Abstract
Objectives
To investigate the pattern of referral for and utilisation of physiotherapy in the continuum of stroke care at a tertiary hospital in Ibadan, Nigeria.
Methods
Referral notes and medical records of patients admitted in the University College Hospital, Ibadan with a clinical diagnosis of stroke between January, 2009 and December, 2013 were retrospectively reviewed. Information on age, sex, type of stroke, length of hospital stay, referral for physiotherapy and utilisation of physiotherapy were retrieved. Data were summarised using descriptive statistics and analysed using Chi-square test.
Results
A total of 783 patients with stroke were admitted in the hospital during the period under study. The in-patient mortality rate was 37.2%. The mean Length of Hospital Stay (LoHS) was 16.17±12.34 days. Referral rate for physiotherapy was high (75.8%) and the mean time from admission to referral for physiotherapy was three days. Majority of patients referred utilised physiotherapy (63.4%) and mean number of physiotherapy sessions received during in-patient care was 8.69±6.45. There was a significant association between LoHS and utilisation of in-patientphysiotherapy (p=0.02).
Conclusion
The referral rate of stroke patients for physiotherapy was relatively high. Utilisation of in-patient physiotherapy reduced length of hospital stay among patients with stroke. Utilisation of out-patient physiotherapy was low. Strategies to enhance out-patient utilisation should be explored.
Keywords: Stroke, utilisation, physiotherapy
Introduction
Stroke is a major public health problem, and a leading cause of adult disability and Disability Adjusted Life Years (DALY) loss1,2 in low and middle income countries. Prevention and effective rehabilitation strategies are paramount to reducing the burden of stroke. Rehabilitation following a stroke begins during the acute phase of hospitalization as soon as the diagnosis of stroke is established and life-threatening problems are under control3,4. Early initiation of rehabilitation procedures can enhance return of neurological function, reduce stroke-related disability, improve long term outcome and quality of life among stroke patient5,6,7. Effective rehabilitation requires multidisciplinary team approach8.
Physiotherapy, a key component of stroke rehabilitation9 focuses on the recovery of physical function for stroke survivors10,11,12 and plays a positive role in enhancing independent living13. Immediate and intensive physiotherapy after a stroke has been associated with reduction in morbidity and mortality and improvement in performing activities of daily living14,15. Bernhardt et al16 identified physiotherapists as important drivers of mobility in the acute phase of stroke care. In fact, early mobilization and functional training provided by physiotherapists were considered the most important aspect of acute treatment in a Stroke Unit17. Therefore, timely access to physiotherapy is valuable to the persons concerned, their families and society as a whole15.
Physician referrals are required for stroke survivors to access physiotherapy services in Nigeria, a factor which increases the time from stroke onset to initiation of physiotherapy intervention. Although, the effectiveness of physiotherapy in stroke rehabilitation has been proven18 and physiotherapist's assessment of a stroke patient within the first 72 hours of admission is considered one of the indicators of effective stroke care8, evidence has suggested that physicians' use of physiotherapy services may be suboptimal19,20. Several factors have been postulated for this low level of utilisation of physiotherapy among physicians. These include poor communication between physiotherapists and physicians; doubt about the effectiveness and indications for physiotherapy treatment as well as low level of knowledge and awareness of the scope of physiotherapy among physicians21–24.
The importance and utilisation of physiotherapy in the continuum of stroke care have been studied in different countries25,26,27 Most of these studies were conducted in high income countries. It is inappropriate to generalise studies on utilisationof physiotherapy from a high income country to a low resourced country due to differences in therapeutic procedures and socio-economic strata. There is a dearth of studies evaluating the pattern of referral for physiotherapy after stroke in Nigeria and the proportion of stroke patients who actually utilised this service is unclear. Therefore, this study was conducted to investigate the pattern of referral and utilisation of physiotherapy in the continuum of stroke care in the foremost teaching hospital in Nigeria. Investigating the pattern of referral for physiotherapy services maybe the first step in identifying the extent to which physicians adhere to Clinical Practice Guidelines for the management of patients with stroke. Examining the level of utilisation may help determine if access to physiotherapy is equitable among stroke patients. This may guide healthcare policy makers on the need to adopt and implement best practices in the management of stroke patients for better treatment outcomes.
