Abstract
Introduction
The guidelines of the international hernia societies recommend laparo-endoscopic inguinal hernia repair for recurrent hernias after open primary repair. To date, no randomized trials have been conducted to compare the TEP vs TAPP outcome for recurrent inguinal hernia repair. A Swiss registry study identified only minor differences between the two techniques, thus suggesting the equivalence of the two procedures.
Materials and Methods
Between September 1, 2009 and August 31, 2013 data were entered into the Herniamed Registry on a total of 2246 patients with recurrent inguinal hernia repair following previous open primary operation in either TAPP (n = 1,464) or TEP technique (n = 782).
Results
Univariable and multivariable analysis did not find any significant difference between TEP and TAPP with regard to the intraoperative complications, complication-related reoperations, re-recurrences, pain at rest, pain on exertion, or chronic pain requiring treatment. The only difference identified was a significantly higher postoperative seroma rate after TAPP, which was influenced by the surgical technique, previous open primary operation and EHS-classification medial and responded to conservative treatment.
Conclusion
TEP and TAPP are equivalent surgical techniques for recurrent inguinal hernia repair following previous open primary operation. The choice of technique should be tailored to the surgeon’s expertise.
Keywords: Hernia, Recurrent inguinal hernia, TEP, TAPP, Seroma
In the updated guidelines on laparoscopic (TAPP) and endoscopic (TEP) treatment of inguinal hernia, the International Endohernia Society states as grade A recommendation for primary inguinal hernias, following comparison of the two laparo-endoscopic techniques, that both techniques are acceptable treatment options for inguinal hernia repair and there are sufficient data to conclude that both TAPP and TEP are effective methods of laparo-endoscopic primary inguinal hernia repair (1). A comparative Swiss registry study with a large proportion of TEP operations identified for primary inguinal hernias higher perioperative complication rates for TEP (2), whereas a German registry study with a large proportion of TAPP operations detected a higher perioperative complication rate for TAPP (3). Comparison of the outcome of laparo-endoscopic inguinal hernia repair for primary inguinal hernias with that of recurrent inguinal hernias revealed that recurrent procedures are associated with significantly higher postoperative complication rates, complication-related reoperation rates, and higher pain and recurrence rates (4).
There are six meta-analyses available for comparison of laparo-endoscopic with open repair of recurrent inguinal hernias (5, 6, 7, 8, 9, 10). The meta-analysis by Pisanu (8) contained the largest number of exclusively prospective randomized trials (RCTs) (11, 12, 13, 14, 15, 16, 17). All the RCTs included in that meta-analysis compared the laparo-endoscopic procedures with the open Lichtenstein technique. Three RCTs compared the Lichtenstein operation with TAPP (13, 15, 17), two RCTs compared it with TEP (11, 16), and two RCTs compared it with both TEP and TAPP (12, 14).
In the meta-analysis, only joint comparison of the two laparo-endoscopic techniques (TEP, TAPP) with the open Lichtenstein technique was performed. There was no high risk of bias in any of the included trials (8). The meta-analysis by Pisanu et al. (8) detected for laparo-endoscopic repair of recurrent hernias a significantly lower chronic pain rate and significantly earlier resumption of normal everyday activities. Compared with the Lichtenstein operation, the operative time for laparo-endoscopic procedures was significantly longer (8). On the basis of the meta-analyses, the European Hernia Society recommends laparo-endoscopic inguinal hernia repair for recurrent hernias after conventional open repair (10, 18). No distinction is made here between the laparo-endoscopic TEP and TAPP techniques.
To date, no randomized trials have been conducted to compare the TEP vs TAPP outcome for recurrent inguinal hernia repair following previous open repair. A Swiss registry study (19) compared the outcome of a total of 1309 laparo-endoscopic recurrent operations, of which 1022 used the TEP technique and 287 the TAPP technique. A significantly higher intraoperative complication rate and longer operative time was identified for the TEP group. The postoperative length of hospital stay was longer for patients undergoing TAPP (19). Surgical postoperative complications, general postoperative complications, and conversion rates were not significantly different (19). The authors concluded that the absolute outcome differences are small and that both techniques appear to be safe and effective for patients undergoing laparo-endoscopic repair for unilateral recurrent inguinal hernia (19).
Based on data from the Herniamed Registry (20), the present analysis now compares the outcome of elective laparo-endoscopic recurrent unilateral inguinal hernia repair in men following previous open operation.
Patients and methods
The Herniamed Registry is a multicenter, internet-based hernia registry (20) into which 427 participating hospitals and surgeons engaged in private practice (Herniamed Study Group) have entered data prospectively on their patients who had undergone hernia surgery. All postoperative complications occurring up to 30 days after surgery are recorded. On one-year follow-up, postoperative complications are once again reviewed when the general practitioner and patient complete a questionnaire. They are also asked about any re-recurrence, pain at rest, and on exertion as well as pain requiring treatment. This present analysis compares the prospective data collected for all male patients with a minimum age of 16 years who had undergone elective recurrent unilateral inguinal hernia repair using either transabdominal preperitoneal patch plasty (TAPP) or total extraperitoneal patch plasty (TEP).
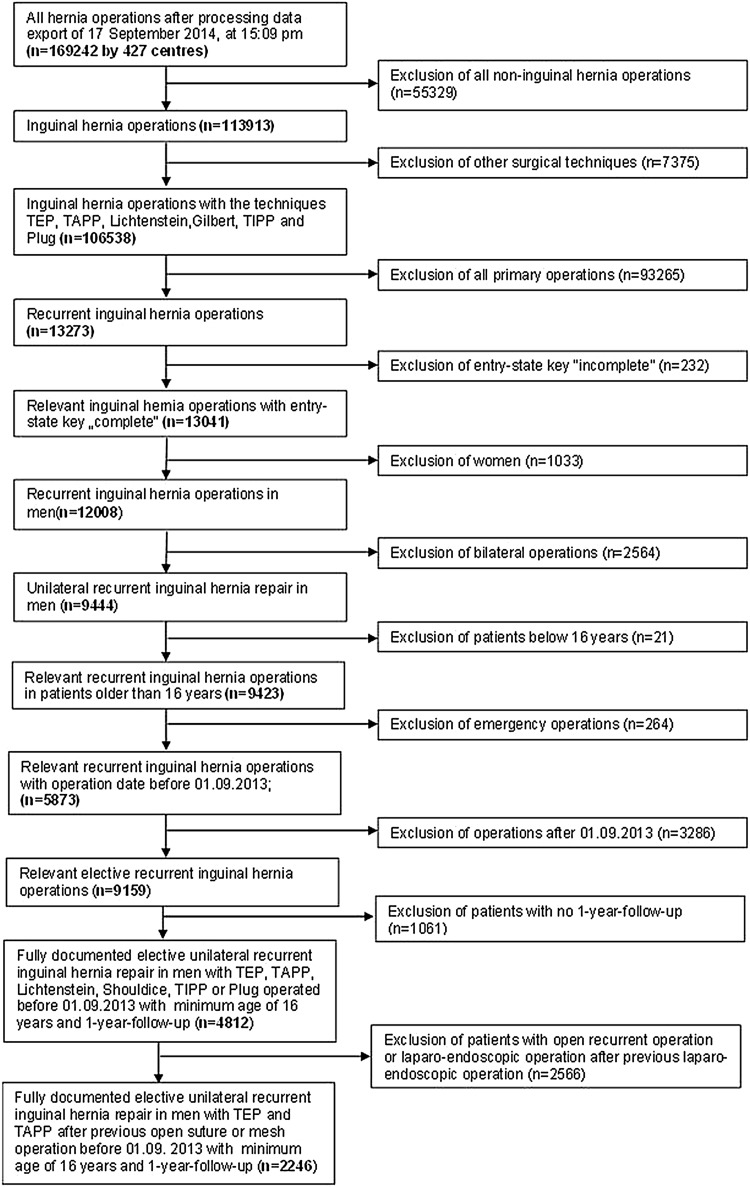
In total, 2,246 patients were enrolled between September 1, 2009, and August 31, 2013 (Fig. 1). Of these patients, 782 (34.8%) had TEP and 1,464 (65.2%) TAPP repair. All the patients had to have one-year follow-up data available (follow-up-rate: 100%).
