Abstract
Objectives
Aging is often characterized by declines in physical and mental health and increased risk for depression and social isolation. A protective factor that has been found to effectively moderate these phenomena is psychological well-being. The aim of his study was to pilot test a novel group intervention (Lighten UP! program) for the promotion of psychological well-being in older adults living in the community.
Methods
Lighten UP! is an 8-week program consisting of 90 min group session designed to teach participants to identify and savor positive experiences across multiple domains of eudaimonic well-being. It was delivered to a sample of 103 men and women aged 60 or over, that were assessed pre and post intervention with Ryff’s Psychological Well-being Scale (PWB), Life Satisfaction scale, Geriatric Depression Scale, Symptom Questionnaire, and items measuring sleep complaints and social well-being.
Results
At the end of the 8 weeks, participants reported significantly increased PWB, life satisfaction, and social well-being along with lower levels of depression and fewer physical symptoms and sleep complaints. These gains were particularly robust for individuals with lower pre-program levels of PWB.
Conclusions
This pilot investigation suggests the feasibility of a short group program for enhancing well-being in older adults. Future controlled investigations with long-term follow-up assessment are needed to confirm the effectiveness and sustained benefits of the Lighten UP! program.
Keywords: psychological well-being, positive aging, group intervention, depression, positive psychotherapy
Introduction
Aging is characterized by declines in physical health and functional capacities and by the loss of significant roles and relationships, experiences that challenge quality of life. A protective factor that moderates the impact of these phenomena is psychological well-being. Both hedonic (positive affect and life satisfaction) and eudaimonic (purpose in life, positive social relations) aspects of well-being have been linked to better physical health and reduced biological risk of disease (Friedman & Ryff, 2012; Pressman & Cohen, 2005; Ryff, 2014; Steptoe, Dockray, & Wardle, 2009). Prospective studies with older samples have linked purpose in life to reduced subsequent risk of Alzheimer’s disease and cognitive impairment (Boyle, Buchman, Barnes, & Bennett, 2010), stroke (Kim, Sun, Park, & Peterson, 2013), myocardial infarction (Kim, Sun, Park, Kubzansky, & Peterson, 2013), and mortality (Boyle, Barnes, Buchman, & Bennett, 2009; Hill & Turiano, 2014). Greater purpose in life also predicts increased use of preventive health care practices and reduced likelihood of hospitalization (Kim, Strecher, & Ryff, 2014).
Given these health benefits, a central question is whether psychological well-being can be promoted in older adults by targeted intervention. Programs focused on gratitude, forgiveness, and positive affect have increased these aspects of positive functioning in older adults and reduced depressive and anxiety symptoms (Proyer, Gander, Wellenzohn, & Ruch, 2014; Ramirez, Ortega, Chamorro, & Colmenero, 2014; Webster, Bohlmeijer, & Westerhof, 2014). However, to date no program guided by eudaimonic principles and designed to improve quality of life in older adults has been developed. Although related, hedonic and eudaimonic well-being are conceptually and empirically distinct (Keyes, Shmotkin, & Ryff, 2002; Ryan & Deci, 2001), and they have different trajectories of change with age. Specifically, hedonic well-being, including positive affect and life satisfaction, tends to remain stable or increase with age. A recent longitudinal investigation documented a positive correlation between subjective (hedonic) well-being and age in a European older age cohort (Gaymu & Springer, 2010). Similarly, a 23-year study of 2,800 adults observed declines in negative affect with age, but stable levels of positive affect (Charles, Reynolds, & Gatz, 2001). Further, in a sample of American older adults, life satisfaction displayed a u-shaped trend, with linear increases starting from around age 50 (Stone, Schwartz, Broderick, & Deaton, 2010). Gana et al. (2013) documented an increasing trend of life satisfaction over an 8 year period, even when controlling for initial age, gender, education, and perceived health.
Conversely, both cross sectional and longitudinal studies confirm that purpose in life, personal growth, and other existential dimensions of well-being tend to decline from middle adulthood to older age (Ryff, 2014; Springer, Pudrovska, & Hauser, 2011). Further, these declines represent important vulnerability factors for mental and physical health of older individuals (Friedman, 2012; Ryff, 2014; Wood & Joseph, 2010). The maintenance and/or promotion of eudaimonic well-being in aging individuals may thus be uniquely beneficial for older adults.
