Abstract
Purpose
Obesity is one of the most common health problems among children and its prevalence has increased in recent decades. Socioeconomic status (SES) is a well-known risk factor for childhood obesity although the associations were different across countries. Previous studies in other countries have reported a positive association between childhood obesity and SES in developing countries, and inverse correlation has been reported in developed countries. For this reason, we wanted to investigate the relationship between SES and obesity in Korean children.
Methods
Data were acquired 3,095 boys and girls who participated in the fifth Korea National Health and Nutrition Examination Survey, which was conducted from 2010 to 2012. Body mass index was calculated from measured anthropometric data using the 2007 Korean National Growth Charts.
Results
Upon univariate analysis, we did not find any statistically significant differences in the parental employment status, monthly family income between children with and without obesity. Multiple logistic regression analysis showed childhood obesity was positively associated with maternal overweight (OR, 1.889; 95% CI, 1.079-3.309), maternal obesity (OR, 3.409; 95% CI, 2.228-5.215) and paternal obesity (OR, 2.135; 95% CI, 1.257-3.627).
Conclusion
The present study showed that socioeconomic status might not an important risk factor for obesity in Korean children. These results warrant further studies to clarify the association between SES and obesity in Korean children.
Keywords: Obesity, Income, Education
INTRODUCTION
Obesity is one of the most common public health problems among children. The worldwide prevalence of childhood obesity has increased in recent decades [1,2], and the incidence of childhood obesity is also rising in Korea [3].
While the exact reason for this increasing prevalence of obesity is unclear, it is widely believed that genetics [4], ethnicity [5], lower physical activity [6], diet [7], shorter sleep [8], and socioeconomic status (SES) [9] contribute to the etiology of obesity.
SES is a well-known risk factor for childhood obesity, although many controversies remain regarding the association between SES and obesity. Many previous studies have reported that individuals with lower SES are at an increased risk for obesity than those with higher SES [9,10], but other studies reported that individuals in higher SES groups tend to be more obese than those in low SES groups [11,12]. In previous Korean studies [13,14,15], results have shown that SES might be an important risk factor for childhood obesity, but the results have not been consistent. Therefore, we investigated whether lower SES was associated with childhood obesity using the most recent dataset (Korea National Health and Nutrition Examination Survey [KNHANES]: 2010-2012).
MATERIALS AND METHODS
Study population
This study was based on data obtained from the fifth KNHANES. The KNHANES was a cross-sectional survey designed to examine the health and nutritional status of the non-institutionalized Korean population. It was conducted by the Division of Chronic Disease Surveillance at the Korea Centers for Disease Control and Prevention (KCDC). Data were collected in a variety of ways, including household interviews, physical examinations, laboratory tests, and nutritional status assessments. All survey protocols were approved by the KCDC Institutional Review Board. Written informed consent was obtained from all participants before the survey began.
We included 5,250 people younger than 18 years of age from the total of 18,066 who participated in the fifth KNHANES study (2010-2012). We excluded participants who we did not have data from both parents and under 2 years old aged children. The remaining 3,095 participants (1,640 boys and 1,455 girls) were included in the final analysis.
General characteristics, anthropometrics and the definition of obesity
The health interview and health behavior surveys included well-established questions to determine the demographic and socioeconomic characteristics of the participants. These surveys included questions regarding age, sex, height, weight, residence area, family income, education level, employment status, marital status, smoking habits and number of household members. The respondents' residential areas were categorized as urban (an administrative division of a city) or rural (not classified as an administrative division of a city). The definition of a city in Korea is a place where more than 50,000 people live and that is larger than a town. Monthly family income indicates monthly equalized family income and was calculated by dividing total family income by the square root of the number of household members. In KNHANES, monthly family income was classified into quartiles to determine monthly household income level (1, low; 2, middle low; 3, middle high; 4, high). Education level was defined as less than high school, high school or college or more. Cigarette use was divided into three categories: current smoker, ex-smoker and non-smoker.
The directly measured anthropometric data (height, weight and body mass index [BMI]) were transformed to the age- and sex-specific percentiles based on the 2007 Korean Growth Charts [16]. The weight status of children was classified as obese (BMI, ≥95th percentile for BMI-for-age), overweight (BMI, 85th to 95th percentile), and normal weight (BMI, <85th percentile) according to the 2007 Korean National Growth Charts [16]. The weight status of parents was classified as normal weight (BMI, <25.0 kg/m2), overweight (BMI, 25.0-29.9 kg/m2), and obese (BMI, ≥30 kg/m2) according to World Health Organization reference [17].
