Abstract
Objectives
We aimed to identify the factors that predict the likelihood of remission based on a health assessment questionnaire (HAQ) in rheumatoid arthritis (RA) patients who received non-tumor necrosis factor (TNF) biologics for six months before they commenced definitive treatment.
Methods
The subjects consisted of 97 RA patients treated with tocilizumab or abatacept for 6 months. The following characteristics were investigated: age, gender, body mass index, steroid and methotrexate dosage, serum matrix metalloproteinase-3 levels, simplified disease activity index (SDAI) score, HAQ score (for assessing the activities of daily living [ADL]) and the short form (SF)-36 score (for assessing the quality of life [QOL]). Remission based on the HAQ score is defined as HAQ ≤0.5 after 6 months of treatment. The subjects were divided into two groups: patients with HAQ score ≤0.5 and HAQ score >0.5, and a retrospective study was conducted.
Results
The group of RA patients who entered remission based on the HAQ (53 patients) had a lower SDAI than the patients who did not enter remission (44 patients), and the RA patients had a lower tender joint count (TJC) and HAQ scores and a lower physician's global assessment (PGA) than those who did not enter remission. The physical component summary score (PCS) and role/social component summary score (RCS) of the SF-36 summary score were higher in the remission patients than in those without. Before the start of the treatment, the HAQ score, patients' global assessment (PtGA) and PCS and mental component summary score (MCS) of the SF-36 were determined based on a logistic regression analysis.
Conclusion
Our findings suggest that RA patients with lower HAQ scores and PtGA and higher PCS and MCS of the SF-36 at baseline are more likely to achieve HAQ remission with non-TNF biologic treatment than others.
Keywords: rheumatoid arthritis, health assessment questionnaire disability index (HAQ-DI), quality of life (QOL), functional remission, non-tumor necrosis factor (TNF)
Introduction
Recommendations regarding the treatment of rheumatoid arthritis (RA) have been well established (1), and the usage of methotrexate (MTX) as an anchor agent, in combination with biological disease-modifying antirheumatic drugs (bDMARDs), has contributed to an increased number of patients achieving clinical remission. As a result of this increase in the rate of clinical remission, the number of patients achieving structural and functional remission has also increased (2). Complete remission in a patient is defined as the achievement of clinical, structural and functional remission (3). Although multiple studies regarding clinical and radiographic remission have been reported to date, there are few reports regarding functional remission. It is important for patients to achieve functional remission as a final treatment outcome. There are reports of health assessment questionnaire (HAQ) remission using a biological agent containing a tumor necrosis factor (TNF) biologic agent. Although analyses of effectiveness and prognostic factors of TNF biologic agents have been frequently reported, there are few reports of non-TNF biologics (tocilizumab or abatacept). Additionally, several reports have addressed the prognostic factors for clinical (4, 5) and radiographic (6) remission; however, no prognostic factors for functional remission have yet been reported.
In this study, we analyzed the relationship between various baseline factors and functional outcomes after six-month non-TNF biologic treatment to determine the prognostic factors for functional remission.
Materials and Methods
A retrospective study was performed in patients treated at a single hospital facility. RA patients who initiated non-TNF bDMARDs treatment from 1 January 2007 to 31 March 2016 were examined. Among 120 patients treated with either or both tocilizumab or abatacept treatment, 97 were deemed eligible to participate as subjects in this study. The non-TNF bDMARDs used in the study were tocilizumab for 72 patients and abatacept for 48 patients, with no other bDMARDs used in any subjects. The selection of bDMARDs was deferred to the primary physician of each patient. The choice between subcutaneous injection and intravenous drip was made by the patient.