Therapeutic approaches based on eudaimonic well-being have been used successfully in clinical and educational settings. Patients with major depression who received well-being therapy (WBT), for example, were less likely to relapse up to six years after treatment compared to patients who received clinical management alone (Fava, Rafanelli, Grandi, Conti, & Belluardo, 1998; Fava et al., 2004). WBT has also been applied successfully to patients with generalized anxiety disorder (Fava et al., 2005). A school-based protocol designed to teach children and adolescents about the importance of well-being demonstrated increases in eudaimonic well-being in a non-clinical sample (Ruini, Belaise, Brombin, Caffo, & Fava, 2006; Ruini et al., 2009). In these prior investigations, a sequential combination of CBT techniques was followed by specific strategies and homework assignments to tailor dimensions of eudaimonic well-being. This sequential approach successfully addressed the complex balance of positive and negative affects characterized by inverse correlations. As a result, changes in well-being may induce a decrease in distress, and vice versa (Ruini & Fava, 2014).
The primary aim of this study was to determine the feasibility of a community-based group intervention based on principles of eudaimonic well-being – the Lighten UP! Program – and designed to promote psychological well-being in older adults. Given links between well-being and multiple aspects of physical and mental functioning (Diener, 2000; Steptoe, O’Donnell, Marmot, & Wardle, 2008), we also examined potential improvements in depression, life satisfaction, social well-being, physical symptoms, and sleep.
Method
This study was performed in collaboration with the Aging and Disability Resource Center (ADRC) of Kenosha County, Wisconsin. All aspects of the study were approved by the Health Sciences Institutional Review Board at the University of Wisconsin-Madison.
Men and women age 60 or over living independently in a Midwestern community in the U.S. were referred by community service organizations (e.g. Meals on Wheels) and recruited using advertisements in local newspapers and informational flyers. Candidate participants (N = 134) were screened for severe cognitive impairment using the short form of the Mini Mental State Examination (Haubois et al., 2011) by a trained staff member from the Kenosha County ADRC who was not otherwise involved in the intervention. Candidates with a score of 3 or below were excluded. The screener explained the study’s aims and procedures, and candidate participants had to provide their written informed consent.
Protocol
The protocol is based on a school program developed by Ruini et al. (Ruini et al., 2009) aimed at promoting eudaimonic well-being in a critical life stage, such as adolescence. A team of experts in aging populations composed by academic researchers (EF and CR) and by nurses and social workers with consolidated experiences in working with older adults (LVJ, RF, ES) was supervised by one of the school program developers (CR) and created a protocol that maintained the same group format and the same sequential approach. It encompassed the use of self observation in a structured diary, the use of psychoeducation and cognitive behavioral strategies, followed by a specific focus on dimensions of eudaimonic well-being. The protocol was adapted for older adults through the addition of age-appropriate exercises such as life review (Serrano, Latorre, Gatz, & Montanes, 2004). For example, the dimension of purpose in life, which was addressed in adolescents using techniques such as future goal planning, in older adults was adapted by asking participants to report past goal achievements and by sharing meaningful life experiences. Further, the Lighten up protocol contains two additional sessions (Session 6 and 8, see supplemental materials) describing the trajectories of well-being along the lifespan and their benefits in terms of physical and mental health. These sessions were not included in the previous school program since literature concerning eudaimonic well-being in adolescence did not provide such evidence. The final Lighten up protocol was revised and discussed among the researchers and ADRC staff until final consensus was reached and a structured manual for group leaders was created. It encompasses 8 90-minute group sessions to be delivered once per week in community settings (e.g. senior centers; public libraries).
The program is designed to teach participants to identify and savor positive experiences across multiple domains of eudaimonic well-being (Ryff, 1989; Ryff & Keyes, 1995). They also learn and apply principles of Cognitive Behavioral Therapy (CBT), such as identification of automatic thoughts and cognitive restructuring (Butler, Chapman, Forman, & Beck, 2006). The first classes focus on identifying positive experiences and introduce different conceptual domains of eudaimonic well-being. Later classes use CBT techniques to restore and sustain well-being (see supplemental materials for a week-by-week description). In-class activities are supported by at-home behavioral assignments and diaries in which participants record daily positive experiences and their reactions to them. Detailed description of Lighten UP! Protocol is provided in the Appendix.
Participants were placed into groups of 12–15. Two staff members from the Kenosha ADRC who had received initial training and supervision by the protocol developers administered the protocol following the structured manual for group leaders. They were not involved in subsequent procedures and data analysis.
Measures
Before and after the program, participants completed self-administered questionnaires consisting of diverse measures of mental and physical health. The measures were selected because they have all been shown to have significant associations with health and well-being in older adults, and they have been widely used in previous research on aging populations as well as in interventions for promoting well-being. Questionnaires were distributed to participants by the group leaders and then collected and mailed to the research team where data were entered and analyzed. Reliability statistics for each instrument are from the study sample.