Methods
This retrospective study was conducted using data from the health records of stroke patients admitted in the University College Hospital (UCH), Ibadan, Nigeria. The hospital is the premier teaching hospital in Nigeria and government-designated centre of excellence in neurosciences. Ethical approval was obtained from the appropriate Institutional Health Research Ethics Committee. All cases of stroke admitted in the hospital between January 2009 and December 2013 were identified from the hospital's records. The records indicated the patients' outcome as either deceased or discharged home alive.
Case files of patients who survived their stroke event were subsequently retrieved and reviewed regardless of the cause of stroke. Case files of patients who died while on admission were excluded from the review for pattern of referral for and utilisation of physiotherapy. Other sources of data used for information retrieval were the physiotherapy referral cards and physiotherapy attendance register of the stroke survivors.
Referral cards are given to patients by the referring physicians and are kept as part of the patients' record in the physiotherapy department. Physiotherapy attendance registers are used for both in-patients and out-patients. The registers document the number of times the physiotherapists had contact with the patients. They are used alongside documentations on the physiotherapy treatment received by the patients in the patients' case files for quality control. Physiotherapy intervention for patients with stroke at the University College Hospital is targeted at improving muscle strength and extensibility in the affected extremities, relieving pain and spasticity where present, improving cardiovascular fitness and enhancing functional independence. This is achieved through the use of specific therapeutic exercises ranging from passive to assisted active to free active and resisted active exercises; static and dynamic balance retraining exercises; task specific functional exercises and gait retraining. Information on the socio-demographic and clinical characteristics of the patients, date of onset of stroke, length of hospital stay, referral for physiotherapy, date of referral for physiotherapy, date physiotherapy commenced, number of physiotherapy sessions during in-patient care and the date out-patient physiotherapy commenced were extracted from the data sources into a data sheet. Each patient's identification number in the patients' record was encrypted for privacy and protection.
Data analysis
Descriptive statistics of mean, percentages and proportion were used to summarize the socio-demographic and clinical characteristics of stroke survivors managed at the UCH between January 2009 and December 2013. Referral for physiotherapy was based on a documented plan to refer for physiotherapy in patient's case file and its corresponding physiotherapy referral card. It was recorded as a ‘Yes’ or ‘No’. Utilisation was based on documented evidence of a physiotherapy assessment after referral. Number of physiotherapy session was the number of documented contacts between the physiotherapist and the patients. Chi square test was used to examine the relationship among socio-demographic and clinical characteristics of patients, length of hospital stay and each of pattern of referral for and utilisation of physiotherapy. Level of significance was set at 0.05.
Results
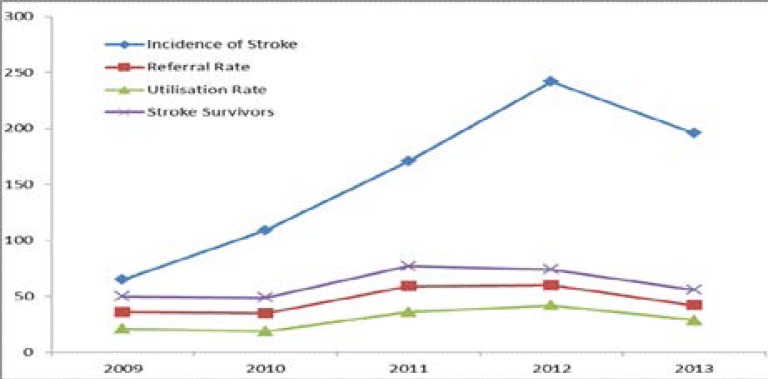
A total of 783 patients with stroke made up of 397 (50.7%) males and 386 (49.3%) females, were admitted in the University College Hospital (UCH), Ibadan between January, 2009 and December, 2013. There was a steady increase in stroke incidence from 8.3% in 2009 to 30.9% in 2012. There was a 5.9% decrease in the rate of admission between 2012 and 2013 (Figure 1).
Figure 1.
