Abstract
Nitrogen excreted from body tissues impacts the calculation of multiple breath nitrogen washout (MBWN2) outcomes. The aim of this study was to determine the effect of tissue N2 on MBWN2 outcomes in both healthy subjects and patients with CF and to assess whether it is possible to correct for tissue N2. The contribution of tissue N2 to MBWN2 outcomes was estimated by comparing MBWN2-derived functional residual capacity (FRCN2) to FRC measured by body plethysmography (FRCpleth) and by comparing MBW outcome measures derived from MBWN2 and sulfur hexafluoride MBW (MBWSF6). Compared to plethysmography and MBWSF6, MBWN2 overestimated FRC and lung clearance index (LCI). Application of mathematical tissue N2 corrections reduced FRCN2 values closer to FRCpleth in health and reduced LCIN2 in both health and CF, but did not explain all of the differences observed between N2-dependent and -independent techniques. Use of earlier washout cut-offs could reduce the influence of tissue N2. Applying tissue N2 corrections to LCIN2 measurements did not significantly affect the interpretation of treatment effects reported in a previously published interventional trial. While tissue N2 excretion likely has an impact on MBWN2 outcomes, better understanding of the nature of this phenomenon is required before routine correction can be implemented into current MBWN2 protocols.
Introduction
Multiple breath nitrogen washout (MBWN2) has been shown to be a feasible and sensitive test to measure ventilation inhomogeneity and detect early obstructive lung disease in children and adults [1,2]. Nitrogen (N2) excreted from body tissues through the lungs can impact the calculation of MBWN2 outcomes, including the functional residual capacity (FRC) and lung clearance index (LCI) [3,4]. Several studies have measured the elimination of tissue N2 in healthy adults from its accumulation during breathing of 100% oxygen for prolonged periods [5–11]. Based on these studies, the tissue N2 excretion rate and accumulated volume over time was found to fit a multi-phase exponential curve with the early phases representing the desaturation of highly perfused tissues and the later phases representing the slower desaturation of poorly-circulated and fat-containing tissues. Elimination rates were found to vary both within and between individuals.
Recently, Nielsen et al. applied a tissue N2 excretion equation to a simulated washout in a two compartment lung model with variable dead space and ventilation heterogeneity [3]. Yammine et al. used a different approach to illustrate the effect of tissue N2 on the washout by subtracting 1% end-tidal concentration of N2 evenly over the course of the washout for one healthy subject and one subject with cystic fibrosis (CF) [4]. These two studies confirmed that there is a greater effect of tissue N2 on MBWN2 outcomes in disease versus health, but they did not explore whether the contribution of tissue N2 can be adequately offset in measurements from subjects with a range of body size and lung disease severity. In patients with CF, increased ventilation inhomogeneity leads to greater washout duration, and in theory, longer washouts have a greater total contribution of tissue N2. Therefore, the impact of tissue N2 excretion likely introduces greater bias in a subject with significant lung disease compared to a healthy subject of similar size and leads to the overestimation of their FRC and other MBWN2 outcomes [2–4,12].
There are limited data to support correcting for the contribution of tissue N2; thus it is not currently recommended as per American Thoracic Society/European Respiratory Society (ATS/ERS) consensus statement [12]. As MBWN2 develops into an increasingly important clinical research tool for the monitoring of CF lung disease and the assessment of treatment effects, the role of tissue N2 must be clarified in order to determine whether it is necessary to correct for its contribution to the MBWN2 test. The aim of this study was to estimate the magnitude of tissue N2 in both healthy pediatric and adult subjects and patients with CF across a range of disease severity and to assess the effect of applying correction factors for tissue N2 on the MBWN2 test and on treatment effects in interventional trials.
Materials and methods
Study participants
Data were collected as part of four previously published studies [2,13–15]. Healthy participants without a history of respiratory disease or current acute respiratory tract symptoms were recruited from staff and families at the Hospital for Sick Children. Participants with a confirmed diagnosis of CF (defined by a positive newborn screening test or at least one clinical feature of CF in combination with either a documented sweat chloride >60 mEq/L by quantitative pilocarpine iontophoresis test or a genotype with two CF-causing mutations) were recruited from families attending a routine visit to the CF outpatient clinic at the Hospital for Sick Children or St. Michael’s Hospital in Toronto, Canada. Informed written consent was obtained from the participant or parent/guardian for all subjects. The original studies were approved by the Research Ethics Board at the Hospital for Sick Children (REB #1000019945, #1000024909, and #1000023162) and St. Michael’s Hospital (REB #12–139), Toronto, Canada.
Pulmonary function testing
MBWN2 measurements were performed using an open circuit, bias flow system (Exhalyzer D®, EcoMedics AG, Duernten, Switzerland) and associated software (Spiroware® 3.1 EcoMedics AG). A subgroup of subjects also performed MBW tests using a respiratory mass spectrometer system (AMIS 2000, Innovision A/S, Odense, Denmark), which used sulfur hexafluoride (SF6) as the tracer gas. MBWSF6 traces were analyzed by a single trained observer using custom-written analysis software (TestPoint, Capital Equipment Corp., Billerica, MA, USA). All MBW trials were reviewed for quality control according to guidelines proposed in the ATS/ERS consensus statement [12]. In addition to MBW testing, subjects performed plethysmographic lung volume measurements using the Vmax system (VIASYS CareFusion, San Diego, California, USA) according to ATS standards [16].
Estimates of tissue N2 contribution
FRC measured by body plethysmograph (FRCpleth) includes the volume of all compressible intrathoracic gas, whereas only the volume of communicating lung units is measured during MBW. Therefore, in healthy individuals, FRC measured by a gas-dilution technique (such as MBWN2) should be equal to or less than that measured by plethysmography [17] in the absence of endogenous production of the tracer gas. Thus the differences between FRCpleth and FRCN2 can be used to approximate the contribution of tissue N2 to the MBWN2. Similarly, as SF6 is an exogenous, biologically inert gas that does not dissolve significantly in blood or other tissues, it was used as an indirect reference method to assess the magnitude of the contribution of tissue N2 to FRC derived by gas dilution.
