Abstract
Background
Diverticulosis and redundant colon are colonic conditions for which underlying pathophysiology, management and prevention are poorly understood. Historical papers suggest an inverse relationship between these two conditions. However, no further attempt has been made to validate this relationship. This study set out to assess the correlation between diverticulosis and colonic redundancy.
Methods
Redundant colon, diverticulosis and patient demographics were recorded during colonoscopy. Multivariate binary logistic regression was performed with redundant colon as the dependent variable and age, gender and diverticulosis as independent variables. Nagelkerke R 2 and a receiver operator curve were calculated to assess goodness of fit and internally validate the multivariate model.
Results
Redundant colon and diverticulosis were diagnosed in 31 and 113 patients, respectively. The probability of redundant colon was increased by female gender odds ratio (OR) 8.4 (95% CI 2.7–26, p = 0.00020) and increasing age OR 1.7 (95% CI 1.1–2.6, p = 0.017). Paradoxically, diverticulosis strongly reduced the probability of redundant colon with OR of 0.12 (95% CI 0.42–0.32, p = 0.000039). The Nagelkerke R 2 for the multivariate model was 0.29 and the area under the curve at ROC analysis was 0.81 (95% CI 0.73–0.90 p–value 3.1 × 10−8).
Conclusions
This study found an inverse correlation between redundant colon and diverticulosis, supporting the historical suggestion that the two conditions rarely occur concurrently. The underlying principle for this relationship remains to be found. However, it may contribute to the understanding of the aetiology and pathophysiology of these colonic conditions.
Keywords: Diverticulosis, Redundant colon, Acquired megacolon, Idiopathic megacolon, Colonoscopy
Introduction
Diverticulosis and redundant colon are colonic conditions posing significant morbidity and mortality risks for those affected [1, 2]. Despite this, the pathophysiological mechanisms, management and prevention of these conditions are not well understood [3, 4].
Diverticulosis
Diverticulosis is the most common pathological condition of the colon, affecting 10% of individuals under the age of 40 years and 50–70% of those greater than 80 years of age. Suggestions of altered connective tissue and enteric neuropathy exist, although the exact pathological mechanisms remain unknown [5–9].
Diverticulosis pertains to the presence of the colonic diverticula, regardless of clinical significance. Symptomatic uncomplicated diverticular disease has been attributed to short-lived abdominal pain, distension and irritable bowel syndrome-like symptoms [10, 11].
Redundant colon
In contemporary practice, endoscopists, radiologist and surgeons alike frequently note the presence of a ‘redundant colon’ [12–29]. Hanson et al. (2007) defined redundant colon as an elongated or tortuous colon or in the presence of two or more acute flexures [14]. Raahave et al. (2009) recorded colonic redundancy as a sigmoid loop rising above the iliac crests, transverse colon below iliac crests, supernumerary loops of left and right colonic flexures or a combination of these. This study also described increasing symptoms and colonic transit time with increasing numbers of redundant loops of bowel [15].
The term describes the presence of a chronically distended, elongated and tortuous colon, with no obvious cause [30–34]. Validated diagnostic criteria for the diagnosis of a redundant colon remain elusive. Its clinical significance is not readily appreciated or understood. The condition can involve any part or the entire colon, most commonly affecting the sigmoid [30, 32, 33, 35, 36]. Commonly associated symptoms include constipation and gas distress [30, 35–37]. The role of surgical management is debatable, except in instances of acute complications. Its presence is loosely associated with colonic volvulus [36, 38, 39]. Whether it consists of a heterogenous group of conditions or is due to a single cause is unknown [40]. Varying enteric neurochemical and histological findings have been suggested [41–51]. Publications on redundant colon are largely low-level evidence case reports, case series and cohort studies.
While colonoscopy is not a validated tool to diagnose the presence of colonic redundancy, endoscopists often identify the condition in the presence of tortuosity, flaccidity and difficulty maintaining insufflation [14, 35, 37].
The correlation between diverticulosis and redundant colon
Two historical papers, Ewing (1975) and Goulston (1976), suggested a low incidence of diverticulosis with redundant colon [31, 31, 52]. A common belief also exists among many gastroenterologists and general surgeons that diverticulosis and redundant colon are two conditions rarely seen together. However, no further attempts have been made to substantiate this observation.