Statistical analyses
We conducted all statistical analyses using SPSS complex sample procedure because KNHANES data was collected through a representative, stratified, and clustered sampling method. For more accurate statistical comparisons, univariate analysis was conducted to select significant covariates. After selection of significant covariates, we carried out binary logistic regression analysis to identify the relationships between risk factors and the prevalence of obesity. Statistical analysis was conducted using the IBM SPSS Statistics ver. 21.0 (IBM Co., Armonk, NY, USA). For all analyses, p-values were two-tailed, and a p-value less than 0.05 was considered statistically significant.
Ethics statement
The study protocol was approved by the institutional review board (IRB) of Samsung Changwon Hospital (IRB no. 2016-SCMC-019-00). Informed consent was exempted by the board.
RESULTS
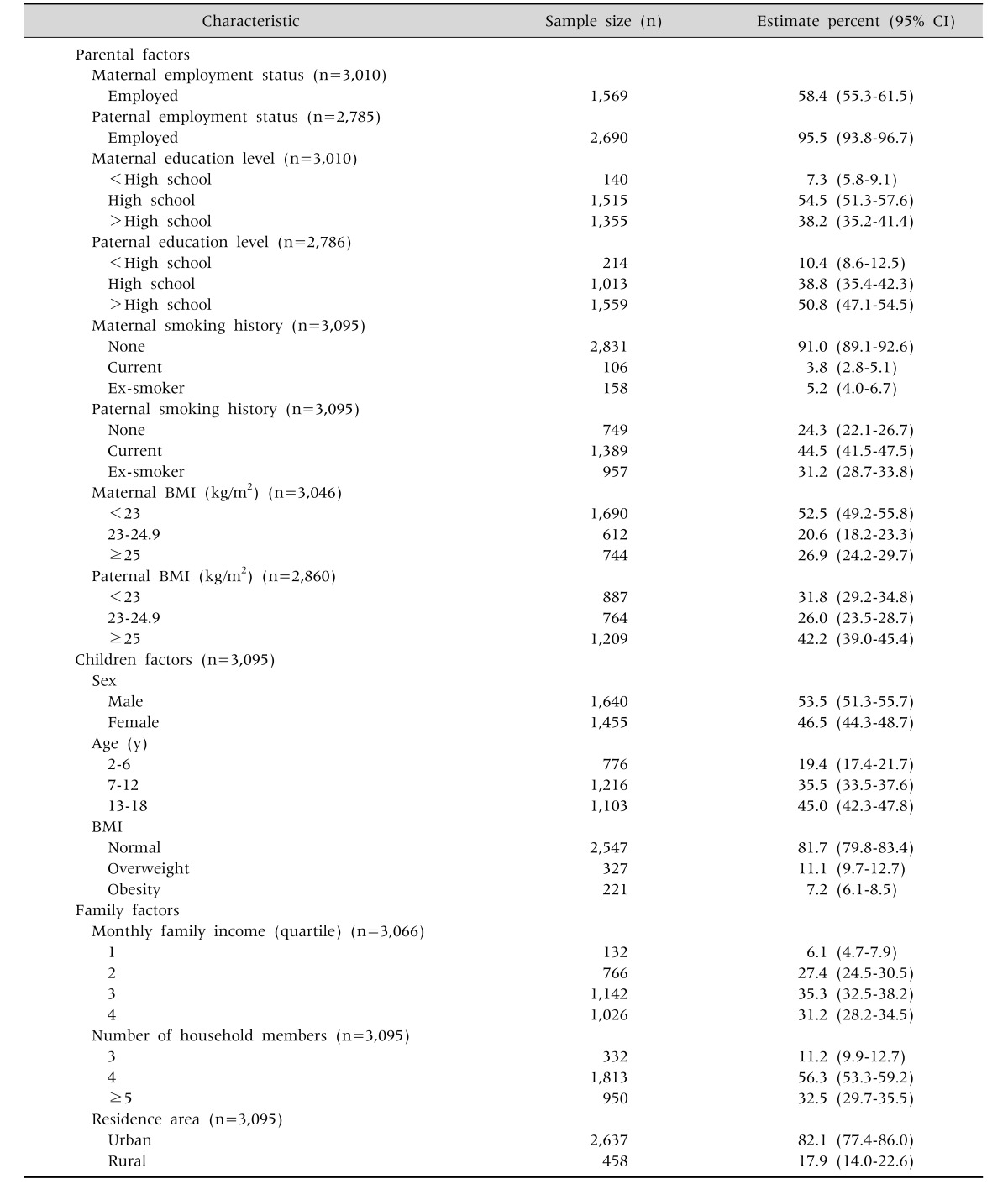
Table 1 summarized clinical characteristics of participants. A total of 3,095 boys and girls from the 2010-2012 periods of the fifth KNHANES were included in this study, and 3,010 mothers and 2,785 fathers were also included. Most of the fathers were employed (95.5%), and the majority of parent had a higher than high school education level (92.7% for mothers, 89.6% for fathers). Current smoking was more prevalent in fathers (44.5%), while mothers were more likely to be non-smokers (91.0%). The mean age of the children was 10.0±4.6, and the proportion of boys was 53.5%. Most enrolled children lived in urban areas (82.1%). The prevalence of childhood obesity was 7.2%, and the proportion of overweight children was 11.1%.
