Abstract
Cigarette cravings, especially those in response to environmental stressors and other smoking-related triggers (e.g., passing by a favorite smoking spot), are important contributors to smoking behavior and relapse. Previous studies have demonstrated significant individual differences in such cravings. This study explores the possibility that attitudes about smoking can influence the experience of cigarette craving. Consistent with classical theories of the links between cognition and motivation, we predicted that smokers who exhibit more favorable attitudes towards smoking would have greater cravings. Daily smokers (n=103, mean age=41.8 years, 33% female) were instructed to imagine smoking, stress, and neutral scenarios. Cravings were measured prior to and after each exposure. Participants also completed an abridged version of the Smoking Consequence Questionnaire (SCQ) that had them rate the: 1) desirability and 2) likelihood, for eighteen separate negative smoking consequences (e.g., “The more I smoke, the more I risk my health”, “People will think less of me if they see me smoking”). Findings revealed that favorable attitudes about the consequences of smoking, as measured by the SCQ-desirability index, significantly predicted cigarette cravings. Findings suggest that individual attitudes toward smoking may play an important role in better understanding cigarette cravings, which may ultimately help identify targets for more efficient and effective cognitive/attitude-based interventions for smoking cessation.
Keywords: Smoking consequences questionnaire, attitudes, negative consequences, cigarette craving, cue-induced craving
1. Introduction
Cigarette smoking is a major public health concern worldwide. Estimates from the U.S., suggest that cigarette smoking is responsible for up to 20% of all deaths each year (U.S. Department of Health & Human Services, 2014). Despite the recognized negative health consequences of smoking, approximately 15% of adults from the U.S. reported in 2015 that they were currently smoking. (Jamal et al., 2016). Furthermore, while many smokers express the desire to quit, smoking cessation success rates are between 4 to 7% on any given attempt without assistance (American Cancer Society, 2014). Accumulating evidence has found that individual differences between smokers are critical in elucidating the underlying mechanisms of smoking initiation, maintenance and cessation (McClernon, Kozink, & Rose, 2008; Shiffman, Brockwell, Pillitteri, & Gitchell, 2008; Vink, Willemsen, & Boomsma, 2005). In particular, research focusing on cognitive and attitudinal factors has found that smokers who substantially minimize their perceptions of health-related smoking risks following a quit attempt are more likely to relapse (Gibbons, McGovern, & Lando, 1991).
Prior studies have demonstrated that smokers hold diverse perceptions about their own smoking risks. For instance, although they acknowledge that smoking increases health risks, many smokers minimize the magnitude of these risks—especially when comparing their own risk to that of other smokers (Weinstein, 1998). Besides perceptions of disease risk, other attitudes about the pros and cons of smoking have also been shown to predict smoking behavior. For example, Halpern-Fesher, Biehl, Kropp and Rubinstein (2004) found that smoking was negatively correlated with perceived negative consequences (e.g. bad breath, smelling of smoke) and positively correlated with perceived benefits (e.g. feeling relaxed, popularity). Accordingly, other studies have suggested that smokers—especially those who smoke daily and/or are nicotine-dependent—strongly believe that smoking improves mood, ability to cope with stress, and social enhancement; and, while they maximize the benefits of smoking, they deemphasize negative smoking consequences—including the unpleasant side effects and addictiveness (Arnett, 2000; Hendricks & Brandon, 2005; Mullenix, Kilbey, Fisicaro, Farnsworth, & Torrento, 2003; Pokhrel & Herzog, 2015).
Government guidelines have suggested that primary physicians should specifically address potential negative smoking consequences in order to motivate smokers to quit (Fiore et al., 2008). Similarly, public health campaigns often depict smoking consequences in an attempt to discourage initiation and to encourage cessation (Wakefield, Flay, Nichter, & Giovino, 2003; Durkin, Brennan, & Wakefield, 2012). Indeed, adolescents from the United States who minimized the long-term consequences of smoking were found to be more than three times more likely to initiate smoking (Song et al. 2009). Similarly, they were more than twice as likely to initiate smoking if they underestimated short-term consequences of smoking in comparison to their peers. Brandon and Baker (1991) and others (e.g., McCoy et al., 1992; Seigers & Terry, 2011) found that,, compared to non-smokers and ex-smokers, daily and occasional smokers of college age rated negative consequences as less likely to occur. Analogous results have been observed abroad (Aryal, Petzold, & Kretteck, 2013; Piko, 2001).
Motivations to quit and treatment outcomes have also been negatively associated with perceived risks (Costello, Logel, Fong, Zanna, & McDonald, 2012; Copeland & Brandon, 2000; Gibbons, McGovern, & Lando, 1991; Lipkus, Green, Feaganes & Sedikides, 2001; McKee, O’Malley, Salovey, Krishnan-Sarin, & Mazure, 2005; Wetter et al., 1994). For example, McKee et al. (2005) observed that smokers who perceived risks of smoking as more likely had greater pretreatment motivation to quit. Gibbons, McGovern and Lando (1991) demonstrated that following a quit attempt, relapsers had significantly lowered their perceptions of smoking risks from their original rating prior to cessation, while abstainers’ perceptions remained the same. Taken together, these findings demonstrate the important role of risk perceptions in smoking cessation.
