Abstract
Introduction
Globally, maternal age is identified as an important predictor of institutional service utilization during delivery. This study aims to assess the correlates of institutional delivery among teenage and non-teenage mothers in Nepal by using the data from Nepal Demographic and Health Survey 2011.
Methods
The study population consisted of 5391 women of reproductive age (15–49 years) who had given birth to a child within five years before the survey. Out of them, 381 (7.07%) were teenage mothers. The association between the background characteristics and institutional delivery was assessed separately for the teenage and non-teenage mothers using chi-square test and multiple logistic regression analysis.
Results
After adjusting for background characteristics, teenage mothers were found more likely to deliver at a health facility [AOR: 2.25; 95% CI: 1.10 4.59] in comparison to the non-teenage mothers. Place of residence, occupation, socioeconomic status, and frequency of ANC visits were associated with institutional delivery in both the teenage and non-teenage mothers. However, educational status, parity, birth preparedness and women autonomy had statistically significant association with institutional delivery among the non-teenage mothers only. None of the background characteristics were significantly associated with institutional delivery in teenage mothers only.
Conclusions
This study identified a significant difference in institutional delivery service utilization among the teenage and non-teenage mothers. While the association of most of the background characteristics with institutional delivery was uniform for both teenage and non-teenage mothers, the association with educational status, parity, birth preparedness and women autonomy was significant only for non-teenage mothers. Considering this difference in the interaction of women’s background characteristics with institutional delivery between teenage and non-teenage mothers might help in identifying the pain points and devise targeted interventions to encourage institutional delivery in teenage mothers or non-teenage mothers or both.
Introduction
Despite the notable progress in reducing maternal deaths around the world by 43% over 25 years since 1990, approximately 830 women die every day due to perinatal complications [1]. Nearly 99% of these deaths occur in developing countries like Nepal.
Acknowledging the need for programs to reduce preventable maternal deaths, the Government of Nepal (GoN) has implemented programs like user fee exemption, travel incentives for delivery at health facilities, and provision of 24-hour emergency obstetric services to enhance institutional deliveries by skilled birth attendants. To encourage delivery at health facilities and make pregnancy and childbirth safer, health posts are being gradually upgraded to include birthing centers [2]. As a result, some progress has been achieved. Nepal has been successful in increasing institutional delivery from 8% to 35% in between 1996 and 2011 [3,4], and in reducing maternal mortality ratio from 539 to 190 per 100,000 live births in between 1995 and 2015 [5].
Still, several challenges remain in further reducing the maternal deaths. The remoteness of health facilities is one of the challenges. Health institutions are inaccessible in many rural sites and the available health services are underutilized [6]. A recent study linked longer distance of hospital from home with unaccounted costs that possibly prevent utilization of health services in rural Nepal, especially among poor households [7].
About 17 percent of adolescent women aged 15–19 years are already mothers or pregnant with the first child. Majority of newly married women are teenagers as reflected by the median age at marriage among women aged 25–49 years [4]. In these young mothers, poor pregnancy outcomes and negative social consequences are common. Teenage mothers who find themselves biologically fit to deliver a baby may be struck by a myriad of problems that range from marital instability, sexual harassment to depressive symptoms [8,9]. Compared with older women, teenage mothers are at higher risk of maternal death [10] but are less likely to use maternal health services [11]. In response to these specific needs of teenage mothers, GoN has developed the National Reproductive Health Strategy 1998 and has integrated adolescent sexual and reproductive health issues in national long-term program and plans in a row. Despite these policy and programmatic level plans and commitments, reduction in teenage pregnancy rate is very slow and Nepal still has one of the highest teenage pregnancy rates in South Asia [12,13]. For these reasons, teenage pregnancy remains a huge challenge in further reduction of maternal mortality in Nepal.
In terms of research, the effect of mother’s age on the utilization of maternal health services has been studied frequently; however, the determinants of maternal health service utilization in teenage and non-teenage mothers have not been compared often. Aggregated data fail to provide a lucid picture of the differential needs and situation of teenage mothers. Considering the diverse culture, socioeconomic status, and ethnicity of Nepalese society, it becomes more necessary to explore the potential determinants of institutional delivery among teenage and non-teenage mothers and their difference. So, in this study, we aimed to identify the factors associated with institutional delivery among teenage and non-teenage mothers in Nepal.
Material and methods
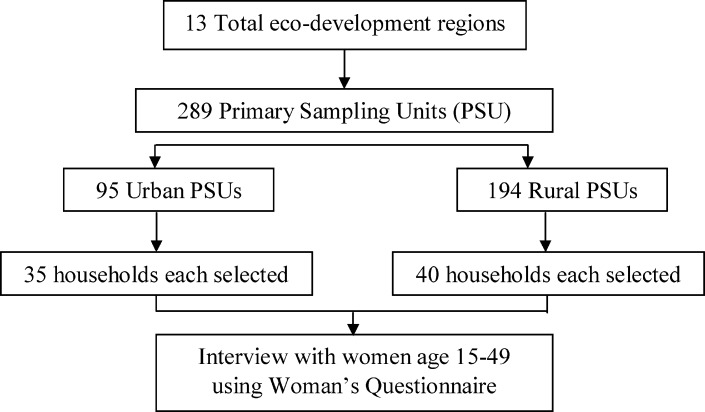
This study used data from Nepal Demographic and Health Survey (NDHS) 2011. NDHS was conducted based on a two-stage cluster sampling technique. The country was at the first divided into 13 sample domains and 25 sample strata. At the second stage, 289 primary sampling units (PSU) were created. Then, households were selected randomly from the PSU according to probability-proportionate-to-size technique. (Fig 1)
Fig 1. Flowchart depicting selection of mothers interviewed.