Table 1. Baseline Characteristics of Parents and Children.
BMI: body mass index, 95% CI: 95% confidence interval.
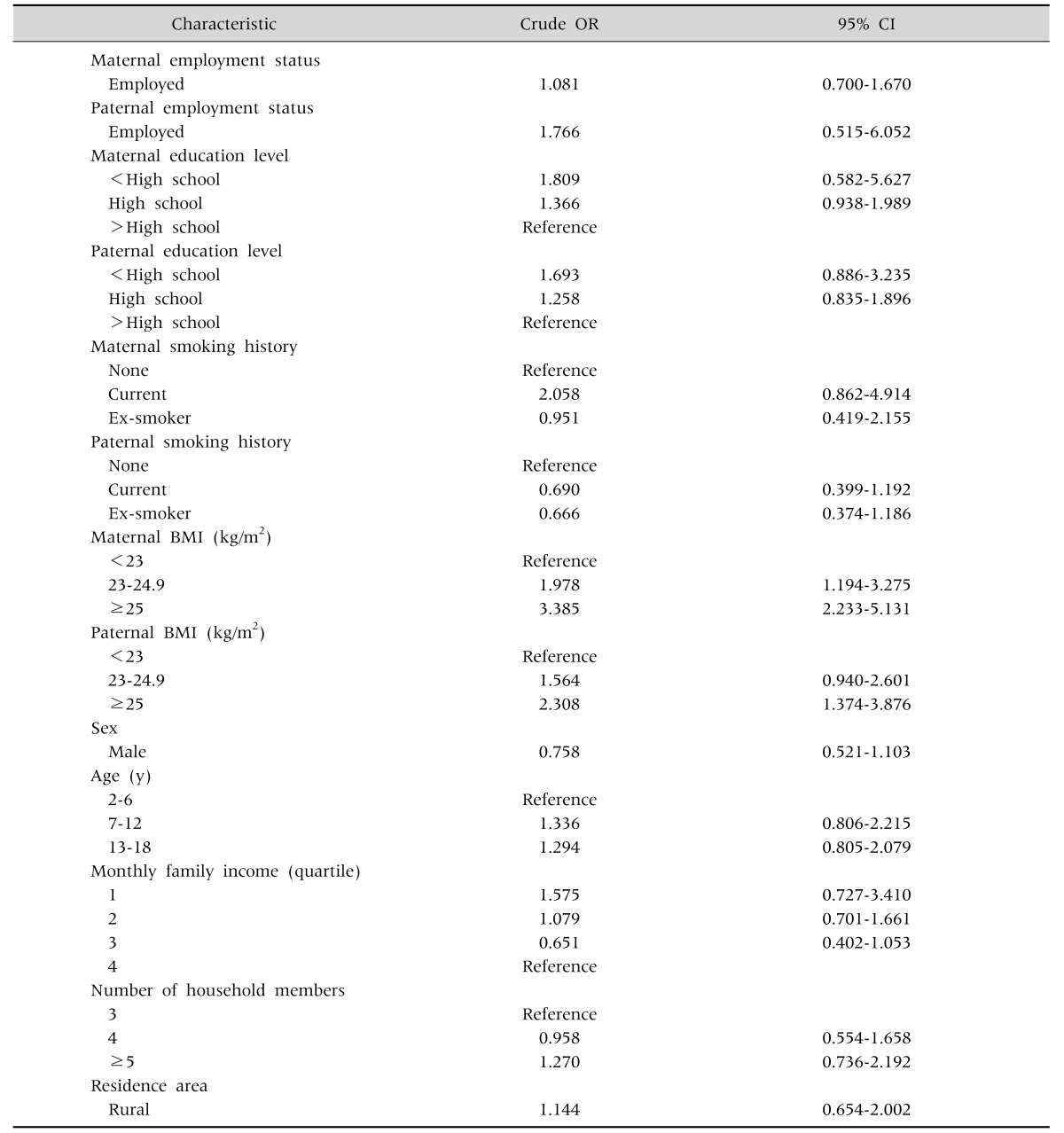
Upon univariate analysis, we did not find any statistically significant differences in the parental employment status, parental education level, parental smoking history, sex, age, monthly family income, number of household members and residence area between children with and without obesity. Compared with the normal weight children, obese children were more prone to have obese mothers (odds ratio [OR], 3.385; 95% confidence interval [CI], 2.233-5.131), obese fathers (OR, 2.308; 95% CI, 1.374-3.876), overweight mothers (OR, 1.978, 95% CI, 1.194-3.275) (Table 2).
