Abstract
Background
Given the increasing societal focus on health care utilization and value-based care, it is essential to understand the demographic and economic data surrounding percutaneous vertebral augmentation procedures performed in the United States. Double-blinded prospective randomized controlled trials have shown no benefit to the use of vertebroplasty over a sham procedure in the treatment of vertebral fractures. Contrastingly, kyphoplasty may be beneficial when appropriately indicated.
Methods
The National Inpatient Sample (NIS) database was queried for patients who underwent either kyphoplasty (ICD-9-CM 81.66) or vertebroplasty (ICD-9-CM 81.65) procedures between 2006 and 2014 across 44 states. Demographic and economic data were obtained which included the annual number of surgeries, age, sex, insurance type, location, and frequency of routine discharge. The NIS database represents a 20% sample of discharges from U.S. hospitals, which is weighted to provide national estimates.
Results
In 2014, an estimated total number of 19,420 kyphoplasty and 6,130 vertebroplasty procedures were performed across the United States. The number of vertebroplasty procedures decreased 53% from 13,128 in 2008. Similarly, the number of kyphoplasty procedures decreased 17% from 23,320 in 2007. Based on payer, Medicare patients comprised 83% of those billed for kyphoplasty and vertebroplasty, and 75% of procedures were utilized in areas designated as “not low income”. In 2014, patients in the South Atlantic region comprised 24% of vertebroplasty and 28% of kyphoplasty cases, far more than any other region. Additionally, kyphoplasty and vertebroplasty were more often performed in teaching facilities rather than community hospitals (60% and 67%, respectively).
Conclusions
Since the publication of two double-blind, prospective randomized controlled trials showed no benefit of vertebroplasty over a sham procedure, there has been a significant decrease in both kyphoplasty and vertebroplasty procedures.
Keywords: Vertebroplasty, kyphoplasty, percutaneous vertebral augmentation, National Inpatient Sample (NIS)
Introduction
The incidence of vertebral compression fractures (VCFs) increases markedly with age and is one of the most common sequelae of osteoporosis, comprising almost half of all osteoporotic fractures in the US annually (1-3). Patients with VCFs often experience severe back pain that may limit mobility and subsequently increase mortality in an already vulnerable elderly population (1). Thus, multiple treatment modalities have been indicated including pain medication, medical osteoporosis treatment, physical therapy, bracing, and surgery. The surgical indications for vertebral augmentation procedures, such as kyphoplasty and vertebroplasty, have varied in the literature, but are most commonly reserved for fractures with significant local deformity and patients with pain refractory to conservative management (4,5).
Vertebroplasty procedures involve the percutaneous injection of bone cement into a fractured vertebra, with the intent of stabilizing the vertebral body thereby improving pain control. Unfortunately, vertebroplasty is unable to restore vertebral height and has been associated with retropulsion of cement into the canal in up to 67% of cases (6-9). Kyphoplasty, a subset of the vertebroplasty procedure, involves the inflation of a small balloon in the vertebral cavity and restoration of sagittal parameters in addition to stabilizing the fractured vertebra (10). Multiple retrospective and prospective trials demonstrating the efficacy of vertebroplasty or kyphoplasty compared to placebo and standard medical therapy have been published (11-13). However, the evidence in those trials was limited by a lack of true blinding with sham-surgery.
In 2009, two double-blind randomized controlled trials utilizing sham-surgery were published and reported no demonstrable difference in pain control or function between study groups. The authors attributed findings of prior studies to a procedural placebo effect (14-17). Due to concerns about low enrollment numbers, inclusion criteria, and particularities of cement injection in these studies, the debate about treatment efficacy has continued (17-19). Nevertheless, the 2009 trials were highly regarded by the orthopaedic and general medical community at large.
The purpose of this study was to determine the trends in kyphoplasty and vertebroplasty procedures over the recent decade, and to evaluate the decline in procedure utilization. By performing a longitudinal analysis of an administrative inpatient database, we may understand the yearly trends and economic data surrounding percutaneous vertebral augmentation procedures. An appreciation for the yearly national aggregate cost of these procedures is of significant importance to surgeons, policy makers and hospital administrators. In this study, we utilized data from the National Inpatient Sample (NIS) database to compare a large national cohort of patients who underwent kyphoplasty and vertebroplasty procedures from 2006 to 2014.