The items described below were evaluated at baseline (before the treatment initiation) and six months after the treatment initiation. The patient background items were age, sex, body mass index (BMI), experience of bDMARDs usage (either bio-naïve or bio-switch), disease duration, steroid dosage and MTX dosage. The serological examination included the assessment of matrix metalloproteinase 3 (MMP 3), C-reactive protein (CRP) and the erythrocyte sedimentation rate (ESR). The disease activity was evaluated using the Simplified Disease Activity Index (SDAI) (7). The activities of daily living (ADL) were evaluated using the HAQ disability index (HAQ-DI) (8), and the nonspecific health-related quality of life (QOL) was evaluated using the Short Form 36 (SF 36) (9). The usage of conventional synthetic DMARDs (csDMARDs), adrenocortical steroids (steroids) and non-steroidal anti-inflammatory drugs (NSAIDs) and their dosages before the initiation of biologic treatment as well as patient age or disease duration were not included in the inclusion or exclusion criteria.
As a primary outcome index, HAQ-DI ≤0.5 was defined as functional remission. To determine the relationship between the baseline factors and functional outcomes, the baseline values of each item were analyzed based on the presence or absence of functional remission. The study exclusion criteria included the following: discontinuation of biologic treatment due to primary or secondary response failure or adverse effects; additional oral treatment using csDMARDs agents, steroids, or NSAIDs; complications, such as infection; likelihood of continuing the study because of situations such as hospital transfer, patient withdrawal from the study, or other circumstances that the primary physician deemed inappropriate for the study. For the excluded patients, a last observation carried forward (LOCF) analysis was performed. However, the patients who stopped the treatment regimen after only 3 months were excluded from the analysis.
All of the statistical analyses were performed using univariate and multivariate analyses with the JMP12 software program (SAS Institute, Cary, USA). We obtained written informed consent from all patients who enrolled in the study. The study received approval from the Bio-Ethics Committee of the Department of Medicine, Showa University School of Medicine (No. 1435).
Results
Ninety-seven patients were included in the study, as is shown in Figure. No patient received additional oral treatment with steroids or NSAIDs during the treatment period.
Figure.
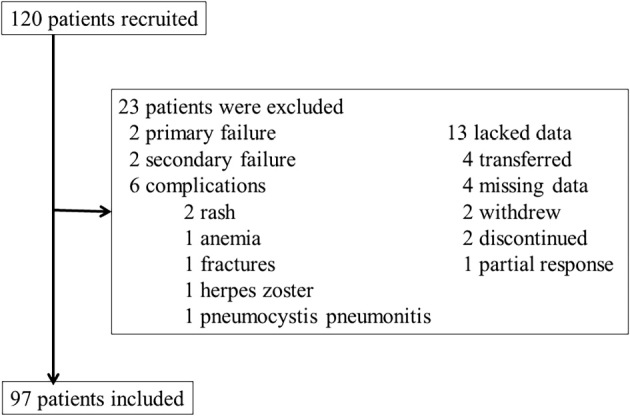
Flow chart of the study.
For the background parameters of the study subjects, there were 53 patients with functional remission (Group A) and 44 with no remission (Group B) (Table 1). Based on the univariate analyses, Group A had a significantly younger age (p=0.001), higher dosage of MTX (p=0.026), lower SDAI at the time of study initiation (p=0.001), lower HAQ-DI (p=0.000), lower tender joint count (TJC) (p=0.000) and lower physician's global assessment (PGA) (p=0.003) than Group B. With regard to the QOL, Group A had significantly higher values for the physical component summary score (PCS) (p=0.000) and role/social component summary score (RCS) (p=0.000) of the SF 36 than Group B.
Table 1.
Univariable Analysis of the Demographics and Baseline Characteristics of 97 RA Patients.
