KEY POINTS
Quebec’s private–public system of prescription drug insurance increased access to insurance for working-age residents and increased user charges for beneficiaries of public drug plans.
Quebec’s regime increased access to medicines for working-age residents of Quebec; however, access to medicines in Quebec is lower than in comparable countries.
The premiums, deductibles and coinsurance under Quebec’s regime represent a greater proportion of income for lower-income households than for high-income ones.
Quebec’s regime did not reduce taxpayer-financed drug expenditures and substantially increased employer- and household-financed expenditures.
As calls for universal pharmacare across Canada become stronger and models for its delivery are considered, it is worth looking at whether Quebec’s current system of drug coverage could serve as a model for the rest of the country. Canada is the only high-income country with a universal health care system that does not include universal coverage of prescription drugs. This was not supposed to be the case. From the 1940s through to the 1964 Royal Commission on Health Services, universal “pharmacare” was envisioned as part of the Canadian “medicare” system.1 However, only the province of Saskatchewan acted on those recommendations by offering universal, comprehensive public drug coverage from 1975 to 1987, after which it switched to universal public coverage for catastrophic drug costs only — a style of more limited drug coverage that would later also be adopted by Manitoba and British Columbia.2 In 1997, Quebec implemented a private–public system of drug coverage designed to ensure that all residents have some form of drug insurance, without increasing public spending on medicines. We review the origins of the Quebec regime and assess its impact on three important goals of financing policy: promoting access to necessary medicines, distributing financial burdens equity and managing system costs efficiently.
How did Quebec’s policy originate?
Quebec’s private–public system of drug coverage emerged in the mid-1990s out of provincial efforts to address public concerns about Quebec’s patchwork of public drug plans at the time.3–6 In particular, there was concern that Quebec’s “Malades sur pied” circular (outpatient circular), which provided drugs directly from hospitals to outpatients with HIV and other specific conditions, had become a “disease lottery” that lacked clear rationale for giving free treatments to some patients but not to others.4 The program was also placing uncompensated financial strains on hospitals.
From 1993 to 1995, Quebec’s Liberal and then Parti Québécois governments commissioned three separate reports on drug coverage. 5 The commissions concluded that more targeted assistance programs would be an inadequate solution to inequities and inefficiencies in Quebec’s system of drug coverage; they also concluded that universal, catastrophic drug coverage would not be sufficient to improve access to medicines. Citizens’ groups, health professionals and Dr. Jean Rochon — Quebec’s minister of health under the Parti Québécois from September 1994 to December 1998 — supported a universal public drug plan as the most equitable and efficient option for covering the Quebec population. 4,5 However, such a plan posed substantial political risks, owing to opposition from the insurance industry and retail pharmacies and in view of the Quebec government’s commitment to balancing budgets at a time when global pharmaceutical expenditures were growing rapidly and federal transfers for health care were diminishing.3–5
In the end, the Quebec government compromised: it opted for a mixed, private–public system designed to ensure that all residents had drug insurance without an increase in public spending on medicines.7 To achieve coverage goals without increasing government spending, Quebec increased user charges for senior citizens and recipients of social assistance who were beneficiaries of existing public drug programs as of August 1996. Charges for persons aged 65 and older, for example, increased from a premium-free public plan that involved copayments of $2 per prescription before August 1996, to a public plan that required premiums of up to $175 per year, deductibles of $100 per year and coinsurance of 25% of prescription costs.3
Then, as of January 1997, all employers that provided any health benefits to employees were required to provide private drug coverage that met or exceeded minimum standards defined by the terms of a basic public plan. Individuals who were not eligible for private insurance by way of occupation were required to enrol in, and pay premiums for, a basic public plan administered by government.
The general structure of the Quebec regime has not changed substantially since 1997. However, the deductibles, coinsurance rates and maximum annual contributions have increased over time. Between 1997 and 2017, monthly deductibles under the public plan increased by 133%, from $8.33 to $19.45; the coinsurance rate for costs beyond deductibles increased from 25% to 34.8%; and the maximum annual out-of-pocket contribution increased from $750 to $1066 per adult.8 These terms of coverage under the public plan also serve as limits on the allowable charges under private drug plans in Quebec.
