Abstract
Resistant or difficult to treat hypertension is defined as high blood pressure that remains uncontrolled with 3 or more different antihypertensive medications, including a diuretic. Recent definitions also include controlled blood pressure with use of 4 or more medications as also being resistant to treatment. Recently, refractory hypertension, an extreme phenotype of antihypertensive treatment failure has been defined as hypertension uncontrolled with use of 5 or more antihypertensive agents, including a long-acting thiazide diuretic and a mineralocorticoid receptor antagonist. Patients with resistant vs refractory hypertension share similar characteristics and comorbidities, including obesity, African American race, female sex, diabetes, coronary heart disease, chronic kidney disease, and obstructive sleep apnea. Patients with refractory vs resistant hypertension tend to be younger and are more likely to have been diagnosed with congestive heart failure. Refractory hypertension might also differ from resistant hypertension in terms of underlying cause. Preliminary evidence suggests that refractory hypertension is more likely to be neurogenic in etiology (ie, heightened sympathetic tone), vs a volume-dependent hypertension that is more characteristic of resistant hypertension in general.
The terms, “resistant” and “refractory” hypertension have historically been used interchangeably to refer to patients with difficult to treat hypertension, that is, hypertension resistant to pharmacologic intervention.1,2 Most commonly, resistant or refractory hypertension has been defined as high blood pressure with 3 or more medications needed to control, including a diuretic.3 Recently, however, the term, refractory hypertension has been applied to an extreme phenotype of antihypertensive treatment failure.4 In this context, the definition of refractory hypertension has been evolving, but has been largely based on failure to achieve blood pressure goal with use of 5 or more antihypertensive medications, including a long-acting thiazide diuretic. Recent considerations by investigators who evaluated this subgroup of patients have suggested defining the phenotype as hypertension uncontrolled (>140/90 mm Hg) with use of 5 or more different classes of antihypertensive agents, including a long-acting thiazide diuretic and a mineralocorticoid receptor antagonist.4,5
In this viewpoint we discuss the emerging data on this novel phenotype of antihypertensive treatment failure and how it compares and contrasts with resistant hypertension in terms of definition, prevalence, patient characteristics, risk factors, comorbidities, and possible underlying etiologies.
Definition
Resistant hypertension
Resistant hypertension is defined as high blood pressure that remains uncontrolled (>140/90 mm Hg) despite the use of effective doses of 3 or more different classes of antihypertensive agents, including a diuretic. The first American Heart Association Scientific Statement on resistant hypertension included patients whose blood pressure was controlled (<140/90 mm Hg) with 4 or more medications within the category of resistant hypertension.3
Refractory hypertension
The term, refractory hypertension has been recently used to refer to an extreme phenotype of antihypertensive treatment failure. The first application of the term in this context was in a retrospective analysis of the phenotype from investigators at the University of Alabama at Birmingham.4 In that report, refractory hypertension was defined uncontrolled blood pressure with use of 5 or more different antihypertensive classes, including a diuretic.
Based on the literature that showed superiority of chlorthalidone over hydrocholorothiazide (HCTZ) and specific benefit of spironolactone6–9 for treatment of resistant hypertension, 5 drug combinations that include these 2 agents, likely represent maximal antihypertensive treatment. Accordingly, the working definition of refractory hypertension has evolved to be increased blood pressure levels (>140/90 mm Hg) despite the use of optimal doses of 5 or more different classes of antihypertensive agents, including chlorthalidone and a mineralocorticoid receptor antagonist (Fig. 1).
Figure 1.
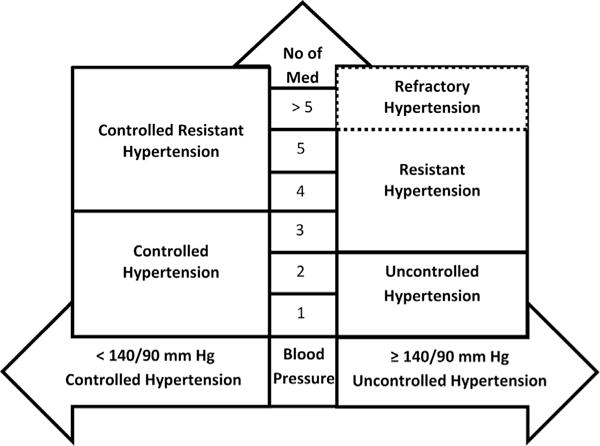
Hypertension classification based on blood pressure control and number of antihypertensive medications (No of Med).
Prevalence
Resistant hypertension
A number of observational studies have characterized patients with resistant hypertension from a variety of different cohorts. Multiple studies indicate that the prevalence of resistant hypertension is approximately 10%–15% of treated hypertensive patients. For example, in a cross-sectional analysis of > 470,000 individuals, 60,327 had resistant hypertension.10 This represented 12.8% of all hypertensive individuals and 15.3% of those taking antihypertensive medications.
