Abstract
Introduction:
Percutaneous nephrolithotomy (PCNL) is an effective treatment for renal stones. Due to the significant pain and morbidity after standard PCNL because of nephrostomy tubes, various modifications of PCNL are being performed. We report a randomized trial comparing these modalities.
Materials and Methods:
A total of 75 patients were randomized into three groups of 25 each: standard PCNL with nephrostomy tubes (Group 1), tubeless PCNL with ureteric stent and no nephrostomy (Group 2), and totally tubeless PCNL without ureteric catheter or nephrostomy (Group 3). Randomization was done at the end of the procedure for those patients satisfying the inclusion criteria based on duration of surgery, single puncture tract, intraoperative bleeding, stone burden, intact pelvicalyceal system, and no residual stones at the end of procedure. The outcomes measured were hemoglobin (Hb) drop, hemorrhage, need for blood transfusion, pyrexia, urine leak, pain score, analgesic requirement, and duration of hospital stay.
Results:
There was no significant difference in hemorrhage, Hb drop, need for blood transfusion, and postoperative pyrexia among the groups. All patients except one in the standard group only had variable amount of urinary leak. The analgesic requirement and duration of hospital stay attained statistical significance in favor of tubeless and totally tubeless groups compared to the standard.
Conclusions:
Tubeless and totally tubeless PCNL are safe and effective method of renal stone management. Totally tubeless PCNL significantly reduced postoperative pain and morbidity compared to the tubeless method.
INTRODUCTION
Percutaneous nephrolithotomy (PCNL) is a minimally invasive treatment modality for the management of renal calculi. First introduced in 1976,[1] PCNL was associated with morbidities such as bleeding, pyrexia, incomplete stone removal, pleural injury, and adjacent organ injury.[2] Refinements in the technique, optics of the instruments, and better lithotripsy technologies have led to a reduction in these morbidities. In the standard PCNL procedure, after stone removal, a nephrostomy is placed. Studies showed that smaller nephrostomy tubes were as effective as larger ones.[3,4,5] The presence and removal of nephrostomy is associated with morbidities such as infection, pain, urine leak, bleeding, and prolonged hospitalization.[6] Tubeless PCNL was then introduced with the insertion of a double J ureteric stent following PCNL. However, the presence of double-J stent in tubeless PCNL is often associated with stent-related problems such as frequency, urgency, nocturia, pain, and hematuria.[7] Totally tubeless PCNL was reintroduced to minimize these problems. Although there are randomized controlled studies comparing any two of the standard, tubeless or totally tubeless PCNL, a randomized controlled study comparing all the three techniques together is not known. The aim of this study is to determine whether tubeless and totally tubeless PCNL are safe and less morbid management techniques for renal stones compared to the standard PCNL with nephrostomy tube.
MATERIALS AND METHODS
This randomized controlled study was approved by the Institutional Review Board and included patients who gave consent for randomization and underwent PCNL at our hospital. The inclusion criteria were <3 stones, size <3 cm, single puncture tract, PCNL lasting <2 h, complete clearance of stones as ensured by fluoroscopy and endoscopy, no significant bleeding, and intact pelvicalyceal system at the end of procedure. Patients with renal anatomical abnormalities, staghorn calculus, active urinary tract infections, coagulopathy, and those who are unfit for general anesthesia were excluded from the study. Preoperatively, all the patients were evaluated with blood and urine routine examinations, renal function studies, urine culture, coagulation profile, and computed tomography (CT) scan. Under aseptic precaution, a ureteral catheter was introduced into the renal pelvis. The patient was then turned prone, and percutaneous access into the corresponding pelvicalyceal system was achieved under image intensification using an 18-gauge needle. The tract was then dilated using a single-step 30 F Amplatz dilator. Renal stones were fragmented using ballistic lithotripsy. All the surgeries were done by a single surgeon (SB).