Trends in stroke incidence, survival rate, referral rate for physiotherapy and utilization of physiotherapy
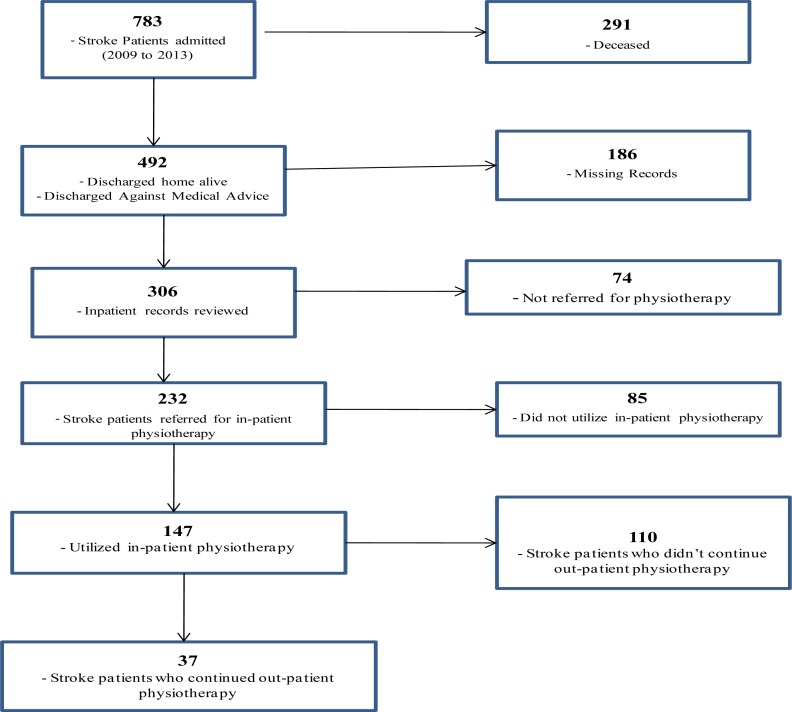
Less than two-thirds (62.8%) of the stroke patients admitted in the hospital survived the stroke event giving an in-patient mortality rate of 37.2% for the period studied. Survival was slightly higher among female patients (50.4%). Out of the 492 (62.8%) identified stroke survivors, the case files of only 306 (62.2%) patients could be retrieved for review. The identified records were reviewed and categorized on the basis of referral for physiotherapy and utilisation of physiotherapy during and after in-patient care (Figure 2).
Figure 2.
Flowchart of Patients' Medical Records Reviewed
Data was extracted from the medical records (case files and physiotherapy attendance registers) of 306 stroke survivors. The mean age of the stroke survivors was 59.9±13.0 years (median = 60.0years). 129 (42.2%) of them were aged 65 years and above (Table 1). Majority of the patients (55.9%) had no documentation on the type of stroke. The ratio of ischaemic to haemorrhagic stroke was approximately 5:3 in those for which it was documented. The risk factors for stroke in majority of the patients were hypertension (67.4%), followed by hypertension coexisting with diabetes (23.0%).
Table 1.
Socio-demographic and clinical characteristics of stroke survivors (N = 306)
| Frequency | Percentage | |
| N | % | |
| Sex | ||
| Male | 151 | 49.3 |
| Female | 155 | 50.7 |
| Occupation | ||
| Artisan | 20 | 6.5 |
| Employed | 65 | 21.2 |
| Retired | 44 | 14.4 |
| Self-employed | 157 | 51.3 |
| Unemployed | 20 | 6.5 |
| Age Group | ||
| Young Adult (≤ 45 years) | 43 | 14.0 |
| Middle Age (46 – 64years) | 134 | 43.8 |
| Elderly (≥ 65 years) | 129 | 42.2 |
| Mean Age (years) | 59.93±13.05 | |
| Type of stroke | ||
| Haemorrhagic | 48 | 15.7 |
| Ischaemic | 87 | 28.4 |
| Not Documented | 171 | 55.9 |
The mean length of hospital stay for the stroke survivors was 16.2±12.3 days (median = 13days). 232 patients out of a total of 306 patients were referred for physiotherapy while on admission amounting to an in-patient referral rate of 75.8% over the five year period (Table 2).
Table 2.