Table 2. Crude Odds Ratio (OR) and 95% Confidence Interval (CI) for the Prevalence of Childhood Obesity.
BMI: body mass index.
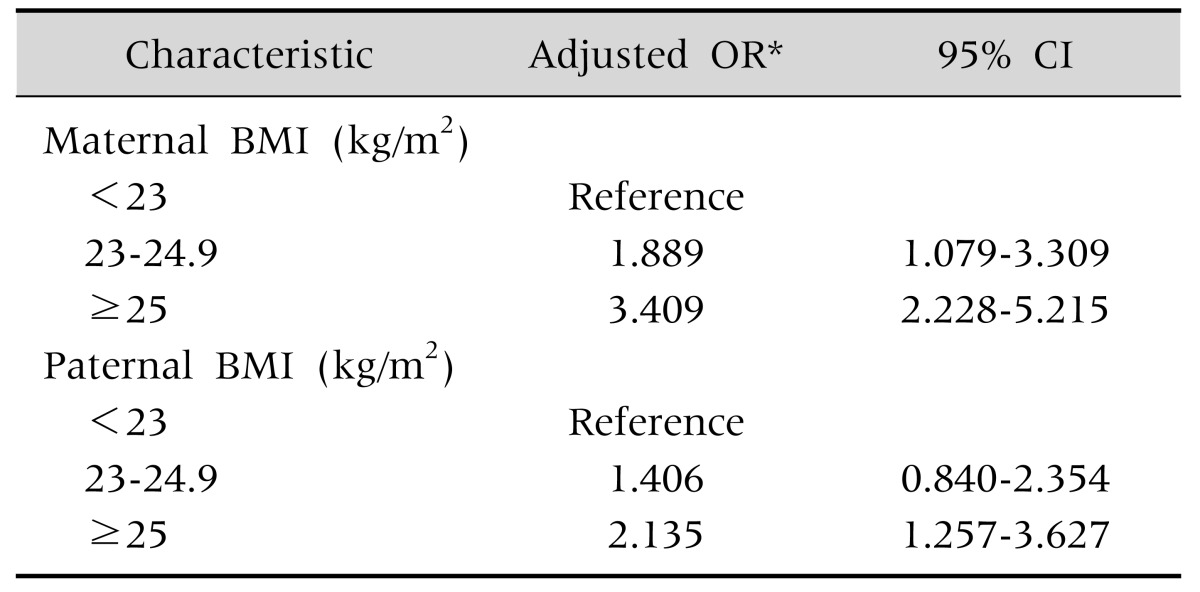
After controlling for confounding factors, the binary logistic regression analysis showed overweight mothers (adjusted OR [aOR], 1.889; 95% CI, 1.079-3.309), obese mothers (aOR, 3.409; 95% CI, 2.228-5.215), obese fathers (aOR, 2.135, 95% CI, 1.257-3.627) were associated with childhood obesity (Table 3).
Table 3. Adjusted Odds Ratio (OR) and 95% Confidence Interval (CI) for the Prevalence of Childhood Obesity.
*Adjusted for maternal body mass index (BMI), paternal BMI.