Eudaimonic well-being was assessed using the Ryff Psychological Well-Being (PWB) scales (Ryff, 1989; Ryff & Keyes, 1995), including sub-scales assessing Environmental Mastery, Personal Growth, Purpose in Life, Positive Relations with Others, Self-Acceptance, and Autonomy (7 statement items for each scale; response options were 1=Disagree Strongly; 7=Agree Strongly). Possible scores ranged from 7–49 with higher scores indicating greater well-being. Internal reliability was good (Cronbach’s alpha =.90). Subjective well-being was assessed by the Satisfaction with Life Scale (SWLS) (Kobau, Sniezek, Zack, Lucas, & Burns, 2010), a 5-item scale that used the same 7 response options as the PWB scales. Possible scores ranged from 5–35. Internal reliability was excellent (alpha = .92). Depression was assessed using the Geriatric Depression Scale (GDS) (Yesavage, 1986), a set of 15 questions requiring a “yes” or “no” response. “Yes” responses were scored a ‘1’ and total score ranged from 0–15. Scores on the GDS were ln-transformed to impose a normal distribution for analyses. Internal reliability was good (alpha = .86).
Social connectedness was assessed by the Integration (3 items) and Contribution (3 items) subscales from the Keyes Social Well-Being Scale (Keyes, 1998). Participants responded to statements about social well-being using the same 7 response options. Internal reliability was .82 for the Integration subscale and .65 for the Contribution subscale.
The Kellner Symptom Questionnaire (Kellner, 1987) is a 92-item checklist of items grouped into 4 subscales – anxiety, depression, somatic symptoms, and hostility – each consisting of 23 items. Participants checked the box next to any emotion or feeling (e.g. “nervous,” “feeling friendly”) they experienced during the prior week. Check marks were scored a ‘1’ (range was 0–23 for each scale). Internal reliabilities ranged from .71 – .83.
Finally, respondents indicated how often they have trouble falling asleep, waking during the night, waking too early in the morning, and feel unrested during the day (response options: 1 = Never; 5 = Almost Always (4 or more times per week)). Possible scores ranged from 4–20.
Participants also completed a post-program qualitative survey with open-ended questions to evaluate their satisfaction and the quality of their experience during Lighten UP!
Statistical Analyses
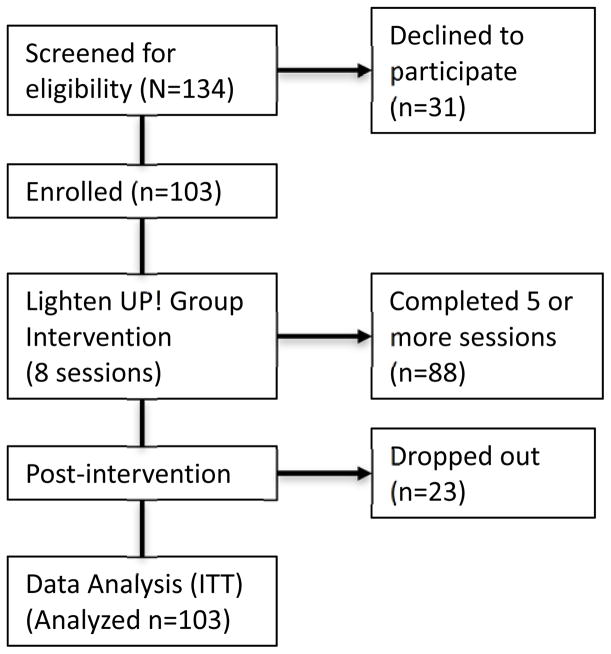
Repeated measures general linear models were used to estimate pre-post change in key outcome measures. Of the 103 participants who completed the pre-program assessments, 23 did not complete the post-program ones. Data were analyzed according to intention-to-treat approaches. An alpha of .05 was the threshold for statistically significant change. The flow diagram for Lighten UP! is shown in Figure 1.
Figure 1.
Lighten UP! flowchart.
Results
No participant who completed the initial screening and was eligible for the study declined to start the first class, although not all participants completed the program. One hundred and three (103) people were consented for participation and started the program, and 88 (85.4%) completed at least 5 classes (our criterion for “completion” for statistical analyses). Compared to those who attended fewer classes, those attending 5 or more rated their health better (2.7 vs. 2.3, p<.05; 1= poor; 5 = excellent) but were comparable on other measures. Mean age for “completers” was 71.7 (range: 59–97), 85% were women, 38.8% were married, and 40.8% had a college education or more. Twenty-five (25) people attended fewer than 5 classes (“drop-outs”), and most of these attended only the first class. The majority of the drop-outs (n = 18) did not provide reasons for not attending, and they did not respond to our attempts to contact them. Five people withdrew for health reasons and one person stopped attending because of winter road conditions.