An independent literature has highlighted the importance of drug craving as a contributor to the maintenance of drug use, as well as quit failure (Conklin et al., 2015; Erblich & Bovbjerg, 2004; Franken, 2003; Pickens & Johanson, 1992; Piasecki, 2006; Tiffany and Wray, 2011). For example, Killen and Fortman (1997) found that craving was a significant predictor of relapse in a combined sample of more than 2,600 smokers from three separate cessation studies. In addition to these “tonic” levels of craving, research has consistently demonstrated that smokers exhibit powerful “phasic” craving reactions in response to being exposed to smoking paraphernalia (Carter & Tiffany, 1999), and when under stress (Sinha, 2009). Ubiquitous presence of cues and stressors in the environment, and their attendant phasic cravings, has been postulated as another important contributor to smoking cessation failure (Ferguson & Shiffman, 2009). Although many theories of cue- and stress-induced craving have been advanced, including biological models (Robinson & Berridge, 1993), cognitive models (Tiffany, 1990), and conditioning models (Siegel, 1983; Stewart, de Wit and Eikelboom, 1984), little research has been done to evaluate the potential role of attitudinal factors on craving. The possibility that attitudes and beliefs about drugs predict craving is generally consistent with a number of classical theoretical models of behavior, including Festinger’s (1957) Cognitive Dissonance Theory and Ajzen’s (1985) Theory of Planned Behavior (see also Armitage & Conner, 2001). Indeed, these theories highlight the importance of attitudinal factors as predictors of behavior. As one example, using the Theory of Planned Behavior, Spijkerman et al. (2004) found that attitudes toward smoking and drinking predicted willingness and desire to drink in the future. Similarly, in an experimental study, Simmons et al. (2004) found that increasing cognitive dissonance about the benefits of smoking increased intentions to quit. What has received less attention, however, is the possibility that attitudes are related to actual urges for drug use, which may in turn be the driving force behind the resultant motivated behavior. The influence of smoking attitudes on cravings may be particularly salient when facing a specific smoking trigger (e.g., smoking cue, stress) that activates motivation to smoke. Consistent with this possibility, one study found that explicit positive smoking reinforcement expectancies predicted cue-induced craving (Palfai, 2002). Another study found that implicit positive attitudes about smoking were related to “tonic” craving levels (Waters et al. 2007). To our knowledge, however, no study has explored how negative smoking attitudes influence cravings in dependent adult smokers.
In this study, we aimed to evaluate the possible relationship between self-reported attitudes about the negative consequences of smoking and cravings. Our primary hypothesis was that smokers who exhibited more favorable attitudes towards smoking would have: 1) higher basal levels of cigarette cravings, 2) higher levels of cravings when exposed to smoking cues, and 3) higher levels of cravings when exposed to stress.
2. Methods and Materials
2.1 Participants
Advertisements posted in and around a medical center in New York City were used to recruit cigarette smokers to a study of attitudes about smoking and cigarette craving. Participants had to be at least 23 years old, had been smoking at least 10 cigarettes per day for the past 5 years (minimum purchase age at the time of the study was 18) and met the criteria for DSM-IV diagnosis of nicotine dependence (American Psychiatric Association, 1994). Exclusion criteria were: 1) current treatment for smoking cessation, 2) a history of other substance abuse, and 3) a history of hospitalization for major mental illness. Inclusion and exclusion criteria were described in detail in the advertisements, and all respondents to the ads met screening criteria. Six respondents left messages indicating interest in participating, but could not be reached. A total of 110 eligible participants were enrolled in the study, and 7 did not return for the second session, yielding a final sample of 103 participants. Each participant was compensated $40 for completing the study
2.2 Measures
Background Questionnaires
Participants’ completed a demographic questionnaire assessing age, gender, ethnicity and education. In addition to demographic information, participants also completed a face-valid smoking history questionnaire, including items assessing the number cigarettes smoked per day, age at initiation, years smoked, and number of quit attempts.
Fagerstrom Test of Nicotine Dependence (FTND)
The 6-item FTND was used to assess the degree of participants’ nicotine dependence. The FTND is a valid and reliable instrument (Heatherton, Kozlowski, Frecker and Fagerstrom, 1991), and has been widely used in the smoking literature.