Fig. 1.
Flowchart of patient inclusion
The majority of primary unilateral repairs in the Herniamed Registry have been performed as open mesh repair (Lichtenstein) with 32.5% and laparo-endoscopic mesh repair (TAPP, TEP) with 49.9%. Non-mesh repairs (Shouldice, Bassini) in primary unilateral inguinal hernia repair in the Herniamed Registry make only a contribution of 4.7% of all cases.
The demographic and surgery-related parameters included age (years), BMI (kg/m2), ASA-score (I, II, III, IV) as well as EHS classification (hernia type: medial, lateral, femoral, scrotal) and defect size: grade I = < 1.5 cm, grade II: 1.5–3 cm, grade III: > 3 cm) (21) and general risk factors (nicotine, COPD, diabetes, cortisone, immunosuppression, etc.). Risk factors were dichotomized, i.e., ‘yes’ if at least one risk factor is positive and ‘no’ otherwise.
The dependent variables were intra- and postoperative complication rates, number of reoperations due to complications as well as the one-year results (re-recurrence rate, pain at rest, pain on exertion, and pain requiring treatment).
All analyses were performed with the software SAS 9.2 (SAS institute Inc. Cary, NY, USA) and intentionally calculated to a full significance level of 5%, i.e., they were not corrected in respect of multiple tests, and each p value ≤ 0.05 represents a significant result. To discern differences between the groups in unadjusted analyses, Fisher’s exact test was used for categorical outcome variables, and the robust t test (Satterthwaite) for continuous variables.
To rule out any confounding of data caused by different patient characteristics, the results of unadjusted analyses were verified via multivariable analyses in which, in addition to TEP or TAPP operation, other influence parameters were simultaneously reviewed.
To identify influence factors in multivariable analyses, the binary logistic regression model for dichotomous outcome variables was used. Estimates for odds ratio (OR) and the corresponding 95% confidence interval based on the Wald test were given. For influence variables with more than two categories, one of the latter forms was used in each case as reference category. For age (years) the 10-year OR estimate and for BMI (kg/m2) the 5-point OR estimate were given. Results were presented in tabular form, sorted by descending impact.
Results
Univariable analysis
In the TEP group, recurrent repair was performed for n = 554/782 (70.8%) patients following previous suture repair and for n = 228/782 (29.2%) after mesh repair. In the TAPP group, recurrent repair was performed for n = 974/1,464 (66.5%) patients after suture and n = 490/1,464 (33.5%) after mesh repair (Table 1).
Table 1.
Laparo-endoscopic recurrent unilateral inguinal hernia repair in men and previous operation
| Previous operation | Total | |||||
|---|---|---|---|---|---|---|
| Suture | Open mesh | |||||
| N | % | N | % | N | % | |
| Procedure | 554 | 36.3 | 228 | 31.8 | 782 | 34.8 |
| TEP | ||||||
| TAPP | 974 | 63.7 | 490 | 68.2 | 1464 | 65.2 |
| Total | 1528 | 100.0 | 718 | 100.0 | 2246 | 100.0 |
No significant difference in mean age and BMI was found between the recurrent operations in TEP and TAPP technique (Table 2). That was also true for the ASA-score, defect size, and risk factors (Table 3). With regard to EHS localization, there were significantly more medial recurrent inguinal hernia defects (52.2% vs. 44.8%; p < 0.001) and significantly fewer lateral defects (55.4% vs. 68.8%; p < 0.001) in the TAPP group (Table 3).
Table 2.
Age and BMI of patients with laparo-endoscopic recurrent unilateral inguinal hernia repair in men
| TEP | TAPP | p | ||
|---|---|---|---|---|
| Age [years] | Mean ± STD | 58.3 ± 15.8 | 59.2 ± 15.4 | 0.186 |
| BMI | Mean ± STD | 26.1 ± 3.5 | 25.9 ± 3.3 | 0.152 |
Table 3.
Demographic- and surgery-related parameters and risk factors of patients with laparo-endoscopic recurrent unilateral inguinal hernia repair in men
| TEP | TAPP | p | |||||
|---|---|---|---|---|---|---|---|
| n | % | n | % | ||||
| ASA-score | I | 186 | 23.79 | 376 | 25.63 | 0.467 | |
| II | 454 | 58.06 | 849 | 57.87 | |||
| III/IV | 142 | 18.16 | 242 | 16.50 | |||
| Defect size | I (< 1,5 cm) | 137 | 17.52 | 282 | 19.22 | 0.524 | |
| II (1,5–3 cm) | 510 | 65.22 | 950 | 64.76 | |||
| III (>3 cm) | 135 | 17.26 | 235 | 16.02 | |||
| Risk factors | Total | yes | 249 | 31.84 | 438 | 29.86 | 0.330 |
| no | 533 | 68.16 | 1029 | 70.14 | |||
| COPD | yes | 63 | 8.06 | 88 | 6.00 | 0.063 | |
| no | 719 | 91.94 | 1379 | 94.00 | |||
| Diabetes | yes | 45 | 5.75 | 84 | 5.73 | 0.978 | |
| no | 737 | 94.25 | 1383 | 94.27 | |||
| Aortic aneurysm | yes | 6 | 0.77 | 10 | 0.68 | 0.818 | |
| no | 776 | 99.23 | 1457 | 99.32 | |||
| Immunosuppression | yes | 5 | 0.64 | 9 | 0.61 | 0.941 | |
| no | 777 | 99.36 | 1458 | 99.39 | |||
| Corticoid | yes | 9 | 1.15 | 11 | 0.75 | 0.335 | |
| no | 773 | 98.85 | 1456 | 99.25 | |||
| Smoking | yes | 88 | 11.25 | 174 | 11.86 | 0.669 | |
| no | 694 | 88.75 | 1293 | 88.14 | |||
| Coagulopathy | yes | 11 | 1.41 | 22 | 1.50 | 0.861 | |
| no | 771 | 98.59 | 1445 | 98.50 | |||
| Antiplatelet medication | yes | 73 | 9.34 | 129 | 8.79 | 0.669 | |
| no | 709 | 90.66 | 1338 | 91.21 | |||
| Anticoagulation therapy | yes | 16 | 2.05 | 28 | 1.91 | 0.823 | |
| no | 766 | 97.95 | 1439 | 98.09 | |||
| EHS-classification medial | yes | 350 | 44.76 | 765 | 52.15 | <0.001 | |
| no | 432 | 55.24 | 702 | 47.85 | |||
| EHS-classification lateral | yes | 538 | 68.80 | 813 | 55.42 | <0.001 | |
| no | 244 | 31.20 | 654 | 44.58 | |||
| EHS-classification femoral | yes | 22 | 2.81 | 55 | 3.75 | 0.245 | |
| no | 760 | 97.19 | 1412 | 96.25 | |||
| EHS-classification scrotal | yes | 6 | 0.77 | 21 | 1.43 | 0.168 | |
| no | 776 | 99.23 | 1446 | 98.57 | |||
As regards the target parameters, no differences were found between TEP and TAPP recurrent inguinal hernia repair in the intraoperative complications (Table 4). For the postoperative complications, significantly lower values (1.7% vs. 4.6%; p < 0.001) were identified for TEP, but that was mainly due to the difference in the seroma rate (0.5% vs. 3.2%; p < 0.001) (Table 4).