This study set out to assess if an inverse relationship exists between diverticulosis and redundant colon. If such a correlation is demonstrated, it may indicate that mechanisms exist leading to the development of one condition and not the other.
Methods
The James Cook University Human Research Ethics Committee approved this study (approval number H5759) and it was performed in accordance with the recommendation of the Declaration of Helsinki (Edinburgh revision, 2010). Individual consent was obtained from all participants.
Study design
This was a prospective study performed over 11 months of patients undergoing colonoscopy with participating endoscopists at the Cairns Private Hospital and Cairns Day Surgery, located in Cairns, Australia. Three endoscopists participated in this project—two general surgeons and one gastroenterologist. Each endoscopist had a minimum of 10-year experience.
Eligibility criteria
Patients undergoing colonoscopy with a participating endoscopist between July 2014 and June 2015, greater than 15 years old, were invited to participate. Those with incomplete data or with a history of colectomy or colostomy were excluded.
Data measurement and bias
Patients were invited to participate by mail. The presence of redundant colon was recorded as either present or absent. The diagnosis of redundant colon was based upon a subjective finding by the endoscopist of an excessively tortuous, elongated, flaccid or difficult to insufflate colon.
Statistical analysis
Multivariate binary logistic regression was performed with redundant colon as the dependent variable and gender, age in decades and the presence of diverticulosis as independent variables. Nagelkerke’s R 2 was calculated to evaluate the goodness of fit to the logistic regression model. To internally validate the multivariate model, we constructed a receiver operator curve (ROC) estimating the area under the curve with 95% confidence interval. Data analysis was performed in SPSS version 22.0 (IBM Corp, Armonk, NY).
Results
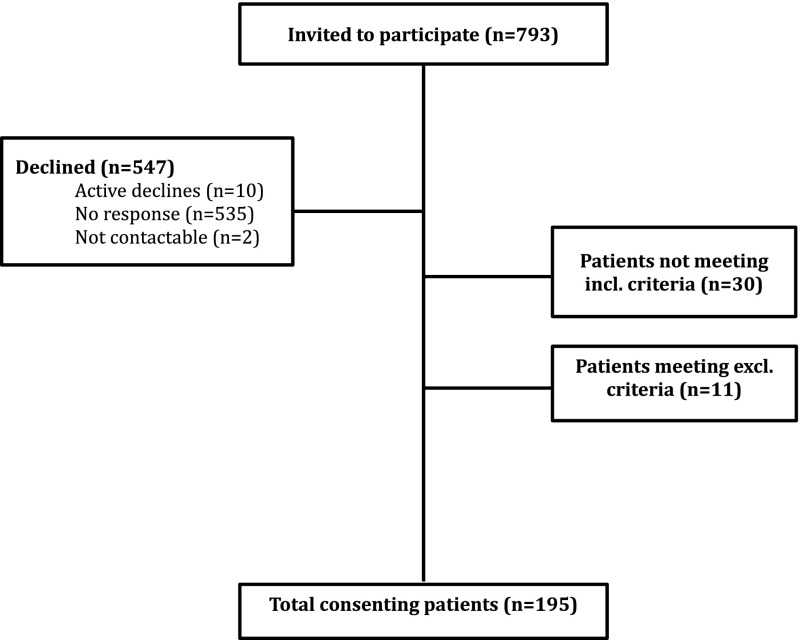
Of 793 patients undergoing colonoscopy, 195 were included in final data analysis (Fig. 1).
Fig. 1.
Outcomes of patient recruitment
Diverticulosis was diagnosed in 113 (58%) of patients. Redundant colon was diagnosed in 31 (16%) patients. The probability for redundant colon was increased by female gender with odds ratio (OR) 8.4 (95% CI 2.7–26, p = 0.00020) and age in decades with OR 1.7 (95% CI 1.1–2.6, p = 0.017). The probability for redundant colon was strongly reduced by the presence of diverticulosis with an OR of 0.12 (95% CI 0.42–0.32, p = 0.000039). The Nagelkerke R 2 for the multivariate model was 0.29 and area under the curve at ROC analysis was 0.81 (95% CI 0.73–0.90 p–value 3.1 × 10−8).