Smoking Consequences Questionnaire- Adult (SCQ-A)
The Smoking Consequences Questionnaire (SCQ) is a well-established tool that measures smokers’ beliefs and attitudes about positive and negative consequences of smoking—both long- and short-term. Originally developed by Brandon and Baker (1991) for college-aged individuals in the United States, the questionnaire has since been modified and validated to measure perceptions in adult populations in the U.S. and abroad (Copeland, Brandon, & Quinn, 1995; Cepeda-Benito, & Reig Ferrer, 2000). The initial questionnaire consisted of 50-items, divided into four scales: 1) Negative Consequences, 2) Positive Reinforcement, 3) Negative Reinforcement, and 4) Appetite/Weight Control. Because the focus of the study was on the perceptions of negative consequences, participants only completed the Negative Consequences scale of the Smoking Consequences Questionare-Adult (SCQ-A). This brief scale contained 16 items describing the potential Negative Consequences (e.g., “Smoking is taking years off my life”, “People think less of me if they see me smoking”). Copeland, Brandon and Quinn (1995) also further divided the Negative Consequences scale into four subscales for the SCQ-A (i.e., Health Risk, Negative Physical Feelings, Negative Social Impressions, and Craving/Addiction). Items were randomly presented to participants and were not chunked by subscale. Because the objective of the study was to relate negative consequences to craving outcomes, the six Craving/Addiction items were omitted from the analyses (yielding a 10-item scale for analysis) even though they were presented to participants during the survey.
As with the full SCQ, participants were instructed to first rate the desirability of each consequence on a scale of −5 (extremely undesirable) to +5 (extremely desirable). Next, they rated the likelihood of each on a scale of 0 (extremely likely) to 9 (extremely unlikely). The instrument yielded three scores per item: 1) Desirability, 2) Likelihood, and 3) Subjective Expected Utility (SEU) (Baker & Brandon, 1991), which is calculated by multiplying the desirability and likelihood responses for each item. The SEU index is thought to characterize a decision making processes rooted in both subjective evaluations and estimated probabilities of plausible outcomes. Cronbach’s alpha in this sample ranged from 0.88 to 0.93 for the three SCQ scores (desirability, likelihood, SEU), reflecting excellent internal consistency.
Cigarette Craving Questionnaire
To measure craving levels at baseline and during cue-exposure, participants were asked to rate five items (“I crave a cigarette right now,” “I have an urge for a cigarette right now,” “I have a desire for a cigarette right now,” If it were possible, I would smoke right now,” “All I want right now is a cigarette”) on a scale of 0 (not at all) to 100 (strongest feeling possible) immediately before and immediately after each cue exposure. As in prior studies (Hutchinson, LaChance. Niaura, Bryan, & Smolen, 2002; Erblich, Boyarsky, Spring, Niaura & Bovberg, 2003), the five items were averaged to obtain an overall craving score. Coefficient alpha across the four administrations ranged from 0.83 to 0.96, reflecting excellent internal consistency.
2.3 Procedures
Participants came to the laboratory for the study on two separate days, approximately one week apart. During the first study session, they completed the demographic, smoking history questionnaires, and the SCQ. Prior to their second visit, they were instructed to smoke one cigarette immediately before the experimental session. As in previous studies (Erblich & Bovbjerg, 2004), this was done to avoid possible ceiling effects during the craving task (see below).
Upon arrival for the second session, participants took part in a cue- and stress-induced craving task. Consistent with well-established methods in our lab and others (e.g., Erblich and Bovbjerg, 2004; Maude-Grifffin and Tiffany, 1996), participants were exposed to smoking cues, mild stress cues, and neutral cues in counterbalanced order. We used imaginal cues, which are thought to yield similar craving effects to standard in vivo cues (Erblich and Bovbjerg, 2004), but may have the added benefit of triggering more of the cognitive representations of smoking urge (Tiffany, 1990). Standard scripts were utilized, based on the imaginal cues used by Maude-Griffin and Tiffany (1996). Neutral imagery involved changing a lightbulb, the stress imagery involved a trip to the dentist and anticipating undergoing painful dental work, and the smoking imagery involved smoking a cigarette following a meal. Participants listened with their eyes closed to each 60-second script and then were allowed an additional 30 seconds to continue to imagine the scene as vividly as possible. To familiarize participants with the procedure, a practice script involving a trip to the grocery store was read prior to the experimental cues. Craving was measured immediately before and after each exposure. Finally, between each presentation, participants viewed a 3-minute nature video (Hannan, 1999) to minimize potential carryover effects (Piferi, Kline, Younger, & Lawler, 2000).
2.4 Data Analysis
Preliminary review of the data revealed sporadic missing values on the SCQ items. Pattern mixture methods revealed 2.4% of the data to be missing at random (MAR). Because performing listwise deletion would have resulted in significant data loss and potentially biased results, we employed multiple imputation techniques, using the study variables as predictors.
We then conducted a repeated measures ANOVA, with Exposure [neutral, smoking, stress] and Time [pre-exposure, post-exposure] as within-subjects factors, to confirm that the experimental manipulations elicited craving responses. To address the study’s hypothesis, we then added participants’ ratings of smoking consequences (likelihood, desirability, and SEU) as predictors, and tested the Smoking Consequences x Time x Exposure interaction terms to determine whether smoking consequences predicted craving responses.