What are the effects of the policy?
Access to medicines
Quebec’s system of drug coverage involved a combination of increased access to insurance for some and increased user charges for others, which has generated mixed results in terms of access to medicines. National survey data showed that the implementation of Quebec’s policy increased access to insurance and increased the use of both medicines and physicians’ services among the working-age population.9 This advantage with respect to insurance for working-aged Quebecers appears to have been sustained: as of 2014, 9.2% of Quebecers aged 55 to 64 reported that they had not filled prescriptions because of cost, whereas 13.9% of similarly aged residents in the rest of Canada reported such access barriers.10
Observational studies found that the implementation of Quebec’s policy was associated with reductions in the use of essential and nonessential medicines among beneficiaries of existing public drug plans, particularly recipients of social assistance.11,12 The Quebec government therefore reduced user charges for recipients of social assistance in 2002 and eliminated those charges in 2007. As a result of remaining user charges under Quebec’s public drug plan, survey data indicate that older Quebecers do not have the same comparative access advantages as working-age Quebecers: in 2014, 6.6% of Quebecers aged 65 and older reported that they had not filled prescriptions owing to cost, whereas 4.1% of similarly aged residents in the rest of Canada reported such access barriers.10
Overall access to medicines in Quebec is lower than in comparable high-income countries with universal coverage of prescription drugs. As shown in Table 1, among all adults aged 18 and older, 8.8% of Quebecers skipped prescriptions because of cost in 2016.13 That is better than the 10.7% average for the rest of Canada, but worse than the 6% or less in most comparator countries. The poorer-performing systems in international comparisons of access to medicines, including Canada’s and Quebec’s, involve higher user charges for prescriptions than those found in better-performing systems, such as the United Kingdom’s.16
Table 1:
Cost-related nonadherence to prescription drugs, total out-of-pocket payments and total pharmaceutical expenditure per capita for Canada, Quebec and 9 comparable high-income countries with universal health insurance*
| Jurisdiction | Cost-related nonadherence: % of adult population reporting they did not fill a prescription or skipped doses because of the cost in 2016 | Out-of-pocket costs: % of adult population reporting their household spent $1000 or more in out-of-pocket costs in 2007 | Total pharmaceutical expenditure per capita in 2014, Canadian dollars (purchasing power parity), $ |
|---|---|---|---|
| Quebec | 8.8 | 8.7 | 1087 |
| Rest of Canada | 10.7 | 4.8 | 912 |
| Population-weighted average for Canada | 10.2 | 5.7 | 952 |
| Australia | 6.3 | 5.3 | 753† |
| New Zealand | 5.7 | 2.4 | 369‡ |
| Norway | 3.4 | – | 564 |
| Sweden | 5.7 | – | 603 |
| United Kingdom | 2.1 | 1.2 | 598 |
| Population-weighted average for universal public systems | 3.6 | – | 621 |
| France | 3.9 | – | 809 |
| Germany | 3.2 | 2.8 | 900 |
| Netherlands | 4.4 | 0.9 | 494 |
| Switzerland | 8.9 | – | 914 |
| Population-weighted average for social insurance systems | 3.8 | – | 826 |
Authors’ calculations based on the Commonwealth Fund’s 2016 International Health Policy Survey; the Commonwealth Fund’s 2007 International Health Policy Survey; Statistics Canada’s 2007 Survey of Household Spending; and the Organisation for Economic Co-operation and Development’s Health Data 2016 data sets.13–15
Projected from 2013 based on growth rates in other comparator countries.
Projected from 2007 based on growth rates in other comparator countries.