Length of hospital stay, pattern of referral and utilisation of physiotherapy
| Frequency | Percentage (%) | |
| Length of hospital stay in days (n = 306) | ||
| 1 – 20 | 231 | 75.5 |
| 21 – 40 | 60 | 19.6 |
| 41 – 60 | 13 | 4.2 |
| ≥ 61 | 2 | 0.7 |
| Mean LOS (days) | 16.2 ±12.3 | |
| Referral for In-patient Physiotherapy (n = 306) | ||
| Yes | 232 | 75.8 |
| No | 74 | 24.2 |
| Utilisation of In-patient Physiotherapy (n = 232) | ||
| Yes | 147 | 63.4 |
| No | 85 | 36.6 |
| Mean physiotherapy session | 8.7±6.5 | |
| Utilisation of Out-patient Physiotherapy (n = 147) | ||
| Yes | 37 | 25.2 |
| No | 110 | 74.8 |
The referral rate was highest (81.1%) in year 2012 and lowest (71.4%) in 2010. Only about a third (35.3%) of the patients were referred for and assessed by physiotherapists within 24 hours of admission while 9.1% of patients were referred about a week or more post-admission. The mean length of time from admission to first physiotherapy assessment was 3.0±3.2 days (median = 2.0 days). Almost two-thirds (63.4%) of the patients referred for physiotherapy utilised physiotherapy services while on admission. The mean in-patient physiotherapy session received by the patients was 8.7±6.5 (median = 7). Utilisation rate was highest (28.6%) in 2012 and lowest (12.9%) in 2010. The rate of utilisation of in-patient physiotherapy was highest (67.6%) among elderly patients and lowest (53.3%) among those less than 46 years. 67.0% of the female patients utilisedphysiotherapy while on admission while 59.8% of the male patients utilised it. Utilisation of physiotherapy did not vary with the type of stroke. Only a quarter (25.2%) of the patients who utilised in-patient physiotherapy received out-patient physiotherapy in the hospital. The mean out-patient physiotherapy session was 8.9±9.4 (median 6).
There was no significant association (p > 0.05) between length of hospital stay and each of patients' age and sex. However, there was an observed age-related increase in length of hospital stay. More than a quarter (28.0%) of the patients above 65 years of age stayed in the hospital beyond three weeks while less than a fifth (18.6%) of those below 45 years of age stayed in the hospital for the same duration. There was no significant association (>0.05) between utilisation of in-patient physiotherapy and each of age, sex and stroke type (Table 3).
Table 3.
Association among patients' profile and utilisation of physiotherapy (n = 147)
| Characteristics | YES n |
(%) | NO n |
(%) | χ2 | p-value |
| Sex | ||||||
| Male | 70 | (59.8) | 47 | (40.2) | 1.27 | 0.28 |
| Female | 77 | (67.0) | 38 | (33.0) | ||
| Age | ||||||
| ≤ 45 years | 16 | (53.3) | 14 | (46.7) | 2.19 | 0.34 |
| 46 – 64 years | 62 | (62.0) | 38 | (38.0) | ||
| ≥ 65 years | 69 | (67.6) | 33 | (32.4) | ||
| Type of stroke | ||||||
| Ischaemic | 44 | (63.8) | 25 | (36.2) | 0.02 | 0.99 |
| Haemorrhagic | 23 | (63.9) | 13 | (36.1) | ||
| Missing values | 80 | (63.0) | 47 | (37.0) |
However, a significant association was observed between length of hospital stay and utilisation of physiotherapy (p = 0.02). The length of hospital stay was shortest among patients who utilised physiotherapy most (63.9%) while it was longest (>6 weeks) in patients with the lowest rate of utilisation.
Discussion
This study examined the proportion of stroke patients admitted in a tertiary hospital referred for physiotherapy and the proportion that utilised physiotherapy. The results showed an increasing incidence of stroke during the study period. Evidence has shown an increasing incidence and prevalence of stroke in Nigeria28,29. The slight dip observed in 2013 may be due to the incessant industrial action in the health sector in the country that year. Though stroke incidence in the study population cut across the 3rd to 8th decade of life, the median age of the patients reviewed was 60 years. This is in congruence with previous findings that age remains a non-modifiable and most important singular risk factor for stroke. This risk increases with each successive decade above age 55 years30,31.
