Introduction
The cervicothoracic junction (CTJ) is defined as the area extending from vertebral segments C7 to T4. Because most pathological processes occur in the anterior segment of the vertebrae, the anterior approach is usually the best surgical option, allowing neural decompression, stabilization and restoration of anatomical spinal alignment. Nevertheless, it represents a big challenge for the spinal surgeon for the presence of important anatomical structures of the upper mediastinum: manubrium, thymus gland, left and right brachiocephalic veins (or innominate veins), right brachiocephalic artery, left common carotid artery, aortic arc, esophagus, trachea and thoracic duct. Varied approaches to the CTJ have been described in literature [low lateral anterior cervical approach (LACA), full sternotomy, lateral parascapular thoracotomy, clavicular dissection]. Among them, the low LACA combined with manubriotomy is the most used and safe (1).
Surgical indications
LACA combined with manubriotomy can be used for pathological processes occurring in the anterior segment of the CTJ: cervico-thoracic disc disease, vertebral osteomyelitis or discitis, fractures and tumors. To establish the need of a manubriotomy, the most recently published guidelines can be used. We can discern guidelines based on magnetic resonance imaging (MRI) scans and computer tomography (CT) scans:
MRI scan guidelines: based on T2 sagittal MR imaging at the midline including sternal manubrium. According to Teng guidelines (2), a line is drawn that starts from the suprasternal notch and extends horizontally to the corresponding anterior border of the vertebrae at the CTJ; another line that also starts from the suprasternal notch and extends posterosuperiorly to the midpoint of the anterior border of the C7/T1 intervertebral disc is drawn subsequently. The angle that meets at the suprasternal notch (SSN) is specified as the cervicothoracic angle (CTA). If the lesion is located above CTA (Type A), only LACA can be used. If the lesion is located within the CTA (Type B), LACA with manubriotomy can be used (Figure 1);
CT scan guidelines: based on sagittal CT scan reconstruction at the midline including the sternal manubrium. According to Karikari guidelines (3), the lowest accessible disc space that can be approached with LACA alone is determined by constructing a straight line passing through and parallel to the disc space that also passes above the manubrium (the intervertebral disc line). If the lesion is above this line, the manubriotomy is necessary (Figure 2). According to Falavigna guidelines (4), the superior healthy vertebrae are the first normal ones above the diseased levels in corpectomy cases, or the vertebra above the herniated intervertebral disc in microdiscectomy cases. The so-called "surgeons’ view line" is defined as a line parallel to the inferior plateau of the superior healthy vertebrae and its correlation with the manubrium. If the surgeons’ view line crosses below the manubrium, the manubriotomy is necessary.
Figure 1.
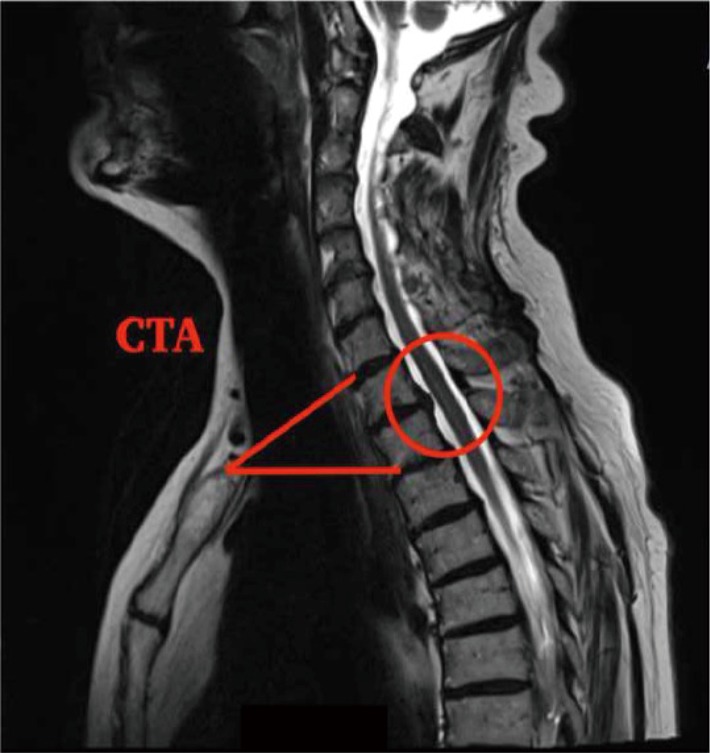
Sagittal T2 MRI scan showing the cervico-thoracic angle according to Teng Guidelines. CTA, cervicothoracic angle; MRI, magnetic resonance imaging.