Methods
Data source
Data was collected from 44 states between 2006 and 2014 in the NIS database. The NIS database was developed for the Healthcare Cost and Utilization Project (HCUP) and constitutes the largest all-payer inpatient database in the United States. The database represents a 20% sample of discharges from U.S. hospitals (excluding rehabilitation and long-term acute care hospitals), which is weighted to provide national estimates.
Patient selection and characteristics
The NIS database was queried for patients who underwent either kyphoplasty or vertebroplasty procedures between 2006–2014 using international classification of diseases, ninth revision, clinical modification (ICD-9 CM) codes 81.66 and 81.65, respectively. There were no additional criteria for patient exclusion.
Demographic and economic data were obtained for both kyphoplasty and vertebroplasty procedures. Insurance types included Medicare, Medicaid, private, uninsured, and other. The “other” category included workman’s compensation, TRICARE/CHAMPUS, CHAMPVA, Title V, and a number of other government insurance programs. The annual number of surgeries, patient age, sex, total charges, total costs (in then-year dollars), insurance type, length of stay (LOS), location, and frequency of routine discharge were recorded. Aggregate charges or the “national bill” was defined as the sum of all charges for all hospital stays in the United States. Total charges were converted to costs using cost-to-charge ratios based on hospital accounting reports from the Centers for Medicare and Medicaid Services (CMS). Costs reflect the actual costs of production, while charges represent what the hospital billed for the case. Relative standard error (SE) (SE/weighted estimate) was reported where applicable.
Descriptive statistics were performed to compare variables. A two-sample student t-test was employed to analyze the difference in continuous variables and Chi-squared or Fisher’s exact test was employed for categorical variables. Findings were considered statistically significant when P<0.05. Analysis was conducted using IBM SPSS Statistics Version 24. The NIS database is de-identified and was therefore deemed exempt by our institutional review board.
Results
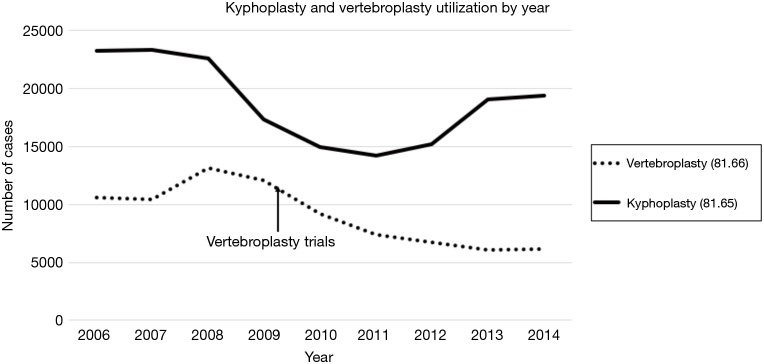
An estimated 81,690 patients underwent vertebroplasty and 169,413 patients underwent kyphoplasty in the United States from 2006 to 2014. The annual total number of procedures for vertebroplasty and kyphoplasty fluctuated until 2009. Subsequently, the number of kyphoplasty cases continued to fluctuate, while vertebroplasty cases progressively declined for the next 5 years. The number of vertebroplasty procedures decreased 53% from 13,128 in 2008. Similarly, the number of kyphoplasty procedures decreased 17% from 23,320 in 2007. The most dramatic decline for vertebroplasty procedures over a single year was 24% from 12,093 cases in 2009 to 9,179 cases in 2010, while the most dramatic decline for kyphoplasty procedures over a single year was 23% from 22,591 cases in 2008 to 17,367 cases in 2009 (Figure 1).
Figure 1.
Total number of discharges per year was plotted for both vertebroplasty and kyphoplasty from 2006–2014. Vertebroplasty ICD-9-CM: 81.66; Kyphoplasty ICD-9-CM: 81.65. The two trials questioning the validity of vertebroplasty were published in 2009. Vertebroplasty cases decreased from 2009–2014 while kyphoplasty cases initially decreased and then increased from 2012–2014.