Tissue N2 excretion equations
MBWN2 assesses ventilation inhomogeneity by examining N2 clearance over a series of breaths for the duration of the washout. To generate MBWN2 outcomes, the total volume of exhaled gas (net cumulative expired volume; CEV) and the total volume of inert gas expired per breath (cumulative expired volume of N2; CEVN2) must be measured. FRC and LCI are calculated when CetN2 falls below a predefined threshold (typically 2.5% of the initial CetN2).
| Eq 1 |
| Eq 2 |
where CetN2 is the end tidal concentration of nitrogen. CetN2, initial is the end tidal concentration of N2 in the first breath of the washout phase, and CetN2, final is the end tidal concentration of N2 in the first breath of the washout phase where CetN2 is less than the target threshold. DSpre is the equipment deadspace proximal to the sampling point of the apparatus.
In order to correct these values for tissue N2 excretion, breath-by-breath end tidal body tissue N2 concentration (CetN2 BT) as well as the volume of body tissue nitrogen excreted over the washout (VN2 BT) are subtracted from Eqs 1 and 2 (Eqs 3–5). The volume of tissue nitrogen was generated for the entire breath (from the start of inhalation to the end of exhalation).
| Eq 3 |
| Eq 4 |
| Eq 5 |
where VN2,BTi is the volume of body tissue nitrogen expired in breath i and VExpi is the net volume of expired gas in breath i. CetN2 is the end tidal concentration of nitrogen. CetN2 BT is the end tidal concentration of nitrogen derived from the body tissues. Initial subscript indicates the first breath of the washout phase, and final subscript indicates the first breath of the washout phase where (CetN2- CetN2 BT) is less than the target threshold.
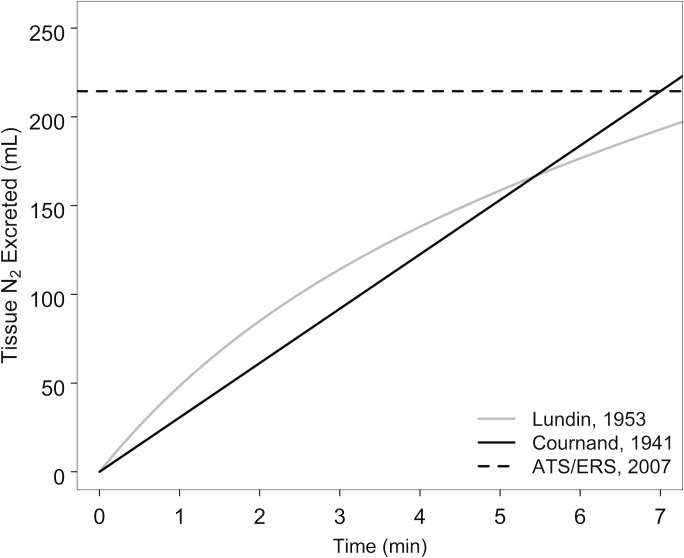
Three different equations (Table 1, Fig 1) were used to derive (VN2 BT). Cournand’s body size-dependent Eq (6) and Lundin’s three-phase exponential excretion rate Eq (14) are time-dependent and calculate the end tidal tissue N2 concentration (CetN2 BT). The ATS/ERS (22) equation is time-independent and is therefore only used to generate VN2 BT and not CetN2 BT. Therefore, corrected FRC values were generated from all three equations (with CetN2, final being uncorrected in the ATS/ERS equation), but corrected LCI values were only generated from the time-dependent equations.
Table 1. Summary of tissue nitrogen correction equations.
| Study (citation) | n | Age range | Equation used |
|---|---|---|---|
| Lundin, 1953 [9] | 7 | 16–42 | Rate of excretion (in mL/min) at time t: Integrating to derive VN2 at time t: Where t = time in minutes |
| Cournand, 1941 [6] | 30 | 9–44 |
Where t = time in seconds |
| ATS/ERS [16] | NA | NA | VN2 = (96.5 × BSA) + 35 |
VN2 = excreted volume of nitrogen (mL)
NA = Not applicable
Fig 1. Tissue N2 excretion equations used for correction of MBWN2 measurements.
The three equations used to estimate the volume of N2 excreted from the body tissues are plotted over a 7 minute time period. The Cournand 1941 equation was adjusted for a constant excretion rate and plotted for a subject with the average body size of the subjects measured in the Lundin 1953 study. The ATS/ERS equation calculates the volume of tissue N2 excreted using Cournand’s 1941 equation standardized to a 7 minute washout for all subjects.
To assess whether the breath-by-breath calculated FRC achieves a plateau, linear regression slopes of the FRCN2/time curves were calculated for the second half all uncorrected and corrected washouts.
Comparisons of the corrected and uncorrected FRC and LCI results were made with FRCpleth and the difference in FRC and LCI measured by MBWN2 and MBWSF6, when available. FRC and LCI values were also re-calculated from the Cournand and Lundin-corrected measurements at the standard MBW end-point of 2.5% normalized end-tidal N2 concentration, as well as for earlier end-points of 5%, 9%, 12%, and 18% normalized end-tidal N2 concentration. These end-points were chosen to reflect previous studies that evaluated earlier cut-offs and existing software algorithms [18].