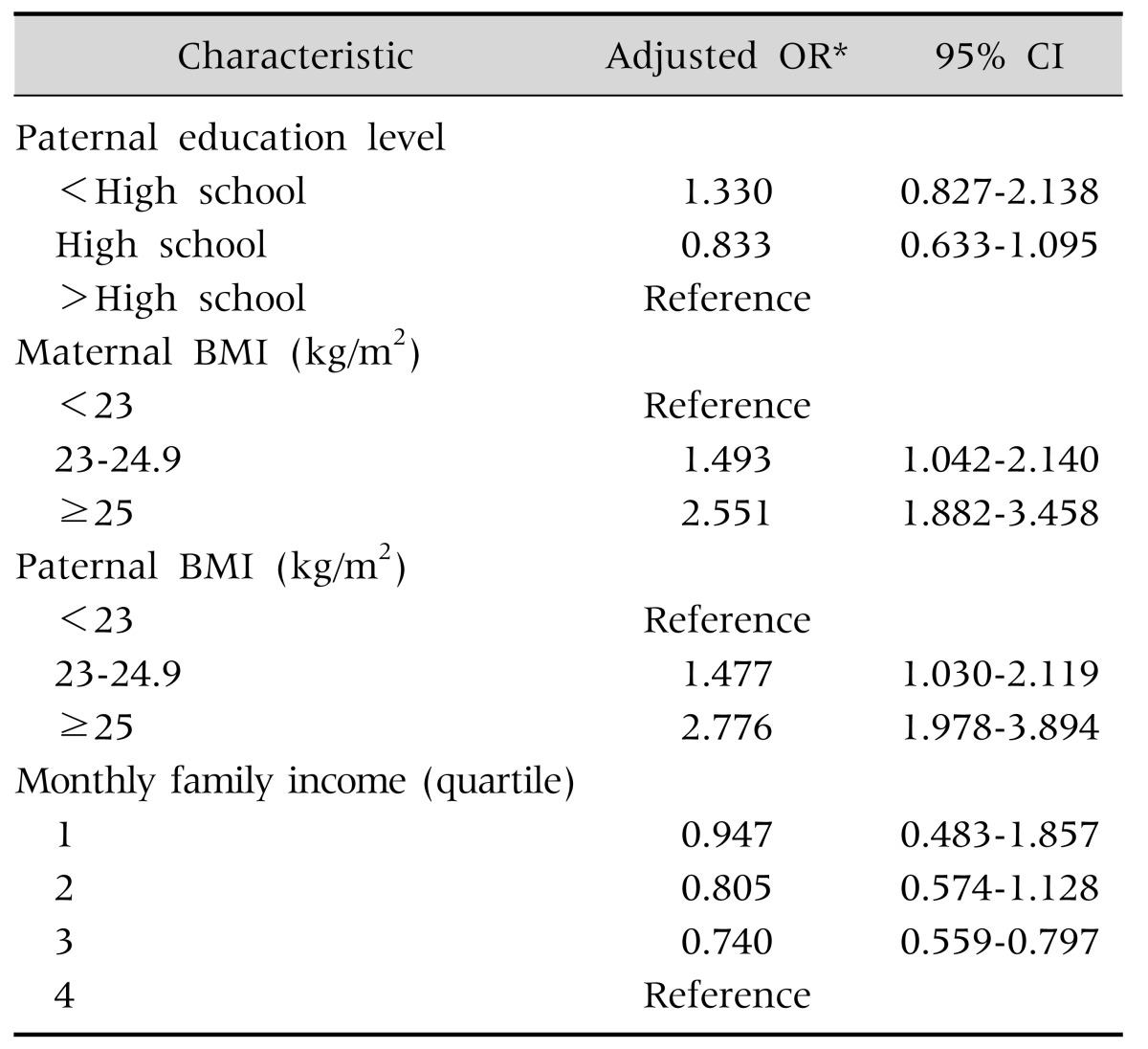
Overweight mothers (aOR, 1.493; 95% CI 1.042-2.140), obese mothers (aOR, 2.551; 95% CI, 1.882-3.458), overweight fathers (aOR, 1.477; 95% CI, 1.030-2.119) and obese fathers (OR, 2.776; 95% CI, 1.978-3.894), were significant factors in binary logistic regression analysis comparing between children with normal weight and those with overweight and obesity (Table 4).
Table 4. Adjusted Odds Ratio (OR) and 95% Confidence Interval (CI) for the Prevalence of Childhood Overweight (Including Obesity).
*Adjusted for paternal education level, maternal body mass index (BMI), paternal BMI, and monthly family income.