Details of the survey and sampling procedure have been published in the original report [4]. Total 5391 women of reproductive age (15–49 years), who had become pregnant within five years before the survey, were included in this analysis.
Definitions of variables
Two specific geographical variables were included—Place of residence (‘Urban’, ‘Rural’) and Ecological zone (‘Mountain’, ‘Hill’, ‘Terai’). Here, Terai refers to the plain ecological belt of Nepal that lies in the South. Respondent’s and her husband’s education status was categorized into ‘No education’, ‘Primary education’ and ‘Secondary education or higher’. Participant’s occupation was categorized as ‘Not working’, ‘Agriculture’ and ‘Paid jobs’. Ethnicity was first classified into seven groups according to the classification criteria used by NDHS [14] and then regrouped into four categories: ‘Advantaged ethnicities’ comprising Brahmin and Chhetri, ‘Relatively disadvantaged ethnicities’ including Newar, Janajati, Madheshi and Muslims, ‘Disadvantaged ethnicities’ consisting Dalits, and ‘Other ethnic minorities’ consisting of unspecified and unidentified ethnic groups. This categorization is frequently used in other reports on the further analysis of NDHS data [15–17]. It has to be noted that ethnic group mainly represents the traditional social hierarchy mainly in the caste system and might not necessarily represent the social class. Similarly, the socioeconomic group was derived from wealth quintile; wealth quintile was calculated from household assets using principal component analysis [18] and was divided into five equal categories in rank (poorest, poorer, middle, richer and richest) each comprising 20% of the population. The quintiles were further merged into three categories to form economic status variable- the lowest 40% (poorest and poor) as ‘Poor’; middle 40% (middle and rich) as ‘Middle’; and the upper 20% (richest) as ‘Rich’, as done by previous researchers [16,19,20].
Some women-specific behavioral and fertility-related factors included in this study were–number of Antenatal Care (ANC) visits by the woman (‘None’, ‘1–3 visits’, 4 or more visits’), parity (‘Primi’, ‘Multi’), pregnancy intentness and level of birth preparedness. As recommended by the GoN, birth preparedness consists of the family saving money for emergencies, arranging transportation facilities best for the locality, identifying suitable blood donors, identifying and contacting health workers who can provide maternity services, and having a clean delivery kit handy [21].
Similarly, women autonomy was derived from the information obtained during the interview, mainly regarding the woman’s participation in the household decision making on spending the money earned, purchasing household goods/property, visiting a friend/relative and ability to make decisions regarding her health care. Autonomy was categorized into- ‘No autonomy’: if the woman did not participate at all in the decisions made in the family, ‘Partial autonomy’: if the woman had a say in the decisions, and ‘Full autonomy’: if the woman could decide solely on all the above-mentioned issues.
Statistical analysis
Statistical analysis was performed on STATA 14.0 using survey analysis technique. The association between background characteristics and the utilization of institutional delivery services by the teenage and non-teenage woman was assessed separately by calculating chi-square test for each group. Adjusted odds ratio and its 95% confidence interval (CI) were calculated, while statistically adjusting for background characteristics, separately for both age groups by multiple logistic regression analysis. A stepwise backward elimination method was deployed to select the variables to be included in the multiple logistic regressions. A cut–off of p = 0.05 was chosen and the variables significantly associated (p<0.05) with institutional delivery were selected to be included in the final multiple regression analysis. To address the false discovery rate, we deployed Benjamini-Hochberg procedure [22] to calculate the adjusted p-values.
Ethical clearance
This study was based on the secondary data from NDHS 2011. The NDHS obtained ethical approval from Nepal Health Research Council, Kathmandu, and Macro Institutional Review Board, Maryland, USA [4]. Informed consent was obtained from the respondents (women of reproductive age and their husband) to participate in the survey before the interview was conducted. A special statement was included in the beginning of the household and the individual questionnaire. This statement explained the purpose of the study. Participation in the survey was completely voluntary and the respondent was informed that s/he had the right to refuse to answer any questions or stop the interview at any point. The informed consent statement was read exactly as it was written before the respondent was asked to participate in the interview. Then the interviewer signed his or her name attesting to the fact that s/he read the consent statement to the respondent. However, no written consent was obtained from the respondents. Details on the ethical measures employed during the survey are explained elsewhere [4,23]. Measure DHS program permitted access to the secondary data for this study.