Descriptive statistics for the final sample are shown in Table 1.
Table 1.
Descriptive Statistics.
| Variable | Mean (SD) or % | Range |
|---|---|---|
| Age | 71.7 (7.7) | 59 – 97 |
| Sex (% Female) | 85.6 | |
| % Married | 38.8 | |
| Educational Attainment (%) | ||
| High School or less | 34.0 | |
| Some college | 25.2 | |
| College or more | 40.8 | |
Aggregate eudaimonic well-being increased significantly between pre- and post-program assessments [F(1,102)=15.83, p<.001]. Supplemental analyses showed significant increases in Environmental Mastery, Personal Growth, Purpose in Life, and Self-Acceptance; increases in Autonomy and Positive Relations with Others were also observed but were not statistically significant (see Figure 2). Finally, to determine whether gains in eudaimonic well-being varied depending on participants’ initial well-being levels, we stratified the sample by tertiles of pre-program PWB scores and estimated a separate model for each tertile. The results showed significant gains for participants in the bottom (8% increase; η2partial = 0.23, P=.003) and middle thirds (4% increase; η2partial = 0.24, P=.003), but no change for those in the top tertile.
Figure 2.
Modification of Eudaimonic well-being following Lighten Up! intervention.
Note to Figure 2: All changes were statistically significant at P<.05 except for Autonomy (P = .19) and Positive Relations with Others (P = .07).
Scores on the Geriatric Depression Scale (GDS) decreased significantly [F(1,98)=34.54, p<.001]. Supplemental analyses showed significant declines in all three tertiles of GDS scores, although declines were more robust among participants in the middle (η2partial =.43) and top (η2partial = .32) tertiles compared to those in the lowest tertile (η2partial =0.10). Scores for anxiety [F(1,101) = 12.19, P = .001], depression [F(1,101) = 11.65, P = .001], hostility [F(1,101) = 17.72, P<.001], and somatic symptoms [F(1,101) = 10.13, P = .002] from the Symptom Questionnaire all declined significantly. Scores on the Satisfaction with Life Scale increased significantly [F(1,101)=18.55, P<.001] as did scores on the Social Integration [F(1,102) = 15.08, P<.001] and Social Contribution [F(1,101) = 5.26, P = .02] dimensions of the Social Well Being Scale. Finally, sleep complaints declined significantly [F(1,101) = 6.12, P = .02]. Supplemental analyses showed that the frequency of having trouble getting to sleep (P<.01) and feeling unrested during the day (P<.05) both declined significantly, while awakenings at night or in the early morning did not change.
Pre-post means and effect sizes for all key measures are shown in Table 2.
Table 2.
Pre-post changes in key measures. Means and standard errors are shown.
| Variable | Scale Range | Pre – Mean (SE) | Post – Mean (SE) | Effect Size (partial η2 ) |
|---|---|---|---|---|
| Eudaimonic well-being | 7 – 49 | 34.0 (0.5) | 35.3 (0.6) | 0.12*** |
| Geriatric Depression Scale | 0 – 15 | 3.4 (0.3) | 2.5 (0.3) | 0.26*** |
| Symptom Questionnaire | ||||
| Anxiety | 0 – 23 | 6.9 (0.4) | 5.7 (0.4) | 0.11** |
| Depression | 0 – 23 | 6.7 (0.4) | 5.6 (0.4) | 0.10** |
| Hostility | 0 – 23 | 4.5 (0.3) | 3.5 (0.3) | 0.15*** |
| Somatic Symptoms | 0 – 23 | 7.1 (0.3) | 6.4 (0.3) | 0.09** |
| Satisfaction with Life Scale | 5 – 35 | 21.1 (0.7) | 23.1 (0.7) | 0.15*** |
| Social Well Being Scale | ||||
| Social Integration | 1 – 7 | 4.9 (0.2) | 5.2 (0.2) | 0.13*** |
| Social Contribution | 1 – 7 | 5.3 (0.1) | 5.5 (0.1) | 0.05* |
| Sleep complaints | 4 – 20 | 10.8 (0.4) | 10.2 (0.3) | 0.06* |
| Trouble falling asleep | 2.8 (0.1) | 2.5 (0.1) | 0.09** | |
| Waking at night | 2.7 (0.1) | 2.7 (0.1) | 0.01 | |
| Early wakening in morning | 2.5 (0.1) | 2.5 (0.1) | 0.01 | |
| Feeling unrested | 2.8 (0.1) | 2.5 (0.1) | 0.05* | |
P<.001;
P<.01;
P<.05
Finally, Table 3 displays example answers to the qualitative survey performed after the intervention.