DISCUSSION
In our study, childhood obesity was positively associated with maternal overweight, maternal obesity, paternal obesity. Parental obesity is a well-known risk factor of childhood obesity [13,18]. Our results were similar to results of previous studies. Genetics and environmental components are both known to be associated with obesity. Obesity-related genes are inherited from obese parents to their children [19]. In regard to epigenetics, the inherited obesity-related genes interact with the personal environment and this interaction can drive the development of childhood obesity [20]. Epigenetic changes can influence obesity related hormones such as leptin (reduces food intake and decreases body weight) [21], insulin (increases food intake, adiposity, and peripheral insulin resistance) [22], and ghrelin (promotes feeding, suppresses energy expenditure, and causes weight gain) [23]. Moreover, familial life style is an important risk factor of childhood obesity [24] and parental eating behaviors are likely to determine the dietary patterns of children at an early age [25]. In our study, maternal overweight and obesity more influenced childhood obesity than paternal overweight and obesity. These results were also observed in a previous study [26]. We thought this association due to more similarity in nutrient intake between mothers and children than between fathers and children [27]. Traditionally, in Korea, mothers have more responsibility for children care and takes more time than fathers have.
We did not find any association between parental employment status and childhood obesity. The association between parental employment and childhood obesity was controversial. European study showed maternal work hours have no effect on child overweight and obesity [28], but the other study showed parental work hours increased the prevalence of childhood obesity in United States [29]. We assumed these different results might be due to cultural difference in child care system.
In our study, the association between childhood obesity was not dependent on their age and gender. Because childhood obesity was defined as more than 95th percentile BMI for BMI-for-age in our study, obesity was not significantly associated with gender and age in children.
Our study showed parental smoking was not associated with childhood obesity. The effect of paternal smoking on childhood obesity was inconsistent. Some study reported no association between paternal smoking and childhood obesity [30], but the other study reported positive associations [31]. Previous study showed maternal smoking was positively associated with childhood obesity in non-Hispanic white and non-Hispanic Black mothers, while maternal smoking was not associated with childhood obesity in Asian mothers [32].
We did not find urban-rural differences in childhood obesity. The association between residence area and childhood obesity was controversial. One study reported no difference between residence area in childhood obesity [33], the others study reported higher prevalence of childhood obesity in rural area [34]. Because the proportion of urban residence in our study was higher than previous study [34], we thought higher proportion of residence in urban might have some role in our study result.
In our study, number of household members was not associated with childhood obesity, which was different from a previous study [35]. In a previous study, they reported number of household members was negatively associated with childhood obesity [35]. We assume these results might be due to racial or cultural difference.
Two Korean studies using national representative sample data from KNHANES (2007-2010, 1998-2009) showed that SES did not have any association with childhood obesity [13,14]. However, another study using a national representative sample (2009 Korean Survey on the Obesity of Youth and Children) showed that lower SES was associated with childhood obesity [15]. In our study, we found lower SES (parental education, monthly family income) was associated with childhood obesity, but not significant. In previous studies, developed countries have an increasing prevalence of childhood obesity in lower SES group [9,10], but developing countries showed an increasing prevalence of obesity in higher SES group [11,12]. Korea is a recently developed country, and we thought our study results might be similar from other studies in developed countries [9,10].
This study had several limitations. First, because this study was cross-sectional, we could not confirm causality as an explanation for the observed associations. Second, even though this study was based on a national survey, the different results from previous studies might be due to a selection bias or a recall bias. Despite these limitations, this study has important implications. First, this study used a national, widely sampled dataset to determine the association between SES and obesity in Korean children. Second, we were able to adequately address the association between SES and childhood obesity and to shine more light on the discrepancies in previous Korean studies.
Considering the results of other studies, we suggest that SES might be not an important risk factor of obesity in Korean children. Although this hypothesis will require further study, we conclude that each socioeconomic factor affects childhood obesity in a different manner in each country.