Our findings suggest that the incidence of stroke is slightly higher in males than females based on the proportion of male patients admitted on account of stroke compared to females which is consistent with findings from previous studies32,33,34. However, survival was higher among females than males resulting in a tilt in favour of-females at discharge. The severity of stroke for male and female participants in this study could not be ascertained. It is probable that males suffered worse stroke than females. Furthermore, there could be variation in premorbid status and prevalence of comorbidities between male and female stroke patients in this study. It has been postulated that co-morbidities can compromise recovery from a stroke35. Therefore, inferences on sex differences in survival rate among the stroke patients in this study must be drawn with caution.
About three-quarters of the stroke survivors were referred for physiotherapy. This is a rather high proportion of stroke patients admitted in the hospital. Physiotherapy is not provided routinely for patients in Nigeria because of the need for physician referral. The high referral rate found in this study suggests that physicians are aware of the importance of physiotherapy in improving functional independence post-stroke. It could also be a reflection of the level of adherence of physicians in this hospital to recommended clinical practice guidelines that stroke patients be referred for physiotherapy as soon as life-threatening problems are under control. Evidence indicates that patients do better with a well-organized, multidisciplinary approach to post-acute rehabilitation after a stroke36. This multi-disciplinary approach to stroke rehabilitation includes physiotherapy. There is a wide variation in the time between patients' admission to the hospital and initiation of physiotherapy. Most clinical practice guidelines suggest 24 hours post stroke onset. It should be noted that life-threatening problems vary in severity among patients and practice settings. This may contribute to the delay in referral of stroke patients in this hospital.
Only about two-thirds of the patients referred for physiotherapy actually received physiotherapy. This is comparable to findings in literature about utilisation of physiotherapy26,37. McKevitt et al26 and Leemrijse et al37 reported utilisation rates of 70.7% and 69.0% respectively for physiotherapy. However, Lee et al27 in a similar study reported a utilisation rate of 33% for physiotherapy in acute stroke. This is rather low compared to the findings of this study. The findings of Lee and colleagues27 may be related to the reported dearth of physiotherapists and consequent rationing of rehabilitation services in Taiwan. Although the physiotherapist to population ratio in Nigeria is worse at 1:42,000, the utilisation rate was higher and comparable with utilisation in countries with high physiotherapists to patient ratio. This suggests that non-availability or dearth of physiotherapists all by itself has minimal effect on utilisation of physiotherapy.
In comparison to the referral rate, the number of treatment recipients is somewhat low. Physiotherapy intervention after stroke is often long-term and considered expensive in Nigeria. This may account for the underutilisation. When patients are initially admitted into hospital they enjoy a lot of social and financial support. This support system dwindles as the illness becomes protracted and patients oftentimes are out of funds by the time they are referred for physiotherapy and might therefore not be able to afford the service. Moreover, most patients had no health insurance coverage and were expected to pay for their treatment out of pocket. In addition, inadequate information on the importance of physiotherapy in motor recovery post stroke among the patients may affect their choices. Many would rather spend money on drugs and investigations than pay for physiotherapy services. Utilisation was higher among elderly stroke survivors. Research has demonstrated an association between increasing age and provision of physiotherapy after stroke26. This could be because the elderly tend to have worse stroke in view of possible age-related co-morbidity. It may also be that they tend to be referred more by physicians in order to avoid the complications of stroke which are likely to be higher and worse in this age group.
Length of hospital stay was shortest in patients with higher rate of utilisation. This suggests that stroke patients who received in-patient physiotherapy early recovered faster and got discharged earlier than those who did not. This is consistent with the results of an earlier study by Freburger38 on utilisation of physiotherapy and outcomes of care for patients with stroke. This is likely due to the proven benefit of physiotherapy in improving/maximising function after a stroke. Early initiation of rehabilitation procedures can enable greater return of neurological function and improve long term outcome and quality of life in stroke patients5,6,7. Many of the immediate complications of stroke such as deep vein thrombosis, skin breakdown, contracture formation, constipation, and hypostatic pneumonia are related to immobility and are preventable with early mobilisation6.