Accuracy of derived nitrogen concentration
Since N2 concentration values generated by the Exhalyzer D are derived from O2 and CO2 concentrations and not directly measured, our results may be biased if these derived values are inaccurate. To ensure the accuracy of the derived N2 values over the range observed during a MBWN2 test, we compared the CET N2 calculated by the Spiroware software to a set of reference gases generated by blending medical air (compressed on site with presumed gas concentrations: F1CO2 = 0.0004, F1O2 = 0.2095, F1N2 = 0.7808, F1Ar = 0.0093) with a high precision gas mixture (F2CO2 = 0.0500, F2O2 = 0.9500; Praxair Canada, Mississauga ON). FN2 of the mixed reference gas (FMN2) was calculated using Dalton’s Law of partial pressures, the fractional concentrations of the reference gases and the measured FO2 of the mixed gas (FMO2).
FMO2 was measured using the Oxigraf laser oxygen analyzer (Oxigraf Inc, Sunnyvale CA, USA) within the Exhalyzer D®. The accuracy of the Oxigraf analyzer was confirmed against a paramagnetic oxygen analyzer (Servomex 570A, Servomex, Sugar Land TX, USA). The reported FN2 from the Exhalyzer D® was compared to FMN2 over the range of FN2 observed in a washout (0.01–0.8).
Statistical analysis
Study population characteristics and lung function measurements were summarized as mean and standard deviation (SD). Group differences were calculated using two-sample t-tests, whereas differences in outcomes within the same subject were compared using paired t-tests. The agreement between outcomes within the same subject was assessed using Bland-Altman plots. Pearson correlations were used to determine the correlation between two outcomes. All statistical analysis was conducted using R version 3.1.2 (R Foundation for Statistical Computing, Vienna, Austria).
Results
Accuracy of derived nitrogen concentration
The absolute difference between FN2 reported by the Exhalyzer D and the reference concentrations (FMN2) was measured over the full range of washout nitrogen concentrations. The mean absolute difference was 0.064% (95% CI -0.032 to 0.16). All measured differences (n = 14) were less than 0.12%. Therefore, we considered the CetN2 derived by the Exhalyzer D to accurately reflect the true CetN2.
Estimates of tissue N2 contribution to FRC
Characteristics of study participants included are shown in Table 2. Healthy subjects and individuals with CF did not differ in age or lung volumes measured by either MBWN2 or body plethysmography. As expected, LCI measured by MBWN2 was significantly higher in patients with CF.
Table 2. Characteristics of study participants.
Values are presented as mean (SD) unless otherwise indicated. P value indicates group difference between health and CF.
| Health (n = 43) | CF (n = 35) | Mean difference (95% CI) | P-value | |
|---|---|---|---|---|
| Age (years) | 16.5 (5.5) | 16.2 (8.3) | 0.3 (-2.9 to 3.6) | 0.83 |
| Females (%) | 60.5 | 60.0 | 0.5 (-21 to 22) | 0.96 |
| Height (cm) | 163.0 (15.8) | 157.5 (16.8) | 5.5 (-1.9 to 12.9) | 0.14 |
| Weight (kg) | 57.8 (20.6) | 51.7 (17.0) | 6.1 (-2.4 to 14.6) | 0.16 |
| FRCpleth (L) | 2.29 (0.88) | 2.49 (1.06) | -0.2 (-0.72 to 0.33) | 0.47 |
| FRCN2 (L) | 2.59 (0.92) | 2.46 (0.96) | 0.13 (-0.31 to 0.55) | 0.58 |
| LCI | 6.88 (0.49) | 12.04 (3.60) | -5.16 (-6.40 to -3.91) | <0.001 |
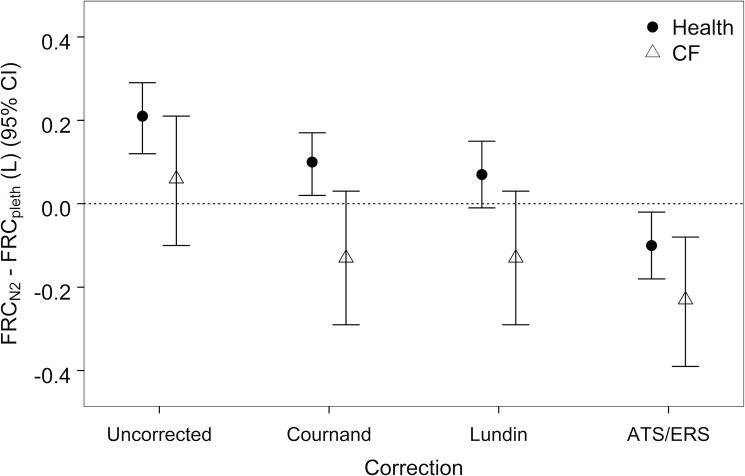
FRC measured by the MBWN2 gas dilution technique (FRCN2) should be smaller than or equal to, but not exceed, FRC measured by body plethysmography (FRCpleth). However, healthy subjects who performed both techniques had FRCN2 values that were on average greater than FRCpleth (mean difference 0.21L; 95% CI 0.12 to 0.29, p<0.001). In contrast, the relationship between FRCN2 and FRCpleth was inconsistent in subjects with CF (mean difference 0.06; 95% CI -0.10 to 0.21, p = 0.44). FRCN2 values were recalculated by applying the three tissue N2 excretion equations. Application of all three tissue N2 excretion equations decreased FRCN2 values compared to FRCpleth in health and CF (Fig 2).
Fig 2. Within-subject difference in FRC measured by multiple breath nitrogen washout (FRCN2) and body plethysmography (FRCpleth).
The mean within-subject difference FRCN2—FRCpleth decreased after the three tissue N2 excretion equations were applied to washout data from healthy and CF populations.
Given that the Cournand and Lundin excretion equations improve the FRCN2 agreement with plethysmography, the uncorrected FRCN2 (FRCuncorr) and the FRCN2 corrected (FRCCournand and FRCLundin) were then compared within subjects (Table 3).