References
- 1.Bundred P, Kitchiner D, Buchan I. Prevalence of overweight and obese children between 1989 and 1998: population based series of cross sectional studies. BMJ. 2001;322:326–328. doi: 10.1136/bmj.322.7282.326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Troiano RP, Flegal KM, Kuczmarski RJ, Campbell SM, Johnson CL. Overweight prevalence and trends for children and adolescents. The national health and nutrition examination surveys, 1963 to 1991. Arch Pediatr Adolesc Med. 1995;149:1085–1091. doi: 10.1001/archpedi.1995.02170230039005. [DOI] [PubMed] [Google Scholar]
- 3.Oh K, Jang MJ, Lee NY, Moon JS, Lee CG, Yoo MH, et al. Prevalence and trends in obesity among Korean children and adolescents in 1997 and 2005. Korean J Pediatr. 2008;51:950–955. [Google Scholar]
- 4.Ramachandrappa S, Farooqi IS. Genetic approaches to understanding human obesity. J Clin Invest. 2011;121:2080–2086. doi: 10.1172/JCI46044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Freedman DS, Khan LK, Serdula MK, Ogden CL, Dietz WH. Racial and ethnic differences in secular trends for childhood BMI, weight, and height. Obesity (Silver Spring) 2006;14:301–308. doi: 10.1038/oby.2006.39. [DOI] [PubMed] [Google Scholar]
- 6.Janssen I. Active play: an important physical activity strategy in the fight against childhood obesity. Can J Public Health. 2014;105:e22–e27. doi: 10.17269/cjph.105.4154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Moreno LA, Rodríguez G. Dietary risk factors for development of childhood obesity. Curr Opin Clin Nutr Metab Care. 2007;10:336–341. doi: 10.1097/MCO.0b013e3280a94f59. [DOI] [PubMed] [Google Scholar]
- 8.Al Mamun A, Lawlor DA, Cramb S, O'Callaghan M, Williams G, Najman J. Do childhood sleeping problems predict obesity in young adulthood? Evidence from a prospective birth cohort study. Am J Epidemiol. 2007;166:1368–1373. doi: 10.1093/aje/kwm224. [DOI] [PubMed] [Google Scholar]
- 9.Nogueira H, Gama A, Mourão I, Marques V, Ferrão M, Padez C. The associations of SES, obesity, sport activity, and perceived neighborhood environments: is there a model of environmental injustice penalizing Portuguese children? Am J Hum Biol. 2013;25:434–436. doi: 10.1002/ajhb.22384. [DOI] [PubMed] [Google Scholar]
- 10.Thibault H, Carriere C, Langevin C, Kossi Déti E, Barberger-Gateau P, Maurice S. Prevalence and factors associated with overweight and obesity in French primary-school children. Public Health Nutr. 2013;16:193–201. doi: 10.1017/S136898001200359X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dinsa GD, Goryakin Y, Fumagalli E, Suhrcke M. Obesity and socioeconomic status in developing countries: a systematic review. Obes Rev. 2012;13:1067–1079. doi: 10.1111/j.1467-789X.2012.01017.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wang Y. Cross-national comparison of childhood obesity: the epidemic and the relationship between obesity and socioeconomic status. Int J Epidemiol. 2001;30:1129–1136. doi: 10.1093/ije/30.5.1129. [DOI] [PubMed] [Google Scholar]
- 13.Lee HS, Duffey KJ, Kim CI, Popkin BM. The relationship between family and child weight status by household structure in South Korea: 2007-2010. Nutr Diabetes. 2013;3:e73. doi: 10.1038/nutd.2013.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nam SY, Lee SK. The associations between socioeconomic status and obesity in Korean children from 1998 to 2009. Health. 2013;5:1899–1904. [Google Scholar]
- 15.Noh JW, Kim YE, Oh IH, Kwon YD. Influences of socioeconomic factors on childhood and adolescent overweight by gender in Korea: cross-sectional analysis of nationally representative sample. BMC Public Health. 2014;14:324. doi: 10.1186/1471-2458-14-324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Moon JS, Lee SY, Nam CM, Choi JM, Choe BK, Seo JW, et al. 2007 Korean National Growth Charts: review of developmental process and an outlook. Korean J Pediatr. 2008;51:1–25. [Google Scholar]
- 17.James PT. Obesity: the worldwide epidemic. Clin Dermatol. 2004;22:276–280. doi: 10.1016/j.clindermatol.2004.01.010. [DOI] [PubMed] [Google Scholar]