Table 3.
Selected responses to open-ended questions from Lighten UP! participants.
| What were some of the things you gained from Lighten UP? |
|
|
| “I learned that most of my bad feelings about getting old are fixable by me. My approach and outlook are paramount to getting through and enjoying the last part of me.” |
| “More aware of doing some things that were mundane but very important to my life.” |
| “Each day brings something of value.” |
|
|
| Have you made changes in your life or routines because of Lighten UP? |
|
|
| “I do things with friends more. I’m exercising more.” |
| “Took positive steps to control leg pain.” |
|
|
| What will you take away with you? |
|
|
| “…the trick is to continue on – even with the obstacle. E.g. on a cruise I rent a scooter so I can get where I want to go; but I still go.” |
| “I will pay more attention to my emotions. Recognize what I’m feeling and address it…maybe just let it go.” |
Discussion
The results of this pilot study suggest that the Lighten UP! Program is a feasible intervention that yielded positive effects in promoting psychological well-being in older adults. Eudaimonic well-being as measured using the Ryff PWB scales increased significantly albeit modestly from before Lighten UP! to afterward. Although the lack of a control group hampers any definitive conclusions, supplemental analyses showed that the largest gains were made among those with lower PWB scores prior to the intervention. To provide some context for these relatively modest increases, recent longitudinal assessments of eudaimonic well-being in approximately 3,900 middle aged and older adults over a 9–10 year period showed that individuals tend to have highly stable levels of well-being (Ryff, Radler, & Friedman, In Press). These results may have important implications, particularly for those with lower levels of eudaimonic well-being. Unlike hedonic well-being, which tends to increase with age (Gana, Bailly, Saada, Joulain, & Alaphilippe, 2013; Stone et al., 2010), decline or stability in eudaimonic well-being in older adults appears to be the norm. For this reason, even modest increases in well-being may constitute significant improvements in quality of life. On this point, participants’ own perceptions of improvements in their quality of life – examples shown in Table 3 – echo the results of the quantitative analyses and provide additional support for the perceived benefits of this new intervention.
In clinical settings, improvements on PWB through the use of WBT have been associated with lower relapse rates in patients with recurrent depression (Fava et al., 1998; Fava et al., 2004). Further, in school settings, eudaimonic well-being has been promoted through a specific group program that yielded benefits for anxiety and somatization which were maintained at 1 year follow up (Ruini et al., 2009). Even though the current pilot study lacks a controlled design, it replicates some of these prior findings and underscores the potential feasibility and utility of such interventions with older adults in community settings. Other positive psychology interventions tailored to older adults (Proyer et al., 2014; Ramirez et al., 2014) have been shown to increase life satisfaction, gratitude, forgiveness, and positive emotions. A critical question for these approaches as well as for Lighten UP! is how long these improvements last. Although most positive psychology interventions have shown benefits, such effects have tended to fade in the subsequent follow-up periods (Bolier et al., 2013; Seligman, Steen, Park, & Petersen, 2005). In contrast, previous interventions designed specifically to promote eudaimonic well-being have yielded beneficial effects lasting a year or longer (Fava et al., 2004; Ruini & Fava, 2009). These interventions consisted of a sequential administration of CBT techniques, followed by well-being enhancing psychotherapeutic strategies. Thus, the applications of multicomponent treatment modalities triggered a more complete and enduring recovery from affective disorders compared to the single administration of CBT (Fava et al., 2005), which was effective in reducing symptoms, but not in the specific promotion of eudaimonic well-being. Since Lighten UP! parallels the sequential administration of CBT and well-being enhancing strategies, it will be critical going forward to determine whether Lighten UP! will also have long-term benefits in older people compared to a control condition.
Beyond changes in eudaimonic well-being there were improvements in multiple other domains. Most notably, scores on the Geriatric Depression Scale declined by more than 25%. Considering the naturalistic design and the absence of a control group, this decline could be due to casual variations in depressive symptoms. However, the average decrease here of 1.1 points is comparable to the average increase in GDS score (1.2 points) from a study of older adults who had recently lost a spouse (Vinkers, Gussekloo, Stek, Westendorp, & Van Der Mast, 2004), suggesting that the changes observed here may be more than what would be expected from natural variation. In addition, physical symptoms in all domains assessed by the Kellner SQ declined significantly, while life satisfaction and social well-being improved significantly. Finally, participants reported fewer sleep complaints overall with specific improvements in falling asleep at night and feeling rested during the day. It is important to note that data for participants who did not complete the post-program assessment were based on their pre-program responses, consistent with the intention-to-treat approach. Thus, improvements were detected in the context of this conservative analytical strategy.