Table 3. Estimates of tissue N2 contribution to MBW outcomes at the 2.5% washout cut-off.
Values are presented as the mean within-subject difference (95% CI) of the uncorrected–corrected MBWN2 outcome. Outcomes were corrected by applying either the Cournand or Lundin tissue N2 excretion equations.
| Outcome | Health Mean difference (95% CI) |
CF Mean difference (95% CI) |
|---|---|---|
| FRCN2 (L) | ||
| Cournand | 0.11 (0.10; 0.13), p<0.001 | 0.18 (0.15; 0.21), p<0.001 |
| Lundin | 0.13 (0.12; 0.15), p<0.001 | 0.19 (0.17; 0.20), p<0.001 |
| CEVN2 (L) | ||
| Cournand | 1.63 (1.36; 1.90), p<0.001 | 4.41 (3.30; 5.52), p<0.001 |
| Lundin | 1.57 (1.37; 1.76), p<0.001 | 3.22 (2.40; 4.03), p<0.001 |
| LCIN2 | ||
| Cournand | 0.35 (0.29; 0.42), p<0.001 | 0.90 (0.63; 1.17), p<0.001 |
| Lundin | 0.30 (0.23; 0.36), p<0.001 | 0.41 (0.17; 0.65), p = 0.001 |
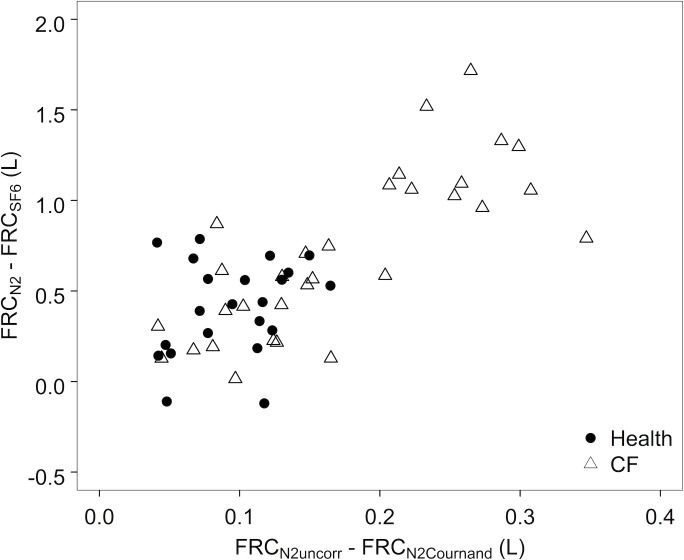
The within-subject difference in FRC as measured by MBWN2 and MBWSF6 (FRCN2 –FRCSF6) were also compared with the estimated contribution of tissue N2 to FRCN2. The difference between FRCN2 and FRCSF6 was positively correlated with increased washout time (r = 0.69, p<0.001). FRCN2 became disproportionately larger than FRCSF6 as the contribution of tissue N2 as estimated by FRCuncorr−FRCCournand increased (r = 0.68, p<0.001) (Fig 3).
Fig 3. Relationship between the contribution of tissue N2 to FRCN2 and the difference between FRC as measured by MBWN2 and MBWSF6.
FRCN2 became disproportionately greater than FRCSF6 as the contribution of tissue N2 estimated by the within-subject difference FRCN2—FRCCournand increased.
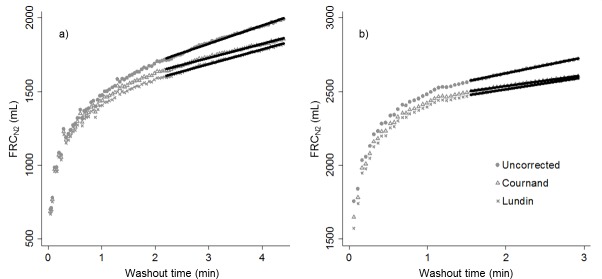
When plotted against washout time, the breath-by-breath calculation of FRCN2 did not plateau as would be expected in a closed system, but rather continued to increase throughout the washout (representative examples from health and CF shown in Fig 4). This is consistent with continuous tissue N2 excretion. Breath-by-breath correction of the FRCN2 values using the Cournand and Lundin equations decreased the rate of rise of the FRCN2 by 23–34%, but did not reduce it to zero (Fig 4, Table 4). The absolute and relative magnitudes of the decrease in the FRC/time slope were greater in healthy subjects than in those with CF for both the Lundin and Cournand equations (Table 4).
Fig 4.
Representative examples of FRCN2 plotted against washout time in a) a healthy subject and b) a patient with CF. Application of the Cournand and Lundin tissue N2 excretion equations resulted in a less pronounced increase in the calculation of FRCN2 over the course of the washout, but a plateau was never achieved. Linear regressions of these curves over the second half of the washout are shown, demonstrating the slopes that are reported in Table 4.
Table 4. Average slopes of the second half of all uncorrected, Lundin-corrected and Cournand-corrected FRCN2/breath number curves (depicted graphically in Fig 4) for healthy subjects and those with CF.