Table 4.
Univariable analysis of intra- and postoperative complications, complication-related reoperations, and 1-year follow-up results of patients with laparo-endoscopic recurrent unilateral inguinal hernia repair in men
| TEP | TAPP | p | ||||||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | |||||
| Intraoperative complication | Total | yes | 13 | 1.66 | 13 | 0.89 | 0.101 | |
| no | 769 | 98.34 | 1454 | 99.11 | ||||
| Bleeding | yes | 7 | 0.90 | 8 | 0.55 | 0.332 | ||
| no | 775 | 99.10 | 1459 | 99.45 | ||||
| Injury | Total | yes | 8 | 1.02 | 9 | 0.61 | 0.286 | |
| no | 774 | 98.98 | 1458 | 99.39 | ||||
| Vascular | yes | 4 | 0.51 | 4 | 0.27 | 0.365 | ||
| no | 778 | 99.49 | 1463 | 99.73 | ||||
| Bowel | yes | 0 | 0.00 | 5 | 0.34 | 0.102 | ||
| no | 782 | 100.0 | 1462 | 99.66 | ||||
| Bladder | yes | 2 | 0.26 | 0 | 0.00 | 0.053 | ||
| no | 780 | 99.74 | 1467 | 100.0 | ||||
| Postoperative complication | Total | yes | 13 | 1.66 | 67 | 4.57 | <0.001 | |
| no | 769 | 98.34 | 1400 | 95.43 | ||||
| Bleeding | yes | 10 | 1.28 | 19 | 1.30 | 0.974 | ||
| no | 772 | 98.72 | 1448 | 98.70 | ||||
| Seroma | yes | 4 | 0.51 | 47 | 3.20 | <0.001 | ||
| no | 778 | 99.49 | 1420 | 96.80 | ||||
| Infection | yes | 0 | 0.00 | 1 | 0.07 | 0.465 | ||
| no | 782 | 100.0 | 1466 | 99.93 | ||||
| Bowel injury | yes | 0 | 0.00 | 1 | 0.07 | 0.465 | ||
| no | 782 | 100.0 | 1466 | 99.93 | ||||
| Wound healing disorders | yes | 0 | 0.00 | 1 | 0.07 | 0.465 | ||
| no | 782 | 100.0 | 1466 | 99.93 | ||||
| Reoperation | yes | 11 | 1.41 | 16 | 1.09 | 0.512 | ||
| no | 771 | 98.59 | 1451 | 98.91 | ||||
| Recurrence on follow-up | yes | 7 | 0.90 | 21 | 1.43 | 0.275 | ||
| no | 775 | 99.10 | 1446 | 98.57 | ||||
| Pain in rest on follow-up | yes | 54 | 6.91 | 79 | 5.39 | 0.146 | ||
| no | 728 | 93.09 | 1388 | 94.61 | ||||
| Pain on exertion on follow-up | yes | 92 | 11.76 | 158 | 10.77 | 0.475 | ||
| no | 690 | 88.24 | 1309 | 89.23 | ||||
| Pain requiring treatment on follow-up | yes | 35 | 4.48 | 50 | 3.41 | 0.206 | ||
| no | 747 | 95.52 | 1417 | 96.59 | ||||
However, since this did not result in any difference in the complication-related reoperation rate, it only meant that TAPP was associated with a higher seroma rate, which responded to conservative treatment.
On one-year follow-up no differences were detected in the re-recurrence rate after recurrent inguinal hernia repair following TAPP and TEP, or in the rates of pain at rest, pain on exertion, or chronic pain requiring treatment (Table 4).
Multivariable analyses
For the intraoperative complications, complication-related re-reoperations, and recurrences on follow-up it was not possible to calculate a valid model since the number of positive cases was too small.
Postoperative complications
The results of the model that explored how the variables related to patient and operation characteristics (surgical technique, previous open primary operation, age, BMI, ASA-score, defect size, and defect localization as well as the presence of risk factors) impacted onset of postoperative complications are illustrated in Table 5 (model matching: p < 0.001).
Table 5.
Multivariable analysis of postoperative complications
| Parameter | p value | Category | OR estimate | 95% CI | |
|---|---|---|---|---|---|
| Procedure | <0.001 | TAPP vs TEP | 3.010 | 1.636 | 5.538 |
| Previous operation | 0.044 | Suture vs open mesh | 1.753 | 1.016 | 3.025 |
| EHS-classification medial | 0.049 | yes vs no | 0.457 | 0.209 | 0.997 |
| Defect size | 0.055 | II (1,5–3 cm) vs I (<1,5 cm) | 1.052 | 0.539 | 2.055 |
| III (>3 cm) vs I (<1,5 cm) | 2.012 | 0.935 | 4.329 | ||
| Risk factors | 0.165 | yes vs no | 1.428 | 0.864 | 2.360 |
| Age [10-years-OR] | 0.270 | 1.107 | 0.924 | 1.326 | |
| EHS-classification femoral | 0.297 | yes vs no | 1.717 | 0.621 | 4.746 |
| BMI [5-points-OR] | 0.394 | 0.857 | 0.601 | 1.223 | |
| ASA-score | 0.414 | II vs I | 0.896 | 0.473 | 1.695 |
| III/IV vs I | 1.340 | 0.592 | 3.034 | ||
| EHS-classification scrotal | 0.552 | yes vs no | 1.500 | 0.394 | 5.715 |
| EHS-classification lateral | 0.646 | yes vs no | 0.827 | 0.368 | 1.860 |
The postoperative complications, primarily seromas, were affected by the surgical technique. Conduct of TAPP operation (OR = 3.010 [1.636; 5.538]; p < 0.001) increased the risk of postoperative complications. With a prevalence of 3.6%, this would amount to 53 postoperative complications for every 1000 patients undergoing TAPP operation compared with 18 complications for patients operated on in TEP technique. The risk for development of postoperative complications was also increased in patients with previous open suture repair (OR = 1,753 [1.016; 3.025]; p = 0.044) and decreased in EHS medial classification (OR = 0.457. [0.209; 0.997].