- 18.Svensson V, Jacobsson JA, Fredriksson R, Danielsson P, Sobko T, Schiöth HB, et al. Associations between severity of obesity in childhood and adolescence, obesity onset and parental BMI: a longitudinal cohort study. Int J Obes (Lond) 2011;35:46–52. doi: 10.1038/ijo.2010.189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Li P, Tiwari HK, Lin WY, Allison DB, Chung WK, Leibel RL, et al. Genetic association analysis of 30 genes related to obesity in a European American population. Int J Obes (Lond) 2014;38:724–729. doi: 10.1038/ijo.2013.140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Herrera BM, Keildson S, Lindgren CM. Genetics and epigenetics of obesity. Maturitas. 2011;69:41–49. doi: 10.1016/j.maturitas.2011.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Halaas JL, Boozer C, Blair-West J, Fidahusein N, Denton DA, Friedman JM. Physiological response to long-term peripheral and central leptin infusion in lean and obese mice. Proc Natl Acad Sci U S A. 1997;94:8878–8883. doi: 10.1073/pnas.94.16.8878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Obici S, Feng Z, Karkanias G, Baskin DG, Rossetti L. Decreasing hypothalamic insulin receptors causes hyperphagia and insulin resistance in rats. Nat Neurosci. 2002;5:566–572. doi: 10.1038/nn0602-861. [DOI] [PubMed] [Google Scholar]
- 23.Nakazato M, Murakami N, Date Y, Kojima M, Matsuo H, Kangawa K, et al. A role for ghrelin in the central regulation of feeding. Nature. 2001;409:194–198. doi: 10.1038/35051587. [DOI] [PubMed] [Google Scholar]
- 24.Sung-Chan P, Sung YW, Zhao X, Brownson RC. Family-based models for childhood-obesity intervention: a systematic review of randomized controlled trials. Obes Rev. 2013;14:265–278. doi: 10.1111/obr.12000. [DOI] [PubMed] [Google Scholar]
- 25.Kral TV, Rauh EM. Eating behaviors of children in the context of their family environment. Physiol Behav. 2010;100:567–573. doi: 10.1016/j.physbeh.2010.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Linabery AM, Nahhas RW, Johnson W, Choh AC, Towne B, Odegaard AO, et al. Stronger influence of maternal than paternal obesity on infant and early childhood body mass index: the Fels longitudinal study. Pediatr Obes. 2013;8:159–169. doi: 10.1111/j.2047-6310.2012.00100.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Oliveria SA, Ellison RC, Moore LL, Gillman MW, Garrahie EJ, Singer MR. Parent-child relationships in nutrient intake: the Framingham children's study. Am J Clin Nutr. 1992;56:593–598. doi: 10.1093/ajcn/56.3.593. [DOI] [PubMed] [Google Scholar]
- 28.Greve J. New results on the effect of maternal work hours on children's overweight status: does the quality of child care matter? Labour Econ. 2011;18:579–590. [Google Scholar]
- 29.Anderson PM, Butcher KF, Levine PB. Maternal employment and overweight children. J Health Econ. 2003;22:477–504. doi: 10.1016/S0167-6296(03)00022-5. [DOI] [PubMed] [Google Scholar]
- 30.Durmus B, Kruithof CJ, Gillman MH, Willemsen SP, Hofman A, Raat H, et al. Parental smoking during pregnancy, early growth, and risk of obesity in preschool children: the generation R study. Am J Clin Nutr. 2011;94:164–171. doi: 10.3945/ajcn.110.009225. [DOI] [PubMed] [Google Scholar]
- 31.von Kries R, Bolte G, Baghi L, Toschke AM GME Study Group. Parental smoking and childhood obesity--is maternal smoking in pregnancy the critical exposure? Int J Epidemiol. 2008;37:210–216. doi: 10.1093/ije/dym239. [DOI] [PubMed] [Google Scholar]
- 32.Sharma AJ, Cogswell ME, Li R. Dose-response associations between maternal smoking during pregnancy and subsequent childhood obesity: effect modification by maternal race/ethnicity in a low-income US cohort. Am J Epidemiol. 2008;168:995–1007. doi: 10.1093/aje/kwn223. [DOI] [PubMed] [Google Scholar]
- 33.Salois MJ. The built environment and obesity among low-income preschool children. Health Place. 2012;18:520–527. doi: 10.1016/j.healthplace.2012.02.002. [DOI] [PubMed] [Google Scholar]
- 34.Davis AM, Bennett KJ, Befort C, Nollen N. Obesity and related health behaviors among urban and rural children in the United States: data from the national health and nutrition examination survey 2003-2004 and 2005-2006. J Pediatr Psychol. 2011;36:669–676. doi: 10.1093/jpepsy/jsq117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Morandi A, Meyre D, Lobbens S, Kleinman K, Kaakinen M, Rifas-Shiman SL, et al. Estimation of newborn risk for child or adolescent obesity: lessons from longitudinal birth cohorts. PLoS One. 2012;7:e49919. doi: 10.1371/journal.pone.0049919. [DOI] [PMC free article] [PubMed] [Google Scholar]