Financial equity
Although equity may be a subjective construct, there is reasonable consensus that, at the very least, the system of financing necessary health care should not make economic inequality in a society worse than it already is.17 Quebec’s system of prescription drug coverage is inequitable by that standard because it involves a substantial amount of premium-based financing and user charges, both of which represent a greater financial burden on lower-income households than on higher-income households. For example, under Quebec’s public drug plan, all two-adult households with incomes higher than $39 880 must pay $1334 in annual premiums.8 That mandatory public premium represents more than 3% of household income for couple families earning $40 000; it represents 1.6% of income for couple families earning the $80 000 median income of such households; and it represents 0.7% or less of income for the roughly 10% of couple families with incomes higher than $180 000.18
Premiums for private insurance in Quebec may be even more regressive. This is because private drug coverage is mandatory in Quebec for eligible employee groups and insurers can increase premiums each year to reflect past and expected future costs of medicines used, even if this results in premiums that are higher than in the public plan. As a result, mandatory private drug plan premiums in Quebec can equal 10% or more of annual income for some individuals, such as part-time workers.19,20 Furthermore, as a result of group-specific pooling, private premiums can be lower for members of wealthier and healthier groups (e.g., university professors) than for members of less wealthy and less healthy work groups (e.g., taxi drivers).
The monthly deductibles and coinsurance charges can add substantial additional household costs for those who need medicines. In 2015, 32% of Quebec households reported having spent more than $500 out of pocket on prescription drugs in the year, whereas only 19% of Canadians in the rest of the country reported such levels of out-of-pocket costs.21 Furthermore, as shown in Table 1, high out-of-pocket costs are more common in Quebec and the rest of Canada than in comparator countries. In 2007, 8.7% of Quebec households incurred more than $1000 in out-of-pocket costs for prescriptions, compared with 4.8% for the rest of Canada and less than 3% for comparator countries with universal drug coverage that involves limited user charges (New Zealand, the UK, Germany and the Netherlands).
System costs
A final major consideration for prescription drug financing is efficiency in managing total system costs, including government and nongovernment expenditure. As shown in Table 1, total per capita expenditure on pharmaceuticals during 2014 was $1087 in Quebec and $912 in the rest of Canada. Those levels are substantially higher than the averages of $621 in comparable countries with universal public health insurance and $826 in comparable countries with universal social insurance systems. A study of spending on primary care medicines found that differences in expenditure levels across these countries are driven primarily by prices and product selection decisions rather than prescribing volumes.22
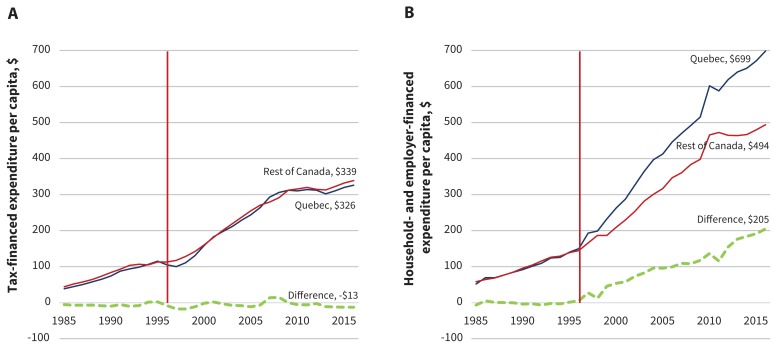
Pharmaceutical spending was not always higher in Quebec than in the rest of Canada. As shown in Figure 1A, on a per capita basis, prescription drug expenditure financed through taxation (government general revenues) in Quebec was similar to that in the rest of Canada before and after Quebec implemented its private–public drug insurance system in 1997. In contrast, Figure 1B shows that per capita expenditure financed by households and employers — through private and public premiums and user charges — was approximately equal in Quebec and the rest of Canada until 1997, but then grew faster in Quebec than in the rest of Canada.
Figure 1:
Expenditure per capita on prescription drugs from 1985 to 2016 in Quebec and the rest of Canada, (A) tax-financed versus (B) household- and employer-financed. Source: Authors’ calculations-based data from Canadian Institute for Health Information National Health Expenditure Trends, 1975 to 2016.23 Tax-financed expenditures are those paid through government general revenues; household- and employer-financed expenditures are those paid out of pocket or through premium contributions to mandatory private or public insurance plans. Quebec data for 2015 and 2016 projected based on five-year average growth rates.