Results
Participant characteristics
Distribution of institutional delivery among the teenage and non-teenage mothers according to their background characteristics is shown in Table 1. (Table 1)
Table 1. Distribution of teenage and non-teenage mothers delivered at the health facility according to their background characteristics-NDHS 2011 (N = 5391).
| Sample | Institutional delivery | |||||||
|---|---|---|---|---|---|---|---|---|
| Characteristics | Total | Non-teenage mothers (n = 5010) | Teenage mothers (n = 381) | Non-teenage mothers (n = 5010) | Teenage mothers (n = 381) | |||
| n | % | n | % | n | % | % | % | |
| Place of residence | P<0.001 | P<0.001 | ||||||
| Urban | 503 | 9.34 | 479 | 9.56 | 24 | 6.42 | 70.86 | 80.6 |
| Rural | 4888 | 90.66 | 4531 | 90.44 | 357 | 93.58 | 30.32 | 48.21 |
| Ecological zone | P<0.001 | P<0.001 | ||||||
| Mountain | 428 | 7.93 | 400 | 7.99 | 27 | 7.18 | 17.48 | 38.72 |
| Hill | 2130 | 39.51 | 2001 | 39.95 | 129 | 33.76 | 31.01 | 35.57 |
| Terai | 2833 | 52.55 | 2608 | 52.06 | 225 | 59.06 | 39.21 | 60.11 |
| Education | P<0.001 | P = 0.032 | ||||||
| No education | 2549 | 47.29 | 2456 | 49.03 | 93 | 24.42 | 18.23 | 48.48 |
| Primary education | 1079 | 20.02 | 964 | 19.25 | 115 | 30.08 | 30.63 | 38.79 |
| Secondary education or higher | 1763 | 32.69 | 1589 | 31.72 | 173 | 45.5 | 61.05 | 58.85 |
| Occupation | P<0.001 | P<0.001 | ||||||
| Not working | 1553 | 28.80 | 1396 | 27.87 | 156 | 41.04 | 50.19 | 63.51 |
| Agriculture | 3692 | 68.49 | 3471 | 69.29 | 221 | 58.01 | 26.28 | 40.12 |
| Paid jobs | 146 | 2.71 | 142 | 2.84 | 4 | 0.95 | 70.25 | 100 |
| Husband’s education | P<0.001 | P = 0.166 | ||||||
| No education | 1244 | 23.07 | 1176 | 23.48 | 67 | 17.66 | 15.34 | 41.83 |
| Primary education | 1311 | 24.31 | 1214 | 24.24 | 96 | 25.29 | 23.31 | 49.18 |
| Secondary education or higher | 2801 | 51.95 | 2589 | 51.67 | 212 | 55.61 | 48.12 | 54.78 |
| Don't know | 36 | 0.67 | 31 | 0.61 | 5 | 1.44 | 12.78 | 0 |
| Ethnicity# | P<0.001 | P = 0.579 | ||||||
| Advantaged ethnicities | 1618 | 30.02 | 1552 | 30.97 | 67 | 17.49 | 43.77 | 51.61 |
| Relatively disadvantaged ethnicities | 2243 | 41.61 | 2080 | 41.52 | 163 | 42.73 | 30.88 | 45.52 |
| Disadvantaged ethnicities | 959 | 17.78 | 860 | 17.16 | 99 | 25.93 | 23.38 | 52.95 |
| Other ethnic minorities | 571 | 10.60 | 519 | 10.35 | 53 | 13.84 | 36.77 | 58.33 |
| Socioeconomic status | P<0.001 | P<0.001 | ||||||
| Poor | 2572 | 47.71 | 2389 | 47.69 | 183 | 47.93 | 15.44 | 36.02 |
| Middle | 2071 | 38.41 | 1900 | 37.92 | 171 | 44.91 | 41.44 | 58.42 |
| Rich | 748 | 13.88 | 721 | 14.39 | 27 | 7.16 | 77.27 | 94.79 |
| Parity | P<0.001 | P = 0.233 | ||||||
| Primi | 1832 | 33.99 | 1499 | 29.92 | 333 | 87.52 | 54.59 | 51.73 |
| Multi | 3559 | 66.01 | 3511 | 70.08 | 48 | 12.48 | 25.49 | 40.17 |
| Pregnancy intentness | P<0.001 | P = 0.044 | ||||||
| Intended | 4065 | 75.41 | 3797 | 75.78 | 269 | 70.54 | 36.16 | 46.09 |
| Unintended | 1326 | 24.59 | 1213 | 24.22 | 112 | 29.46 | 28.06 | 60.33 |
| ANC visit (n = 4149) | P<0.001 | P = 0.010 | ||||||
| No visit | 629 | 11.66 | 602 | 15.77 | 27 | 8.13 | 7.65 | 21.6 |
| 1–3 visits | 1442 | 26.74 | 1316 | 34.51 | 125 | 37.58 | 21.12 | 50.34 |
| 4 or more visits | 2078 | 38.54 | 1898 | 49.72 | 181 | 54.29 | 57.58 | 62.02 |
| Birth preparedness | P<0.001 | P = 0.012 | ||||||
| None | 2609 | 48.40 | 2415 | 63.3 | 194 | 58.29 | 26.82 | 47.16 |
| One | 1382 | 25.64 | 1251 | 32.8 | 131 | 39.38 | 52.09 | 62.28 |
| Two or more | 157 | 2.90 | 148 | 3.9 | 8 | 2.32 | 78.48 | 100 |
| Women autonomy$ | P<0.001 | P = 0.354 | ||||||
| No autonomy | 1424 | 26.76 | 2076 | 42.00 | 97 | 25.58 | 27.81 | 48.66 |
| Partial autonomy | 1984 | 37.27 | 1936 | 39.17 | 141 | 37.12 | 34.63 | 55.79 |
| Full autonomy | 1915 | 35.98 | 931 | 18.84 | 142 | 37.29 | 37.86 | 42.09 |
#Ethnicity is classified into three categories: ‘Advantaged’ category includes Brahmin and Chhetri ethnicities. Similarly, ‘Relatively disadvantaged’ group includes Janajatis, Newar and Muslims and the third category–‘Disadvantaged’ consists Dalits. Other unidentified ethnic groups were kept separately as ‘Other ethnic minorities’.