Out-patient utilisation of physiotherapy was rather low compared to inpatient utilisation among the stroke patients. This is probably because the University College Hospital is a referral centre and patients come from different parts of the country to this foremost healthcare facility. It is likely that most of the patients had out-patient physiotherapy in other hospitals within their community. Underuse may also be a reflection of poor adherence to outpatient appointment schedule among the patients. It could also be that patients went for unorthodox treatment from traditional healers who are purported to have supernatural healing powers that can cure stroke. Future studies should explore reasons for this decrease in utilisation, and identify factors that may improve outpatient physiotherapy utilisation among stroke survivors in Ibadan, Nigeria.
There was no difference in physiotherapy utilisation based on age, sex and type of stroke. This is comparable to the report of Lee et al27 that utilisation of inpatient rehabilitation for acute stroke was similar irrespective of patients' age, sex and year of onset. Redondo-Sendino et al39 however, reported a higher healthcare utilisation among Spanish women compared to men. The fact that demographics were not related to utilisation may be an indication that physiotherapy utilisation for stroke patient in Ibadan, Nigeria is equitable though underused.
Documentation inaccuracies and difficulty in verifying records may affect the pattern of referral and utilisation reported in this study. Records of patients who died during hospital admission were not reviewed. If these records were reviewed, the pattern of referral for and utilisation of physiotherapy among the patients could be different. Comparison between severity of stroke and referral for and utilisation of physiotherapy could not be made because stroke severity was not documented consistently in an objective manner in these patients.
Conclusion
Referral rates of patient with stroke for physiotherapy are satisfactory. However, the rate of utilisation of physiotherapy among patients with stroke appears inadequate. Utilisation of physiotherapy during hospital admission is associated with reduced length of hospital stay among patients with stroke. Therefore, utilisation of physiotherapy among stroke patients should be encouraged for reduced length of hospital stay and improved functional outcome. Utilisation of out-patient physiotherapy was low. Strategies to enhance out-patient utilisation should be explored.
References
- 1.Ogun SA, Ojini FI, Ogungbo B, Kolapo KO, Danesi MA. Stroke in South-West Nigeria, A 10-year review. Stroke. 2005;36:1120–1122. doi: 10.1161/01.STR.0000166182.50840.31. [DOI] [PubMed] [Google Scholar]
- 2.Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJ. Global and regional burden of diseases and risk factors 2001: systematic analysis of population health data. Lancet. 2006;367:1747–1757. doi: 10.1016/S0140-6736(06)68770-9. [DOI] [PubMed] [Google Scholar]
- 3.Agency for Health Care Policy and Research, author. Priorities for future research- Clinical Practice Guidelines for stroke rehabilitation Number 16. Rockwell, Maryland: US Department of Health and Human Services; 1995. AHCPR publication no. 95-0662. [Google Scholar]
- 4.Bernhardt J, Thuy MN, Collier JM, Legg LA. Very early versus delayed mobilisation after stroke. Cochrane Database of Systematic Reviews. 2009;1:CD006187. doi: 10.1002/14651858.CD006187.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lindsay P, Bayley M, McDonald A, et al. Toward a more effective approach to stroke: Canadian best practice recommendations for stroke care. Canadian Medical Association Journal. 2008;178:1418–1425. doi: 10.1503/cmaj.071253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Quinn TJ, Paolucci S, Sunnerhagen KS, et al. An expanded guidance document from the European Stroke Organization (ESO) Guidelines for management of ischaemic stroke and transient ischaemic attack. Journal of Rehabilitation Medicine. 2009;41:99–111. doi: 10.2340/16501977-0301. [DOI] [PubMed] [Google Scholar]
