Abstract
Background
Isthmic spondylolysis (ISY) is a common cause of back pain in the pediatric population. Historically, non-operative treatments have had a very high success rate. The purpose of this study was to review the mid-term results of an indirect pars repair technique on reducing the visual analog score for pain (VAS), spondylolysis defect healing, complication rates and rates of return to pre-surgery activity level in pediatric patients who failed conservative care for ISY.
Methods
A retrospective review of all pediatric patients (<18 years old) treated surgically by one surgeon over a 5-year period was performed. Patients were treated with indirect pars repair utilizing pedicle screws and laminar hooks and local autograft. Preoperative VAS was compared to the final follow-up score, and return to activity was evaluated. Radiographs were reviewed to evaluate healing.
Results
Nine patients (6 females, 3 males) were treated surgically. Average age at the time of surgery was 15.4 years, (range, 13 to 17 years). Average length of final follow-up was 11.9 months (range, 6 to 24 months). Preoperative VAS averaged 5.6 points (range, 2 to 8 points) compared to final follow-up of 1.2 (range, 0 to 3). Definitive bony healing was noted in 7 of 9 cases (77.8%) with at least 6 months follow-up. Eight of nine patients (88.9%) returned to preoperative competitive sports activity level. No complications were noted during the follow-up period.
Conclusions
Pediatric patients treated surgically with indirect pars repair appear to achieve satisfactory mid-term outcomes. This technique appears safe, and has both a high healing rate and return to competitive athletics. Further study is needed to determine durability of this procedure.
Keywords: Pediatric, spondylolysis, spondylolisthesis, indirect repair, surgery, treatment
Introduction
Isthmic spondylolysis (ISY) has a prevalence of 6% in the general population with new research suggesting a rate as high as 11.5% (1,2). This condition is a common cause of back pain in the pediatric population. Historically, non-operative treatments have had a very high success rate (3-5). Pain that is not manageable with conservative treatment, however, presents a dilemma for spine surgeons. Many surgical options exist, including techniques for direct or indirect pars interarticularis repair, as well as spinal segment fusion. The purpose of our study was to review the mid-term results of an indirect pars repair on the visual analog score for pain (VAS) level, isthmic pars defect healing, surgical complication rates and the rates of return to sporting activity following surgery.
Methods
Institutional Review Board (IRB) approval was granted for our study (IRB # 16-728). A retrospective review of all pediatric patients (<18 years old) surgically treated for spondylolysis with or without low-grade spondylolisthesis, was performed. Surgeries were performed by one fellowship-trained pediatric orthopaedic surgeon (senior author RC Goodwin) and occurred between 2010 and 2015. This included a total of nine patients. Patients had failed at least 1 year of conservative treatment, including oral analgesics, physical therapy and activity modification prior to surgery. Gender, age at the time of surgery, sports participation and VAS levels were recorded. Patients were treated with an indirect pars repair utilizing pedicle screw instrumentation with laminar compression hook constructs and local spinous process autograft. At the time of surgery, a high-speed burr was used to decorticate the fibrous pars defect, the local spinous process autograft was placed into the defect area and laminar hooks in compression were applied (Figure 1). Post-operatively, patients were restricted from bending, lifting more than 10 pounds, twisting, or sports activities for 3 months. After this time, patients slowly returned to exercise activities, with full return to activities at 5 to 6 months after surgery.
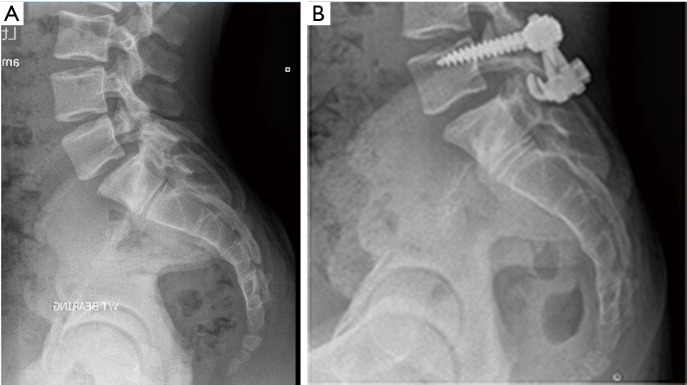
Figure 1.
Indirect pars repair. (A) A preoperative lateral radiograph of a 15-year-old male patient (patient #3) with a transitional L5 spondylolysis with low-grade listhesis; (B) a 6-month follow-up lateral radiograph in the same patient following indirect pars repair with healing of the lysis and decrease in listhesis.
The VAS difference at final follow-up was calculated. A two-tailed t-test was performed on the VAS score reduction to determine statistical significance. Preoperative and final post-operative radiographs were reviewed to evaluate healing. All authors with varying degrees of surgical experience (2 residents, 1 fellow, 1 attending) reviewed final anterior posterior and lateral radiographs on three separate occasions. Overall interrater agreement (kappa) was determined between the four reviewers’ responses. Complications that occurred during the treatment process were reviewed and recorded. Return to sport participation was determined at the final follow-up visit.
Results
Nine patients (6 females, 3 males) were treated surgically after failing conservative treatment. Cases included 6 bilateral L5 spondylolysis, 1 left L5 spondylolysis and 2 bilateral L4 spondylolysis. Two of the bilateral L5 cases exhibited low-grade spondylolisthesis (Figure 1). Average age at the time of surgery was 15.4 years, (range, 13–17 years). Average length of final follow-up was 11.9 months (range, 6–24 months). Preoperative VAS averaged 5.6 points (range, 2–8 points) and post-operative VAS averaged 1.2 (range, 0–3 points). The VAS was reduced on average by 4.4 points (range, 0–8 points), but this did not achieve statistical significance (P=0.99). Definitive bony healing was noted in 7 of 9 cases (77.8%) with at least 6 months follow-up line (Table 1). There was disagreement between raters in determining bony healing in one case. Overall agreement between raters was very high at 0.93 (6). Eight of nine patients (88.9%) returned to preoperative competitive sport activity level. No complications were noted during the study period, including infection, instrumentation failure, or neurological injury.