Figure 2.
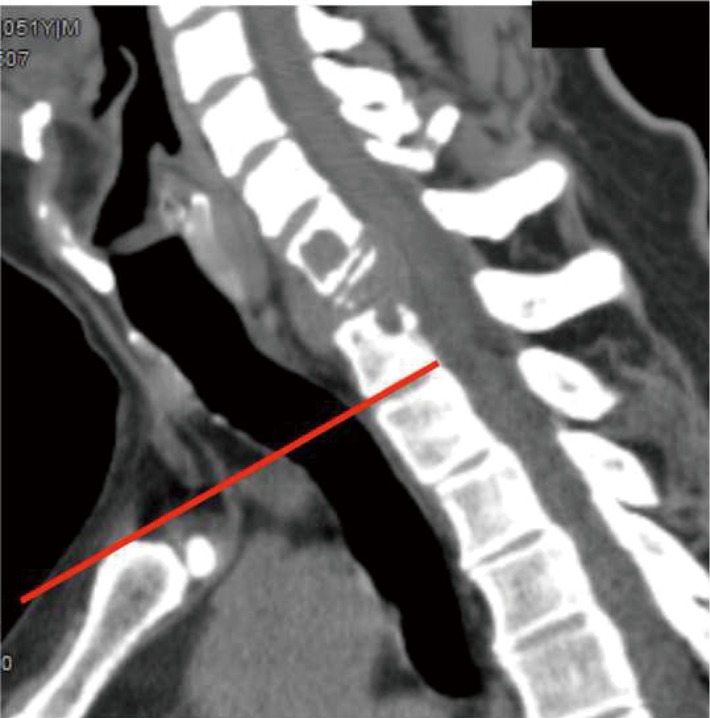
The lowest accessible space according to Karikari Guidelines.
Patient positioning and setup
Before surgery, careful assessment of pulmonary and cardiac function is needed: clinical evaluation, pulmonary function tests including diffusing capacity of the lung for carbon monoxide (DLCO) and blood gas analysis. The patient is positioned supine, the trunk 10° flexed and the head slightly rotated to the right. A roll pad can be placed under the shoulders to extend the cervical spine. Intraoperative monitoring must be used in all the cases.
Step-by-step instructions for the procedure
An incision is made on the left side along the anterior border of the sternocleidomastoid muscle and continued down the midline over the manubrium. The neck dissection is completed first. The sternomastoid, sternohyoid and sternothyroid muscles are sectioned. Then, manubriotomy is performed. A sternal saw is used to make a linear manubriotomy ending at the sternal angle to preserve the sternoclavicular joints, and a sternal retractor is applied. Dissection proceeds with thymus gland resection. The left anonymous vein and the brachiocephalic artery are isolated and gently right-downward retracted using vascular loops. An anterior cervical fusion retractor is positioned allowing exposure of the lower cervical region to the upper thoracic spine. Microdiscectomy, single or multiple corpectomies, tumor resection can be performed. At the end, reconstruction with cages and anterior plating can be assessed with anteroposterior and lateral X-ray scan. A suction drain is left in the prevertebral space and substernal plane. The manubrium is reapproximated with flexible steel wires and the suture completed (Figure 3) (5).
Figure 3.

Step by step instructions for the manubriotomy (5). Available online: http://www.asvide.com/articles/1748
Postoperative management
In the post-operative period intensive care is not routinely recommended.
Effective analgesia is an essential part of postoperative management. Important injectable drugs for pain are the opiate analgesics in the first 2 days. Nonsteroidal anti-inflammatory drugs (NSAIDs), such as diclofenac (1 mg/kg) and ibuprofen can also be given orally as can paracetamol (15 mg/kg) for the next 7–10 days.