$Some missing values (n = 5322)
Among the 5391 women delivered within five years before the survey, 7.07% were below 20 years of age. More than 90% were from rural areas and the majority of them (52.55%) were from Terai ecological region. About 47% had no education and more than two-third (68.49%) worked in agriculture. More than half (51.95%) of the women's husband had secondary or higher education. Ethnically, every two in five (41.61%) belonged to the relatively disadvantaged ethnic group. About 48% of the respondents belonged to the poor socioeconomic group. More than three-quarters of the mothers (75.41%) mentioned that their last-born child was intended. (Table 1)
In the unadjusted model, the odds of institutional delivery was significantly higher among the teenage mothers [OR: 1.94; 95% CI: 1.49 2.54] in comparison to their non-teenage counterparts. After adjusting the model for background characteristics, the odds ratio further increased [AOR: 2.25; 95% CI: 1.10 4.59]. (Table 2)
Table 2. Association between age groups and institutional delivery-NDHS 2011 (N = 5391).
| Age group | n | % | OR | [95% CI] | AOR1 | [95% CI] | ||
|---|---|---|---|---|---|---|---|---|
| >20 years (n = 5010) | 1713 | 34.19 | 1.00 | 1.00 | ||||
| <20 years (n = 381) | 189 | 49.71 | 1.94 | [1.49 | 2.54]*** | 2.25 | [1.10 | 4.59]* |
*p<0.05
***p<0.001
OR: odds ratio; AOR: adjusted odds ratio; CI: confidence interval
1 Adjusted for place of residence, woman’s education, woman’s occupation, socioeconomic status, number of ANC visits, birth preparedness and the interaction term for maternal age group and education status
We assessed the interaction among the socio-demographic variables; however, there was no statistically significant interaction, except for maternal age group and education. The AOR in Table 2 is adjusted for the interaction between maternal education status and age group. The multiple logistic model, in overall, was highly significant (p<0.0001). Similarly, an exploratory check of our aggregate model (keeping both teenage and non-teenage mothers together) was done, using primary sampling units as random variables. In the empty model (without any independent variables), the community level variance was 2.19 (SE = 0.29) whereas, in the final aggregate model, the community level variance was 0.53 (SE = 0.16). The proportion change in variance was 75.79 percent, meaning that about 76% of the variation in the odds of institutional delivery between communities was explained by the background characteristics included in the multiple logistic regression model. However, this study aims to assess the effect of individual background characteristics on institutional delivery utilization and therefore, only the fixed effects will be discussed further.
Factors associated with institutional deliveries
Being a rural resident was found to be negatively associated with institutional delivery among both the teenage [AOR: 0.46; 95% CI: 0.24 0.89] and non-teenage [AOR: 0.42; 95% CI: 0.31 0.57] mothers. (Table 3)
Table 3. Factors associated with the institutional delivery among teenage and non-teenage mothers in Nepal- NDHS 2011 (N = 5391).
| Teenage mothers | Non-teenage mothers | |||||
|---|---|---|---|---|---|---|
| Characteristics | AOR | [95%CI] | AOR | [95%CI] | ||
| Place of residence | ||||||
| Urban | 1.00 | 1.00 | ||||
| Rural | 0.46 | [0.24 | 0.89]* | 0.42 | [0.31 | 0.57]*** |
| Mother's education | ||||||
| No education | 1.00 | |||||
| Primary education | 1.22 | [0.93 | 1.61] | |||
| Secondary education or higher | 1.80 | [1.39 | 2.32]*** | |||
| Mother’s occupation | ||||||
| Not working | 1.00 | 1.00 | ||||
| Agriculture | 0.42 | [0.21 | 0.86]* | 0.57 | [0.45 | 0.72]*** |
| Paid jobs | 1.00 | 0.67 | [0.37 | 1.23] | ||
| Socioeconomic status | ||||||
| Poor | 1.00 | 1.00 | ||||
| Middle | 1.73 | [1.00 | 3.02]* | 1.98 | [1.54 | 2.54]*** |
| Rich | 13.70 | [1.89 | 59.09]* | 4.71 | [3.35 | 6.64]*** |
| ANC visit | ||||||
| No visit | 1.00 | 1.00 | ||||
| 1–3 visits | 3.53 | [1.26 | 9.89]* | 1.94 | [1.17 | 3.20]* |
| 4 or more visits | 5.04 | [1.91 | 13.29]** | 5.25 | [3.13 | 8.78]*** |
| Parity | ||||||
| Primi | 1.00 | |||||
| Multi | 0.40 | [0.32 | 0.50]*** | |||
| Birth preparedness | ||||||
| None | 1.00 | |||||
| One | 1.70 | [1.35 | 2.14]*** | |||
| Two or more | 3.72 | [2.16 | 6.41]*** | |||
| Women autonomy | ||||||
| No autonomy | 1.00 | |||||
| Some autonomy | 1.15 | [0.90 | 1.47] | |||
| Full autonomy | 1.30 | [1.02 | 1.65]* | |||
| Intercept | 0.72 | [0.21 | 2.46] | 0.34 | [0.19 | 0.61]*** |
AOR: adjusted odds ratio; CI: confidence interval
*<0.05
**<0.01
***<0.001
Among non-teenage mothers, the odds of institutional delivery was significantly higher [AOR: 1.80; 95% CI: 1.39 1.23] if the mothers had a secondary or higher education.