Average paired difference (uncorrected-corrected) in absolute and relative (percent of uncorrected slope) terms are shown. Data are expressed as mean 95% confidence interval) unless otherwise stated.
| Health | CF | |
|---|---|---|
| Uncorrected slope (mL/min) | 104.2 (97.9, 110.6) | 125.3 (115.4, 135.2) |
| Corrected slope (Lundin) | 77.4 (71.4, 83.5) | 100.4 (90.1, 110.7) |
| Absolute diff (Lundin) | 26.8 (25.2, 28.4) | 24.9 (23.4, 26.4) |
| Relative diff (Lundin) (%) | 27.4 (25.0, 29.9) | 22.5 (19.6, 25.3) |
| Corrected slope (Cournand) | 70.5 (65.0, 76.0) | 94.2 (84.9, 103.5) |
| Absolute diff (Cournand) | 33.7 (32.3, 35.1) | 31.1 (29.6, 32.6) |
| Relative diff (Cournand) (%) | 33.9 (31.9, 35.8) | 26.7 (24.6, 28.8) |
Estimates of tissue N2 contribution to CEV and LCI
Similar to FRCN2, application of tissue N2 excretion equations to MBWN2 data resulted in lower CEVN2 and LCIN2 values (Table 2). Application of the Cournand excretion equation shortened the washout by an average of 2.9 breaths in health (95% CI 2.5 to 3.3, p<0.001) and 7.6 breaths in CF (95% CI 6.3 to 8.8, p<0.001). Similar results were observed for the Lundin equation (2.9 and 5.9 breaths in health and CF, respectively). Since the ATS/ERS correction is not time-dependent and only corrects FRCN2 for the contribution of tissue N2, it was not used to correct LCI and CEV values.
When LCI as measured by MBWN2 and MBWSF6 were compared within subjects (LCIN2 –LCISF6), LCIN2 became disproportionately greater than LCISF6 as disease severity (LCIN2) increased (r = 0.53, p<0.001). Similar to FRCN2, there was a significant and positive correlation observed between LCIN2 –LCISF6 and the effect of tissue N2 as estimated by LCIuncorr−LCICournand (r = 0.55, p<0.001).
Impact of tissue N2 at earlier washout cut-offs
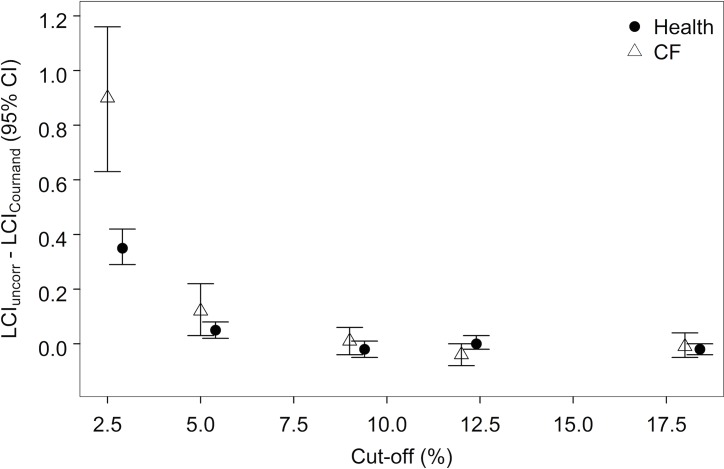
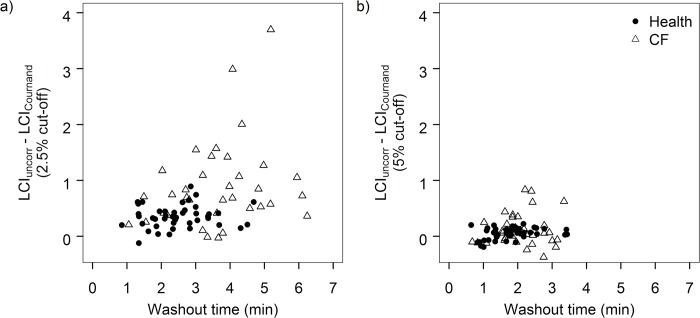
With application of the Cournand tissue N2 excretion equation, the effect of tissue N2 (LCIuncorr−LCICournand) decreased when LCIN2 was calculated at earlier cut-offs of the washout (Fig 5). Compared to the traditional cut-off of 2.5% normalized end-tidal concentration of N2, the difference between corrected and uncorrected LCI (LCIuncorr−LCICournand) was less pronounced at the 5% cut-off and was no longer significant by the 9% cut-off. While the effect of tissue N2 (LCIuncorr−LCICournand) on LCIN2 calculated at the 2.5% cut-off increased as disease severity (LCIN2) increased (r = 0.61, p<0.001) (Fig 6A), this relationship was not observed at the 5% cut-off (r = 0.17, p = 0.13) (Fig 6B).
Fig 5. Within-subject difference between uncorrected LCIN2 and LCIN2 corrected for tissue N2 excretion (LCICournand) at different washout cut-offs.
The difference was progressively smaller when calculated at earlier cut-offs of the washout in both health and CF.
Fig 6.
Relationship between the contribution of tissue N2 to LCIN2 and length of washout calculated at a) the traditional 2.5% washout cut-off and b) the 5% washout cut-off. The contribution of tissue N2 to LCIN2 calculated at the 2.5% cut-off (LCIuncorr−LCICournand) increased as washout time increased. However, this relationship was no longer observed at the earlier 5% cut-off.
Impact of tissue N2 correction on interventional trial outcomes
Both the Cournand and Lundin equations were applied to MBW data of an observational study investigating the effect of ivacaftor on LCI in children with class 3 mutations in CF [14] (Table 5). The Lundin-corrected treatment effect was significantly smaller than the uncorrected value (p = 0.01) and the Cournand-corrected difference showed a similar trend (p = 0.11). This change in treatment effect was driven by a greater negative correction in pre-treatment LCI than post-treatment LCI by both Lundin (pre-treatment correction -0.9 [-1.3, -0.5] units; post-treatment correction -0.6 [-0.8, -0.3] units) and Cournand (pre-treatment correction -1.3 [-1.8, -0.8] units; post-treatment correction -0.9 [-1.3, -0.4] units) equations. Neither correction equations changed the direction or significance of the treatment effect.
Table 5. Effect of applying Lundin and Cournand correction equations to previously published observational MBW data.