Randomization was done only for those patients satisfying the inclusion criteria based on the duration of surgery, single puncture tract, intraoperative bleeding, stone burden, intact pelvicalyceal system following surgery, and no residual stones at the end of procedure. The patients were divided into three groups: Group 1 in which after the procedure, a 22 F nephrostomy tube was inserted into the pelvicalyceal system (standard); Group 2 with ureteral stent and without nephrostomy (tubeless); and Group 3 included neither nephrostomy nor stent (totally tubeless). Twenty-five patients were included in each group. A study by Tefekli et al. comparing postoperative hemoglobin (Hb) drop between tubeless and standard groups was taken as the reference for ascertaining the sample size of this study.[8] The randomization allocation was done by using random number generator, and allocation concealment was done by sequentially numbered opaque-sealed envelope which was opened at the end of stone removal.
Patients were monitored closely in the postoperative period for the following (a) bleeding which is defined as gross hematuria from the nephrostomy in standard group, whereas it is defined as gross hematuria in catheterized urine or visible voided hematuria after catheter removal in tubeless and totally tubeless groups,[9] (b) postoperative Hb drop, (c) requirement of any blood transfusions, (d) pyrexia by maintaining temperature chart, (e) urine leak, (f) postoperative pain assessed 24 h postoperatively by visual analog scale, (g) requirement of analgesia based on the WHO guidelines[10] in which patients were initially given nonopioid drug paracetamol; if there was no pain relief, an opioid drug tramadol was added, and (h) duration of hospital stay. In all the groups, patients were discharged with stable vital signs and no complications. The hospital readmission details if any were also recorded.
The data were coded and entered into Microsoft Excel and analyzed using SPSS software version 16 SPSS Inc., Chicago, USA. Chi-square test and t-test were used for finding association between qualitative and quantitative data, respectively. For comparing the variables between the three groups, ANOVA was used for parametric values and Kruskal–Wallis and Mann–Whitney tests were used for nonparametric values. Post hoc test was done to compare the differences between any two groups.
RESULTS
The clinicodemographic characteristics of the study were comparable between groups and are listed in Table 1. The operative complications and the main outcomes of the study are listed in Table 2.
Table 1.
Clinicodemographic characteristics
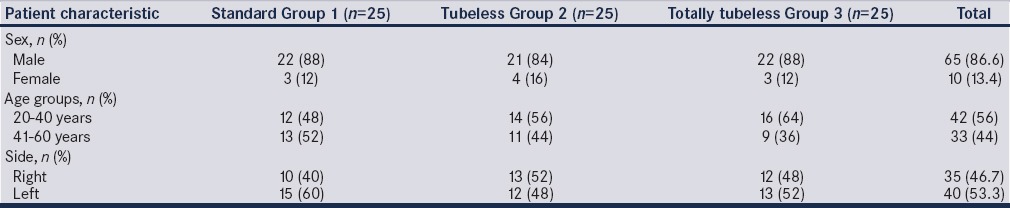
Table 2.
Main outcomes and complications
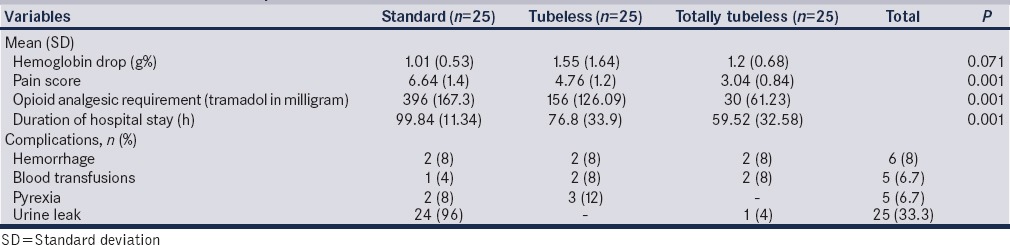
The mean Hb drop in the three groups [Table 2] was not found to be statistically significant with F = 2.75 and P = 0.071. Out of the 75 patients, two patients in each group had bleeding postoperatively. Among these, five patients required blood transfusion and one patient in standard group was managed without blood transfusion. Only five patients developed pyrexia in the postoperative period. The differences in the need for blood transfusion and postoperative pyrexia were not found to be statistically significant with χ2 = 0.429 and 3.0 and P = 0.807 and 0.22, respectively [Table 2].