Discussion
This study verifies the suggestion by Ewing (1975) and Goulston (1976) that the redundant colon and diverticulosis rarely occur concurrently. Based on this study, one can predict the likelihood of a redundant colon occurring in an elderly female without diverticulosis is very high. Comparatively, identifying colonic redundancy in a male with diverticulosis is unlikely. This strong inverse correlation suggests that mechanisms involved with either redundant colon or diverticulosis may protect or impede the development of the other condition. Furthermore, this may provide clues to the pathogenesis.
Methodological discussion
Patient recruitment for this project was difficult from the outset and throughout. Patient participation required active patient completion of a written consent form that was mailed to them. Unfortunately, in-hospital recruitment could not be performed due to both staffing and ethical restraints. A 30% response rate was obtained. Despite this lower response rate, this study recruited sufficient patients to meet sample size calculations and produce a statistically significant finding.
A validated diagnosis for redundant colon does not yet exist. Colonoscopy is an unvalidated, dichotomous and subjective method to diagnose redundant colon. Endoscopists describe the finding based on their own clinical discretion. Another pitfall of colonoscopy-based diagnosis of redundant colon is the inability to quantify the findings into mild, moderate or severe. Such diagnoses require modalities with physically measurable outcomes—such as radiological imaging or at laparotomy. Some radiological methods such as CT colonography allow for standardized, quantitative diagnoses, which are reproducible between clinicians.
Conclusion
This study found a statistically significant inverse correlation between the presence of colonic redundancy and diverticulosis during colonoscopy. This finding is in keeping with the suggestions of Ewing (1975) and possibly Goulston (1976) that the two conditions are rarely observed occurring in a single patient. Whether the pathophysiology of colonic redundancy is ‘protective’ against the development of diverticulosis or likewise, it cannot be extrapolated from this study. Further studies unveiling the underlying mechanism for this inverse correlation may also shed light on the pathogenesis of diverticulosis.
Acknowledgements
We are grateful to Dr. Pieter Prinsloo, Dr. Bernard Chin, Cairns Private Hospital, Cairns Day Surgery and James Cook University for their ongoing support and involvement in this study.
Funding
Funding research number JCU-QLD-417851 James Cook University Honours Research Department.
Compliance with ethical standards
The James Cook University Human Research Ethics Committee approved this study (approval number H5759) and it was performed in accordance with the recommendation of the Declaration of Helsinki (Edinburgh revision, 2010). Individual consent was obtained from all participants.
Conflict of interest
The authors declare that they have no conflict of interest.
References
- 1.Gladman MA, Scott SM, Lunniss PJ, Williams NS. Systematic review of surgical options for idiopathic megarectum and megacolon. Ann Surg. 2005;241(4):562–574. doi: 10.1097/01.sla.0000157140.69695.d3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bohm SK. Risk factors for diverticulosis, diverticulitis, diverticular perforation, and bleeding: a plea for more subtle history taking. Viszeralmedizin. 2015;31(2):84–94. doi: 10.1159/000381867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tursi A. Diverticulosis today: unfashionable and still under-researched. Ther Adv Gastroenterol. 2016;9(2):213–228. doi: 10.1177/1756283X15621228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gladman MA, Knowles CH. Novel concepts in the diagnosis, pathophysiology and management of idiopathic megabowel. Color Dis. 2008;10(6):531–538. doi: 10.1111/j.1463-1318.2007.01457.x. [DOI] [PubMed] [Google Scholar]