Pain at rest
The results of multivariable analysis of pain at rest are presented in Table 6 (model matching: p = 0.009). Here BMI was the only influence factor identified (p < 0.001). A five-point higher BMI increased pain at rest (5-point OR = 1.483 [1.176; 1.170], but there was no evidence of the surgical technique or previous open primary repair having impacted pain at rest.
Table 6.
Multivariable analysis of pain at rest in 1-year follow-up
| Parameter | p value | Category | OR estimate | 95%-CI | |
|---|---|---|---|---|---|
| BMI [5-points-OR] | <0.001 | 1.483 | 1.176 | 1.870 | |
| Defect size | 0.065 | II (1,5–3 cm) vs I (<1,5 cm) | 0.786 | 0.511 | 1.210 |
| III (>3 cm) vs I (<1,5 cm) | 0.444 | 0.225 | 0.877 | ||
| Procedure | 0.124 | TAPP vs TEP | 0.751 | 0.521 | 1.082 |
| Previous operation | 0.232 | Suture vs open mesh | 0.798 | 0.551 | 1.155 |
| EHS-classification lateral | 0.248 | yes vs no | 0.692 | 0.370 | 1.292 |
| Risk factors | 0.328 | yes vs no | 1.222 | 0.818 | 1.827 |
| EHS-classification medial | 0.372 | yes vs no | 0.758 | 0.412 | 1.394 |
| Age [10-years-OR] | 0.513 | 0.957 | 0.837 | 1.093 | |
| EHS-classification femoral | 0.869 | yes vs no | 1.081 | 0.431 | 2.709 |
| ASA-score | 0.899 | II vs I | 0.941 | 0.595 | 1.490 |
| III/IV vs I | 0.851 | 0.427 | 1.694 | ||
| EHS-classification scrotal | 0.980 | yes vs no | 0.000 | 0.000 | I |
Pain on exertion
The results of multivariable analysis of pain on exertion are shown in Table 7 (model matching: p < 0.001). These were significantly influenced by age, BMI, and defect size. A higher age (10-year OR = 0.846 [0.767; 0.933]; p < 0.001) as well as larger hernias (II vs I: OR = 0.699 [0.508; 0.964]; III vs I: OR = 0.517 [0.318; 0.840]; p = 0.018) reduced the risk of pain on exertion. Conversely, a five-point higher BMI (5-point OR = 1.289 [1.073; 1.549]; p = 0.007) increased the pain risk, but there was no evidence of the surgical technique or previous open primary repair having impacted the postoperative complication rate.
Table 7.
Multivariable analysis of pain on exertion in 1-year follow-up
| Parameter | p value | Category | OR estimate | 95%-CI | |
|---|---|---|---|---|---|
| Age [10-years-OR] | <0.001 | 0.846 | 0.767 | 0.933 | |
| BMI [5-points-OR] | 0.007 | 1.289 | 1.073 | 1.549 | |
| Defect size | 0.018 | II (1,5–3 cm) vs I (<1,5 cm) | 0.699 | 0.508 | 0.964 |
| III (>3 cm) vs I (<1,5 cm) | 0.517 | 0.318 | 0.840 | ||
| EHS-classification lateral | 0.066 | yes vs no | 0.646 | 0.406 | 1.029 |
| EHS-classification scrotal | 0.295 | yes vs no | 0.338 | 0.044 | 2.577 |
| Procedure | 0.365 | TAPP vs TEP | 0.878 | 0.664 | 1.163 |
| EHS-classification medial | 0.405 | yes vs no | 0.823 | 0.520 | 1.302 |
| ASA-score | 0.471 | II vs I | 0.870 | 0.623 | 1.217 |
| III/IV vs I | 1.075 | 0.646 | 1.787 | ||
| Risk factors | 0.632 | yes vs no | 0.925 | 0.674 | 1.270 |
| EHS-classification femoral | 0.797 | yes vs no | 1.096 | 0.543 | 2.214 |
| Previous operation | 0.826 | Suture vs open with mesh | 0.968 | 0.727 | 1.290 |
Chronic pain requiring treatment
The results of multivariable analysis of chronic pain requiring treatment are presented in Table 8 (model matching: p = 0.020). Here BMI was the only significant influence factor identified (p = 0.006). Accordingly, a five-point higher BMI increased the rate of chronic pain requiring treatment (5-point OR = 1.477 [1.121; 1.948]), but there was no evidence of the surgical technique or previous open primary repair having impacted the rate of chronic pain requiring treatment.
Table 8.
Multivariable analysis of chronic pain requiring treatment in 1-year follow-up
| Parameter | p-value | Category | OR estimate | 95%-CI | |
|---|---|---|---|---|---|
| BMI [5-points-OR] | 0.006 | 1.477 | 1.121 | 1.948 | |
| Previous operation | 0.076 | Suture vs open mesh | 0.666 | 0.425 | 1.043 |
| EHS-classification medial | 0.088 | yes vs no | 0.501 | 0.227 | 1.108 |
| Procedure | 0.195 | TAPP vs TEP | 0.742 | 0.473 | 1.165 |
| EHS-classification lateral | 0.246 | yes vs no | 0.615 | 0.270 | 1.399 |
| Defect size | 0.287 | II (1,5–3 cm) vs I (<1,5 cm) | 0.836 | 0.486 | 1.438 |
| III (>3 cm) vs I (<1,5 cm) | 0.515 | 0.225 | 1.179 | ||
| EHS-classification femoral | 0.382 | yes vs no | 1.556 | 0.578 | 4.190 |
| Age [10-years-OR] | 0.446 | 0.937 | 0.793 | 1.107 | |
| Risk factors | 0.544 | yes vs no | 1.166 | 0.710 | 1.915 |
| ASA-score | 0.842 | II vs I | 1.048 | 0.584 | 1.881 |
| III/IV vs I | 1.252 | 0.547 | 2.865 | ||
| EHS-classification scrotal | 0.983 | yes vs no | 0.000 | 0.000 | I |
Discussion
In the Guidelines of the European Hernia Society (EHS) and the International Endohernia Society (IEHS), TEP and TAPP are recommended as equivalent procedures for recurrent hernia repair following the previous open mesh and suture repair of primary inguinal hernias (1, 10, 18). To date, no prospective randomized trials have been conducted to compare TEP and TAPP for recurrent inguinal hernia repair following previous open primary repair. A Swiss registry study that compared laparo-endoscopic recurrent hernia operations identified a significantly higher intraoperative complication rate and longer operative time for TEP operations, which were much more common than TAPP procedures in the patient group analyzed (19). The postoperative length of hospital stay was longer for patients undergoing TAPP (19). Surgical postoperative complications, general postoperative complications, and conversion rates were not significantly different (19). The authors concluded that the absolute outcome differences are small and that both techniques appear to be safe and effective for patients undergoing laparo-endoscopic repair for unilateral recurrent inguinal hernia (19).