- 7.Clarke DJ, Forster A. Improving post-stroke recovery: the role of multidisciplinary health care team care. Journal of Multidisciplinary Healthcare. 2015;8:433–442. doi: 10.2147/JMDH.S68764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Intercollegiate Stroke Working Party, author. National Clinical Guidelines for Stroke. 4th Edition. London: Royal College of Physicians; 2012. Prepared by the Intercollegiate Stroke Working Party. [Google Scholar]
- 9.Kwakkel G, Kollen B, Lindeman E. Understanding the pattern of functional recovery after stroke, facts and theories. Restorative Neurology and Neuroscience. 2004;22:281–299. [PubMed] [Google Scholar]
- 10.Salter K, Jutai J, Hartley M, Foley N, Bhogal S, Bayona N, Teasell R. Impact of early versus delayed admission to rehabilitation on functional outcomes in persons with stroke. Journal of Rehabilitation Medicine. 2006;38:113–117. doi: 10.1080/16501970500314350. [DOI] [PubMed] [Google Scholar]
- 11.Aprile D, Di Stasio E, Romitelli F, et al. Effects of rehabilitation on quality of life in patients with chronic stroke. Brain Injury. 2008;22:451–456. doi: 10.1080/02699050802060639. [DOI] [PubMed] [Google Scholar]
- 12.Khan FR, Vijesh PV, Rahool S, et al. Physiotherapy practice in stroke rehabilitation: A cross-sectional survey of Physiotherapists in the state of Kerala, India. Topics in Stroke Rehabilitation. 2012;19:405–410. doi: 10.1310/tsr1905-405. [DOI] [PubMed] [Google Scholar]
- 13.Mahler MP, Zuger K, Kaspar K, et al. A cost analysis of the first year after stroke - early triage and inpatient rehabilitation may reduce long term costs. Swiss Medical Weekly. 2008;138:459–465. doi: 10.4414/smw.2008.11845. [DOI] [PubMed] [Google Scholar]
- 14.Langhorne P, Bernhardt J, Kwakkel G. Stroke Rehabilitation. Lancet. 2011;377:1693–1702. doi: 10.1016/S0140-6736(11)60325-5. [DOI] [PubMed] [Google Scholar]
- 15.Fielder S, Mpezeni S, Benjamin L, Cary I. Physiotherapy in Malawi; A Step in the right direction. Malawi Medical Journal. 2013;25:83–85. [PMC free article] [PubMed] [Google Scholar]
- 16.Bernhardt J, Dewey H, Thrift A, Donnan G. Inactive and alone: physical activity within the first 14 days of acute stroke unit care. Stroke. 2004;35:1005–1009. doi: 10.1161/01.STR.0000120727.40792.40. [DOI] [PubMed] [Google Scholar]
- 17.Indredavik B, Bakke F, Slǿrdahl SA, Rokseth R, Haheim LL. Treatment in a combined acute and rehabilitation stroke unit: which aspects are most importan? Stroke. 1999;30:917–923. doi: 10.1161/01.str.30.5.917. [DOI] [PubMed] [Google Scholar]
- 18.Pollock A, Baer G, Pomeroy V. Physiotherapy treatment approaches for the recovery of postural control and lower limb function following stroke. Cochrane Database Systemic Review. 2007;1:CD001920. doi: 10.1002/14651858.CD001920.pub2. [DOI] [PubMed] [Google Scholar]
- 19.Mielenz TJ, Carey TS, Dyrek DA, et al. Physical therapy utilization by patients with acute low back pain. Physical Therapy. 1997;77:1040–1051. doi: 10.1093/ptj/77.10.1040. [DOI] [PubMed] [Google Scholar]
- 20.Overman SS, Kent DL, Uslan DW, Lewis RS. Cost of care and patient-satisfaction from routine referral to nonsurgical musculoskeletal specialists in a Medicare risk plan. Journal of Clinical Rheumatology. 1998;4:120–128. doi: 10.1097/00124743-199806000-00006. [DOI] [PubMed] [Google Scholar]
- 21.Hendriks HJ, Oostendorp RA, Bernards AT, et al. The diagnostic process and indication for physiotherapy: a prerequisite for treatment and outcome evaluation. Physical Therapy Reviews. 2000;5:29–47. [Google Scholar]
- 22.Hendriks HJM, Kerssens YE, Elvers JWH, et al. Referral patterns and utilization of physiotherapy services following a one-time physiotherapist consultation in general practice. Physiotherapy Theory and Practice. 2003;19:5–21. [Google Scholar]
- 23.Quartey JN, Agbelie C, Owusu-Ansah B, Bello AI, Appiah-kubi KO. Content analysis of physicians' referrals to physiotherapy at Korle Bu Teaching Hospital Accra, Ghana. Ghana Journal of Physiotherapy. 2009;1:10–12. [Google Scholar]