Twenty-four patients in standard group and one patient in totally tubeless group developed urine leak through the wound postoperatively, but none in the tubeless group developed urine leak. Residual stones were not detected on plain CT scan of abdomen in these patients. The urine leak lasted for 2–14 days and resolved spontaneously. The difference was found to be statistically significant with χ2 = 66.36 and P = 0.001. Comparing tubeless and totally tubeless groups, the difference was not found to be statistically significant with P = 0.312 [Table 2].
There was a statistically significant difference in pain score between the different groups (P = 0.001). There was a statistically significant difference in pain score between tubeless and totally tubeless groups with P = 0.001 [Table 2].
The difference in mean opioid analgesic requirement (tramadol) between the groups was found to be statistically significant with F = 54.530 and P = 0.001 [Table 2]. There is a significant difference in opioid analgesic requirement between tubeless and totally tubeless groups.
The duration of hospital stay between the groups was found to be statistically significant with F = 13.102 and P = 0.001 [Table 2]. However, there was no significant difference in hospital stay between tubeless and totally tubeless groups.
DISCUSSION
PCNL is the standard method for removal of large stones. Since its first description in 1976 by Fernström and Johansson,[1] considerable changes have occurred in the techniques and technology of PCNL. After completion of stone removal, traditionally, a nephrostomy tube is placed. This helped in tamponade of bleeding, drainage of urine, tract recovery, and a guide for second look nephroscopy if needed.[11,12] However, in the beginning, large bore tubes were used leading to pain and discomfort to the patients. Maheshwari et al. and Desai et al. showed that smaller caliber tubes were equally effective for this purpose, thus reducing pain, need for analgesics, urine leak, and duration of hospital stay.[3,5]
Totally tubeless PCNL was first described by Wickham et al. in 1984.[13] Winfield et al. in 1986 also reported two cases of totally tubeless PCNL.[14] However, due to prolonged hospitalization, increased analgesic requirement, and significant inconveniences to the patients, this practice was given up. Bellman et al. in 1997 first described “tubeless” PCNL which involved placement of a ureteric stent without nephrostomy.[15] Goh and Wolf in 1999 proposed “almost totally tubeless” PCNL wherein an externalized ureteric catheter was retained for 1–2 days and they concluded that PCNL without nephrostomy is effective, safe, and reduced the morbidity.[16] Several studies in the recent years have reported the success and advantages of totally tubeless PCNL.[17,18,19,20,21]
Hemorrhage is the most significant complication of PCNL requiring blood transfusion in 3%–12% of cases.[22,23,24] A meta-analysis of standard versus tubeless PCNL by Borges et al. showed that there was no difference in Hb drop between tubeless and standard PCNL (P = 0.09).[6] In the study by Tefekli et al., the mean Hb drop (g%) in standard and tubeless PCNL was 1.3 and 1.7, respectively.[8] In our study, the difference in mean Hb drop in standard, tubeless, and totally tubeless groups was not found to be statistically significant (F = 2.75, P = 0.07). A total of six patients had postoperative bleeding and five patients were managed with blood transfusion and spontaneous resolution occurred in one patient [Table 2]. Single-step totally tubeless PCNL did not lead to significant hemorrhagic complications compared to other groups.