- 5.Whiteway J, Morson BC. Elastosis in diverticular disease of the sigmoid colon. Gut. 1985;26(3):258–266. doi: 10.1136/gut.26.3.258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wess L, Eastwood MA, Wess TJ, Busuttil A, Miller A. Cross linking of collagen is increased in colonic diverticulosis. Gut. 1995;37(1):91–94. doi: 10.1136/gut.37.1.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.von Rahden BH, Germer CT. Pathogenesis of colonic diverticular disease. Langenbeck's Arch Surg. 2012;397(7):1025–1033. doi: 10.1007/s00423-012-0961-5. [DOI] [PubMed] [Google Scholar]
- 8.Macbeth WA, Hawthorne JH. Intramural ganglia in diverticular disease of the colon. J Clin Pathol. 1965;18:40–42. doi: 10.1136/jcp.18.1.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wedel T, Busing V, Heinrichs G, Nohroudi K, Bruch HP, Roblick UJ, Bottner M. Diverticular disease is associated with an enteric neuropathy as revealed by morphometric analysis. Neurogastroenterol Motil. 2010;22(4):407–414. doi: 10.1111/j.1365-2982.2009.01445.x. [DOI] [PubMed] [Google Scholar]
- 10.Annibale B, Lahner E, Maconi G, Usai P, Marchi S, Bassotti G, Barbara G, Cuomo R. Clinical features of symptomatic uncomplicated diverticular disease: a multicenter Italian survey. Int J Color Dis. 2012;27(9):1151–1159. doi: 10.1007/s00384-012-1488-5. [DOI] [PubMed] [Google Scholar]
- 11.Lembcke B. Diagnosis, differential diagnoses, and classification of diverticular disease. Viszeralmedizin. 2015;31(2):95–102. doi: 10.1159/000380833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gan T, Yang JL, JC W, Wang YP, Yang L. When and why a colonoscopist should discontinue colonoscopy by himself? World J Gastroenterol. 2015;21(25):7834–7841. doi: 10.3748/wjg.v21.i25.7834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schembre DB, Ross AS, Gluck MN, Brandabur JJ, McCormick SE, Lin OS. Spiral overtube-assisted colonoscopy after incomplete colonoscopy in the redundant colon. Gastrointest Endosc. 2011;73(3):515–519. doi: 10.1016/j.gie.2010.11.047. [DOI] [PubMed] [Google Scholar]
- 14.Hanson ME, Pickhardt PJ, Kim DH, Pfau PR. Anatomic factors predictive of incomplete colonoscopy based on findings at CT colonography. AJR Am J Roentgenol. 2007;189(4):774–779. doi: 10.2214/AJR.07.2048. [DOI] [PubMed] [Google Scholar]
- 15.Raahave D, Christensen E, Loud FB, Knudsen LL. Correlation of bowel symptoms with colonic transit, length, and faecal load in functional faecal retention. Dan Med Bull. 2009;56(2):83–88. [PubMed] [Google Scholar]
- 16.Anderson JC. Water-aided colonoscopy. Gastrointest Endosc Clin N Am. 2015;25(2):211–226. doi: 10.1016/j.giec.2014.11.002. [DOI] [PubMed] [Google Scholar]
- 17.Eickhoff A, Pickhardt PJ, Hartmann D, Riemann JF. Colon anatomy based on CT colonography and fluoroscopy: impact on looping, straightening and ancillary manoeuvres in colonoscopy. Dig Liver Dis. 2010;42(4):291–296. doi: 10.1016/j.dld.2009.04.022. [DOI] [PubMed] [Google Scholar]
- 18.Gawron AJ, Veerappan A, Keswani RN. High success rate of repeat colonoscopy with standard endoscopes in patients referred for prior incomplete colonoscopy. BMC Gastroenterol. 2014;14:56. doi: 10.1186/1471-230X-14-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jung Y, Lee SH. How do I overcome difficulties in insertion? Clin Endosc. 2012;45(3):278–281. doi: 10.5946/ce.2012.45.3.278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Luo M, Shan H, Zhou K. CT virtual colonoscopy in patients with incomplete conventional colonoscopy. Chin Med J. 2002;115(7):1023–1026. [PubMed] [Google Scholar]