By 2016, Quebecers were financing $205 more per capita through household and employer contributions than residents in the rest of Canada. Thus, if household- and employer-financed costs in Quebec had grown at the same rate as they did in the rest of Canada since 1997, Quebec households and employers would be spending $1.7 billion less per year on prescription drugs. Put another way, if the rest of Canada had matched Quebec’s expenditure growth rates since 1997, households and employers in all other provinces would be spending $5.7 billion more per year on prescription drugs.
What are the lessons for Quebec and the rest of the country?
The introduction of Quebec’s private–public system of drug insurance 20 years ago was a political compromise by a government that wanted all Quebecers to have drug coverage while it avoided both conflict with industry stakeholders and tax increases.3–5 The policy successfully increased drug insurance coverage, which improved access to medicines for working adults. Measures to appease stakeholders and limit tax increases have had negative impacts on access, financial equity and overall cost control.
Quebec’s private–public system of drug insurance brought with it new and steadily increasing deductibles, coinsurance rates and premiums. These charges had predictable negative consequences on access to medicine among beneficiaries of public plans that were previously more comprehensive. Furthermore, Quebec’s private–public system of drug financing has not spared taxpayers a heavy burden; on the contrary, it has added substantial charges to households and employers that constitute a fast-rising and regressive tax under a different name.
It is not too late for Quebec to adopt what, 20 years ago, was viewed to be the most equitable and efficient system of drug coverage for Quebecers: a universal, public program. Such a system would increase purchasing power and better integrate the management of pharmaceuticals with the management of other major components of health care. Quebec could achieve this by mandating participation in a public drug program, leaving private insurance for voluntary coverage of other extended health services and medicines not covered by the universal public plan. If such a system achieved outcomes for Quebec on par with average comparable countries abroad, it could save Quebecers $3.8 billion every year — 12 times the annual amount that was recently saved through voluntary rebates from manufacturers of generic drugs in Quebec.24
The lessons for the rest of Canada are similar. Quebec’s experience indicates that a mixed private–public system of prescription drug financing in Canada would improve access to insurance while generating mixed results in terms of access to medicines and very negative results in terms of control of overall expenditure. In contrast, a universal public pharmacare program could save Canadians $7.3 billion per year if designed like the universal public systems abroad, which also achieve better outcomes in terms of access to medicines and out-of-pocket costs for patients.25 Making that happen will require political leadership that puts the interest of the public good — and the goals of access, equity and efficiency — above the interests of a few, albeit powerful, stakeholders.
Footnotes
Competing interests: Marc-André Gagnon reports a grant from Health Canada and personal fees from Prescrire International and from the Canadian Association of Pharmacy in Oncology, all outside the submitted work. No other competing interests were declared.
This article has been peer reviewed.
Contributors: Steven Morgan and Marc-André Gagnon contributed to the conception of the work. All authors contributed to the collection and interpretation of evidence. Steven Morgan drafted the article and all other authors revised the manuscript for important intellectual content. All of the authors agree to be accountable for all aspects of the work.