Refractory hypertension
Two studies have been published on refractory hypertension based on a definition that distinguishes it from resistant hypertension. The first was a retrospective analysis of patients referred to the University of Alabama at Birmingham for evaluation and treatment of resistant hypertension.4 Of the 304 patients referred for resistant hypertension and who had adequate follow-up (a minimum of 3 clinic visits), 29 (10%) never achieved blood pressure control despite maximal antihypertensive therapy of 6 different classes of antihypertensive agents, including chlorthalidone and spironolactone.
The second published study of refractory hypertension was a cross-sectional evaluation of participants in the Reasons for Geographic and Racial Differences in Stroke (REGARDS) study, a large (n = 30,239), community-based cohort study.5 In this analysis, refractory hypertension was defined as uncontrolled clinic blood pressure (>140/90 mm Hg) despite use of 5 or more different antihypertensive classes of agents. The prevalence of refractory hypertension was 3.6% of patients with resistant hypertension (uncontrolled blood pressure with 3 or more medications or controlled blood pressure with 4 or more) and 0.5% of all hypertensive participants included in the cohort.
Patient Characteristics and Associated Comorbidities
Resistant hypertension
Compared with individuals with nonresistant hypertension, that is, controlled blood pressure (<140/90 mm Hg) with 1 or 2 medications, individuals with resistant hypertension were older, obese, and more likely African American and female,11 and also had a greater prevalence of comorbid conditions, including diabetes, ischemic heart disease, cerebrovascular disease, and chronic kidney disease (CKD).
Refractory hypertension
In the retrospective analysis by Acelajado et al., of patients referred to a hypertension specialty clinic, 29 subjects identified as having refractory hypertension were compared with 275 subjects with controlled resistant hypertension.4 Subjects with refractory hypertension tended to be younger and heavier compared with subjects with controlled resistant hypertension. In addition, the refractory subjects tended to be more often African American and female. With regard to comorbidities, refractory hypertensive subjects were more likely to have a history of congestive heart failure, stroke, and obstructive sleep apnea. CKD and diabetes association was not statistically significant between the 2 groups.
In the cross-sectional assessment of the REGARDS cohort, of the 14,809 participants being treated for hypertension, 78 were identified as having refractory hypertension based on an uncontrolled blood pressure (>140/90 mm Hg) while receiving 5 or more antihypertensive medications, which included in all cases, HCTZ.5 These 78 refractory subjects were compared with all participants with treated hypertension and all participants with resistant hypertension. In an unadjusted and adjusted comparison with all hypertensive participants, African American race, male sex, and higher body mass index were associated with an increased prevalence ratio of having refractory hypertension. In the adjusted comparison, African American race was the strongest predictor of having refractory hypertension, with a prevalence ratio of 4.88 (95% confidence interval, 2.79–8.72). Compared with resistant hypertension, African American race only was associated with a higher prevalence ratio, before and after multivariate adjustment. Increased age was not associated with higher risk of refractory hypertension, with the mean age of the participants with refractory hypertension tending be less than that of participants with resistant hypertension.
Comorbidities associated with refractory hypertension compared with all hypertensive participants in the REGARDS cohort included reduced estimated glomerular filtration rate, albuminuria, diabetes, history of stroke, and known coronary heart disease after multivariate adjustment.5 Of these comorbidities, the strongest predictor was albuminuria, with an adjusted prevalence ratio of 4.02 (95% confidence interval, 2.53–6.41). Compared only with the participants with resistant hypertension, the comorbidities associated with refractory hypertension were albuminuria and diabetes.
Possible Mechanisms of Resistant vs Refractory Hypertension
A large body of literature implicates persistent intravascular fluid retention as a common underlying cause of resistant hypertension, including studies that documented intravascular expansion estimated according to thoracic fluid content.12 Causes of excess fluid retention are no doubt multifactorial but include CKD, hyperaldosteronism,12,13 heightened sodium sensitivity, and high dietary sodium intake.14
In contrast to resistant hypertension, refractory hypertension might represent a different phenotype in terms of etiology in not being volume-dependent. The analysis by Acelajado et al. showed consistently higher resting heart rates in the individuals with refractory hypertension compared with individuals with controlled resistant hypertension, suggesting a more likely neurogenic etiology of antihypertensive failure.4 In contrast, failure of intensive diuretic therapy with chlorthalidone and spironolactone to control blood pressure in the refractory patients argued against a volume-dependent cause of treatment failure.4
Conclusions
Refractory hypertension has been proposed as an extreme phenotype of antihypertensive treatment failure. The definition of refractory hypertension, although evolving, has most recently been suggested as failure to control blood pressure despite maximal antihypertensive effort based on use of at least 5 different classes of antihypertensive agents, including if tolerated, chlorthalidone and spironolactone.
Refractory hypertension is uncommon, with an estimated prevalence of 10% of patients referred to a hypertension specialty clinic for resistant hypertension and < 1% of treated hypertensive participants in a community-based cohort.4,5 Like resistant hypertension, obesity, diabetes, CKD, and especially African American race are associated with having refractory hypertension compared with patients with more easily controlled hypertension. Patients with refractory hypertension are at increased risk of having already had a cardiovascular complication, such as stroke and congestive heart failure, compared with patients with resistant but controlled hypertension.