Mothers working in the agricultural sector compared to non-working mothers had lower odds of institutional delivery in both teenage [AOR: 0.42; 95% CI: 0.21 0.86] and non-teenage [AOR: 0.57; 95% CI: 0.45 0.72] groups. Higher odds of institutional delivery were found among a higher socioeconomic group within both age groups. Among teenage mothers, the odds of institutional delivery was higher at the marginally significant level (p = 0.05) among the middle [AOR: 1.73; 95% CI: 1.00 3.02] and rich [AOR: 13.70; 95% CI: 1.89 59.09] economic groups. A similar pattern was found among non-teenage mothers across the economic groups where the odds for middle and higher socioeconomic status were about two-fold [AOR: 1.98; 95% CI: 1.54 2.54] and five-fold [AOR: 4.71; 95% CI: 3.35 6.64] higher respectively.
The frequency of ANC visits was found positively correlated with the institutional delivery in both age groups. Among the teenage mothers, the odds of institutional delivery was higher among those who visited ANC 1–3 times [AOR: 3.53; 95% CI: 1.26 9.89] or 4 times [AOR: 5.043; 95% CI: 1.91 13.29] in comparison to no ANC visits. Among the non-teenage mothers too, it was almost two-fold [AOR: 1.94; 95% CI: 1.17 3.20] for those who visited ANC 1–3 times and five-fold [AOR: 5.25; 95% CI: 3.13 8.78] for 4 or more ANC visits.
Multiparity was found to be associated with lower odds of institutional delivery among non-teenage mothers [AOR: 0.40; 95% CI: 0.32 0.50], whereas, the association was non-significant among teenage mothers.
Birth preparedness was found to have a positive effect on institutional delivery among the non-teenage mothers. Presence of at least one birth preparedness component was associated with higher odds [AOR: 1.70; 95% CI: 1.35 2.70] of institutional delivery among non-teenage mothers while birth preparedness had no significant effect on institutional delivery among teenage mothers. Similarly, women autonomy had rather small but positive effect on institutional delivery, however, the association was only significant among the non-teenage mothers [AOR: 1.30; 95% CI: 1.02 1.65].
Discussion
This study was carried out to understand the influence of age on the utilization of institutional facilities and to assess factors associated with institutional delivery among teenage and non-teenage mothers separately. This study found that teenage mothers were more likely to deliver in health institution than non-teenage mothers. Other factors consistently associated with institutional delivery among both age groups were the place of residence, occupation, socioeconomic status, and frequency of ANC visits. However, educational status, parity, birth preparedness and women autonomy were found significantly associated with institutional delivery among non-teenage mothers only.
This study found higher odds of institutional delivery among teenage mothers than non-teenage mothers. No association of maternal age with the utilization of the institutional delivery service was observed in an earlier study carried out in Chitwan district of Nepal by Shah et al [24]. Evidence on the relation of maternal age with the site of delivery is inconsistent: while an earlier study from Ethiopia suggested no association [25], Nepal Demographic and Health Survey 2001 and 2006 consistently reported a greater percentage of teenage population delivering in a health facility [26,27]. Pregnancy in teenage women is often riskier than that in non-teenage women because of the underdeveloped pelvic organs [28]. Often, women with high-risk pregnancy are the ones who perceive themselves at risk [29]. This risk perception might have contributed to higher rates of institutional deliveries among teenage women.
Mothers residing in rural areas had lower odds of institutional delivery for both age groups. This might be because of the long distance to reach the health facility, difficult transportation and substandard quality of maternity care services at the poorly staffed rural health centers of Nepal [24,30]. According to a study from Western Nepal, distant health service is linked with added unaccounted costs [7], which can discourage poor pregnant women from seeking delivery in health institutions.While the health institutions in urban locations are relatively well-equipped in terms of health workers and transportation facility, most of the rural settlements of Nepal do not share these facilities [31,32]. To increase access to health service, outreach clinics providing maternal and child health services at a location flexible to most people have been introduced by GoN. These mobile clinics might be an alternative to establishing a permanent health service delivery site in these rural sites. However, no deliberate study has been carried out till date to compare utilization and cost-effectiveness of these outreach clinics. Beside these regular outreach clinics, health camps targeting these hard-to-reach areas are also conducted [33]; but these camps are infrequent and sporadic in nature.
Furthermore, the result of our study showed a positive influence of socioeconomic status on institutional delivery among both teenage and non-teenage mothers. Studies from Nigeria and Pakistan have also reported a positive association between socioeconomic status and institutional delivery [34,35]. Wagle et al. in their study among women from Central Nepal observed that likelihood of home delivery is high for women with low amenity score [36]. Hospital care, including medicines in the Essential Medicine List (list of medicines pre-specified by the GoN), is free in the district public hospitals and peripheral public health facilities. However, people have to make out-of-pocket payments for health services- including maternity care- in the tertiary and other private health facilities. GoN is trying to promote institutional deliveries in Mountainous, Hilly and Terai region by providing NPR 1500, 1000 and 500 respectively for women undergoing institutional delivery. However, this remuneration appears to be inadequate given the formal payment alone for stay at a tertiary maternity hospital averaged NPR 1965 according to a study in Kathmandu [37]. In addition to the ‘formal payment’, this allowance might also be inadequate to compensate for the hidden costs of seeking institutional delivery in rural areas [7].