- 24.Odunaiya NA, Ilesanmi T, Adeniran FO, Oguntibeju OO. Attitude and practices of obstetricians and gynecologists towards involvement of physiotherapists in management of obstetric and gynecologic conditions. International Journal of Women's Health. 2013;5:109–114. doi: 10.2147/IJWH.S34350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tyson S, Turner G. Discharge and follow-up for people with stroke: What happens and why? Clinical Rehabilitation. 2000;14:381–392. doi: 10.1191/0269215500cr331oa. [DOI] [PubMed] [Google Scholar]
- 26.McKevitt C, Coshall C, Tilling K, Wolfe C. Are there inequalities in the provision of stroke care? Analysis of an inner-city stroke register. Stroke. 2005;36:315–320. doi: 10.1161/01.STR.0000152332.32267.19. [DOI] [PubMed] [Google Scholar]
- 27.Lee HC, Chang KC, Huang YC, et al. Inpatient rehabilitation utilization for acute stroke under a universal health insurance system. American Journal of Managed Care. 2010;16:e67–e74. [PubMed] [Google Scholar]
- 28.Wahab KW. The burden of stroke in Nigeria. International Journal of Stroke. 2008;3(4):290–292. doi: 10.1111/j.1747-4949.2008.00217.x. [DOI] [PubMed] [Google Scholar]
- 29.Talabi OA. A 3-year review of neurologic admissions in University College Hospital, Ibadan, Nigeria. West African Journal of Medicine. 2003;22(2):150–151. doi: 10.4314/wajm.v22i2.27937. [DOI] [PubMed] [Google Scholar]
- 30.Miah MNA, Azhar MA, Rahman A, et al. Risk Factors of Stroke in young and old age groups - A Comparative Study. Journal of Medicine. 2012;13:138–142. [Google Scholar]
- 31.Russo T, Felzani G, Marini C. Stroke in the very old: a systematic review of studies on incidence, outcome and resource use. Journal of Ageing Research. 2011 doi: 10.4061/2011/108785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kolapo KO, Ogun SA, Danesi MA, Osalusi BS, Odusote KA. Validation study of the Siriraj stroke score in African Nigerians and evaluation of the discriminating values of its parameters: a preliminary prospective CT scan study. Stroke. 2006;37:1997–2000. doi: 10.1161/01.STR.0000229893.02732.02. [DOI] [PubMed] [Google Scholar]
- 33.Karaye KM, Nashabaru I, Fika GM, et al. Prevalence of traditional cardiovascular risk factors among Nigerians with stroke. Cardiovascular Journal of Africa. 2007;18:290–294. [PMC free article] [PubMed] [Google Scholar]
- 34.Schulz UGR, Rothwell PM. Differences in vascular riskfactors between aetiological subtypes of ischemic stroke: importance of population-based studies. Stroke. 2003;34:2050–2059. doi: 10.1161/01.STR.0000079818.08343.8C. [DOI] [PubMed] [Google Scholar]
- 35.Lim JH, Cheon SH. Analysis of variation in length of stay (LOS) after ischemic and hemorrhagic stroke using the Charlson Comorbidity Index (CCI) Journal of Physical Therapy Science. 2015;27:799–803. doi: 10.1589/jpts.27.799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Duncan PW, Zorowitz R, Bates B. Management of adult stroke rehabilitation care: A clinical practice guideline. Stroke. 2005;36:e100–e143. doi: 10.1161/01.STR.0000180861.54180.FF. [DOI] [PubMed] [Google Scholar]
- 37.Leemrijse CJ, de Boer ME, van den Ende CHM, van den Ende CHM, Ribbe MW, Dekker J. Factors associated with physiotherapy provision in a population of elderly nursing home residents; a cross sectional study. BMC Geriatrics. 2007;7:7. doi: 10.1186/1471-2318-7-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Freburger JK. An analysis of the relationship between the utilization of physical therapy services and outcomes of care for patients with acute stroke. Physical Therapy. 1999;79:906–918. [PubMed] [Google Scholar]
- 39.Redondo-Sendino A, Guallar-Castillón P, Banegas JR, Rodríguez-Artalejo F. Gender differences in the utilization of health-care services among the older adult population of Spain. BMC Public Health. 2006;6:155. doi: 10.1186/1471-2458-6-155. [DOI] [PMC free article] [PubMed] [Google Scholar]