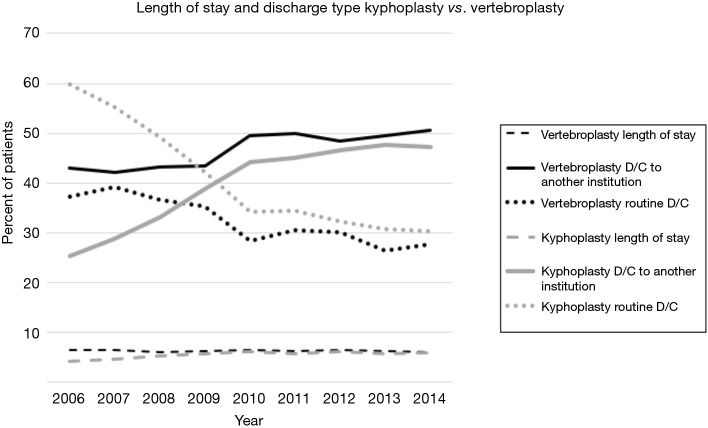
Vertebroplasty patients had a longer LOS and a higher rate of discharges to another institution, defined as discharge to a nursing home or rehabilitation facility. The mean LOS for vertebroplasty over the 9-year period was 6.3 days (SD: 0.15; range: 6.1 to 6.5 days), while mean LOS for kyphoplasty was 5.5 days (SD: 0.68; range: 4.2 to 6.1 days; P=0.0031) (Figure 2). The mean percentage of patients with discharge to another facility after vertebroplasty was 46.6% (SE: 1.2; range: 42.1% to 50.5%) compared to 39.6% after kyphoplasty (SE: 2.8; range: 25.4% to 47.6%; P=0.0365). While LOS has been relatively stable, discharge to another institution increased over the 9-year period in both vertebroplasty and kyphoplasty groups (Figure 2).
Figure 2.
Length of stay and type of discharge were plotted for both vertebroplasty and kyphoplasty from 2006–2014. Length of stay remained relatively stable at 6.3 days for vertebroplasty and at 5.5 days for kyphoplasty. Discharge to another institution increased over the 9-year period after both vertebroplasty and kyphoplasty and differed significantly between the two procedures (P=0.0365).
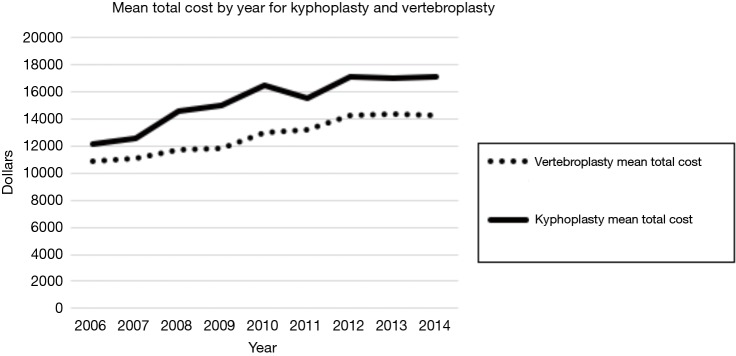
The mean total hospital cost for both vertebroplasty and kyphoplasty increased over the 9-year period from 2006 to 2014 (Figure 3). The mean total cost of vertebroplasty increased from $10,897 per case in 2006 to $14,114 per case in 2014 (mean: $12,747; SE: $464; range: $10,897 to $14,404). The mean total cost of kyphoplasty increased from $12,184 per case in 2006 to $17,174 per case in 2014 (mean: $15,295; SE: $638; range: $12,184 to $17,174).
Figure 3.
Mean total cost per year was plotted for both vertebroplasty and kyphoplasty from 2006–2014. Mean total cost increased for both procedures over the 9-year procedure, from $10,897 per case in 2006 to $14,114 per case in 2014 for vertebroplasty, and from $12,184 per case in 2006 to $17,174 per case in 2014 for kyphoplasty.