Likewise, the present analysis of data from the Herniamed Registry, in which the proportion of TAPP operations was higher than that of the TEP operations, revealed similar outcomes for the laparo-endoscopic recurrent operations following previous open primary operation. Based on the Herniamed Registry data, no significant differences were found between the recurrent operations in TEP vs TAPP technique with regard to the intraoperative complications, complication-related reoperations, re-recurrence rates, rates of pain at rest, pain on exertion, or chronic pain requiring treatment. Unfavorable results were identified only with regard to the higher seroma rates associated with TAPP; these responded to conservative treatment. The influence variables identified here on multivariable analysis were, in addition to the surgical technique, the previous open primary operation and the EHS-classification medial. A previous open primary suture repair has a higher risk for development of a postoperative complication as a previous open primary mesh repair and the EHS-classification medial a lower risk. The results of multivariable analysis of the other parameters did not find any evidence of any impact exerted by the surgical technique.
Accordingly, this analysis of data from the Herniamed Registry corroborates the findings of the Swiss registry study. Similarly, the Herniamed Registry did not detect any significant differences between TEP and TAPP for recurrent unilateral inguinal hernia repair in men following previous open suture or mesh primary operation. That was true for the intraoperative complications, complication-related reoperations, re-recurrence, pain at rest, pain on exertion, and chronic pain requiring treatment on one-year follow-up. The only difference was that TAPP was associated with a higher seroma rate, which responded to conservative treatment. There was no difference in the other postoperative complications between TEP and TAPP for recurrent repair.
In summary, both TEP and TAPP can be recommended as effective techniques for treatment of recurrent inguinal hernia following previous open primary operation. The decision to use one or the other technique should be based solely on the surgeon’s expertise. The registry study presented here thus confirms the recommendations in the guidelines on laparo-endoscopic treatment of recurrent inguinal hernia following previous open primary operation.
Acknowledgements
Ferdinand Köckerling – Grants to fund the Herniamed Register from Johnson & Johnson, Norderstedt, Karl Storz, Tuttlingen, pfm medical, Cologne, Dahlhausen, Cologne, B Braun, Tuttlingen, MenkeMed, Munich and Bard, Karlsruhe.
Herniamed Study Group
Scientific Board
Köckerling, Ferdinand (Chairman) (Berlin); Bittner, Reinhard (Rottenburg); Fortelny, René (Wien); Jacob, Dietmar (Berlin); Koch, Andreas (Cottbus); Kraft, Barbara (Stuttgart); Kuthe, Andreas (Hannover); Lippert, Hans (Magdeburg):Lorenz, Ralph (Berlin); Mayer, Franz (Salzburg); Moesta, Kurt Thomas (Hannover); Niebuhr, Henning (Hamburg); Peiper, Christian (Hamm); Pross, Matthias (Berlin); Reinpold, Wolfgang (Hamburg); Simon, Thomas (Weinheim); Stechemesser, Bernd (Köln); Unger, Solveig (Chemnitz).
Participants
Ahmetov, Azat (Saint-Petersburg); Alapatt, Terence Francis (Frankfurt/Main); Albayrak, Nurettin (Herne); Amann, Stefan (Neuendettelsau); Anders, Stefan (Berlin); Anderson, Jürina (Würzburg); Antoine, Dirk (Leverkusen); Arndt, Anatoli (Elmshorn); Asperger, Walter (Halle); Avram, Iulian (Saarbrücken); Baikoglu-Endres, Corc (Weißenburg i. Bay.); Bandowsky, Boris (Damme); Barkus; Jörg (Velbert); Becker, Matthias (Freital); Behrend, Matthias (Deggendorf); Beuleke, Andrea (Burgwedel); Berger, Dieter (Baden–Baden); Birk, Dieter (Bietigheim-Bissingen); Bittner, Reinhard (Rottenburg); Blaha, Pavel (Zwiesel); Blumberg, Claus (Lübeck); Böckmann, Ulrich (Papenburg); Böhle, Arnd Steffen (Bremen); Bolle, Ludger (Berlin); Borchert, Erika (Grevenbroich); Born, Henry (Leipzig); Brabender, Jan (Köln); Breitenbuch von, Philipp (Radebeul); Brož, Miroslav (Ebersbach); Brütting, Alfred (Erlangen); Buchert, Annette (Mallersdorf-Pfaffenberg); Budzier, Eckhard (Meldorf); Burchett, Bert (Waren); Burghardt, Jens (Rüdersdorf); Cejnar, Stephan-Alexander (München); Chirikov, Ruslan (Dorsten); Claußnitzer, Christian (Ulm); Comman, Andreas (Bogen); Crescenti, Fabio (Verden/Aller); Daniels, Thies (Hamburg); Dapunt, Emanuela (Bruneck); Decker, Georg (Berlin); Demmel, Michael (Arnsberg); Descloux, Alexandre (Baden); Deusch, Klaus-Peter (Wiesbaden); Dick, Marcus (Neumünster); Dieterich, Klaus (Ditzingen); Dietz, Harald (Landshut); Dittmann, Michael (Northeim); Drummer, Bernhard (Forchheim); Eckermann, Oliver (Luckenwalde); Eckhoff, Jörn /Hamburg); Ehmann, Frank (Grünstadt); Eisenkrein, Alexander (Düren); Elger, Karlheinz (Germersheim); Engelhardt, Thomas (Erfurt); Erichsen, Axel (Friedrichshafen); Eucker, Dietmar (Bruderholz); Fackeldey, Volker (Kitzingen); Farke, Stefan (Delmenhorst); Faust, Hendrik (Emden); Federmann, Georg (Seehausen); Feichter, Albert (Wien); Fiedler, Michael (Eisenberg); Fikatas, Panagiotis (Berlin); Firl, Michaela (Perleberg); Fischer, Ines (Wiener Neustadt); Fleischer, Sabine (Dinslaken); Fortelny, René H. (Wien); Franczak, Andreas (Wien); Franke, Claus (Düsseldorf); Frankenberg von, Moritz (Salem); Frehner, Wolfgang (Ottobeuren); Friedhoff, Klaus (Andernach); Friedrich, Jürgen (Essen); Frings, Wolfram (Bonn); Fritsche, Ralf (Darmstadt); Frommhold, Klaus (Coesfeld); Frunder, Albrecht (Tübingen); Fuhrer, Günther (Reutlingen); Gassler, Harald (Villach); Gawad, Karim A. Frankfurt/Main); Gehrig, Tobias (Sinsheim); Gerdes, Martin (Ostercappeln); Germanov, German (Halberstadt; Gilg, Kai-Uwe (Hartmannsdorf); Glaubitz, Martin (Neumünster); Glauner-Goldschmidt, Kerstin (Werne); Glutig, Holger (Meissen); Gmeiner, Dietmar (Bad Dürrnberg); Göring, Herbert (München); Grebe, Werner (Rheda-Wiedenbrück); Grothe, Dirk (Melle); Gürtler, Thomas (Zürich); Hache, Helmer (Löbau); Hämmerle, Alexander (Bad Pyrmont); Haffner, Eugen (Hamm); Hain, Hans-Jürgen (Gross-Umstadt); Hammans, Sebastian (Lingen); Hampe, Carsten (Garbsen); Hanke, Stefan (Halle); Harrer, Petra (Starnberg); Hartung, Peter (Werne); Heinzmann, Bernd (Magdeburg); Heise, Joachim Wilfried (Stolberg); Heitland, Tim (München); Helbling, Christian (Rapperswil); Hempen, Hans-Günther (Cloppenburg); Henneking, Klaus-Wilhelm (Bayreuth); Hennes, Norbert (Duisburg); Hermes, Wolfgang (Weyhe); Herrgesell, Holger (Berlin); Herzing, Holger Höchstadt); Hessler, Christian (Bingen); Heuer, Matthias (Herten); Hildebrand, Christiaan (Langenfeld); Höferlin, Andreas (Mainz); Hoffmann, Henry (Basel); Hoffmann, Michael (Kassel); Hofmann, Eva M. (Frankfurt/Main); Hornung, Frederic (Wolfratshausen); Hügel, Omar (Hannover); Hüttemann, Martin (Oberhausen); Hunkeler, Rolf (Zürich); Imdahl, Andreas (Heidenheim); Isemer, Friedrich-Eckart (Wiesbaden); Jablonski, Herbert Gustav (Sögel); Jacob, Dietmar (Berlin); Jansen-Winkeln, Boris (Leipzig); Jantschulev, Methodi (Waren); Jenert, Burghard (Lichtenstein); Jugenheimer, Michael (Herrenberg); Junger, Marc (München); Kaaden, Stephan (Neustadt am Rübenberge); Käs, Stephan (Weiden); Kahraman, Orhan (Hamburg); Kaiser, Christian (Westerstede); Kaiser, Gernot Maximilian (Kamp-Lintfort); Kaiser, Stefan (Kleinmachnow); Kapischke, Matthias (Hamburg); Karch, Matthias (Eichstätt); Kasparek, Michael S. (München); Keck, Heinrich (Wolfenbüttel); Keller, Hans W. (Bonn); Kienzle, Ulrich (Karlsruhe); Kipfmüller, Brigitte (Köthen); Kirsch, Ulrike (Oranienburg); Klammer, Frank (Ahlen); Klatt, Richard (Hagen); Klein, Karl-Hermann (Burbach); Kleist, Sven (Berlin); Klobusicky, Pavol (Bad Kissingen); Kneifel, Thomas (Datteln); Knoop, Michael (Frankfurt/Oder); Knotter, Bianca (Mannheim); Koch, Andreas (Cottbus); Koch, Andreas (Münster); Köckerling, Ferdinand (Berlin); Köhler, Gernot (Linz); König, Oliver (Buchholz); Kornblum, Hans (Tübingen); Krämer, Dirk (Bad Zwischenahn); Kraft, Barbara (Stuttgart); Kratsch, Barthel (Dierdorf/Selters); Kreissl, Peter (Ebersberg); Krones, Carsten Johannes (Aachen); Kronhardt, Heinrich (Neustadt am Rübenberge); Kruse, Christinan (Aschaffenburg); Kube, Rainer (Cottbus); Kühlberg, Thomas (Berlin); Kühn, Gert (Freiberg); Kuhn, Roger (Gifhorn); Kusch, Eduard (Gütersloh); Kuthe, Andreas (Hannover); Ladberg, Ralf (Bremen); Ladra, Jürgen (Düren); Lahr-Eigen, Rolf (Potsdam); Lainka, Martin (Wattenscheid); Lammers, Bernhard J. (Neuss); Lancee, Steffen (Alsfeld); Lange, Claas (Berlin); Langer, Claus (Göttingen); Laps, Rainer (Ehringshausen); Larusson, Hannes Jon (Pinneberg); Lauschke, Holger (Duisburg); Leher, Markus (Schärding); Leidl, Stefan (Waidhofen/Ybbs); Lenz, Stefan (Berlin); Liedke, Marc Olaf (Heide); Lienert, Mark (Duisburg); Limberger, Andreas (Schrobenhausen); Limmer, Stefan (Würzburg); Locher, Martin (Kiel); Loghmanieh, Siawasch (Viersen); Lorenz, Ralph (Berlin); Luther, Stefan (Wipperfürth); Luyken, Walter (Sulzbach-Rosenberg); Mallmann, Bernhard (Krefeld); Manger, Regina (Schwabmünchen); Maurer, Stephan (Münster); May, Jens Peter (Schönebeck); Mayer, Franz (Salzburg); Mayer, Jens (Schwäbisch Gmünd); Mellert, Joachim (Höxter); Menzel, Ingo (Weimar); Meurer, Kirsten (Bochum); Meyer, Moritz (Ahaus); Mirow, Lutz (Kirchberg); Mittag-Bonsch, Martina (Crailsheim); Mittenzwey, Hans-Joachim (Berlin); Möbius, Ekkehard (Braunschweig); Mörder-Köttgen, Anja (Freiburg); Moesta, Kurt Thomas (Hannover); Moldenhauer, Ingolf (Braunschweig); Morkramer, Rolf (Xanten); Mosa, Tawfik (Merseburg); Müller, Hannes (Schlanders); Münzberg, Gregor (Berlin); Murr, Alfons (Vilshofen); Mussack, Thomas (St. Gallen); Nartschik, Peter (Quedlinburg); Nasifoglu, Bernd (Ehingen); Neumann, Jürgen (Haan); Neumeuer, Kai (Paderborn); Niebuhr, Henning (Hamburg); Nix, Carsten (Walsrode); Nölling, Anke (Burbach); Nostitz, Friedrich Zoltán (Mühlhausen); Obermaier, Straubing); Öz-Schmidt, Meryem (Hanau); Oldorf, Peter (Usingen); Olivieri, Manuel (Pforzheim); Passon, Marius (Freudenberg); Pawelzik, Marek (Hamburg); Pein, Tobias (Hameln); Peiper, Christian (Hamm); Peiper, Matthias (Essen); Peitgen, Klaus (Bottrop); Pertl, Alexander (Spittal/Drau); Philipp, Mark (Rostock); Pickart, Lutz (Bad Langensalza); Pizzera, Christian (Graz); Pöllath, Martin (Sulzbach-Rosenberg); Possin, Ulrich (Laatzen); Prenzel, Klaus (Bad Neuenahr-Ahrweiler); Pröve, Florian (Goslar); Pronnet, Thomas (Fürstenfeldbruck); Pross, Matthias (Berlin); Puff, Johannes (Dinkelsbühl); Rabl, Anton (Passau); Raggi, Matthias Claudius (Stuttgart); Rapp, Martin (Neunkirchen); Reck, Thomas (Püttlingen); Reinpold, Wolfgang (Hamburg); Reuter, Christoph (Quakenbrück); Richter, Jörg (Winnenden); Riemann, Kerstin (Alzenau-Wasserlos); Riesener, Klaus-Peter (Marl); Rodehorst, Anette (Otterndorf); Roehr, Thomas (Rödental); Rössler, Michael (Rüdesheim am Rhein); Roncossek, Bremerhaven); Rosniatowski, Rolland (Marburg); Roth Hartmut (Nürnberg); Sardoschau, Nihad (Saarbrücken); Sauer, Gottfried (Rüsselsheim); Sauer, Jörg (Arnsberg); Seekamp, Axel (Freiburg); Seelig, Matthias (Bad Soden); Seidel, Hanka (Eschweiler); Seiler, Christoph Michael (Warendorf); Seltmann, Cornelia (Hachenburg); Senkal, Metin (Witten); Shamiyeh, Andreas (Linz); Shang, Edward (München); Siemssen, Björn (Berlin); Sievers, Dörte (Hamburg); Silbernik, Daniel (Bonn); Simon, Thomas (Weinheim); Sinn, Daniel (Olpe); Sinner, Guy (Merzig); Sinning, Frank (Nürnberg); Smaxwil, Constatin Aurel (Stuttgart); Sörensen, Björn (Lauf an der Pegnitz); Syga, Günter (Bayreuth); Schabel, Volker (Kirchheim/Teck); Schadd, Peter (Euskirchen); Schassen von, Christian (Hamburg); Scheidbach, Hubert (Neustadt/Saale); Schelp, Lothar (Wuppertal); Scherf, Alexander (Pforzheim); Scheuerlein, Hubert (Paderborn); Scheyer, Mathias (Bludenz); Schilling, André (Kamen); Schimmelpenning, Hendrik (Neustadt in Holstein); Schinkel, Svenja (Kempten); Schmid, Michael (Gera); Schmid, Thomas (Innsbruck); Schmidt, Ulf (Mechernich); Schmitz, Heiner (Jena); Schmitz, Ronald (Altenburg); Schöche, Jan (Borna); Schoenen, Detlef (Schwandorf); Schrittwieser, Rudolf /Bruck an der Mur); Schroll, Andreas (München); Schubert, Daniel (Saarbrücken); Schüder, Gerhard (Wertheim); Schultz, Christian (Bremen-Lesum); Schultz, Harald (Landstuhl); Schulze, Frank P. Mülheim an der Ruhr); Schulze, Thomas (Dessau-Roßlau); Schumacher, Franz-Josef (Oberhausen); Schwab, Robert (Koblenz); Schwandner, Thilo (Lich); Schwarz, Jochen Günter (Rottenburg); Schymatzek, Ulrich (Eitorf); Spangenberger, Wolfgang (Bergisch-Gladbach); Sperling, Peter (Montabaur); Staade, Katja (Düsseldorf); Staib, Ludger (Esslingen); Staikov, Plamen (Frankfurt am Main); Stamm, Ingrid (Heppenheim); Stark, Wolfgang (Roth); Stechemesser, Bernd (Köln); Steinhilper, Uz (München); Stengl, Wolfgang (Nürnberg); Stern, Oliver (Hamburg); Stöltzing, Oliver (Meißen); Stolte, Thomas (Mannheim); Stopinski, Jürgen (Schwalmstadt); Stratmann, Gerald (Goch); Stubbe, Hendrik (Güstrow/); Stülzebach, Carsten (Friedrichroda); Tepel, Jürgen (Osnabrück); Terzić, Alexander (Wildeshausen); Teske, Ulrich (Essen); Tichomirow, Alexej (Brühl); Tillenburg, Wolfgang (Marktheidenfeld); Timmermann, Wolfgang (Hagen); Tomov, Tsvetomir (Koblenz; Train, Stefan H. (Gronau); Trauzettel, Uwe (Plettenberg); Triechelt, Uwe (Langenhagen); Ulbricht, Wolfgang (Breitenbrunn); Ulcar, Heimo (Schwarzach im Pongau); Unger, Solveig (Chemnitz); Verweel, Rainer (Hürth); Vogel, Ulrike (Berlin); Voigt, Rigo (Altenburg); Voit, Gerhard (Fürth); Volkers, Hans-Uwe (Norden); Volmer, Ulla (Berlin); Vossough, Alexander (Neuss); Wallasch, Andreas (Menden); Wallner, Axel (Lüdinghausen); Warscher, Manfred (Lienz); Warwas, Markus (Bonn); Weber, Jörg (Köln); Weber, Uwe (Eggenfelden); Weihrauch, Thomas (Ilmenau); Weiß, Johannes (Schwetzingen); Weißenbach, Peter (Neunkirchen); Werner, Uwe (Lübbecke-Rahden); Wessel, Ina (Duisburg); Weyhe, Dirk (Oldenburg); Wieber, Isabell (Köln); Wiesmann, Aloys (Rheine); Wiesner, Ingo (Halle); Withöft, Detlef (Neutraubling); Woehe, Fritz (Sanderhausen); Wolf, Claudio (Neuwied); Wolkersdörfer, Toralf (Pößneck); Yaksan, Arif (Wermeskirchen); Yildirim, Can (Lilienthal); Yildirim, Selcuk (Berlin); Zarras, Konstantinos (Düsseldorf); Zeller, Johannes (Waldshut-Tiengen); Zhorzel, Sven (Agatharied); Zuz, Gerhard (Leipzig);
Compliance with ethical standards
Disclosures
R. Bittner, A, Kuthe, M. Hukauf, F. Mayer, R. Fortelny, C. Schug-Pass have no conflicts of interest or financial ties to disclose.