Data are shown as pre-treatment and post-treatment LCI with paired treatment effect. Values are presented as mean (SD) unless otherwise indicated.
| Pre-treatment LCI | Post-treatment LCI | Treatment effect mean difference (95%CI) | |
|---|---|---|---|
| Ivacaftor [14] | |||
| Uncorrected | 13.7 (3.7) | 11.6 (4.1) | -2.2 (-3.0, -1.3) |
| Lundin | 12.8 (3.8) | 11.0 (3.9) | -1.8 (-2.6, -0.9) |
| Cournand | 12.4 (3.6) | 10.7 (3.6) | -1.8 (-2.8, -0.7) |
Discussion
In agreement with previous studies, these data suggest that excretion of N2 from body tissues affects MBWN2 outcomes. The effects of tissue N2 are greater in patients with longer washouts. This contribution of tissue N2 to FRCN2 and LCIN2 is less pronounced at earlier cut-offs of the washout. Application of correction equations for tissue N2 significantly reduced, but did not completely eliminate, the effect of tissue N2 on MBWN2 outcomes. Importantly, application of these tissue N2 correction equations did not significantly alter treatment effects previously observed in interventional trials. Thus, while the excretion of tissue N2 has a measurable effect on MBWN2 outcomes, correction for tissue N2 using currently available approaches cannot be recommended at the present time.
FRC is an integral component of the calculation of LCI by MBW and therefore a reliable FRC is required to derive a reliable LCI. While there is no gold standard for the determination of FRC, body plethysmography and inert gas washout are the most commonly used techniques [16,17]. In the current study, FRCN2 was compared to FRCpleth and FRCSF6 to estimate the contribution of tissue N2 excretion. With FRCpleth, the volume of all compressible intrathoracic gas is measured whereas only the volume of communicating lung units is measured with FRCN2. Therefore, FRC measured by gas-dilution technique (such as MBWN2) should be equal to or less than that measured by plethysmography in the absence of endogenous production of the tracer gas [17]. FRCSF6 is also calculated using a gas-dilution technique, and because it is an exogenous, biologically inert gas that does not dissolve significantly in blood or other tissues, it was used as comparator to assess for the contribution of tissue N2 excretion to FRCN2.
We found that FRCN2 was systematically overestimated compared to FRCSF6 and, to a more variable extent, FRCpleth (Figs 2 and 5). This suggests that there is a systematic difference between these tests and that the observed differences were not entirely due to intrinsic differences between the MBW and plethysmographic techniques. While our analyses focused on the potential effect of tissue nitrogen excretion on this overestimation, there are other explanations for this disparity that could contribute to the observed differences that were not assessed in the current study, such as testing order, technical inconsistencies in the MBW equipment, and physical differences between SF6 and N2 tracer gases.
The order of tests could have inadvertently biased the results through effects of tissue hysteresis or other unknown mechanisms. In the original study, all plethysmographic testing was performed after the MBW testing and the order of MBWSF6 and MBWN2 was randomized [2]. All MBW-based outcomes can be affected by errors in gas concentration measurement, flow-gas signal alignment, dead-space correction and other device-specific settings [19–21]. In this study, we used working-group recommended equipment and software settings on both the Exhalyzer D and AMIS 2000 devices and applied standardized quality control criteria to each MBW trial. We also confirmed the accuracy of the N2 concentration calculation (as FN2 is derived from measured O2 and CO2 concentrations using the Exhalyzer device) across a range of gas standards. Despite our attempts to minimize technical software or device-specific inconsistencies, these cannot be completely ruled out as sources of systematic error that could contribute to the discrepancies observed.
The intrinsic properties of MBWSF6 and MBWN2 tests could also have contributed to these differences. The molecular properties of SF6 and N2 likely result in differences in their diffusion-convection fronts, which could potentially impact MBW outcomes [22]. MBWSF6 requires a wash-in equilibration phase as SF6 is an exogenous tracer gas, and while standardized quality control techniques were implemented to attempt to ensure complete SF6 washing, it is possible that incomplete wash-in of the SF6 could result in altered excretion kinetics. Finally, the 100% oxygen washout phase in MBWN2 could also theoretically have pro-atelectatic effects, thus altering pulmonary gas flow dynamics. While simultaneous direct measurements of N2 and SF6 on the same device would permit an ideal comparison of these two MBW systems, unfortunately, high O2 concentration impairs the ability of the AMIS 2000 respiratory mass spectrometer to measure N2 concentrations and can therefore not be used to measure the two gases in the context of a 100% oxygen washout. Overall, our results need to be interpreted in the context of these potential limitations; nevertheless, the consistent overestimation of FRCN2 when compared to FRCpleth and FRCSF6 suggests that tissue N2 likely contributes to this phenomenon.
Both FRCN2 and LCIN2 decreased significantly upon application of the tissue N2 excretion equations in both healthy subjects and subjects with CF, with greater differences observed in CF. The estimates of the contribution of tissue N2 to FRCN2 and LCIN2 are similar to those previously predicted by a two-compartment lung model including variable ventilation heterogeneity and dead space effects [3]. However, the difference between FRCSF6 and FRCN2 was significantly greater than the degree of correction applied by either Lundin or Cournand equations (Fig 3). Also, application of the correction equations only decreased the time-dependent-rise in FRCN2 by ~30% (Fig 4; Table 4). These findings suggest either that the equations used in this study underestimate the amount of tissue N2 excretion, or that there are other factors in addition to tissue N2 secretion that are driving this difference.
