/AUD.0b013e31817e7409. [DOI] [PubMed] [Google Scholar]
- 24.Williams W. Noise exposure levels from personal stereo use. Int J Audiol. 2005;44(04):231–236. doi: 10.1080/14992020500057673. [DOI] [PubMed] [Google Scholar]
- 25.Beach E F, Gilliver M, Williams W. Leisure noise exposure: participation trends, symptoms of hearing damage, and perception of risk. Int J Audiol. 2013;52 01:S20–S25. doi: 10.3109/14992027.2012.743050. [DOI] [PubMed] [Google Scholar]
- 26.Chung J H, Des Roches C M, Meunier J, Eavey R D. Evaluation of noise-induced hearing loss in young people using a web-based survey technique. Pediatrics. 2005;115(04):861–867. doi: 10.1542/peds.2004-0173. [DOI] [PubMed] [Google Scholar]
- 27.Shargorodsky J, Curhan S G, Curhan G C, Eavey R. Change in prevalence of hearing loss in US adolescents. JAMA. 2010;304(07):772–778. doi: 10.1001/jama.2010.1124. [DOI] [PubMed] [Google Scholar]
- 28.Widén S E, Holmes A E, Johnson T, Bohlin M, Erlandsson S I. Hearing, use of hearing protection, and attitudes towards noise among young American adults. Int J Audiol. 2009;48(08):537–545. doi: 10.1080/14992020902894541. [DOI] [PubMed] [Google Scholar]