The findings of our study suggested no significant influence of husband’s educational status on institutional delivery among both teenage and non-teenage mothers, which is contradictory to other research findings [25,35]. But, this might be a true reflection with regard to Nepalese population where the father being well-educated or illiterate might not do much on decision making when a woman gives birth to her child. We can only speculate as no such findings have been established by this study. Pregnant women’s educational status, however, showed significantly positive influence among non-teenage mothers. Similar findings are demonstrated in other studies as well [34,38]. This may be due to the fact that education makes women more aware of the risks of delivery at home and benefits of delivery at a health institution. It means that perceived need for institutional care is created among non-teenage mothers who otherwise were satisfied with delivery at home. Intriguingly, teenage mother’s utilization of delivery facility which was already higher than that of non-teenage mothers was not influenced by their educational status.
In this study, we found an interesting association between women’s occupation and institutional delivery. The pregnant women involved in agricultural occupation were less likely to deliver at health institution than not-working women or women engaged in any other occupation. This finding is, however, inconsistent with the findings from an earlier study in Ethiopia in which it was observed that occupational status of a mother had no association with institutional delivery service utilization [25]. The observed association seems to suggest that women involved in a job as demanding as agriculture might prefer home delivery to institutional delivery because of limited leisure time. Alternatively, it is possible that women involved in the agricultural occupation are not provided equal opportunity to entertain the right to decision making regarding the place of delivery than their counterparts or they may have lower perceived benefits of institutional delivery.
Among the non-teenage population, multiparous mothers were less likely to visit health facility for delivery. A study carried out in Nepal more than a decade ago [39], in addition to other studies [25,34] showed that multiparity was associated with increased likelihood of home delivery. This pattern can be reasoned by the human behavior of risk-perceiving. Perhaps, a woman who gave a normal vaginal delivery during her earlier deliveries may consider that giving birth is a normal phenomenon and institutional delivery is hence considered unnecessary in her subsequent deliveries.
This study also corroborates with the findings of previous studies regarding the association between ANC visit and its effect on institutional delivery [32,40,41]. Women who made ANC visits had a higher chance of having an institutional delivery. On the first hand, a woman who makes the antenatal visits is generally more health-conscious than a woman with no ANC visit. Such a woman, more often, will continue to follow healthy behaviors and hence deliver in an institution. Additionally, during ANC visits, pregnant women are informed about the risks of home delivery and danger signs of delivery and they are counseled for institutional delivery.
The positive correlation between birth preparedness and institutional delivery among the non-teenage mothers suggest that birth preparedness program prepares pregnant women for institutional delivery. As a part of birth preparedness, pregnant women are more likely to have financial preparations and to be counseled on the danger signs and the health risks associated with home delivery. It could be reasoned that all these planned behaviors work out to address the hindrances (educational and economic) of institutional delivery. This finding is consistent with two earlier studies carried out in two separate locations of Nepal [24,41].
Autonomous women were found to have higher odds of institutional delivery; this finding, however, was only significant among non-teenage mothers. Women autonomy as a strong predictor of institutional delivery was reported from other studies too [42,43]. The linkage between autonomy and institutional delivery service utilization can be explained by the woman’s relative position in the household in terms of decision making. Making a decision regarding the place of delivery is a matter of financial and cultural circumstances [44]. Therefore, if anyone else makes a decision on pregnant woman’s behalf regarding the place of delivery, the health of the mothers might not be a top priority. If the woman herself has a final say regarding delivery place or other health care related matters, she is more likely to make a decision which results in better health outcomes [45]. This might be true in case of choosing the health facility as the place of delivery.
This study has some limitations. Instead of the facility based service utilization data, this study represents the information of service utilization based on the participant’s response. Similarly, other potentially influencing factors for the health service utilization including the quality of health services, and the influence of the community were not included because of the unavailability of such information. Similarly, we have used categorical variable for age, education, etc to make the findings easily interpretable and comparable, which however resulted in the loss of information to some extent.
Conclusion
This study identified a significant difference in institutional delivery service utilization among the teenage and non-teenage mothers. While the association of most of the background characteristics with institutional delivery was uniform for both teenage and non-teenage mothers, the association with educational status, parity, birth preparedness and women autonomy was significant only for non-teenage mothers. Considering the difference in the interaction of women’s background characteristics with institutional delivery between teenage and non-teenage mothers might help in identifying the pain points and devise targeted interventions to encourage institutional delivery in teenage mothers or non-teenage mothers or both. Future studies may need to focus on exploring why background characteristics behave differently for teenage and non-teenage in determining the institutional delivery service utilization.
Acknowledgments
The authors are grateful to Measure DHS program for allowing access to the NDHS dataset for this analysis. Authors are also deeply indebted towards the entire women who took part in the NDHS.
Data Availability
The third-party DHS data used in this study are found in the publicly available repositories owned by the DHS program. A request to download the dataset can be submitted to the DHS Program at: https://dhsprogram.com/data/Using-Datasets-for-Analysis.cfm. After the approval, non-transferrable dataset can be freely downloaded from the data repository. The authors did not have any special privileges in obtaining this data set.