References
- 1.Bittner R, Montgomery MA, Arregui E, Bansal V, Bingener J, Bisgaard T, Buhck H, Dudai M, Ferzli GS, Fitzgibbons RL, Fortelny RH, Grimes KL, Klinge U, Köckerling F, Kumar S, Kukleta J, Lomanto D, Misra MC, Morales-Conde S, Reinpold W, Rosenberg J, Singh K, Timoney M, Weyhe D, Chowbey P; International Endohernia Society Update of guidelines on laparoscopic (TAPP) and endoscopic (TEP) treatment of inguinal hernia (International Endohernia Society) Surg Endos. 2015 ; 29 (2): 289–321 DOI:10.1007/s00464-014-3917-8 [DOI] [PMC free article] [PubMed]
- 2.Gass M, Banz VM, Rosella L, Adamina M, Candinas D, Güller U TAPP or TEP? Population-Based Analysis of Prospective Data on 4,552 Patients Undergoing Endoscopic Inguinal Hernia RepairWorld J Surg (2012) 36: 2782–2786 Doi:10.1007/s00268-012-1760-4 [DOI] [PubMed]
- 3.Köckerling F, Bittner R, Jacob DA, Seidelmann L, Keller T, Adolf D, Kraft B, Kuthe A. TEP versus TAPP: comparison of the perioperative outcome in 17,587 patients with an primary unilateral inguinal hernia. Surg Endosc. 2015;29:3750–3760. doi: 10.1007/s00464-015-4150-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Köckerling F, Jacob D, Wiegank W, Hukauf M, Schug-Pass C, Kuthe A, Bittner A. Endoscopic repair of primary versus recurrent male unilateral inguinal hernias: Are there differences in the outcome? Surg Endosc. 2016;30:1146–1155. doi: 10.1007/s00464-015-4318-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Karthikesalingam A, Markar SR, Holt PJE, Praseedom RK. Meta-analysis of randomized controlled trials comparing laparoscopic with open mesh repair of recurrent inguinal hernia. Br J Surg. 2010;97:4–11. doi: 10.1002/bjs.6902. [DOI] [PubMed] [Google Scholar]
- 6.Dedemadi G, Sgourakis G, Radtke A, Dounavis A, Gockel I, Fouzas I, Karaliotis C, Anagnostou E Laparoscopic versus open mesh repair for recurrent inguinal hernia: a meta-analysis of outcomes The American Journal of Surgery (2010) 200, 291–297 [DOI] [PubMed]
- 7.Yang J, Tong DN, Yao J, Chen W. Laparoscopic or Lichtenstein repair for recurrent inguinal hernia: a meta-analysis of randomized controlled trials. ANZ J Surg. 2012 doi: 10.1111/ans.12010. [DOI] [PubMed] [Google Scholar]
- 8.Pisanu A, Podda M, Saba A, Porceddu G, Uccheddu A. Meta-analysis and review of prospective randomized trials comparing laparoscopic and Lichtenstein techniques in recurrent inguinal hernia repair. Hernia. 2014 doi: 10.1007/s10029-014-1281-1. [DOI] [PubMed] [Google Scholar]
- 9.Li, J, Ji Z, Li Y Comparison of laparoscopic versus open procedure in the treatment of recurrence inguinal hernia: a meta-analysis of the results The American Journal of Surgery (2014) 207, 602–612 DOI:10.1016/j.amjsurg.2013.05.008 [DOI] [PubMed]
- 10.Miserez M, Peeters E, Aufenacker T, Bouillot JL, Campanelli G, Conze J, Fortelny R, Heikkinen T, Jorgensen LN, Kukleta J, Morales-Conce S, Nordin P, Schumpelick V, Smedberg S, Smietanski M, Weber G, Simons MP. Update with level 1 studies of the European Hernia Society guindelines on the treatment of inguinal hernia in adult patients. Hernia. 2014;18(2):151–163. doi: 10.1007/s10029-014-1236-6. [DOI] [PubMed] [Google Scholar]
- 11.Kumar S, Nixon SL, MacIntryre IM Laparoscopic or Lichtenstein repair for recurrent inguinal hernia: one unit’s experience JR Coll Surg Edinb. 1999 Oct; 44 (5): 301–302 [PubMed]
- 12.Neumayer L, Giobbie-Hurder A, Jonasson O, Fitzgibbons R, Jr, Dunlop D, Gibbs J Reda D, Henderson W. Veterans Affairs Cooperative Studies Program 456 Open mesh versus laparoscopic mesh repair of inguinal hernia. N Engl J Med. 2004;350(8):1819–27. doi: 10.1056/NEJMoa040093. [DOI] [PubMed] [Google Scholar]
- 13.Rahr HB, Bendix J, Ahlburg P, Gjedsted J, Funch-Jensen P, Coagulation Tønnesen E, inflammatory and stress responses in a randomized comparison of open and laparoscopic repair of recurrent inguinal hernia. Surg Endosc. 2006;20(3):468–472. doi: 10.1007/s00464-005-0305-4. [DOI] [PubMed] [Google Scholar]
- 14.Dedemadi G, Sgourakis G, Karaliotas C, Christofides T, Kouraklis G, Karaliotas C. Comparison of laparoscopic and open tension-free repair of recurrent inguinal hernias: a prospective randomized study. Surg Endosc. 2006;20(7):1099–1104. doi: 10.1007/s00464-005-0621-8. [DOI] [PubMed] [Google Scholar]
- 15.Eklund A, Rudberg C, Leijonmarck CE, Rasmussen I, Spangen L, Wickborn G, Wingren U, Montgomery A. Recurrent inguinal hernia: randomized multicenter trial comparing laparoscopic and Lichtenstein repair. Surg Endosc. 2007;21(4):634–640. doi: 10.1007/s00464-006-9163-y. [DOI] [PubMed] [Google Scholar]
- 16.Kouhia St, Huttunen R, Silvasti SO, Heiskanen JT, Ahtola H, Aotila-Nieminen M, Kiviniemi VV, Hakala T. Lichtenstein hernioplasty versus totally extraperitoneal laparoscopic herniaplasty in treatment of recurrent inguinal hernia – a prospective randomized trial. Ann Surg. 2009;249(3):384–387. doi: 10.1097/SLA.0b013e318196d0b0. [DOI] [PubMed] [Google Scholar]
- 17.Demetrashvili Z, Qerqadze V, Kamkamidze G, Topchishvili G, Lagvilava L, Chartholani T, Archvadze V. Comparison of Lichtenstein and laparoscopic transabdominal preperitoneal repair of recurrent inguinal hernias. Int Surg. 2011;96(3):233–8. doi: 10.9738/CC53.1. [DOI] [PubMed] [Google Scholar]
- 18.Simons M, Aufenacker T, Bay-Nielsen M, Bouillot JL, Campanelli G, Conze J, de Lange D, Fortelny R, Heikkinen T, Kingsnorth A, Kukleta J, Morales-Conde S, Nordin P, Schumpelick V, Smedberg S, Smietanski M, Weber G, Miserez M. European Hernia Society guidelines on the treatment of inguinal hernia in adult patients. Hernia. 2009;13(4):343–403. doi: 10.1007/s10029-009-0529-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gass M, Scheiwiller A, Sykora M, Metzger J TAPP or TEP for Recurrent Inguinal Hernia? Population-Based Analysis of Prospective Data on 1309 Patients Undergoing Endoscopic Repair for Recurrent Inguinal Hernia World J Surg; Published online: 05 May 2016 DOI:10.1007/s00268-016-3545-7 [DOI] [PubMed]
- 20.Stechemesser B, Jacob DA, Schug-Pass C, Köckerling F Herniamed: an Internet-based registry for outcome research in hernia surgery Hernia (2012) 16: 269–276 DOI:10.1007/s10029-012-0908-3 [DOI] [PubMed]
- 21.Miserez M, Alexandre JH, Campanelli G, Corcione F, Cuccurullo D, Pascual MH, Hoeferlin A, Kingsnorth AN, Mandala V, Palot JP, Schumpelick V, Simmermacher RK, Stoppa R, Flament JB. The European hernia society groin hernia classification: simple and easy to remember. Hernia. 2007;11(2):113–116. doi: 10.1007/s10029-007-0198-3. [DOI] [PubMed] [Google Scholar]