Fever following PCNL is a significant complication. However, a study by Jou et al. showed that postoperative fever was common in those patients with residual fragments. Stone burden, composition and duration of surgery did not produce increased incidence of fever in these patients who underwent PCNL.[25] A study by Sharifi Aghdas et al. found the incidence of postoperative fever to be more in patients with nephrostomy.[26] Fever which is mostly seen on the first or second postoperative days has a low risk of progressing to a life-threatening condition. In our study, five patients had fever in the postoperative period out of which three were from tubeless and the other two were from the standard group. None of the patients in totally tubeless group had fever and the difference was statistically insignificant (P = 0.22). In the meta-analysis of six trials by Borges et al., postoperative fever did not attain any statistical difference between the groups.[6]
Urinary leak is not an uncommon problem following PCNL and varied from 0% to 11.1%.[6] This could be due to retained fragments, blood clots, infundibular narrowing, mucosal edema, etc., Though it is difficult to quantify, urine leak persisting 48 h following nephrostomy removal is considered as prolonged urine leakage. The important risk factors for urine leak persisting for 48 h or more depend on stone complexity, severity of hydronephrosis, thickness of renal parenchyma, intraparenchymal renal pelvis, multiple punctures, surgeons's experience, and residual stones.[27] Most of these subside over a period of time. The meta-analysis by Borges et al. reported urine leak to be lower in tubeless group compared to standard group (P = 0.0002).[6] In our study, all except one patient in the standard PCNL group had postoperative urinary leak following removal of nephrostomy. Only one patient in the totally tubeless group had postoperative urinary leak. None of the tubeless patients had urinary leak. The difference was found to be statistically significant (P = 0.001) though no difference was noted between tubeless and totally tubeless groups (P = 0.312). The urine leak may be due to the temporary edema at the pelviureteric junction due to the trauma of lithotripsy or may be due to the maturation of tissues and establishing an anomalous tract.[6]
The presence of a foreign body like nephrostomy tube or double J stent is frequently associated with pain. Visual analog scale was used for pain assessment 24 h after surgery. The mean pain score in standard, tubeless, and totally tubeless groups was 6.64, 4.76, and 3.04, respectively, in our study with a statistically significant difference between the groups (P = 0.001). A significant difference was also noted in pain scores between tubeless and totally tubeless groups (P = 0.001). In a study by Agrawal et al., the mean pain score was 5.9 and 3.1 in standard and tubeless groups, respectively (P ≤ 0.01).[28]
Analgesics were given according to the WHO guidelines.[10] The mean opioid analgesic requirement (tramadol in milligram) was in favor of tubeless and totally tubeless groups compared to standard group and the difference was statistically significant (P = 0.001). Agrawal et al. showed mean opioid analgesic requirement with significant difference between standard and tubeless groups (P = 0.001).[28] The mean duration of hospital stay in standard, tubeless, and totally tubeless groups was 99.84, 76.8, and 59.5 h, respectively, and the difference was statistically significant (P = 0.001). The meta-analysis by Borges et al. noted a significant reduction in duration of hospital stay in tubeless PCNL compared to the standard group (P = 0.00001).[6] Crook et al. showed mean duration of hospital stay in standard and tubeless groups to be 80.64 and 55.66 h, respectively (P = 0.05).[9] The duration of hospital stay did not show a statistical difference in a study by Abbott et al.[29] In a study by Mandhani et al., the analgesic requirement and duration of hospital stay were comparable between the tubeless and totally tubeless groups and concluded that PCNL without nephrostomy or ureteric stent was a safe procedure in selected patients.[30] A study by Moosanejad et al. showed that totally tubeless PCNL is a safe and effective technique and is associated with decreased pain, analgesic need, and length of hospitalization.[31]
CONCLUSIONS
Tubeless and totally tubeless PCNL are safe and effective methods of renal stone management. These modifications in the PCNL technique help in reducing pain, analgesic requirement, urinary leak, and postoperative fever, thereby favoring early hospital discharge. Early discharge also helps in reducing the financial burden to the patient. The need for analgesia is less in totally tubeless PCNL compared to tubeless method.
Financial support and sponsorship
This study was financially supported by the State board of medical research.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We wish to acknowledge Dr. Binu Areekkal, associate professor of community medicine, Government Medical College, Kottayam, for his help and support in the statistical analysis of this study.