- 21.Martinez F, Kondylis P, Reilly J. Limitations of barium enema performed as an adjunct to incomplete colonoscopy. Dis Colon Rectum. 2005;48(10):1951–1954. doi: 10.1007/s10350-005-0140-7. [DOI] [PubMed] [Google Scholar]
- 22.Moreels TG, Macken EJ, Roth B, Van Outryve MJ, Pelckmans PA. Cecal intubation rate with the double-balloon endoscope after incomplete conventional colonoscopy: a study in 45 patients. J Gastroenterol Hepatol. 2010;25(1):80–83. doi: 10.1111/j.1440-1746.2009.05942.x. [DOI] [PubMed] [Google Scholar]
- 23.Rex DK, Chen SC, Overhiser AJ. Colonoscopy technique in consecutive patients referred for prior incomplete colonoscopy. Clin Gastroenterol Hepatol. 2007;5(7):879–883. doi: 10.1016/j.cgh.2007.03.015. [DOI] [PubMed] [Google Scholar]
- 24.Sato K, Shigiyama F, Ito S, Kitagawa T, Tominaga K, Suzuki T, Maetani I. Colonoscopy using a small-caliber colonoscope with passive-bending after incomplete colonoscopy due to sharp angulation or pain. Surg Endosc. 2013;27(11):4171–4176. doi: 10.1007/s00464-013-3016-2. [DOI] [PubMed] [Google Scholar]
- 25.Saunders BP, Halligan S, Jobling C, Fukumoto M, Moussa ME, Williams CB, Bartram CI. Can barium enema indicate when colonoscopy will be difficult? Clin Radiol. 1995;50(5):318–321. doi: 10.1016/S0009-9260(05)83424-5. [DOI] [PubMed] [Google Scholar]
- 26.Tan EJ, Soh KC, Ngiam KY. Colonic architectural change on colonoscopy in patients taking psychotropic medications. Surg Endosc. 2013;27(5):1601–1606. doi: 10.1007/s00464-012-2636-2. [DOI] [PubMed] [Google Scholar]
- 27.Vemulapalli KC, Rex DK. Water immersion simplifies cecal intubation in patients with redundant colons and previous incomplete colonoscopies. Gastrointest Endosc. 2012;76(4):812–817. doi: 10.1016/j.gie.2012.05.033. [DOI] [PubMed] [Google Scholar]
- 28.Wexner SD, Forde KA, Sellers G, Geron N, Lopes A, Weiss EG, Nogueras JJ. How well can surgeons perform colonoscopy? Surg Endosc. 1998;12(12):1410–1414. doi: 10.1007/s004649900870. [DOI] [PubMed] [Google Scholar]
- 29.Yucel C, Lev-Toaff AS, Moussa N, Durrani H. CT colonography for incomplete or contraindicated optical colonoscopy in older patients. Am J Roentgenol. 2008;190(1):145–150. doi: 10.2214/AJR.07.2633. [DOI] [PubMed] [Google Scholar]
- 30.Kantor J (1924) A clinical study of some common anatomical abnormalities of the colon. Am Roentgenray Soc 12:414–430
- 31.Ewing M. Dolichocolon. ANZ J Surg. 1975;45(2):160–163. doi: 10.1111/j.1445-2197.1975.tb05750.x. [DOI] [PubMed] [Google Scholar]
- 32.Liu R, Lin M, Yeh S. Dolichocolon: an incidental finding on gallium scintigraphy. Clin Nucl Med. 1989;15(5):356. doi: 10.1097/00003072-199005000-00019. [DOI] [PubMed] [Google Scholar]
- 33.Madiba TE, Haffajee MR, Sikhosana MH. Radiological anatomy of the sigmoid colon. Surg Radiol Anat. 2008;30(5):409–415. doi: 10.1007/s00276-008-0344-3. [DOI] [PubMed] [Google Scholar]
- 34.Friedenwald J, Feldman E. Clinical observations on the redundant colon (dolichocolon) South Med J. 1934;XXVII(2):147–154. doi: 10.1097/00007611-193402000-00010. [DOI] [Google Scholar]
- 35.Brummer P, Seppala P, Wegelius U. Redundant colon as a cause of constipation. Gut. 1962;3:140–141. doi: 10.1136/gut.3.2.140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lane RH, Todd IP. Idiopathic megacolon: a review of 42 cases. Br J Surg. 1977;64(5):307–310. doi: 10.1002/bjs.1800640502. [DOI] [PubMed] [Google Scholar]
- 37.Galambos A, Galambos W. Redundancy of the colon. Am J Dig Dis. 1946;13(3):87–101. doi: 10.1007/BF03002757. [DOI] [PubMed] [Google Scholar]