The aggregate national charges (“The National Bill”) for vertebroplasty increased from 2006 to 2008 and decreased from 2008 to 2014, totaling $3,378,378,418 (mean: $375,375,380; SE: $20,846,686; range: $331,711,173 to $488,299,608). The aggregate national charges for kyphoplasty over the same 9-year period fluctuated, but totaled $8,849,590,697 (mean: $983,287,855; SE: $68,345,099; range: $804,921,243 to $1,372,915,605). After initially increasing to $154,301,736 in 2008, the aggregate national cost for vertebroplasty decreased 43% to $87,710,069 in 2014. The total aggregate national costs for vertebroplasty totaled $1,019,443,490 (mean: $113,271,499; SE: $7,941,765; range: $87,374,974 to $154,301,736). Total aggregate national costs for kyphoplasty fluctuated similarly to the aggregate national charges and totaled $2,555,095,658 (mean: $283,899,518; SE: $13,300,787; range $221,337,683 to $334,029,287).
The majority of patients undergoing vertebroplasty and kyphoplasty procedures were between the ages of 65–84 (54%) and older than 85 years (33%). Female patients accounted for 73% of both vertebroplasty and kyphoplasty procedures, while male patients accounted for approximately 27%. Medicare accounted for 83% of payer types for both vertebroplasty and kyphoplasty, and 75% of procedures were performed in areas designated as “not low income”. In the South Atlantic region, vertebroplasty and kyphoplasty were performed at rates of 24% and 28%, respectively, far more than any other region. Urban teaching hospitals accounted for 67% of vertebroplasty cases and 60% of kyphoplasty cases.
Discussion
The decreased functional status and severe back pain refractory to conservative management associated with some VCFs has led to the development surgical approaches such as vertebroplasty and kyphoplasty. Despite the differing approaches, the goals behind both treatment modalities are similar: alleviation of pain and prevention of further deformity (10,20). The purpose of the current study was to determine the trends in utilization and cost of these vertebral augmentation procedures over the recent decade.
The data from this study is consistent with previously published studies. Following the publication in 2009 of the two RCTs questioning the efficacy of vertebroplasty, a decline in both vertebroplasty and kyphoplasty procedures was observed. Sayari and colleagues demonstrated a 94.5% decrease in vertebral augmentation procedures performed in the Medicare dataset alone (20). Soon after the RCTs in 2009, results of the VERTOS II trial were published in 2010, demonstrating vertebroplasty as more effective than conservative therapy treatment of refractory pain following vertebral osteoporotic fractures (21). Despite these positive results, utilization of vertebroplasty procedures continued to decrease. Our analysis showed a 53% decrease in the use of vertebroplasty from its peak in 2008.
The decline in utilization of vertebral augmentation procedures was sustained until 2014 for vertebroplasty but interestingly changed direction from 2011 to 2014 for kyphoplasty (Figure 1). The emerging increase in kyphoplasty procedures may be the result of a majority of procedures performed by radiologists since 2012 (22). Though the efficacy of vertebroplasty was questioned in the 2009 studies in the New England Journal of Medicine, a study published in The Lancet in 2009 demonstrated the efficacy of kyphoplasty in alleviating pain in cancer patients with VCFs (23). As a result of these reports in the literature, physicians have gravitated towards kyphoplasty as the surgical treatment of choice for VCFs in recent years. Interestingly, a recent meta-analysis of trials between 2005 and 2014 failed to report significant difference between kyphoplasty and vertebroplasty (24).
The recent increase in kyphoplasty procedures is especially important when considering that kyphoplasty costs more than vertebroplasty. The average cost for a vertebroplasty from 2006–2014 was $12,747 while the average cost for a kyphoplasty in the same time period was $15,295 (Figure 3). In addition, an increased frequency of discharge to other institutions was observed following both types of vertebral augmentation procedures (Figure 2), a trend that will only increase the overall cost burden of these procedures. Though the aggregate national charges for vertebroplasty decreased from 2008–2014 to a total of $331,711,173 in 2014, charges for kyphoplasty increased from 2011–2014 to a total of $1,372,915,605 in 2014. With the observed increase in cost of vertebral augmentation procedures, as well as the increase in utilization of kyphoplasty in recent years, the most cost-effective approach to surgical fracture management in these patients must be defined.