Results are limited by the use of self–report measures, self-selection of participants, and limited follow-up. The absence of a control group also means that we cannot dismiss the possibility that pre-post differences may reflect either natural variability in the assessed measures or possible benefits of something about Lighten UP! other than the specific well-being component. Nonetheless, the findings are promising, with improvements across a wide range of physical and mental health assessments. To our knowledge, Lighten UP! is the first group intervention aimed at promoting eudaimonic well-being in people aged 60 and over. The current study demonstrates the perceived benefits of the Lighten UP! program and illustrate the feasibility of delivering such a program to older adults in community settings. Future randomized controlled studies, with a larger sample and a longitudinal design, are needed to test the efficacy of this new program and its positive effects in promoting eudaimonic well-being and decreasing psychological distress in old age. The links between multiple dimensions of health and eudaimonic aspects of well-being, such as purpose in life, suggest that programs that help older adults sustain or increase well-being may also lead to broad improvements in length and quality of life.
Supplementary Material
Acknowledgments
The project described was supported by the Clinical and Translational Science Award (CTSA) program, through the NIH National Center for Advancing Translational Sciences (NCATS), grant UL1TR000427. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. Additional support was provided by the UW School of Medicine and Public Health from the Wisconsin Partnership Program, by the Community and Academic Aging Research Network (CAARN), and by the National Institute on Aging (AG041750 to EMF).
Footnotes
Disclosure
The Authors have no conflicts of interest to declare
References
- Bolier L, Haverman M, Westerhof GJ, Riper H, Smit F, Bohlmeijer E. Positive psychology interventions: a meta-analysis of randomized controlled studies. BMC Public Health. 2013;13:119. doi: 10.1186/1471-2458-13-119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyle PA, Barnes LL, Buchman AS, Bennett DA. Purpose in life is associated with mortality among community-dwelling older persons. Psychosom Med. 2009;71(5):574–579. doi: 10.1097/PSY.0b013e3181a5a7c0. doi:PSY.0b013e3181a5a7c0 [pii] 10.1097/PSY.0b013e3181a5a7c0 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyle PA, Buchman AS, Barnes LL, Bennett DA. Effect of a purpose in life on risk of incident Alzheimer disease and mild cognitive impairment in community-dwelling older persons. Arch Gen Psychiatry. 2010;67(3):304–310. doi: 10.1001/archgenpsychiatry.2009.208. doi:67/3/304 [pii] 10.1001/archgenpsychiatry.2009.208 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butler AC, Chapman JE, Forman EM, Beck AT. The empirical status of cognitive-behavioral therapy: a review of meta-analyses. Clin Psychol Rev. 2006;26(1):17–31. doi: 10.1016/j.cpr.2005.07.003. [DOI] [PubMed] [Google Scholar]
- Charles ST, Reynolds CA, Gatz M. Age-related differences and change in positive and negative affect over 23 years. J Pers Soc Psychol. 2001;80(1):136–151. [PubMed] [Google Scholar]
- Diener E. Subjective well-being. The science of happiness and a proposal for a national index. Am Psychol. 2000;55(1):34–43. doi: 10.1037/0003-066X.55.1.34. [DOI] [PubMed] [Google Scholar]
- Fava GA, Rafanelli C, Grandi S, Conti S, Belluardo P. Prevention of recurrent depression with cognitive behavioral therapy: preliminary findings. Arch Gen Psychiatry. 1998;55(9):816–820. doi: 10.1001/archpsyc.55.9.816. [DOI] [PubMed] [Google Scholar]
- Fava GA, Ruini C, Rafanelli C, Finos L, Conti S, Grandi S. Six-year outcome of cognitive behavior therapy for prevention of recurrent depression. Am J Psychiatry. 2004;161(10):1872–1876. doi: 10.1176/ajp.161.10.1872. [DOI] [PubMed] [Google Scholar]
- Fava GA, Ruini C, Rafanelli C, Finos L, Salmaso L, Mangelli L, Sirigatti S. Well-being therapy of generalized anxiety disorder. Psychother Psychosom. 2005;74(1):26–30. doi: 10.1159/000082023. doi:PPS2005074001026 [pii] 10.1159/000082023 [doi] [DOI] [PubMed] [Google Scholar]