Funding Statement
The authors received no funding for this work.
References
- 1.WHO (2015) Trends in Maternal Mortality: 1990 to 2015. Geneva, Switzerland: World Health Organization. [Google Scholar]
- 2.Rajendra K (2012) How did Nepal reduce the maternal mortality? A result from analysing the determinants of maternal mortality. JNMA J Nepal Med Assoc 52. [PubMed] [Google Scholar]
- 3.Ministry of Health [Nepal] NE (1996) Nepal- Family Health Survey 1996. Kathmandu, Nepal: Ministry of Health [Nepal], New ERA. [Google Scholar]
- 4.Ministry of Health and Population (MOHP) [Nepal], New ERA, and ICF International Inc (2012) Nepal Demographic and Health Survey 2011. Kathmandu, Nepal: Ministry of Health and Population, New ERA, and ICF International, Calverton, Maryland. [Google Scholar]
- 5.Baral Y, Lyones K, Skinner J, van Teijlingen E (2012) Maternal health services utilisation in Nepal: Progress in the new millennium. Health Sci J 6: 618–633. [Google Scholar]
- 6.Ronsmans C, Graham WJ (2006) Maternal mortality: who, when, where, and why. Lancet 368: 1189–1200. doi: 10.1016/S0140-6736(06)69380-X [DOI] [PubMed] [Google Scholar]
- 7.Acharya J, Kaehler N, Marahatta SB, Mishra SR, Subedi S, et al. (2016) Hidden Costs of Hospital Based Delivery from Two Tertiary Hospitals in Western Nepal. PLoS ONE 11: e0157746 doi: 10.1371/journal.pone.0157746 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Babafemi AA, Adeleke AJ (2012) Health and social problems of teenage pregnancy and future childbearing in Amassoma Community, Bayelsa State, Nigeria. Res J Med Sci 6: 251–260. [Google Scholar]
- 9.Corcoran J (2016) Teenage Pregnancy and Mental Health. Societies 6: 21. [Google Scholar]
- 10.Senderowitz J (1995) Adolescent health: reassessing the passage to adulthood: World Bank Publications. [Google Scholar]
- 11.Sugathan K, Mishra VK, Retherford RD (2001) Promoting institutional deliveries in rural India: The role of antenatal-care services International Institute for Population Sciences, India, East-West Center, Population and Health Studies, U.S.A. [Google Scholar]
- 12.Raj AD, Rabi B, Amudha P, Glyn C (2010) Factors associated with teenage pregnancy in South Asia: a systematic review. Health Sci J 4. [Google Scholar]
- 13.Pradhan R, Fisher J, Wynter K (2016) Pregnancy among adolescent women in Nepal: a mixed methods investigation of a complex persistent phenomenon Australia: Monash University. [Google Scholar]
- 14.Bennett L, Dahal DR, Govindasamy P (2008) Caste ethnic and regional identity in Nepal: Further analysis of the 2006 Nepal Demographic and Health Survey.
- 15.Khanal V, Adhikari M, Karkee R, Gavidia T (2014) Factors associated with the utilisation of postnatal care services among the mothers of Nepal: analysis of Nepal demographic and health survey 2011. BMC Womens Health 14: 19 doi: 10.1186/1472-6874-14-19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Khanal V, Adhikari M, Sauer K, Zhao Y (2013) Factors associated with the introduction of prelacteal feeds in Nepal: findings from the Nepal Demographic and Health Survey 2011. Int Breastfeed J 8: 9 doi: 10.1186/1746-4358-8-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Acharya P, Khanal V (2015) The effect of mother's educational status on early initiation of breastfeeding: further analysis of three consecutive Nepal Demographic and Health Surveys. BMC Public Health 15: 1069 doi: 10.1186/s12889-015-2405-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vyas S, Kumaranayake L (2006) Constructing socio-economic status indices: how to use principal components analysis. Health Policy Plan 21: 459–468. doi: 10.1093/heapol/czl029 [DOI] [PubMed] [Google Scholar]
- 19.Acharya P, Gautam R, Aro AR (2016) Factors Influencing Mistimed and Unwanted Pregnancies among Nepali Women. J Biosoc Sci 48: 249–266. doi: 10.1017/S0021932015000073 [DOI] [PubMed] [Google Scholar]
- 20.Agho KE, Dibley MJ, Odiase JI, Ogbonmwan SM (2011) Determinants of exclusive breastfeeding in Nigeria. BMC Pregnancy Childbirth 11: 2 doi: 10.1186/1471-2393-11-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.New ERA (2010) Family planning, maternal, newborn and child health situation in rural Nepal: A mid-term survey for NFHP II.
- 22.Benjamini Y, Hochberg Y (1995) Controlling the False Discovery Rate: A Practical and Powerful Approach to Multiple Testing. Roy Stat Soc B 57: 289–300. [Google Scholar]
- 23.The DHS Program (2017) Protecting the Privacy of DHS Survey Respondents.