Infections prophylaxis consisting in 3 g Amoxicillin for 7 days is recommended in all cases. Low molecular-weight heparin and compression stockings for thrombo-embolic prophylaxis are mandatory until the complete mobilization of the patient.
The patient usually starts the mobilization on the 3rd postoperative day. The surgical drain can be removed after 48–72 hours. A cervical orthosis such as a Philadelphia collar must be used for 3 months. X-ray scan after the mobilization of the patient is recommended.
Complications
Dysphagia and dysphonia are the most common complications and are usually transient conditions. They can begin in the immediate postoperative period. Dysphagia can be treated protecting the airway with postural adjustments to reduce risk of aspiration, doing exercises to strengthen weak facial muscles, to improve range of oral or pharyngeal structural movement, and/or to improve coordination (6).
Infections may include skin infections, spondylodiscitis and osteomyelitis. Sternal osteomyelitis and mediastinal infection following manubriotomy may be effectively managed through rigorous debridement of infected soft tissues, resection of the damaged sternal segment and adequate postoperative drainage (7).
Pearls and pitfalls
The LACA combined with manubriotomy allows extensile exposure of the CTJ and is associated to a low rate of complications. Age and body mass index are major determinants of accessibility (8), followed by neck shape (long neck vs short neck). In most of cases this approach allows a complete access from C3 to T3. The exposure of T4 in many cases is less adequate because the space is narrow and deep. For T4–T5 level is generally recommended a right thoracotomy (9). A left side approach is preferred to minimize the risks of recurrent nerve injury. The recurrent laryngeal nerve on the left side has a longer route and has a relatively fixed anatomy in the tracheo-esophageal groove while on the right side it presents substantial anatomical variations.
Acknowledgements
None.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.Tarantino R, Donnarumma P, Marruzzo D, et al. Anterior surgical approaches to the cervicothoracic junction: when to use the manubriotomy? Spine J 2013;13:1064-8. 10.1016/j.spinee.2013.02.049 [DOI] [PubMed] [Google Scholar]
- 2.Teng H, Hsiang J, Wu C, et al. Surgery in the cervicothoracic junction with an anterior low suprasternal approach alone or combined with manubriotomy and sternotomy: an approach selection method based on the cervicothoracic angle. J Neurosurg Spine 2009;10:531-42. 10.3171/2009.2.SPINE08372 [DOI] [PubMed] [Google Scholar]
- 3.Karikari IO, Powers CJ, Isaacs RE. Simple method for determining the need for sternotomy/manubriotomy with the anterior approach to the cervicothoracic junction. Neurosurgery 2009;65:E165-6; discussion E166. [DOI] [PubMed]
- 4.Falavigna A, Righesso O, Teles AR. Anterior approach to the cervicothoracic junction: proposed indication for manubriotomy based on preoperative computed tomography findings. J Neurosurg Spine 2011;15:38-47. 10.3171/2011.3.SPINE10342 [DOI] [PubMed] [Google Scholar]
- 5.Donnarumma P, Nigro L, Tarantino R, et al. Step by step instructions for the manubriotomy. Asvide 2017;4:432. Available online: http://www.asvide.com/articles/1748
- 6.Joaquim AF, Murar J, Savage JW, et al. Dysphagia after anterior cervical spine surgery: a systematic review of potential preventative measures. Spine J 2014;14:2246-60. 10.1016/j.spinee.2014.03.030 [DOI] [PubMed] [Google Scholar]
- 7.Gao J, Wang YL, Lu SQ, et al. Management of sternal osteomyelitis and mediastinal infection following median sternotomy. Chin Med J (Engl) 2010;123:2803-6. [PubMed] [Google Scholar]
- 8.Mai HT, Mitchell SM, Jenkins TJ, et al. Accessibility of the Cervicothoracic Junction Through an Anterior Approach: An MRI-based Algorithm. Spine (Phila Pa 1976) 2016;41:69-73. 10.1097/BRS.0000000000001155 [DOI] [PubMed] [Google Scholar]
- 9.De Giacomo T, Francioni F, Diso D, et al. Anterior approach to the thoracic spine. Interact Cardiovasc Thorac Surg 2011;12:692-5. 10.1510/icvts.2010.257360 [DOI] [PubMed] [Google Scholar]