- Friedman EM. Well-being, aging, and immunity. In: Segerstrom SC, editor. The Oxford Handbook of Psychoneuroimmunology. New York: Oxford University Press; 2012. pp. 37–62. [Google Scholar]
- Friedman EM, Ryff CD. Living well with medical comorbidities: a biopsychosocial perspective. J Gerontol B Psychol Sci Soc Sci. 2012;67(5):535–544. doi: 10.1093/geronb/gbr152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gana K, Bailly N, Saada Y, Joulain M, Alaphilippe D. Does life satisfaction change in old age: results from an 8-year longitudinal study. J Gerontol B Psychol Sci Soc Sci. 2013;68(4):540–552. doi: 10.1093/geronb/gbs093. [DOI] [PubMed] [Google Scholar]
- Gaymu J, Springer S. Living conditions and life satisfaction of older Europeans living alone: a gender and cross-country analysis. Ageing Soc. 2010;30:1153–1175. [Google Scholar]
- Haubois G, Annweiler C, Launay C, Fantino B, de Decker L, Allali G, Beauchet O. Development of a short form of Mini-Mental State Examination for the screening of dementia in older adults with a memory complaint: a case control study. BMC Geriatr. 2011;11:59. doi: 10.1186/1471-2318-11-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill PL, Turiano NA. Purpose in Life as a Predictor of Mortality Across Adulthood. Psychol Sci. 2014;25(7):1482–1486. doi: 10.1177/0956797614531799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kellner R. Symptom questionnaire. J Clin Psychiatry. 1987;48:269–274. [PubMed] [Google Scholar]
- Keyes CL. Social well-being. Soc Psychol Quarterly. 1998;61:121–140. [Google Scholar]
- Keyes CL, Shmotkin D, Ryff CD. Optimizing well-being: the empirical encounter of two traditions. J Pers Soc Psychol. 2002;82(6):1007–1022. doi: 10.1037/0022-3514.82.6.1007. [DOI] [PubMed] [Google Scholar]
- Kim ES, Strecher VJ, Ryff CD. Purpose in life and use of preventive health care services. Proc Natl Acad Sci U S A. 2014;111(46):16331–16336. doi: 10.1073/pnas.1414826111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim ES, Sun JK, Park N, Kubzansky LD, Peterson C. Purpose in life and reduced risk of myocardial infarction among older U.S. adults with coronary heart disease: a two-year follow-up. J Behav Med. 2013;36(2):124–133. doi: 10.1007/s10865-012-9406-4. [DOI] [PubMed] [Google Scholar]
- Kim ES, Sun JK, Park N, Peterson C. Purpose in life and reduced incidence of stroke in older adults: ‘The Health and Retirement Study’. J Psychosom Res. 2013;74(5):427–432. doi: 10.1016/j.jpsychores.2013.01.013. [DOI] [PubMed] [Google Scholar]
- Kobau R, Sniezek J, Zack MM, Lucas RE, Burns A. Well-being assessment: an evaluation of well-being scales for public health and population estimates of well-being amofn US adults. Appl Psychol. 2010;2(3):272–297. [Google Scholar]
- Pressman SD, Cohen S. Does positive affect influence health? Psychol Bull. 2005;131(6):925–971. doi: 10.1037/0033-2909.131.6.925. [DOI] [PubMed] [Google Scholar]
- Proyer RT, Gander F, Wellenzohn S, Ruch W. Positive psychology interventions in people aged 50–79 years: long-term effects of placebo-controlled online interventions on well-being and depression. Aging Ment Health. 2014;18(8):997–1005. doi: 10.1080/13607863.2014.899978. [DOI] [PubMed] [Google Scholar]
- Ramirez E, Ortega AR, Chamorro A, Colmenero JM. A program of positive intervention in the elderly: memories, gratitude and forgiveness. Aging Ment Health. 2014;18(4):463–470. doi: 10.1080/13607863.2013.856858. [DOI] [PubMed] [Google Scholar]
- Ruini C, Belaise C, Brombin C, Caffo E, Fava GA. Well-being therapy in school settings: a pilot study. Psychother Psychosom. 2006;75(6):331–336. doi: 10.1159/000095438. doi:95438 [pii] 10.1159/000095438 [doi] [DOI] [PubMed] [Google Scholar]
- Ruini C, Fava GA. Well-being therapy for generalized anxiety disorder. J Clin Psychol. 2009;65(5):510–519. doi: 10.1002/jclp.20592. doi:10.1002/jclp.20592 [doi] [DOI] [PubMed] [Google Scholar]
- Ruini C, Fava GA. Increasing happiness by Well-Being Therapy. In: Sheldon KM, Lucas RE, editors. Theories and Evidence on Whether Happiness can Change. New York: Academic Press; 2014. [Google Scholar]