3. Results
3.1 Background Variables
Of the 103 participants, 33% were female (n=34) and 67% were male (n=69). The mean age of the sample was 41.8 years (SD=6.4). Forty percent of the participants reported African American ethnicity, 14% reported Hispanic ethnicity, 12% reported Caucasian ethnicity, and 34% reported other ethnic backgrounds. Thirty-nine percent of participants reported having a high school education or lower. Participants reported smoking a mean of 18.6 cigarettes (SD=11.4) per day. On average, participants had smoked for 21.0 (SD= 9.2) years and 89.3% had attempted to quit at least once. The mean FTND score of the sample was 6.5 (SD= 2.11). Preliminary analyses indicated that there were no effects of ethnicity on craving at any of the assessment points (p’s > 0.15), and only sporadic effects of gender, with women reporting higher cravings following neutral imagery (p <0.03) and prior to smoking imagery (p < 0.04) than men. Inclusion of gender and/or ethnicity as covariates in the primary analyses did not impact the results.
3.2. Cue- and Stress-Induced Cigarette Cravings
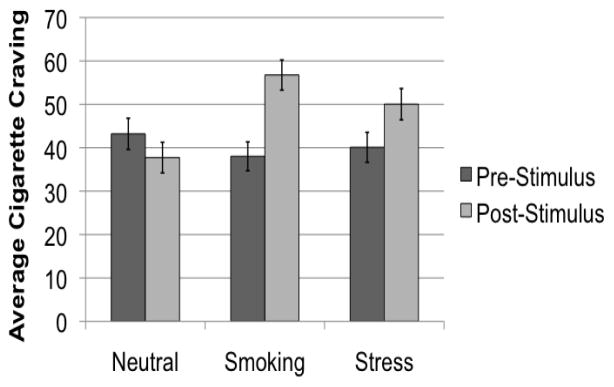
We first examined the effects of smoking and stress exposures on cigarette craving responses. As expected, smoking and stress imagery both elicited significant craving responses (Figure 1). A significant Time [pre exposure, post exposure] x Exposure [neutral, smoking, stress] interaction revealed an increase in craving levels in response to both smoking and stress imagery, but a decrease in cravings following exposure to neutral imagery: F(1,101)= 28.33, p< .0001, η2=0.22.
Figure 1.
Cigarette craving scores before and after exposure to neutral, smoking and stress stimuli. The Time (Pre-exposure, Post-exposure) x Exposure (Neutral, Smoking, Stress) interaction was significant; p < 0.0001.
3.2. Smoking Consequences and Cigarette Cravings
Next, we tested our primary hypothesis that smokers who exhibited more favorable attitudes towards smoking would have greater cue- and stress-induced cravings. To investigate this relationship, we analyzed participants’ SCQ likelihood, desirability and SEU scores as possible moderators of these craving responses for all cues. Interestingly, we identified a significant three-way Time (pre- vs. post-exposure) X Exposure (Neutral, Smoking, Stress) x Consequence interaction, but only for the desirability index, F(2,97)= 7.2, p=.001, η2=0.13. Effects of likelihood and SEU, on the other hand, were found not to be significant, p’s > .05. To probe the significant interaction effect, we examined the two-way Time x Consequence interactions for each of the three exposures. Interestingly, findings indicated that there was a significant interaction for the SCQ-desirability index during the smoking imagery, F(1, 101)= 8.99, p < 0.003, η2=0.08. Similarly, we observed a significant Time x Consequence interaction for the SCQ-desirability index during the stress imagery, F(1, 101)= 7.73, p= .006, η2=0.07, but not during the neutral imagery, p > 0.05.
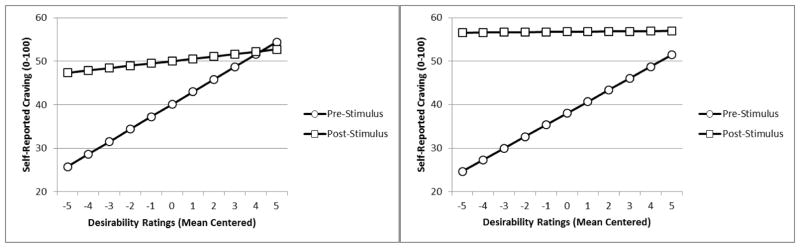
3.3 Slope Analyses
To better understand the nature and direction of the interaction effects, we conducted simple slopes analyses, as recommended by Aiken and West (1991). We mean-centered the desirability ratings and calculated slopes for the relationships between desirability and both pre- and post-exposure craving. Surprisingly, simple slopes analyses revealed that the effects were driven by changes in primarily pre-exposure cravings for both smoking (b=2.7) and stress imagery (b=2.9) [Figure 2]. Slopes for post smoking- and stress-imagery cravings were not statistically different from 0 (b’s of 0.04 and 0.54, respectively). Smokers who rated smoking consequences as less desirable had lower pre-stimulus cravings than those who minimized consequences, while post-stimulus craving levels were relatively insensitive to changes in desirability ratings.
Figure 2.
Regression lines depicting the relationship between desirability ratings and cigarette cravings before and after laboratory exposure to smoking cues. Stress exposure left; Smoking exposure right.
3.4 Subscales of Negative Consequences in Relation to Craving Responses
Lastly, we examined whether there were differences in how each Negative Consequence Subscale predicted cigarette craving levels prior to and after exposures to imagery. Findings indicated that all subscales (except for Health Risk, which was only a borderline significant predictor of craving, p < 0.059) significantly predicted craving responses to smoking and stress cues, suggesting that the effects were not subscale-specific (all p’s < 0.05).