Many of the limitations of this study are due to the intrinsic limitations of large patient databases. The NIS database does not include physician-based fees and costs are calculated from hospital specific cost-to-charge ratios, which may exaggerate surgical cases. Still, these hospital specific cost-to-charge ratios have been internally validated by the Agency for Healthcare Research and Quality. Inherent to a large study, the surgeries were performed by a large variety of surgeons, allowing for differences in surgical technique and potential indication bias. Furthermore, there can be potential inaccuracies of ICD-9 CM billing records, errors transferring data from hospital records to administrative records, underreporting of procedures, or exclusion of missing cases in the NIS database.
Conclusions
Vertebral augmentation procedures continue to be vital surgical procedures for alleviating refractory pain in patients with VCFs. In this analysis of the NIS database, both kyphoplasty and vertebroplasty utilization have declined after the publication of highly regarded trials in 2009 failing to demonstrate efficacy of vertebroplasty procedures for pain relief in VCFs. Since 2011, kyphoplasty procedures have experienced an emerging increase in utilization. Our findings corroborate the trend of kyphoplasty and vertebroplasty in the current literature, which may be a direct consequence of the results of the 2009 trials and increasing radiologist involvement in these procedures. Further prospective randomized trials are necessary to more rigorously evaluate the long-term outcomes and cost-effectiveness of kyphoplasty versus vertebroplasty from a national healthcare perspective.
Acknowledgements
None.
Ethical Statement: The study was approved by the institutional review board (IRB) at Columbia University Medical Center.
Footnotes
Conflicts of Interest: SC Ludwig, MD reports the following disclosures—AO Spine North America Spine Fellowship Support (Research support); ASIP, ISD (Stock or stock options); Cervical Spine Research Society (Board or committee member); DePuy, A Johnson & Johnson Company (IP royalties; Paid consultant; Paid presenter or speaker); Globus Medical (Paid consultant; Research support); Journal of Spinal Disorders and Techniques, The Spine Journal, Contemporary Spine Surgery (Editorial or governing board); K2Medical (Paid consultant, Research support); Synthes (Paid consultant; Paid presenter or speaker); Thieme, QMP (Publishing royalties, financial or material support). LG Lenke, MD reports the following disclosures—Board Membership in OREF and GSO; Personal fees from Consultancy-DePuy Synthes Spine, K2M, and Medtronic; Personal fees from Expert Testimony-Fox Rothschild, LLP; Grants from AO Spine, Scoliosis Research Society, DePuy Synthes Spine, Setting Scoliosis Straight Foundation, EOS; Royalties from Patents-Medtronic; Personal fees from Travel accommodations/meeting expenses-AOSpine, Broadwater, Seattle Science Foundation, Scoliosis Research Society, The Spinl Research Foundation; Other grants from Fellowship Grant-AOSpine, North America, and grants from Philanthropic research funding outside the submitted work. RA Lehman, MD reports the following disclosures—Grants from PRORP (Department of Defense Peer Reviewed Orthopaedic Research Program); Personal fees and non-financial support from DePuy Synthes Spine; Personal fees and non-financial support from Stryker; Personal fees and non-financial support from Medtronic. The other authors have no conflicts of interest to declare.