| Remission (Group A) | No remission (Group B) | p | ||
|---|---|---|---|---|
| n | 53 | 44 | ||
| Age (years) | 59 (50-68) | 70 (62-74) | 0.001* | |
| Sex (female, %) | 83 | 80 | 0.860** | |
| Body mass index | 21 (20-24) | 21 (19-25) | 0.830* | |
| Tocilizmab: Abatacept | 28 : 25 | 25 : 19 | 0.851** | |
| Bio (naïve, %) | 49 | 45 | 0.081** | |
| Disease duration (year) | 7 (3-11) | 8 (3-18) | 0.082* | |
| Steroid dosage (mg/d) | 3 (0-5) | 4 (0-5) | 0.229* | |
| MTX dosage (mg/w) | 8 (0-12) | 3 (0-9) | 0.026* | |
| ESR (mm/H) | 28 (16-41) n=52 | 29 (19-55) n=43 | 0.342* | |
| CRP (mg/dL) | 1 (0-3) n=52 | 1 (0-3) n=43 | 0.436* | |
| MMP-3 (ng/mL) | 180 (69-307) n=51 | 229 (123-321) n=43 | 0.271* | |
| SDAI | 20 (15-29) n=52 | 33 (19-37) n=43 | 0.001* | |
| TJC | 4 (2-8) | 8 (4-14) n=43 | 0.000* | |
| SJC | 3 (2-6) | 5 (2-9) n=43 | 0.080* | |
| PtGA | 52 (25-70) | 60 (40-75) n=43 | 0.156* | |
| PGA | 49 (26-66) | 66 (42-75) n=43 | 0.003* | |
| HAQ-DI | 0.125 (0-0.250) n=52 | 1 (0.750-1.375) n=41 | 0.000* | |
| SF-36 | PCS | 34 (22-42) n=48 | 19 (11-26) n=42 | 0.000* |
| MCS | 50 (43-57) n=48 | 52 (43-58) n=42 | 0.822* | |
| RCS | 47 (40-54) n=48 | 35 (25-39) n=42 | 0.000* | |
MTX: methotrexate
MMP-3: matrix metalloproteinase 3
SDAI: simplified disease activity index
TJC: tender joint count
SJC: swollen joint count
PtGA: patient’s global assessment
PGA: physician’s global assessment
HAQ-DI: health assessment questionnaire disability index
SF-36: short form-36
PCS: physical component summary score
MCS: mental component summary score
RCS: role/social component summary score
*analysis using Mann-Whitney U test
**analysis using chi-squared test for independence test
The findings of the multivariate analyses findings were as follows: patient's global assessment (PtGA) (p=0.0038, odds ratio: 1.080, 95% CI: 1.025-1.138), HAQ-DI (p=0.0004, odds ratio: 49.3, 95% CI: 5.8-416.7), PCS (p=0.0128, odds ratio: 1.132, 95% CI: 1.027-1.248) and mental component summary score (MCS) of the SF-36 (p=0.0359, odds ratio: 1.102, 95% CI: 1.006-1.206) (Table 2).
Table 2.
Prognostic Factor Identified by Multivariate Analysis Showing a Significant Association with Functional Remission.
| Remission | No remission | Odd ratio (95% CI) | p | |
|---|---|---|---|---|
| PtGA | 52 (25-70) n=53 | 60 (40-75) n=43 | 1.080 (1.025-1.138) | 0.0038 |
| HAQ-DI | 0 (0-1) n=52 | 1 (1-1) n=41 | 49.3 (5.8-416.7) | 0.0004 |
| PCS | 34 (22-42) n=48 | 19 (11-26) n=42 | 1.132 (1.027-1.248) | 0.0128 |
| MCS | 50 (43-57) n=48 | 52 (43-58) n=42 | 1.102 (1.006-1.206) | 0.0359 |
TJC: tender joint count
PtGA: patient’s global assessment
HAQ-DI: health assessment questionnaire disability index
PCS: physical component summary score
MCS: mental component summary score
Discussion
In the present study, we determined that a lower PtGA and HAQ-DI and higher PCS and MCS of the SF-36 at baseline were prognostic factors for functional remission after six months of non-TNF bDMARD treatment. Although the disease activity, age, and sex were expected to influence the functional outcomes, our analyses did not find those variables to be prognostic factors.