The mechanisms of refractory hypertension lack full elucidation, but preliminary assessments, based mostly on failure to control blood pressure with intensive diuretic treatment and consistently higher heart rates, suggest that refractory hypertension might be more neurogenic in etiology (ie, heightened sympathetic output), as opposed to being volume-dependent. Additional studies of sympathetic tone, including assessments of peripheral resistance, heart rate variability, norepinephrine levels, and peripheral nerve traffic should provide further insight into this possibility.
Footnotes
Disclosures
The authors have no conflicts of interest to disclose.
References
- 1.Setaro JF, Black HR. Refractory hypertension. N Engl J Med. 1992;327:543–7. doi: 10.1056/NEJM199208203270808. [DOI] [PubMed] [Google Scholar]
- 2.Redon J, Campos C, Narciso ML, et al. Prognostic value of ambulatory blood pressure monitoring in refractory hypertension: a prospective study. Hypertension. 1998;31:712–8. doi: 10.1161/01.hyp.31.2.712. [DOI] [PubMed] [Google Scholar]
- 3.Calhoun DA, Jones D, Textor S, et al. Resistant hypertension: diagnosis, evaluation, and treatment. A scientific statement from the American Heart Association Professional Education Committee of the Council for High Blood Pressure Research. Hypertension. 2008;51:1403–19. doi: 10.1161/HYPERTENSIONAHA.108.189141. [DOI] [PubMed] [Google Scholar]
- 4.Acelajado MC, Pisoni R, Dudenbostel T, et al. Refractory hypertension: definition, prevalence, and patient characteristics. J Clin Hypertens. 2012;14:7–12. doi: 10.1111/j.1751-7176.2011.00556.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Calhoun DA, Booth JN, 3rd, Oparil S, et al. Refractory hypertension: determination of prevalence, risk factors, and comorbidities in a large, population-based cohort. Hypertension. 2014;63:451–8. doi: 10.1161/HYPERTENSIONAHA.113.02026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nishizaka MK, Zaman MA, Calhoun DA. Efficacy of low-dose spironolactone in subjects with resistant hypertension. Am J Hypertens. 2003;16:925–30. doi: 10.1016/s0895-7061(03)01032-x. [DOI] [PubMed] [Google Scholar]
- 7.Chapman N, Dobson J, Wilson S, et al. Effect of spironolactone on blood pressure in subjects with resistant hypertension. Hypertension. 2007;49:839–45. doi: 10.1161/01.HYP.0000259805.18468.8c. [DOI] [PubMed] [Google Scholar]
- 8.Ernst ME, Carter BL, Goerdt CJ, et al. Comparative antihypertensive effects of hydrochlorothiazide and chlorthalidone on ambulatory and office blood pressure. Hypertension. 2006;47:352–8. doi: 10.1161/01.HYP.0000203309.07140.d3. [DOI] [PubMed] [Google Scholar]
- 9.Khosla N, Chua DY, Elliott WJ, Bakris GL. Are chlorthalidone and hydrochlorothiazide equivalent blood-pressure-lowering medications? J Clin Hypertens. 2005;7:354–6. doi: 10.1111/j.1524-6175.2005.04451.x. [DOI] [PubMed] [Google Scholar]
- 10.Sim JJ, Bhandari SK, Shi J, et al. Characteristics of resistant hypertension in a large, ethnically diverse hypertension population of an integrated health system. Mayo Clin Proc. 2013;88:1099–107. doi: 10.1016/j.mayocp.2013.06.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cushman WC, Ford CE, Cutler JA, et al. Success and predictors of blood pressure control in diverse North American settings: the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT) J Clin Hypertens. 2002;4:393–404. doi: 10.1111/j.1524-6175.2002.02045.x. [DOI] [PubMed] [Google Scholar]
- 12.Gaddam KK, Nishizaka MK, Pratt-Ubunama MN, et al. Characterization of resistant hypertension: association between resistant hypertension, aldosterone, and persistent intravascular volume expansion. Arch Intern Med. 2008;168:1159–64. doi: 10.1001/archinte.168.11.1159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Calhoun DA, Nishizaka MK, Zaman MA, Thakkar RB, Weissmann P. Hyperaldosteronism among black and white subjects with resistant hypertension. Hypertension. 2002;40:892–6. doi: 10.1161/01.hyp.0000040261.30455.b6. [DOI] [PubMed] [Google Scholar]
- 14.Pimenta E, Gaddam KK, Oparil S, et al. Effects of dietary sodium reduction on blood pressure in subjects with resistant hypertension: results from a randomized trial. Hypertension. 2009;54:475–81. doi: 10.1161/HYPERTENSIONAHA.109.131235. [DOI] [PMC free article] [PubMed] [Google Scholar]