4. Discussion
The purpose of this study was to evaluate the potential role of attitudinal factors on cigarette cravings in nicotine-dependent adult daily smokers. Findings revealed that the perceived desirability of the negative consequences of smoking, were predictive of smokers’ cigarette cravings. Interestingly, and in contrast with some prior studies that found that SCQ likelihood scores moderated smoking behavior (Brandon & Baker, 1991), neither likelihood nor SEU predicted cravings in this sample. As the mean likelihood rating for negative consequences in the original SCQ sample (Brandon & Baker, 1991) was approximately double the mean in our sample, a possible explanation is that the probability of the consequences of smoking are now, over 25 years later, more widely accepted, and thus less predictive of motivation to smoke.
While our primary hypothesis was that smokers who exhibited more favorable attitudes towards smoking would have higher levels of both pre-exposure and cue-induced cravings, results indicated that effects were driven primarily by differences in pre-exposure cravings. Indeed, simple slopes analyses revealed that attitudes about the negative consequences of smoking were more strongly related to pre-stimulus cravings, rather than to responses to cues. Smokers who rated negative consequences as less desirable had lower initial cravings than those who minimized consequences; however, post-stimulus craving levels were comparable across desirability ratings. These results suggest that cue- and stress-induced cravings may be particularly great for individuals who report low levels of smoking desirability. Among smokers who report high levels of smoking desirability, tonic craving levels are high, and exposure to neither stressful stimuli nor smoking-related stimuli further increase these cravings.
Our findings are in general accord with the previous literature that has found that attitudes toward smoking may influence cigarette cravings and motivations to smoke. Waters et al. (2007), for instance, found that smokers’ implicit positive attitudes about smoking were positively associated with self-reported basal cravings. Palfai (2002), on the other hand, found that positive attitudes toward smoking predicted increased cue-induced craving. The present results suggest that, at least with respective to the negative consequences of smoking, both cue- and stress-induced craving reactions are most apparent among smokers who rate these consequences least favorably. While these findings at first glance may seem counterintuitive, they represent a direct relationship between increased favorable attitudes and pre-stimulus craving levels, which may mask cue- and stress-induced effects at higher levels of favorability, when pre-stimulus cravings are already quite high.
There are several limitations to the present study. First, the study was cross-sectional in nature. As such, we cannot determine how attitudes and craving responses predict smoking outcomes. Additional research is needed to elucidate how individual attitudes influence cravings at all stages of smoking—initiation, dependence and cessation. Similarly, while this study focused on cigarette craving, there are other important motivational factors that may predict smoking outcomes. For example, future studies could investigate how attitudes regarding smoking consequences influence other types of motivational factors (i.e., money spent on cigarettes, effort to obtain cigarettes, and other behavioral economic measures of demand for cigarette consumption). Also, the size of the sample was modest, although the use of repeated measures afforded the additional power of multiple observations per subject. Finally, we only used one of the SCQ-A scales, while omitting some of the items relating to craving. It remains unclear whether administering only a subset of the SCQ-A retains the full psychometric integrity of the instrument. Nevertheless, Cronbach’s alpha for the administered items in this sample was excellent, suggesting that reliability of the scale was maintained.
Despite the limitations, the current findings provide further support for the importance of attitudinal factors in understanding the motivation to smoke. One potential implication of this line of research would be to place additional emphasis on the exploration of attitudes toward smoking as a direct method of managing urges to smoke. Another implication of this work is to focus our study of cue- and stress-induced cigarette cravings on smokers with less desirable attitudes towards smoking. Follow-up prospective studies of attitudes, craving and smoking outcomes may be warranted to further explore this possibility. In addition, studies aimed at exploring factors that modify these effects (e.g., social support, delay discounting), may further elucidate the potentially complex relationship between smoking attitudes, cigarette cravings, and smoking behavior.
HIGHLIGHTS.
Laboratory exposure to smoking and stress imagery induced cigarette craving.
Favorable smoking attitudes predicted higher craving levels.
Result support a link between smoking-related attitudes and motivation to smoke.
Acknowledgments
Supported by NIH Grant # R34 DA031327; No conflicts of interest to report.
Footnotes
Author Disclosures
Funding for this study was provided by NIH Grant #R34A031327. NIH had no role in the study design, collection, analysis or interpretation of the data, writing the manuscript, or the decision to submit the paper for publication.
All authors contributed to conceptualization of the research, contributed to the writing of the manuscript and have approved the final version.
All authors declare that they have no conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Ajzen I. Action Control. Springer; Berlin Heidelberg: 1985. From intentions to actions: A theory of planned behavior; pp. 11–39. [Google Scholar]
- Aiken L, West S. Multiple regression: Testing and interpreting interactions. Newbury Park, CA: Sage Publications; 1991. [Google Scholar]
- American Cancer Society. Guide to Quit Smoking. 2014 Retrieved from http://www.cancer.org/Healthy/StayAwayfromTobacco/GuidetoQuittingSmoking/deciding-to-quit-smoking-and-making-a-plan.