The Lundin tissue N2 excretion equation is based on the average of measurements derived from healthy adults, therefore its application to MBWN2 data derived from subjects of varying size is limited. Compared to the Cournand equation, which was derived from subjects ranging from 9 to 44 years old and adjusts for a subject’s body size, the Lundin equation may overestimate the effect of tissue N2 excretion in smaller pediatric subjects. Although the Cournand equation may introduce less error overall in MBWN2 measurements from subjects with a range of body size, it assumes a constant rate of N2 excretion from the body tissue which is unlikely to be the case in subjects of varying body composition and between health and disease. In a recently published study [23], the rate of tissue N2 excretion was simultaneously performed on MBWN2 and MBWSF6 washouts and confirmed the time-dependent nature of tissue N2 excretion and demonstrated higher rates of tissue N2 excretion during moderate exercise.”
Ideally, direct measurement of pulmonary N2 excretion of tissue N2 with modern equipment across a range of ages, body compositions and disease states would allow us to generate an optimal correction equation. However, due to the long duration of the testing and uncomfortable testing setup, replications of these early studies would be extremely challenging to conduct today, especially in children [6,9]. Furthermore, no mathematical correction for tissue N2 excretions will be ideal for several reasons. First, even with modern technology, it is impossible to precisely isolate all of the N2 in the lungs that was excreted from the body tissue, especially during the beginning of the washout when the relative proportion is very small; the derived equations are reflections of this imprecision. Second, the contribution of N2 from the body tissue is likely dependent not only on time and body size, but also on factors such as cardiac output, tissue perfusion, body fat content, ventilation homogeneity, and dead space [3,6,8,23–26]. Any number of these physiological factors could be altered in a disease like CF and could confound the estimation of tissue N2 excretion.
The extent to which the MBWN2 outcomes diverged from both MBWSF6 and MBWpleth was related to the length of the washout. This correlation makes intuitive sense, since individuals with longer washouts (greater ventilation inhomogeneity) spend a longer time at lower end-tidal N2 concentrations, thereby accentuating the relative contribution of excreted tissue nitrogen. Given this finding, we showed that the contribution of tissue N2 can be minimized by calculating MBWN2 outcomes at earlier cut-offs of the washout, such as at the 5% normalized end tidal concentration of N2. Using an earlier cut-off of the washout has the additional benefit of shortening the total time it takes to perform an MBW test; however, there is some evidence that there may be a trade-off with decreased sensitivity to treatment efficacy [18]. Nevertheless, the use earlier cut-off for MBWN2 did not affect the significance of treatment effects observed in a study of Ivacaftor treatment [14], suggesting that the sensitivity of an MBW cut-off may depend upon the effect size of the intervention. The optimal MBWN2 cutoff for interventional studies may depend on study design and treatment.
Finally, to address the practical question of whether or not the correction for tissue N2 excretion could affect the results of previously reported interventional studies, we applied tissue N2 correction equations to raw MBWN2 data from a study that assessed the effect of ivacaftor on LCI [14]. Overall, this study had a large treatment effect (-2.2 LCI units) and we found that applying tissue N2 correction equations attenuated the treatment response, but did not change the significance or direction of the treatment effect. This attenuation of the treatment response occurred primarily by reducing the post-treatment LCI by a greater amount than the pre-treatment LCI and is likely a reflection of the observation that tissue N2 has a greater contribution in longer washouts. Taken together, these results suggest that non-correction for tissue N2 release may result in marginally overestimated treatment effects. While this does not significantly affect the results of the studied trial, it is conceivable that smaller treatment effects could be amplified by non-correction for tissue N2.
In conclusion, MBWN2 outcomes are systematically different from MBWSF6 and plethysmography. We show that correction for tissue N2 excretion using previously derived equations can reduce, but not eliminate, these differences. This suggests that either there are other physiologic/experimental factors contributing to this difference, or that the correction equations that were used underestimate the quantity of tissue N2 excretion. Given our data, we suggest that there is currently inadequate knowledge of the true rate of pulmonary tissue nitrogen excretion to suggest a standard correction equation for this phenomenon in the calculation of MBW outcomes. Further study (ideally simultaneous MBWN2 and MBWSF6 measurements using an appropriately tuned mass spectrometer) could elucidate the contribution of tissue N2 to MBWN2 outcome measures. Until this is clarified, it should be recognized that the magnitude of treatment responses measured with MBWN2 may be over-estimated by tissue N2 excretion, however, application of correction equations in this study did not change the direction or significance of the treatment effects of a previously studied intervention.
Acknowledgments
We would like to thank the families, children and adults who volunteered to participate in our study and the CF Clinical Research Team at the Hospital for Sick Children.
Data Availability
Our data are ethically restricted by the Research Ethics Board at the Hospital for Sick Children. They can be reached at reb.admin@sickkids.ca. However, REB does not store the data; data are housed on a secure server by the corresponding author, per REB guidelines. Correspondence with the author will also be required to access the primary data.