REFERENCES
- 1.Fernström I, Johansson B. Percutaneous pyelolithotomy. A new extraction technique. Scand J Urol Nephrol. 1976;10:257–9. doi: 10.1080/21681805.1976.11882084. [DOI] [PubMed] [Google Scholar]
- 2.de la Rosette J, Assimos D, Desai M, Gutierrez J, Lingeman J, Scarpa R, et al. The Clinical Research Office of the Endourological Society Percutaneous Nephrolithotomy Global Study: Indications, complications, and outcomes in 5803 patients. J Endourol. 2011;25:11–7. doi: 10.1089/end.2010.0424. [DOI] [PubMed] [Google Scholar]
- 3.Maheshwari PN, Andankar MG, Bansal M. Nephrostomy tube after percutaneous nephrolithotomy: Large-bore or pigtail catheter? J Endourol. 2000;14:735–7. doi: 10.1089/end.2000.14.735. [DOI] [PubMed] [Google Scholar]
- 4.Pietrow PK, Auge BK, Lallas CD, Santa-Cruz RW, Newman GE, Albala DM, et al. Pain after percutaneous nephrolithotomy: Impact of nephrostomy tube size. J Endourol. 2003;17:411–4. doi: 10.1089/089277903767923218. [DOI] [PubMed] [Google Scholar]
- 5.Desai MR, Kukreja RA, Desai MM, Mhaskar SS, Wani KA, Patel SH, et al. A prospective randomized comparison of type of nephrostomy drainage following percutaneous nephrostolithotomy: Large bore versus small bore versus tubeless. J Urol. 2004;172:565–7. doi: 10.1097/01.ju.0000130752.97414.c8. [DOI] [PubMed] [Google Scholar]
- 6.Borges CF, Fregonesi A, Silva DC, Sasse AD. Systematic review and meta-analysis of nephrostomy placement versus tubeless percutaneous nephrolithotomy. J Endourol. 2010;24:1739–46. doi: 10.1089/end.2010.0231. [DOI] [PubMed] [Google Scholar]
- 7.Saltzman B. Ureteral stents. Indications, variations, and complications. Urol Clin North Am. 1988;15:481–91. [PubMed] [Google Scholar]
- 8.Tefekli A, Altunrende F, Tepeler K, Tas A, Aydin S, Muslumanoglu AY. Tubeless percutaneous nephrolithotomy in selected patients: A prospective randomized comparison. Int Urol Nephrol. 2007;39:57–63. doi: 10.1007/s11255-006-9040-6. [DOI] [PubMed] [Google Scholar]
- 9.Crook TJ, Lockyer CR, Keoghane SR, Walmsley BH. A randomized controlled trial of nephrostomy placement versus tubeless percutaneous nephrolithotomy. J Urol. 2008;180:612–4. doi: 10.1016/j.juro.2008.04.020. [DOI] [PubMed] [Google Scholar]
- 10.Cancer pain relief: With a guide to opioid availability. 2nd ed. Geneva: WHO; 1996. WHO Guidelines: World Health Organization. [Google Scholar]
- 11.Paul EM, Marcovich R, Lee BR, Smith AD. Choosing the ideal nephrostomy tube. BJU Int. 2003;92:672–7. doi: 10.1046/j.1464-410x.2003.04454.x. [DOI] [PubMed] [Google Scholar]
- 12.Srinivasan AK, Herati A, Okeke Z, Smith AD. Renal drainage after percutaneous nephrolithotomy. J Endourol. 2009;23:1743–9. doi: 10.1089/end.2009.1545. [DOI] [PubMed] [Google Scholar]
- 13.Wickham JE, Miller RA, Kellett MJ, Payne SR. Percutaneous nephrolithotomy: One stage or two? Br J Urol. 1984;56:582–5. doi: 10.1111/j.1464-410x.1984.tb06121.x. [DOI] [PubMed] [Google Scholar]
- 14.Winfield HN, Weyman P, Clayman RV. Percutaneous nephrostolithotomy: Complications of premature nephrostomy tube removal. J Urol. 1986;136:77–9. doi: 10.1016/s0022-5347(17)44733-1. [DOI] [PubMed] [Google Scholar]
- 15.Bellman GC, Davidoff R, Candela J, Gerspach J, Kurtz S, Stout L. Tubeless percutaneous renal surgery. J Urol. 1997;157:1578–82. [PubMed] [Google Scholar]
- 16.Goh M, Wolf JS., Jr Almost totally tubeless percutaneous nephrolithotomy: Further evolution of the technique. J Endourol. 1999;13:177–80. doi: 10.1089/end.1999.13.177. [DOI] [PubMed] [Google Scholar]