Multiple studies regarding RA prognostic factors have been reported (10). According to the literature, good prognostic factors for remission from disease activity include the following: male sex, young age, late-onset RA, short disease duration, nonsmoking status, low baseline disease activity, mild functional impairment, low baseline radiographic damage, absence of rheumatoid factor (RF) and anti-cyclic citrullinated peptide (CCP), low serum level of acute-phase reactant, interleukin (IL) 2, and receptor activator of nuclear factor kappa-B ligand (RANKL) at baseline, early treatment using csDMARD combinations, the use of anti-TNF, concurrent use of DMARDs in anti-TNF-treated patients, and a moderate or good response to treatments during the first six months. A study on radiographic remission reported that MTX in combination with etanercept resulted in a better radiographic remission rate than MTX alone (11). After this report was published, similar outcomes were reported with other biologic agents (12). As a prognostic factor for complete remission, very early RA was reported (13). None of these studies, however, focused on functional remission. The results regarding the SF-36 vary depending on each component. The PCS involvement may be related to a low HAQ. However, since we did not evaluate any other depressive state in the patients, the association between the PCS and MCS could not be clarified in this study.
Several limitations associated with the present study warrant mention. First, we did not perform a radiographic evaluation of the joints, although the radiographic findings are expected to influence the Damage-HAQ (14). The Total Sharp/van der Heijde Sharp score is one of the factors influencing functional remission, and it is determined using a logistic regression analysis. Although the HAQ-DI contributed to functional remission according to a multiple logistic regression analysis, the modified total vdH-Sharp score did not play a role during abatacept treatment in RA patients (15, 16). In addition, because a radiographic evaluations was only performed in 50 patients, the subjects were analyzed without accounting for radiographic findings. Second, we used actual clinical data accumulated over a long period of time, generating a bias in the biologics used in this study; therefore, the clinical outcomes may be different, depending on the type of biologic treatment applied. Third, the study design is not a prospective study but a retrospective one. Finally, no socioeconomic factors were included in our analysis.
Non-TNF bDMARDs for the treatment of RA demonstrate efficacy, leading to clinical remission as well as radiographic remission in many cases. Good baseline HAQ-DI scores, TJC and PtGA, however, prevent functional remission. This finding is considered to be a limitation of non-TNF bDMARDs treatment. Achieving functional remission will require the establishment of a novel therapy algorithm.
In conclusion, our study demonstrated that RA patients with lower HAQ scores, and PtGA and higher PCS and MCS of the SF-36 at baseline are more likely to achieve HAQ remission with non-TNF biologic treatment than other patients.
Author's disclosure of potential Conflicts of Interest (COI).
Yusuke Miwa: Research funding, Astellas Pharma, Mitsubishi Tanabe Pharma, AbbVie, Pfizer Japan, Chugai Pharmaceutical and Eizai. Tsuyoshi Kasama: Research funding, Mitsubishi Tanabe Pharma and AbbVie.
Acknowledgement
Cooperation on data collection: All Showa University in Rheumatoid Arthritis (ASHURA) group; Nobuyuki Yajima, Takeo Isozaki, Kuninobu Wakabayashi, Ryo Takahashi, Takahiro Tokunaga, Sakiko Isojima, Masayu Umemura, Nao Oguro, Yoko Miura, Sho Ishii, Shinya Seki, Shinichiro Nishimi, Airi Nishimi, Mika Hatano and Kosuke Sakurai
Data entry and management: Hiroka Mitsuhashi and Yuko Mitamura
References
- 1. Singh JA, Saag KG, Bridges SL Jr, et al. 2015 American College of Rheumatology Guideline for the Treatment of Rheumatoid Arthritis. Arthritis Rheumatol 68: 1-26, 2016. [DOI] [PubMed] [Google Scholar]