- Armitage CJ, Conner M. Efficacy of the theory of planned behaviour: A meta-analytic review. British journal of social psychology. 2001;40(4):471–499. doi: 10.1348/014466601164939. [DOI] [PubMed] [Google Scholar]
- Arnett JJ. Optimistic bias in adolescent and adult smokers and nonsmokers. Addictive Behaviors. 2000;25(4):625–632. doi: 10.1016/s0306-4603(99)00072-6. [DOI] [PubMed] [Google Scholar]
- Aryal UR, Petzold M, Krettek A. Perceived risks and benefits of cigarette smoking among Nepalese adolescents: a population-based cross-sectional study. BMC Public Health. 2013;13(187):1–9. doi: 10.1186/1471-2458-13-187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brandon TH, Baker TB. The Smoking Consequences Questionnaire: The subjective expected utility of smoking in college students. Psychological Assessment: A Journal of Consulting and Clinical Psychology. 1991;3(3):484–491. [Google Scholar]
- Cepeda-Benito A, Reig Ferrer A. Smoking Consequences Questionnaire—Spanish. Psychology of Addictive Behaviors. 2000;14(3):219–230. doi: 10.1037//0893-164x.14.3.219. [DOI] [PubMed] [Google Scholar]
- Conklin CA, Vella EJ, Joyce CJ, Salkeld RP, Perkins KA, Parzynski CS. Examining the relationship between cue-induced craving and actual smoking. Experimental and Clinical Psychopharmacology. 2015;23(2):90–96. doi: 10.1037/a0038826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Copeland AL, Brandon TH. Testing the causal role of expectancies in smoking motivation and behavior. Addictive Behaviors. 2000;25(3):445–449. doi: 10.1016/s0306-4603(99)00003-9. [DOI] [PubMed] [Google Scholar]
- Copeland AL, Brandon TH, Quinn EP. The Smoking Consequences Questionnaire-Adult: Measurement of smoking outcome expectancies of experienced smokers. Psychological Assessment. 1995;7(4):484–494. [Google Scholar]
- Costello MJ, Logel C, Fong GT, Zanna MP, McDonald PW. Perceived risk and quitting behaviors: results from the ITC 4-country survey. American Journal of Health Behavior. 2012;36(5):681. doi: 10.5993/AJHB.36.5.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Durkin S, Brennan E, Wakefield M. Mass media campaigns to promote smoking cessation among adults: an integrative review. Tobacco Control. 2012;21(2):127–138. doi: 10.1136/tobaccocontrol-2011-050345. [DOI] [PubMed] [Google Scholar]
- Drummond DC. What does cue-reactivity have to offer clinical research? Addiction. 2000;95:S129–144. doi: 10.1080/09652140050111708. [DOI] [PubMed] [Google Scholar]
- Erblich J, Bovbjerg D. In vivo versus imaginal smoking cue exposures: Is seeing believing? Experimental and Clinical Psychopharmacology. 2004;12(3):208–215. doi: 10.1037/1064-1297.12.3.208. [DOI] [PubMed] [Google Scholar]
- Erblich J, Boyarsky Y, Spring B, Niaura R, Bovbjerg HD. A family history of smoking predicts heightened levels of stress-induced cigarette craving. Addiction. 2003;98(5):657–664. doi: 10.1046/j.1360-0443.2003.00351.x. [DOI] [PubMed] [Google Scholar]
- Ferguson SG, Shiffman S. The relevance and treatment of cue-induced cravings in tobacco dependence. Journal of Substance Abuse Treatment. 2009;36(3):235–243. doi: 10.1016/j.jsat.2008.06.005. [DOI] [PubMed] [Google Scholar]
- Festinger L. A theory of cognitive dissonance. Evanston, IL: Row, Peterson; 1957. [Google Scholar]
- Fiore MC, Jaen CR, Baker TB, Bailey WC, Benowitz NL, Curry SJ, … Wewers ME. Treating tobacco use and dependence: 2008 update-clinical practice guideline. Rockville, MD: U.S. Department of Health and Human Services, Public Health Service; 2008. [Google Scholar]
- Franken IH. Drug craving and addiction: integrating psychological and neuropsychopharmacological approaches. Progress in Neuropsychopharmacology and Biological Psychiatry. 2003;27(4):563–579. doi: 10.1016/S0278-5846(03)00081-2. [DOI] [PubMed] [Google Scholar]
- Gibbons FX, McGovern PG, Lando HA. Relapse and risk perception among members of a smoking cessation clinic. Health Psychology. 1991;10(1):42–45. doi: 10.1037//0278-6133.10.1.42. [DOI] [PubMed] [Google Scholar]
- Halpern-Felsher BL, Biehl M, Kropp RY, Rubinstein ML. Perceived risks and benefits of smoking: differences among adolescents with different smoking experiences and intentions. Preventive Medicine. 2004;39(3):559–567. doi: 10.1016/j.ypmed.2004.02.017. [DOI] [PubMed] [Google Scholar]