- 17.Bdesha AS, Jones CR, North EA, Pinfield J, Boyd PJ. Routine placement of a nephrostomy tube is not necessary after percutaneous nephrostolithotomy. Br J Urol. 1997;79(Suppl 4):1. [Google Scholar]
- 18.Karami H, Gholamrezaie HR. Totally tubeless percutaneous nephrolithotomy in selected patients. J Endourol. 2004;18:475–6. doi: 10.1089/0892779041271580. [DOI] [PubMed] [Google Scholar]
- 19.Aghamir SM, Hosseini SR, Gooran S. Totally tubeless percutaneous nephrolithotomy. J Endourol. 2004;18:647–8. doi: 10.1089/end.2004.18.647. [DOI] [PubMed] [Google Scholar]
- 20.Gupta V, Sadasukhi TC, Sharma KK, Yadav RG, Mathur R. Tubeless and stentless percutaneous nephrolithotomy. BJU Int. 2005;95:905–6. doi: 10.1111/j.1464-410X.2005.05432.x. [DOI] [PubMed] [Google Scholar]
- 21.Crook TJ, Lockyer CR, Keoghane SR, Walmsley BH. Totally tubeless percutaneous nephrolithotomy. J Endourol. 2008;22:267–71. doi: 10.1089/end.2006.0034. [DOI] [PubMed] [Google Scholar]
- 22.Jones DJ, Russell GL, Kellett MJ, Wickham JE. The changing practice of percutaneous stone surgery. Review of 1000 cases 1981-1988. Br J Urol. 1990;66:1–5. doi: 10.1111/j.1464-410x.1990.tb14852.x. [DOI] [PubMed] [Google Scholar]
- 23.Patterson DE, Segura JW, LeRoy AJ, Benson RC, Jr, May G. The etiology and treatment of delayed bleeding following percutaneous lithotripsy. J Urol. 1985;133:447–51. doi: 10.1016/s0022-5347(17)49015-x. [DOI] [PubMed] [Google Scholar]
- 24.el-Kenawy MR, el-Kappany HA, el-Diasty TA, Ghoneim MA. Percutaneous nephrolithotripsy for renal stones in over 1000 patients. Br J Urol. 1992;69:470–5. doi: 10.1111/j.1464-410x.1992.tb15590.x. [DOI] [PubMed] [Google Scholar]
- 25.Jou YC, Lu CL, Chen FH, Shen CH, Cheng MC, Lin SH, et al. Contributing factors for fever after tubeless percutaneous nephrolithotomy. Urology. 2015;85:527–30. doi: 10.1016/j.urology.2014.10.032. [DOI] [PubMed] [Google Scholar]
- 26.Sharifi Aghdas F, Akhavizadegan H, Aryanpoor A, Inanloo H, Karbakhsh M. Fever after percutaneous nephrolithotomy: Contributing factors. Surg Infect (Larchmt) 2006;7:367–71. doi: 10.1089/sur.2006.7.367. [DOI] [PubMed] [Google Scholar]
- 27.Ansari H, Tomar V, Yadav SS, Agarwal N. Study of predictive factors affecting the prolonged urinary leakage after percutaneous nephrolithotomy. Urol Ann. 2016;8:60–5. doi: 10.4103/0974-7796.164856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Agrawal MS, Agrawal M, Gupta A, Bansal S, Yadav A, Goyal J. A randomized comparison of tubeless and standard percutaneous nephrolithotomy. J Endourol. 2008;22:439–42. doi: 10.1089/end.2007.0118. [DOI] [PubMed] [Google Scholar]
- 29.Abbott JE, Deem SG, Mosley N, Tan G, Kumar N, Davalos JG. Are we fearful of tubeless percutaneous nephrolithotomy? Assessing the need for tube drainage following percutaneous nephrolithotomy. Urol Ann. 2016;8:70–5. doi: 10.4103/0974-7796.162214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mandhani A, Goyal R, Vijjan V, Dubey D, Kapoor R. Tubeless percutaneous nephrolithotomy – Should a stent be an integral part? J Urol. 2007;178(3 Pt 1):921–4. doi: 10.1016/j.juro.2007.05.021. [DOI] [PubMed] [Google Scholar]
- 31.Moosanejad N, Firouzian A, Hashemi SA, Bahari M, Fazli M. Comparison of totally tubeless percutaneous nephrolithotomy and standard percutaneous nephrolithotomy for kidney stones: A randomised, clinical trial. Braz J Med Biol Res. 2016;49:e4878. doi: 10.1590/1414-431X20154878. [DOI] [PMC free article] [PubMed] [Google Scholar]