Funding Statement
FR is funded by the Sellers Chair of Cystic Fibrosis at The Hospital For Sick Children and the Irwin Family Fund. Neither source has a specific grant number. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Garcia G, Perez T, Verbanck S (2012) [Functional measurements of the peripheral airways in COPD]. Rev Mal Respir 29: 319–327. doi: 10.1016/j.rmr.2011.09.042 [DOI] [PubMed] [Google Scholar]
- 2.Jensen R, Stanojevic S, Gibney K, Salazar JG, Gustafsson P, et al. (2013) Multiple breath nitrogen washout: a feasible alternative to mass spectrometry. PLoS One 8: e56868 doi: 10.1371/journal.pone.0056868 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nielsen N, Nielsen JG, Horsley AR (2013) Evaluation of the impact of alveolar nitrogen excretion on indices derived from multiple breath nitrogen washout. PLoS One 8: e73335 doi: 10.1371/journal.pone.0073335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yammine S, Lenherr N, Nyilas S, Singer F, Latzin P (2015) Using the same cut-off for sulfur hexafluoride and nitrogen multiple-breath washout may not be appropriate. J Appl Physiol (1985) 119: 1510–1512. [DOI] [PubMed] [Google Scholar]
- 5.Behnke AR TR, Shaw LA (1935) The rate of elimination of dissolved nitrogen in man in relation to the fat and water content of the body. Am J Physiol 114: 137–146. [Google Scholar]
- 6.Cournand A YI, Riley RL (1941) Influence of body size on gaseous nitrogen elimination during high oxygen breathing. Proc Soc Exp Biol Med 48: 280–284. [Google Scholar]
- 7.Curry TB, Lundgren CE (2003) Negative pressure breathing enhances nitrogen elimination. Aviat Space Environ Med 74: 1034–1039. [PubMed] [Google Scholar]
- 8.Darling RC CA, Mansfield JS, Richards DW (1940) Studies on the intrapulmonary mixture of gases. I. Nitrogen elimination from blood and body tissues during high oxygen breathing. J Clin Invest 19: 591–597. doi: 10.1172/JCI101161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.G L (1953) Nitrogen elimination during oxygen breathing. Acta Physiol Scand 30: 130–143. [PubMed] [Google Scholar]
- 10.Pendergast DR, Senf C, Lundgren CE (2012) Is the rate of whole-body nitrogen elimination influenced by exercise? Undersea Hyperb Med 39: 595–604. [PubMed] [Google Scholar]
- 11.Robertson JS, Siri WE, Jones HB (1950) Lung ventilation patterns determined by analysis of nitrogen elimination rates; use of mass spectrometer as a continuous gas analyzer. J Clin Invest 29: 577–590. doi: 10.1172/JCI102295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Robinson PD, Latzin P, Verbanck S, Hall GL, Horsley A, et al. (2013) Consensus statement for inert gas washout measurement using multiple- and single- breath tests. Eur Respir J 41: 507–522. doi: 10.1183/09031936.00069712 [DOI] [PubMed] [Google Scholar]
- 13.Amin R, Stanojevic S, Kane M, Webster H, Ratjen F (2016) A randomized controlled trial to evaluate the lung clearance index as an outcome measure for early phase studies in patients with cystic fibrosis. Respir Med 112: 59–64. doi: 10.1016/j.rmed.2016.01.020 [DOI] [PubMed] [Google Scholar]
- 14.Kane M, Gonska T, Jensen R, Avolio J, Klingel M, et al. (2016) Lung clearance index response in patients with CF with class III CFTR mutations. Thorax 71: 476–477. doi: 10.1136/thoraxjnl-2015-207894 [DOI] [PubMed] [Google Scholar]
- 15.Sonneveld N, Stanojevic S, Amin R, Aurora P, Davies J, et al. (2015) Lung clearance index in cystic fibrosis subjects treated for pulmonary exacerbations. Eur Respir J 46: 1055–1064. doi: 10.1183/09031936.00211914 [DOI] [PubMed] [Google Scholar]
- 16.Wanger J, Clausen JL, Coates A, Pedersen OF, Brusasco V, et al. (2005) Standardisation of the measurement of lung volumes. Eur Respir J 26: 511–522. doi: 10.1183/09031936.05.00035005 [DOI] [PubMed] [Google Scholar]
- 17.Coates AL, Peslin R, Rodenstein D, Stocks J (1997) Measurement of lung volumes by plethysmography. Eur Respir J 10: 1415–1427. [DOI] [PubMed] [Google Scholar]
- 18.Stanojevic S, Jensen R, Sundaralingam D, Salazar JG, Yammine S, et al. (2015) Alternative outcomes for the multiple breath washout in children with CF. J Cyst Fibros 14: 490–496. doi: 10.1016/j.jcf.2014.12.008 [DOI] [PubMed] [Google Scholar]
- 19.Benseler A, Stanojevic S, Jensen R, Gustafsson P, Ratjen F (2015) Effect of equipment dead space on multiple breath washout measures. Respirology 20: 459–466. doi: 10.1111/resp.12470 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Summermatter S, Singer F, Latzin P, Yammine S (2015) Impact of Software Settings on Multiple-Breath Washout Outcomes. PLoS One 10: e0132250 doi: 10.1371/journal.pone.0132250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Poncin W, Singer F, Aubriot AS, Lebecque P (2017) Agreement between multiple-breath nitrogen washout systems in children and adults. J Cyst Fibros 16: 258–266. doi: 10.1016/j.jcf.2016.11.004 [DOI] [PubMed] [Google Scholar]
- 22.Verbanck S (2012) Physiological measurement of the small airways. Respiration 84: 177–188. doi: 10.1159/000341742 [DOI] [PubMed] [Google Scholar]
- 23.Sullivan L, Forno E, Pedersen K, Nielsen JG, Weiner DJ (2017) Nitrogen back-diffusion during multiple-breath washout with 100% oxygen. Eur Respir J 50. [DOI] [PubMed] [Google Scholar]
- 24.Bodkin JJ, Curry TB, Lundgren CE (2006) Negative pressure oxygen breathing and head-down tilt increase nitrogen elimination. Undersea Hyperb Med 33: 455–462. [PubMed] [Google Scholar]
- 25.Hugon J, Rostain JC, Gardette B (2010) A closed-circuit rebreather for the characterization of denitrogenation. Aviat Space Environ Med 81: 1018–1023. [DOI] [PubMed] [Google Scholar]
- 26.Nelson NM, Prodhom LS, Cherry RB (1964) Nitrogen Excretion by Newborn Infants during Oxygen Breathing. J Pediatr 65: 299–300. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Our data are ethically restricted by the Research Ethics Board at the Hospital for Sick Children. They can be reached at reb.admin@sickkids.ca. However, REB does not store the data; data are housed on a secure server by the corresponding author, per REB guidelines. Correspondence with the author will also be required to access the primary data.