- Hannan D. Coral Sea Dreaming. DVD International; Mountain Lakes, NJ: 1999. [Google Scholar]
- Hendricks PS, Brandon TH. Smoking expectancy associates among college smokers. Addictive Behaviors. 2005;30(2):235–245. doi: 10.1016/j.addbeh.2004.05.006. [DOI] [PubMed] [Google Scholar]
- Hutchison KE, LaChance H, Niaura R, Bryan A, Smolen A. The DRD4 VNTR polymorphism influences reactivity to smoking cues. Journal of Abnormal Psychology. 2002;111(1):134–143. doi: 10.1037//0021-843x.111.1.134. [DOI] [PubMed] [Google Scholar]
- Jamal A, King BA, Neff LJ, Whitmill J, Babb SD, Graffunder CM. Current Cigarette Smoking Among Adults — United States, 2005–2015. MMWR Morbitity and Morality Weekly Report. 2016;65:1205–1211. doi: 10.15585/mmwr.mm6544a2. [DOI] [PubMed] [Google Scholar]
- Juliano LM, Brandon TH. Reactivity to Instructed Smoking Availability and Environmental Cues: Evidence With Urge and Reaction Time. Experimental and Clinical Psychopharmacology. 1998;6(1):45–53. doi: 10.1037//1064-1297.6.1.45. [DOI] [PubMed] [Google Scholar]
- Killen JD, Fortmann SP. Craving is associated with smoking relapse: findings from three prospective studies. Experimental and Clinical Psychopharmacology. 1997;5(2):137–142. doi: 10.1037//1064-1297.5.2.137. [DOI] [PubMed] [Google Scholar]
- Lipkus IM, Green JD, Feaganes JR, Sedikides C. The relationship between attitudinal ambivalence and desire to quit smoking among college smokers. Journal of Applied Social Psychology. 2001;31(1):113–133. [Google Scholar]
- Maude-Griffin P, Tiffany ST. Production of smoking urges through imagery: The impact of affect and smoking abstinence. Experimental and Clinical Psychopharmacology. 1996;4(2):198–208. [Google Scholar]
- McClernon FJ, Kozink RV, Rose JE. Individual differences in nicotine dependence, withdrawal symptoms, and sex predict transient fMRI-BOLD responses to smoking cues. Neuropsychopharmacology. 2008;33(9):2148–2157. doi: 10.1038/sj.npp.1301618. [DOI] [PubMed] [Google Scholar]
- McCoy SB, Gibbons FX, Reis TJ, Gerrard M, Luus CE, Sufka AVW. Perceptions of smoking risk as a function of smoking status. Journal of Behavioral Medicine. 1992;15(5):469–488. doi: 10.1007/BF00844942. [DOI] [PubMed] [Google Scholar]
- McKee SA, O’Malley SS, Salovey P, Krishnan-Sarin S, Mazure CM. Perceived risks and benefits of smoking cessation: gender-specific predictors of motivation and treatment outcome. Addictive behaviors. 2005;30(3):423–435. doi: 10.1016/j.addbeh.2004.05.027. [DOI] [PubMed] [Google Scholar]
- Mullennix JW, Kilbey MA, Fisicaro SA, Farnsworth LM, Torrento R. The representation of smoking expectancies by single-word adjectives and their relationship to smoking characteristics. Nicotine & Tobacco Research. 2003;5(5):681–94. doi: 10.1080/1462220031000158654. [DOI] [PubMed] [Google Scholar]
- Palfai TP. Positive outcome expectancies and smoking behavior: The role of expectancy accessibility. Cognitive Therapy and Research. 2002;26(3):317–333. [Google Scholar]
- Piasecki TM. Relapse to smoking. Clinical Psychology Review. 2006;26(2):196–215. doi: 10.1016/j.cpr.2005.11.007. [DOI] [PubMed] [Google Scholar]
- Pickens RW, Johanson CE. Craving: consensus of status and agenda for future research. Drug and Alcohol Dependence. 1992;30(2):127–131. doi: 10.1016/0376-8716(92)90017-7. [DOI] [PubMed] [Google Scholar]
- Piferi RL, Kline KA, Younger J, Lawler KA. An alternative approach for achieving cardiovascular baseline: viewing an aquatic video. International Journal of Psychophysiology. 2000;37(2):207–217. doi: 10.1016/s0167-8760(00)00102-1. [DOI] [PubMed] [Google Scholar]
- Piko B. Smoking in adolescence: Do attitudes matter? Addictive Behaviors. 2001;26(2):201–217. doi: 10.1016/s0306-4603(00)00101-5. [DOI] [PubMed] [Google Scholar]
- Pokhrel P, Herzog TA. Reasons for quitting cigarette smoking and electronic cigarette use for cessation help. Psychology of Addictive Behaviors. 2015;29(1):114–121. doi: 10.1037/adb0000025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson TE, Berridge KC. The neural basis of drug craving: an incentive-sensitization theory of addiction. Brain Research Reviews. 1993;18(3):247–291. doi: 10.1016/0165-0173(93)90013-p. [DOI] [PubMed] [Google Scholar]
- Seigers DK, Terry CP. Perceptions of risk among college smokers: relationships to smoking status. Addiction Research & Theory. 2011;19(6):504–509. [Google Scholar]