- Ruini C, Ottolini F, Tomba E, Belaise C, Albieri E, Visani D, … Fava GA. School intervention for promoting psychological well-being in adolescence. J Behav Ther Exp Psychiatry. 2009;40(4):522–532. doi: 10.1016/j.jbtep.2009.07.002. doi:S0005-7916(09)00035-4 [pii] 10.1016/j.jbtep.2009.07.002 [doi] [DOI] [PubMed] [Google Scholar]
- Ryan RM, Deci EL. On happiness and human potentials: a review of research on hedonic and eudaimonic well-being. Annu Rev Psychol. 2001;52:141–166. doi: 10.1146/annurev.psych.52.1.141. [DOI] [PubMed] [Google Scholar]
- Ryff CD. Happiness is everything, or is it?: explorations on the meaning of psychological well-being. J Pers Soc Psychol. 1989;57:1069–1081. [Google Scholar]
- Ryff CD. Psychological well-being revisited: advances in the science and practice of eudaimonia. Psychother Psychosom. 2014;83(1):10–28. doi: 10.1159/000353263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryff CD, Keyes CL. The structure of psychological well-being revisited. J Pers Soc Psychol. 1995;69(4):719–727. doi: 10.1037/0022-3514.69.4.719. [DOI] [PubMed] [Google Scholar]
- Ryff CD, Radler BT, Friedman EM. Persistent psychological well-being predicts improved self-rated health over 9–10 years: Longitudinal evidence from Midlife in the United States. Health Psychol Open. doi: 10.1177/2055102915601582. (In Press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seligman ME, Steen TA, Park N, Petersen C. Positive psychology progress: empirical validation of interventions. Am Psychol. 2005;60:410–421. doi: 10.1037/0003-066X.60.5.410. [DOI] [PubMed] [Google Scholar]
- Serrano JP, Latorre JM, Gatz M, Montanes J. Life review therapy using autobiographical retrieval practice for older adults with depressive symptomatology. Psychol Aging. 2004;19(2):270–277. doi: 10.1037/0882-7974.19.2.270. [DOI] [PubMed] [Google Scholar]
- Springer KW, Pudrovska T, Hauser RM. Does Psychological Well-Being Change with Age?: Longitudinal Tests of Age Variations and Further Exploration of the Multidimensionality of Ryff’s Model of Psychological Well-Being. Soc Sci Res. 2011;40(1):392–398. doi: 10.1016/j.ssresearch.2010.05.008. doi:10.1016/j.ssresearch.2010.05.008 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steptoe A, Dockray S, Wardle J. Positive affect and psychobiological processes relevant to health. J Pers. 2009;77(6):1747–1776. doi: 10.1111/j.1467-6494.2009.00599.x. doi:JOPY599 [pii] 10.1111/j.1467-6494.2009.00599.x [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steptoe A, O’Donnell K, Marmot M, Wardle J. Positive affect, psychological well-being, and good sleep. J Psychosom Res. 2008;64(4):409–415. doi: 10.1016/j.jpsychores.2007.11.008. doi:S0022-3999(07)00451-5 [pii] 10.1016/j.jpsychores.2007.11.008 [doi] [DOI] [PubMed] [Google Scholar]
- Stone AA, Schwartz JE, Broderick JE, Deaton A. A snapshot of the age distribution of psychological well-being in the United States. Proc Natl Acad Sci U S A. 2010;107(22):9985–9990. doi: 10.1073/pnas.1003744107. doi:1003744107 [pii] 10.1073/pnas.1003744107 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vinkers DJ, Gussekloo J, Stek ML, Westendorp RG, Van Der Mast RC. The 15-item Geriatric Depression Scale (GDS-15) detects changes in depressive symptoms after a major negative life event. The Leiden 85-plus Study. Int J Geriatr Psychiatry. 2004;19(1):80–84. doi: 10.1002/gps.1043. [DOI] [PubMed] [Google Scholar]
- Webster JD, Bohlmeijer ET, Westerhof GJ. Time to flourish: the relationship of temporal perspective to well-being and wisdom across adulthood. Aging Ment Health. 2014;18(8):1046–1056. doi: 10.1080/13607863.2014.908458. [DOI] [PubMed] [Google Scholar]
- Wood AM, Joseph S. The absence of positive psychological (eudemonic) well-being as a risk factor for depression: a ten year cohort study. J Affect Disord. 2010;122(3):213–217. doi: 10.1016/j.jad.2009.06.032. [DOI] [PubMed] [Google Scholar]
- Yesavage R. The use of rating depression scales in the elderly. In: Poon L, editor. Memory Assessment of Older Adults. Washington, DC: American Psychological Association; 1986. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.