References
- 1.Boothe K. Ideas and the limits on program expansion: the failure of nationwide Pharmacare in Canada since 1944. Can J Polit Sci 2013;46:419–53. [Google Scholar]
- 2.Morgan SG, Daw JR. Canadian pharmacare: looking back, looking forward. Healthc Policy 2012;8:14–23. [PMC free article] [PubMed] [Google Scholar]
- 3.Morgan SG. Quebec’s drug insurance plan: a prescription for Canada? HPRU 98-2D. Vancouver: UBC Centre for Health Services and Policy Research; 1998. [Google Scholar]
- 4.Pomey M-P, Forest P-G, Palley HA, et al. Public/private partnerships for prescription drug coverage: policy formulation and outcomes in Quebec’s universal drug insurance program, with comparisons to the Medicare prescription drug program in the United States. Milbank Q 2007;85:469–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pomey M-P, Martin E, Forest P-G. Making decisions about prescriptions drugs in Quebec: implementing the public prescription drug insurance regime in 1996–1997. Kingston (ON): Queen’s University; 2005. [Google Scholar]
- 6.Martin M. Quebec employs user-pay philosophy in launching drug-insurance plan. CMAJ 1996;155:1604–5. [PMC free article] [PubMed] [Google Scholar]
- 7.Castonguay C, Borgeat L, Champigny-Robillard L, et al. Drug insurance: possible approaches. Report of the Committee of Experts on Drug Insurance. Montréal: Bibliothèque nationale du Québec; 1996. [Google Scholar]
- 8.Prescription drug insurance: summary of costs. Québec: City Régie de l’assurance maladie; 2017. Available: www.ramq.gouv.qc.ca/en/citizens/prescription-drug-insurance/Pages/summary-costs.aspx (accessed 2017 July 31). [Google Scholar]
- 9.Wang C, Li Q, Sweetman A, et al. Mandatory universal drug plan, access to health care and health: evidence from Canada. J Health Econ 2015;44:80–96. [DOI] [PubMed] [Google Scholar]
- 10.Lee A, Morgan S. Cost-related nonadherence to prescribed medicines among older Canadians in 2014: a cross-sectional analysis of a telephone survey. CMAJ Open 2017;5:E40–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Blais L, Couture J, Rahme E, et al. Impact of a cost sharing drug insurance plan on drug utilization among individuals receiving social assistance. Health Policy 2003;64:163–72. [DOI] [PubMed] [Google Scholar]
- 12.Tamblyn R, Laprise R, Hanley JA, et al. Adverse events associated with prescription drug cost-sharing among poor and elderly persons. JAMA 2001;285:421–9. [DOI] [PubMed] [Google Scholar]
- 13.How Canada compares: results from the Commonwealth fund’s 2016 international health policy survey of adults in 11 countries [data tables]. Ottawa: Canadian Institute for Health Information (CIHI); 2016. [Google Scholar]
- 14.OECD health statistics 2016. Paris: Organisation for Economic Co-operation and Development (OECD); 2016. [Google Scholar]
- 15.Schoen C, Osborn R, Doty MM, et al. Toward higher-performance health systems: adults’ health care experiences in seven countries, 2007. Health Aff (Millwood) 2007;26:w717–34. [DOI] [PubMed] [Google Scholar]
- 16.Morgan SG, Lee A. Cost-related non-adherence to prescribed medicines among older adults: a cross-sectional analysis of a survey in eleven developed countries. BMJ Open 2017;7:e014287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hurley J. Chapter 2 — An overview of the normative economics of the health sector. In: Culyer AJ, Newhouse JP, editors. Handbook of Health Economics. Vol. 1, Part A Elsevier; 2000:55–118. [Google Scholar]
- 18.Median total income, by family type, by province and territory (all census families). Ottawa: Statistics Canada; 2016. [Google Scholar]
- 19.Roy J. Assurance-médicaments: un retraité obligé de souscrire à un régime privé qu’il juge trop cher. Le Journal de Québec 2017. April 29. [Google Scholar]
- 20.Roy J. L’assurance-médicaments est inéquitable pour plusieurs Québécois. Le Journal de Québec 2017. May 1. [Google Scholar]
- 21.Prescription drug access and affordability: an issue for nearly a quarter of all Canadian households. Vancouver: Angus Reid Institute; 2015. [Google Scholar]
- 22.Morgan SG, Leopold C, Wagner AK. Drivers of expenditure on primary care prescription drugs in 10 high-income countries with universal health coverage. CMAJ 2017;189:E794–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.National health expenditure trends, 1975 to 2016. Ottawa: Canadian Institute for Health Information (CIHI); 2016. Available: www.cihi.ca/en/national-health-expenditure-trends (accessed 2017 Aug. 3). [Google Scholar]
- 24.Morgan SG, Persaud N. Generic drug prices could drop — if rebates are replaced with public tendering. Toronto: La Ki Shing Knowledge Institute, St. Michael’s Hospital; 2017. Available: http://healthydebate.ca/opinions/generic-drug-prices (accessed 2017 Aug. 3). [Google Scholar]
- 25.Morgan SG, Law M, Daw JR, et al. Estimated cost of universal public coverage of prescription drugs in Canada. CMAJ 2015;187:491–7. [DOI] [PMC free article] [PubMed] [Google Scholar]