References
- 1.Felsenberg D, Silman AJ, Lunt M, et al. Incidence of vertebral fracture in Europe: results from the European Prospective Osteoporosis Study (EPOS). J Bone Miner Res 2002;17:716-24. [DOI] [PubMed] [Google Scholar]
- 2.Ensrud KE, Schousboe JT. Clinical practice. Vertebral fractures. N Engl J Med 2011;364:1634-42. [DOI] [PubMed] [Google Scholar]
- 3.Robinson Y, Olerud C. Vertebroplasty and kyphoplasty--a systematic review of cement augmentation techniques for osteoporotic vertebral compression fractures compared to standard medical therapy. Maturitas 2012;72:42-9. [DOI] [PubMed] [Google Scholar]
- 4.Venmans A, Klazen CA, Lohle PN, et al. Natural history of pain in patients with conservatively treated osteoporotic vertebral compression fractures: results from VERTOS II. AJNR Am J Neuroradiol 2012;33:519-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Galibert P, Deramond H, Rosat P, et al. Preliminary note on the treatment of vertebral angioma by percutaneous acrylic vertebroplasty. Neurochirurgie 1987;33:166-8. [PubMed] [Google Scholar]
- 6.Phillips FM, Wetzel TF, Lieberman I, et al. An in vivo comparison of the potential for extravertebral cement leak after vertebroplasty and kyphoplasty. Spine 2002;27:2173-8. [DOI] [PubMed] [Google Scholar]
- 7.Cho DY, Lee W, Sheu A. Treatment of thoracolumbar burst fractures with polymethylmethacrylate vertebroplasty and short-segment pedicle screw fixation. Neurosurgery 2003;53:1354-60. [DOI] [PubMed] [Google Scholar]
- 8.Schmidt R, Cakir B, Mattes T, et al. Cement leakage during vertebroplasty: an underestimated problem. Eur Spine J 2005;14:466-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Patel AA, Vaccaro AR, Martyak GG, et al. Neurologic deficit following percutaneous vertebral stabilization. Spine 2007;32:1728-34. [DOI] [PubMed] [Google Scholar]
- 10.Theodorou DJ, Theodorou SJ, Duncan TD, et al. Percutaneous balloon kyphoplasty for the correction of spinal deformity in painful vertebral body compression fractures. Clin Imaging 2002;26:1. [DOI] [PubMed] [Google Scholar]
- 11.Garfin SR, Yuan H, Reiley M. New technologies in spine: kyphoplasty and vertebroplasty for the treatment of painful osteoporotic compression fractures. Spine 2001;26:1511-5. [DOI] [PubMed] [Google Scholar]
- 12.Barr JD, Barr M, Lemley T, et al. Percutaneous vertebroplasty for pain relief and spinal stabilization. Spine 2000;25:923-8. [DOI] [PubMed] [Google Scholar]
- 13.Zoarski GH, Snow P, Olan W, et al. Percutaneous vertebroplasty for osteoporotic compression fractures: quantitative prospective evaluation of long-term outcomes. J Vasc Interv Radiol 2002;13:139-48. [DOI] [PubMed] [Google Scholar]
- 14.Buchbinder R, Osborne RH, Ebeling PR, et al. A randomized trial of vertebroplasty for painful osteoporotic vertebral fractures. N Engl J Med 2009;361:557-68. [DOI] [PubMed] [Google Scholar]
- 15.Kallmes DF, Comstock BA, Heagerty PJ, et al. A randomized trial of vertebroplasty for osteoporotic spinal fractures. N Engl J Med 2009;361:569-79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Miller FG, Kallmes DF, Buchbinder R. Vertebroplasty and the placebo response. Radiology 2011;259:621-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wong CC, McGirt MJ. Vertebral compression fractures: a review of current management and multimodal therapy. J Multidiscip Healthc 2013;6:205-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Aebi M. Vertebroplasty: about sense and nonsense of uncontrolled "controlled randomized prospective trials". Eur Spine J 2009;18:1247-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Noonan P. Randomized vertebroplasty trials: bad news or sham news? AJNR Am J Neuroradiol 2009;30:1808-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McCall T, Cole C, Dailey A. Vertebroplasty and kyphoplasty: a comparative review of efficacy and adverse events. Curr Rev Musculoskelet Med 2008;1:17-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Klazen CA, Lohle P, de Vries J, et al. Vertebroplasty versus conservative treatment in acute osteoporotic vertebral compression fractures (VERTOS II): an open-label randomized trial. Lancet 2010;376:1085-92. [DOI] [PubMed] [Google Scholar]
- 22.Cox M, Levin DC, Parker L, et al. Vertebral augmentation after recent randomized controlled trials: a new rise in kyphoplasty volumes. J Am Coll Radiol 2016;13:28-32. [DOI] [PubMed] [Google Scholar]
- 23.Berenson J, Pflugmacher R, Jarzem P, et al. Balloon kyphoplasty versus non-surgical fracture management for treatment of painful vertebral body compression fractures in patients with cancer: a multicentre, randomised controlled trial. Lancet Oncol 2011;12:225-35. [DOI] [PubMed] [Google Scholar]
- 24.Chang X, Lv YF, Chen B, et al. Vertebroplasty versus kyphoplasty in osteoporotic vertebral compression fracture: a meta-analysis of prospective comparative studies. Int Orthop 2015;39:491-500. [DOI] [PubMed] [Google Scholar]