- Shiffman S, Brockwell SE, Pillitteri JL, Gitchell JG. Individual differences in adoption of treatment for smoking cessation: demographic and smoking history characteristics. Drug and alcohol dependence. 2008;93(1):121–131. doi: 10.1016/j.drugalcdep.2007.09.005. [DOI] [PubMed] [Google Scholar]
- Siegel S. Research advances in alcohol and drug problems. Springer; US: 1983. Classical conditioning, drug tolerance, and drug dependence; pp. 207–246. [Google Scholar]
- Simmons VN, Webb MB, Brandon TH. College-student smoking: an initial test of an experiential dissonance-enhancing intervention. Addictive Behaviors. 2004;29(6):1129–1136. doi: 10.1016/j.addbeh.2004.03.005. [DOI] [PubMed] [Google Scholar]
- Sinha R. Modeling stress and drug craving in the laboratory: Implications for addiction treatment development. Addiction Biology. 2009;14(1):84–98. doi: 10.1111/j.1369-1600.2008.00134.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song AV, Morrell HE, Cornell JL, Ramos ME, Biehl M, Kropp RY, Halpern-Felsher BL. Perceptions of smoking-related risks and benefits as predictors of adolescent smoking initiation. American Journal of Public Health. 2009;99(3):487–92. doi: 10.2105/AJPH.2008.137679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spijkerman R, van der Eijnden RJ, Vitale S, Engels RC. Explaining adolescents’ smoking and drinking behavior: the concept of smoker and drinker prototypes in relation to variables of the theory of planned behavior. Addictive Behaviors. 2004;29(8):1615–1622. doi: 10.1016/j.addbeh.2004.02.030. [DOI] [PubMed] [Google Scholar]
- Stewart J, De Wit H, Eikelboom R. Role of unconditioned and conditioned drug effects in the self-administration of opiates and stimulants. Psychological Review. 1984;91(2):251–268. [PubMed] [Google Scholar]
- Tiffany ST. A cognitive model of drug urges and drug-use behavior: role of automatic and nonautomatic processes. Psychological Review. 1990;97(2):147–168. doi: 10.1037/0033-295x.97.2.147. [DOI] [PubMed] [Google Scholar]
- Tiffany ST, Warthen MW, Goedeker KC. The functional significance of craving in nicotine dependence. Paper presented at the 55th Annual Nebraska Symposium on Motivation: Motivational Impact of Nicotine and its Role in Tobacco Use; Lincoln, NE. 2007. Apr 12, [DOI] [PubMed] [Google Scholar]
- Tiffany ST, Wray JM. The clinical significance of drug craving. Annals of the New York Academy of Sciences. 2012;1248(1):1–17. doi: 10.1111/j.1749-6632.2011.06298.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. A Report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2014. The Health Consequences of Smoking: 50 Years of Progress. Printed with corrections January 2014. [Google Scholar]
- Vink JM, Willemsen G, Boomsma DI. Heritability of smoking initiation and nicotine dependence. Behavior genetics. 2005;35(4):397–406. doi: 10.1007/s10519-004-1327-8. [DOI] [PubMed] [Google Scholar]
- Wakefield M, Flay B, Nichter M, Giovino G. Effects of anti-smoking advertising on youth smoking: a review. Journal of Health Communication. 2003;8(3):229–247. doi: 10.1080/10810730305686. [DOI] [PubMed] [Google Scholar]
- Waters AJ, Carter BL, Robinson JD, Wetter DW, Lam CY, Cinciripini PM. Implicit attitudes to smoking are associated with craving and dependence. Drug and Alcohol Dependence. 2007;91(2):178–186. doi: 10.1016/j.drugalcdep.2007.05.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinstein ND. Accuracy of smokers’ risk perceptions. Annals of Behavioral Medicine. 1998;20(2):135–140. doi: 10.1007/BF02884459. [DOI] [PubMed] [Google Scholar]
- Wertz JM, Sayette MA. Effects of smoking opportunity on attentional bias in smokers. Psychology of Addictive Behaviors. 2001;15(3):268–271. [PMC free article] [PubMed] [Google Scholar]
- Wetter DW, Smith SS, Kenford SL, Jorenby D, Fiore EMC, Hurt RD, … Baker TB. Smoking Outcome Expectancies: Factor Structure, Predictive Validity, and Discriminant Validity. Journal of Abnormal Psychology. 1994;103(4):801–811. doi: 10.1037//0021-843x.103.4.801. [DOI] [PubMed] [Google Scholar]
- Wilson SJ, Sayette MA, Fiez JA. Prefrontal responses to drug cues: a neurocognitive analysis. Nature Neuroscience. 2004;7(3):211–214. doi: 10.1038/nn1200. [DOI] [PMC free article] [PubMed] [Google Scholar]