- 24.Shah R, Rehfuess EA, Maskey MK, Fischer R, Bhandari PB, et al. (2015) Factors affecting institutional delivery in rural Chitwan district of Nepal: a community-based cross-sectional study. BMC Pregnancy Childbirth 15: 27 doi: 10.1186/s12884-015-0454-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Amano A, Gebeyehu A, Birhanu Z (2012) Institutional delivery service utilization in Munisa Woreda, South East Ethiopia: a community based cross-sectional study. BMC Pregnancy Childbirth 12: 105 doi: 10.1186/1471-2393-12-105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ministry of Health [Nepal], New ERA, and ORC Macro (2002) Nepal Demographic and Health Survey 2001. Calverton, Maryland, USA: Family Health Division, Ministry of Health; New ERA; and ORC Macro. [Google Scholar]
- 27.Ministry of Health and Population (MOHP) [Nepal], New ERA, and Macro International Inc (2007) Nepal Demographic and Health Survey 2006. Kathmandu, Nepal: Ministry of Health and Population, New ERA, and Macro International Inc. [Google Scholar]
- 28.Scholl TO, Hediger ML, Belsky DH (1994) Prenatal care and maternal health during adolescent pregnancy: a review and meta-analysis. J Adolesc Health 15: 444–456. [DOI] [PubMed] [Google Scholar]
- 29.Lee S, Ayers S, Holden D (2012) Risk perception of women during high risk pregnancy: a systematic review. Health Risk Soc 14: 511–531. [Google Scholar]
- 30.Karkee R, Binns CW, Lee AH (2013) Determinants of facility delivery after implementation of safer mother programme in Nepal: a prospective cohort study. BMC Pregnancy Childbirth 13: 193 doi: 10.1186/1471-2393-13-193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Shakya G, Kishore S, Bird C, Barak J (2004) Abortion law reform in Nepal: women's right to life and health. Reprod Health Matters 12: 75–84. [DOI] [PubMed] [Google Scholar]
- 32.Shrestha SK, Banu B, Khanom K, Ali L, Thapa N, et al. (2012) Changing trends on the place of delivery: why do Nepali women give birth at home? Reprod Health 9: 25–25. doi: 10.1186/1742-4755-9-25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pandey A, Paudel P, Paudel L (2011) Scenario of health camps in Nepal. J Nepal Health Res Counc 9: 86–88. [PubMed] [Google Scholar]
- 34.Agha S, Carton TW (2011) Determinants of institutional delivery in rural Jhang, Pakistan. Int J Equity Health 10: 31–31. doi: 10.1186/1475-9276-10-31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Onah HE, Ikeako LC, Iloabachie GC (2006) Factors associated with the use of maternity services in Enugu, southeastern Nigeria. Soc Sci Med 63: 1870–1878. doi: 10.1016/j.socscimed.2006.04.019 [DOI] [PubMed] [Google Scholar]
- 36.Wagle RR, Sabroe S, Nielsen BB (2004) Socioeconomic and physical distance to the maternity hospital as predictors for place of delivery: an observation study from Nepal. BMC Pregnancy Childbirth 4: 8 doi: 10.1186/1471-2393-4-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Simkhada P, Van Teijlingen E, Sharma G, Simkhada B, Townend J (2012) User costs and informal payments for care in the largest maternity hospital in Kathmandu, Nepal. Health Sci J 6: 317–334. [Google Scholar]
- 38.Fikre AA, Demissie M (2012) Prevalence of institutional delivery and associated factors in Dodota Woreda (district), Oromia regional state, Ethiopia. Reprod Health 9: 33 doi: 10.1186/1742-4755-9-33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bolam A, Manandhar DS, Shrestha P, Ellis M, Malla K, et al. (1998) Factors affecting home delivery in the Kathmandu Valley, Nepal. Health Policy Plan 13: 152–158. [DOI] [PubMed] [Google Scholar]
- 40.Dahiru T, Oche OM (2015) Determinants of antenatal care, institutional delivery and postnatal care services utilization in Nigeria. Pan Afr Med J 21: 321 doi: 10.11604/pamj.2015.21.321.6527 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Karkee R, Lee AH, Binns CW (2013) Birth preparedness and skilled attendance at birth in Nepal: implications for achieving millennium development goal 5. Midwifery 29: 1206–1210. doi: 10.1016/j.midw.2013.05.002 [DOI] [PubMed] [Google Scholar]
- 42.Bayu H, Fisseha G, Mulat A, Yitayih G, Wolday M (2015) Missed opportunities for institutional delivery and associated factors among urban resident pregnant women in South Tigray Zone, Ethiopia: a community-based follow-up study. Glob Health Action 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ameyaw EK, Tanle A, Kissah-Korsah K, Amo-Adjei J (2016) Women's Health Decision-Making Autonomy and Skilled Birth Attendance in Ghana. Int J Reprod Med 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sudhinaraset M, Beyeler N, Barge S, Diamond-Smith N (2016) Decision-making for delivery location and quality of care among slum-dwellers: a qualitative study in Uttar Pradesh, India. BMC Pregnancy Childbirth 16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Osamor PE, Grady C (2016) Women’s autonomy in health care decision-making in developing countries: a synthesis of the literature. Int J Womens Health 8: 191–202. doi: 10.2147/IJWH.S105483 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The third-party DHS data used in this study are found in the publicly available repositories owned by the DHS program. A request to download the dataset can be submitted to the DHS Program at: https://dhsprogram.com/data/Using-Datasets-for-Analysis.cfm. After the approval, non-transferrable dataset can be freely downloaded from the data repository. The authors did not have any special privileges in obtaining this data set.