- 2. Haugeberg G, Boyesen P, Helgetveit K, Proven A. Clinical and radiographic outcomes in patients diagnosed with early rheumatoid arthritis in the first years of the biologic treatment era: a 10-year prospective observational study. J Rheumatol 42: 2279-2287, 2015. [DOI] [PubMed] [Google Scholar]
- 3. Izumi K, Kaneko Y, Yasuoka H, et al. Tocilizumab is clinically, functionally, and radiographically effective and safe either with or without low-dose methotrexate in active rheumatoid arthritis patients with inadequate responses to DMARDs and/or TNF inhibitors: a single-center retrospective cohort study (KEIO-TCZ study) at week 52. Mod Rheumatol 25: 31-37, 2015. [DOI] [PubMed] [Google Scholar]
- 4. Kojima M, Kojima T, Suzuki S, et al. Patient-reported outcomes as assessment tools and predictors of long-term prognosis: a 7-year follow-up study of patients with rheumatoid arthritis. Int J Rheum Dis 2015(Epub ahead of print). [DOI] [PubMed] [Google Scholar]
- 5. Odai T, Matsunawa M, Takahashi R, et al. Correlation of CX3CL1 and CX3CR1 levels with response to infliximab therapy in patients with rheumatoid arthritis. J Rheumatol 36: 1158-1165, 2009. [DOI] [PubMed] [Google Scholar]
- 6. Bathon J, Robles M, Ximenes AC, et al. Sustained disease remission and inhibition of radiographic progression in methotrexate-naive patients with rheumatoid arthritis and poor prognostic factors treated with abatacept: 2-year outcomes. Ann Rheum Dis 70: 1949-1956, 2011. [DOI] [PubMed] [Google Scholar]
- 7. Aletaha D, Ward MM, Machold KP, Nell VP, Stamm T, Smolen JS. Remission and active disease in rheumatoid arthritis: defining criteria for disease activity states. Arthritis Rheum 52: 2625-2636, 2005. [DOI] [PubMed] [Google Scholar]
- 8. Ziebland S, Fitzpatrick R, Jenkinson C, Mowat A. Comparison of two approaches to measuring change in health status in rheumatoid arthritis: the Health Assessment Questionnaire (HAQ) and modified HAQ. Ann Rheum Dis 51: 1202-1205, 1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Fukuhara S, Bito S, Green J, Hsiao A, Kurokawa K. Translation, adaptation, and validation of the SF-36 Health Survey for use in Japan. J Clin Epidemiol 51: 1037-1044, 1998. [DOI] [PubMed] [Google Scholar]
- 10. Katchamart W, Johnson S, Lin HJ, Phumethum V, Salliot C, Bombardier C. Predictors for remission in rheumatoid arthritis patients: A systematic review. Arthritis Care Res (Hoboken) 62: 1128-1143, 2010. [DOI] [PubMed] [Google Scholar]
- 11. van der Heijde D, Landewe R, van Vollenhoven R, Fatenejad S, Klareskog L. Level of radiographic damage and radiographic progression are determinants of physical function: a longitudinal analysis of the TEMPO trial. Ann Rheum Dis 67: 1267-1270, 2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Ciubotariu E, Gabay C, Finckh A. Joint damage progression in patients with rheumatoid arthritis in clinical remission: do biologics perform better than synthetic antirheumatic drugs? J Rheumatol 41: 1576-1582, 2014. [DOI] [PubMed] [Google Scholar]
- 13. Bosello S, Fedele AL, Peluso G, Gremese E, Tolusso B, Ferraccioli G. Very early rheumatoid arthritis is the major predictor of major outcomes: clinical ACR remission and radiographic non-progression. Ann Rheum Dis 70: 1292-1295, 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Smolen JS, Aletaha D, Grisar JC, Stamm TA, Sharp JT. Estimation of a numerical value for joint damage-related physical disability in rheumatoid arthritis clinical trials. Ann Rheum Dis 69: 1058-1064, 2010. [DOI] [PubMed] [Google Scholar]
- 15. Takeuchi T, Tanaka Y, Amano K, et al. Clinical, radiographic and functional effectiveness of tocilizumab for rheumatoid arthritis patients--REACTION 52-week study. Rheumatology (Oxford) 50: 1908-1915, 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Yamazaki H, Hirano F, Takeuchi T, et al. Simplified Disease Activity Index remission at month 6 is an independent predictor of functional and structural remissions at month 12 during abatacept treatment in patients with rheumatoid arthritis: A multi-center, prospective cohort study in Japan. Mod Rheumatol 2016(Epub ahead of print). [DOI] [PubMed] [Google Scholar]


