Introduction
Clear cell renal cell carcinoma (ccRCC) is the most common subtype of renal malignancy in adults.1 The disease is usually radiologically imaged with computed tomography (CT) or magnetic resonance imaging (MRI) for diagnosis, staging, treatment planning and follow up. Recently, functional studies targeting glucose or folate metabolism with fludeoxyglucose (FDG) or prostate specific membrane antigen (PSMA) binding ligands respectively have been reported to be used to stage the disease.2 Positron emission tomography (PET) using PSMA ligand detected larger number of lesions in comparison to conventional imaging modalities such as CT in a small prospective clinical trial.3 In this project, we directly compared the findings from FDG and PSMA PET in a patient with metastatic ccRCC. We assessed ex-vivo tumour characteristics to explain these findings.
Case report
A 69-year-old lady was first diagnosed with a 5 cm lesion on the posterior aspect of right kidney on a multi-phase contrast abdominal CT scan. Due to suspicious loco-regional lymph node enlargements, FDG PET scan was performed for surgical planning. It demonstrated primary tumour with tumour extension to the right renal pelvis, proximal ureter and right renal vein.
Within our centre it was previously demonstrated that PSMA PET may detect RCC metastasis with improved sensitivity and positive predictive value. Therefore, the patient underwent staging PSMA PET in addition, which found mildly PSMA avid lesions in lung fields without definitive avidity in right renal vein thrombus. Tumour thrombus was confirmed after laparoscopic cystoreductive right nephrectomy and histopathological examination.
Recent studies have assessed the utility of FDG or PSMA PET scans in diagnosing and staging metastatic RCC, with both of them showing promising results.3, 4 In contrast to previous reports, FDG PET (Fig. 1) was able to visualize renal vein thrombus better than with PSMA PET (Fig. 2) with higher avidity (SUVmax >1.5) in this particular case. Paradoxically, small lung lesions could only be visualized with PSMA PET.
Fig. 1.
FDG PET demonstrating avidity within renal vein. Red arrow points to renal vein. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
Fig. 2.
PSMA PET does not demonstrate any avidity within renal vein. Red arrow points to renal vein. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
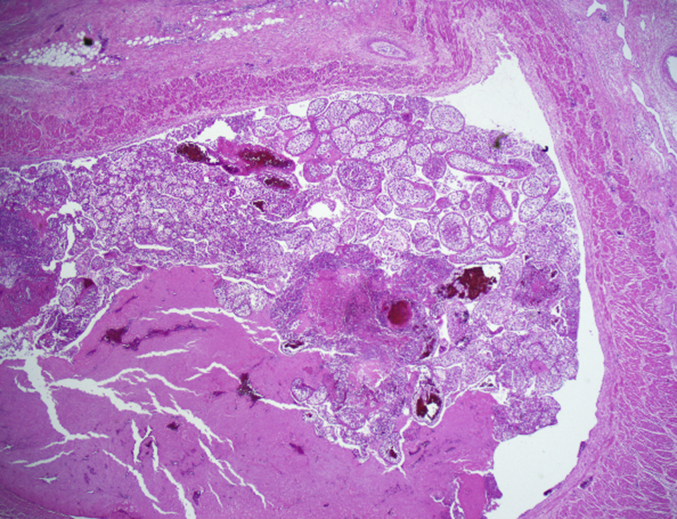
In assessing tumour thrombus, substantial component of thrombus was composed of bland thrombus with tumour necrosis rather than viable tumour, as demonstrated in the histopathological image (Fig. 3).
Fig. 3.
Clear cell carcinoma forming a tumour thrombus within a branch of renal vein, H&E, x20.
The findings are consistent with previous reports that PSMA expression is specific to neovasculature of local and metastatic RCC tumour. Therefore, friable tumour thrombus with minimal neovasculature may be imaged better with FDG PET rather than PSMA PET. However, PSMA PET was able to detect lung lesions not found with FDG PET, suggesting the role of PSMA PET in systemic staging of patients with ccRCC.
Discussion
Detectability of metastatic lesions on PSMA PET relies on neovasculature of tumour and friable tumours without organized neovasculature may not be visible on PSMA PET. FDG PET may be more useful in this subgroup of patients.3 However, this study has demonstrated promising utility of PSMA PET over FDG PET in detecting small lung lesions in patients with ccRCC. This should be considered in a larger multi-centre trial.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- 1.Sankineni S., Brown A., Cieciera M., Choyke P.L., Turkbey B. Imaging of renal cell carcinoma. Urol Oncol. 2016;34:147–155. doi: 10.1016/j.urolonc.2015.05.020. [DOI] [PubMed] [Google Scholar]
- 2.Rhee H., Ng K.L., Tse B.W. Using prostate specific membrane antigen (PSMA) expression in clear cell renal cell carcinoma for imaging advanced disease. Pathology. 2016;48:613–616. doi: 10.1016/j.pathol.2016.05.011. [DOI] [PubMed] [Google Scholar]
- 3.Rhee H., Blazak J., Tham C. Pilot study: use of gallium-68 PSMA PET for detection of metastatic lesions in patients with renal tumour. EJNMMI Res. 2016;6:76. doi: 10.1186/s13550-016-0231-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Win A.Z., Aparici C.M. Clinical effectiveness of (18)f-fluorodeoxyglucose positron emission tomography/computed tomography in management of renal cell carcinoma: a single institution experience. World J Nucl Med. 2015;14:36–40. doi: 10.4103/1450-1147.150535. [DOI] [PMC free article] [PubMed] [Google Scholar]