- 38.Muller-Lissner SA, Kamm MA, Scarpignato C, Wald A. Myths and misconceptions about chronic constipation. Am J Gastroenterol. 2005;100(1):232–242. doi: 10.1111/j.1572-0241.2005.40885.x. [DOI] [PubMed] [Google Scholar]
- 39.Ajao OG. Differences between surgical colorectal conditions seen in the temperate and tropical regions. Dis Colon Rectum. 1982;25(8):795–797. doi: 10.1007/BF02553315. [DOI] [PubMed] [Google Scholar]
- 40.Autschbach F, Gassler N. Idiopathic megacolon. Eur J Gastroenterol Hepatol. 2007;19(5):399–400. doi: 10.1097/MEG.0b013e3280116cb8. [DOI] [PubMed] [Google Scholar]
- 41.Kobak MW, Jacobson MA, Sirca DM. Acquired megacolon in psychiatric patients. Dis Colon Rectum. 1962;5:373–377. doi: 10.1007/BF02616592. [DOI] [PubMed] [Google Scholar]
- 42.Koch TR, Schulte-Bockholt A, Otterson MF, Telford GL, Stryker SJ, Ballard T, Opara EC. Decreased vasoactive intestinal peptide levels and glutathione depletion in acquired megacolon. Dig Dis Sci. 1996;41(7):1409–1416. doi: 10.1007/BF02088566. [DOI] [PubMed] [Google Scholar]
- 43.Koch TR, Schulte-Bockholt A, Telford GL, Otterson MF, Murad TM, Stryker SJ. Acquired megacolon is associated with alteration of vasoactive intestinal peptide levels and acetylcholinesterase activity. Regul Pept. 1993;48(3):309–319. doi: 10.1016/0167-0115(93)90159-6. [DOI] [PubMed] [Google Scholar]
- 44.Gattuso JM, Hoyle CH, Milner P, Kamm MA, Burnstock G. Enteric innervation in idiopathic megarectum and megacolon. Int J Color Dis. 1996;11(6):264–271. doi: 10.1007/s003840050059. [DOI] [PubMed] [Google Scholar]
- 45.Gattuso JM, Kamm MA, Talbot JC. Pathology of idiopathic megarectum and megacolon. Gut. 1997;41(2):252–257. doi: 10.1136/gut.41.2.252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lee J, Park H, Kamm M, Talbot I. Decreased density of interstitial cells of Cajal and neuronal cells in patients with slow-transit constipation and acquired megacolon. J Gastroenterol Hepatol. 2005;20:1292–1298. doi: 10.1111/j.1440-1746.2005.03809.x. [DOI] [PubMed] [Google Scholar]
- 47.Meier-Ruge WA, Muller-Lobeck H, Stoss F, Bruder E. The pathogenesis of idiopathic megacolon. Eur J Gastroenterol Hepatol. 2006;18:1209–1215. doi: 10.1097/01.meg.0000236883.13720.c2. [DOI] [PubMed] [Google Scholar]
- 48.Wedel T, Van Eys GJ, Waltregny D, Glenisson W, Castronovo V, Vanderwinden JM. Novel smooth muscle markers reveal abnormalities of the intestinal musculature in severe colorectal motility disorders. Neurogastroenterol Motil. 2006;18(7):526–538. doi: 10.1111/j.1365-2982.2006.00781.x. [DOI] [PubMed] [Google Scholar]
- 49.Iantorno G, Bassotti G, Kogan Z, Lumi CM, Cabanne AM, Fisogni S, Varrica LM, Bilder CR, Munoz JP, Liserre B, Morelli A, Villanacci V. The enteric nervous system in chagasic and idiopathic megacolon. Am J Surg Pathol. 2007;31(3):460–468. doi: 10.1097/01.pas.0000213371.79300.a8. [DOI] [PubMed] [Google Scholar]
- 50.Ohkubo H, Masaki T, Matsuhashi N, Kawahara H, Yokoyama T, Nakajima A, Ohkura Y. Histopathologic findings in patients with idiopathic megacolon: a comparison between dilated and non-dilated loops. Neurogastroenterol Motil. 2014;26(4):571–580. doi: 10.1111/nmo.12303. [DOI] [PubMed] [Google Scholar]
- 51.Gattuso JM, Smith VV, Kamm MA. Altered contractile proteins and neural innervation in idiopathic megarectum and megacolon. Histopathology. 1998;33(1):34–38. doi: 10.1046/j.1365-2559.1998.00438.x. [DOI] [PubMed] [Google Scholar]
- 52.Goulston E. Diverticular disease of the colon and megacolon. Incidence in a psychiatric centre compared with a teaching hospital. Med J Aust. 1976;2(23):863–864. [PubMed] [Google Scholar]