Table 1. Patient characteristics and outcomes.
| Case | Gender | Age at surgery (years) | Length of follow-up (months) | Levels involved (bilateral) | Pre-VAS | Post-VAS | Healed? | Sport | Return to sport? |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Female | 17 | 12 | L5 | 6 | 0 | Yes | Dance | Yes |
| 2 | Male | 15 | 8 | Left L5 | 7 | 2 | Yes | Football | No** |
| 3 | Male | 15 | 12 | L5 | 3 | 0 | Yes | Wrestling | Yes |
| 4 | Female | 17 | 12 | L5 | 3 | 3 | No | Gymnastics | Yes |
| 5 | Female | 17 | 24 | L4 | 8 | 0 | Yes | Dance | Yes |
| 6 | Female | 15 | 6 | L5 | 8 | 3 | Yes | Softball | Yes |
| 7 | Female | 13 | 6 | L5 | 8 | 3 | Yes | Dance | Yes |
| 8 | Female | 15 | 6 | L5 | 5 | 0 | No* | Track | Yes |
| 9 | Male | 15 | 21 | L4 | 2 | 0 | Yes | Basketball | Yes |
| Avg or total | 6 female; 3 male | 15.4 | 11.9 | 7 L5; 2 L4 | 5.6 | 1.2 | 7 yes; 2 no | 8 yes; 1 no |
*, 50% disagreement between raters; **, returned to non-collision sport only. Avg, average; VAS, visual analog score for pain.
Discussion
ISY has a relatively high prevalence and is a common cause of back pain in pediatric patients. According to Klein et al., a meta-analysis revealed that nearly 84% of patients did well by 1 year following conservative treatment (3). For those that continue to have pain and functional limitations, many surgical options have been developed. Pars repair techniques have been used in an attempt to spare spinal motion segments and minimize fusing the spine. These techniques include direct pars repair with cortical screws, indirect pars repair with posterior wiring, or a combination of pedicle screw instrumentation and some type of instrumentation to apply compression (laminar hooks, wiring, among others) (5,7-20). In adult cases or older pediatric patients with significant degenerative disc disease or high-grade spondylolisthesis, fusion techniques have been recommended (18,21-23).
Traditional direct screw fixation across the defect was popularized by Buck in 1970 (8). Various posterior wiring techniques have been popular as well, including Scott’s wiring and other modifications of this technique (24,25). Tokuhashi and Matsuzak described pedicle screw instrumentation with laminar compression hooks (11). Prior to this, Morscher et al. described placing lateral mass screws and using laminar compression hooks (10). Modern instrumentation and techniques have changed, but the principle remains the same: create a biologic and mechanical environment to limit motion at the defect and promote healing.
Deguchi et al. studied spinal motion in cadaveric models with various pars repair and fixation techniques (14). Techniques included Bucks fixation, Scott’s wiring, modified Scott’s wiring and a pedicle-screw-rod-hook construct. The screw-rod-hook construct allowed the least amount of motion across the defect during flexion. Fan et al. studied the biomechanics of the Texas Scottish Rite Hospital (TSRH) hook screw and screw-rod fixation methods and found these to provide more rigidity during rotation than either Scott’s or Buck’s technique (17). Westacott et al. performed a systematic review of the literature which revealed little clinical difference between pars repair or fusion techniques (26). One comparative study demonstrated improved long-term outcomes with fusion.
Several authors have published recent case series results on pars repairs. Dai et al. described a 93% good or excellent result after direct repair with or without facet fusion for 46 patients (13). Patients with disc disease noted on MRI underwent simultaneous facet fusion with the direct pars repair in the study. de Bodman et al. described restoration of spine stability and a decrease in the Oswestry Disability Index (ODI) in 35 patients treated with a modified-Buck direct repair technique with a mean follow-up of 10 years (9). Chung et al. reported favorable 2-year results and high bony healing rates on 6 patients with indirect pars repairs for multilevel spondylolysis (18). Roca et al. reported results on 19 patients with indirect pars repair and found that patients younger than age 20 had a 92% defect healing rate and better outcomes than those older than age 20 (16). Snyder et al. reported defect healing results of nearly 90% on 16 patients with a median age of 16 years (27). Patients were treated with Buck’s direct repair and recombinant human bone morphogenetic protein (rhBMP-2) regardless of age or gender, as well as bracing, with all athletes returning to play by final follow-up. Deguchi et al. studied the long-term results of 52 patients treated with 1 of 3 different pars repair techniques, including Scotts’s, modified Scott’s, or Buck’s technique (14). The authors found the best outcomes with the modified Scott’s technique. Karatas et al. studied 16 patients that were divided between undergoing either direct screw repair or indirect repair with pedicle screw and laminar hook repair (28). The authors quote a 100% healing rate in both groups by 6 months after surgery, and excellent or good results in 88% of patients, feeling that either repair technique is acceptable.
Our study reviewed the results of indirect pars repair with pedicle screw fixation and laminar compression hooks in a pediatric population only. The technique in our series utilized a simple and familiar midline approach, modern spine instrumentation and locally harvested spinous process autograft. We did see a consistent reduction in VAS following surgery, and a high rate of both the defect healing and return to sports by 6 months after surgery. This was true for the 2 patients (patient #3 & #7) that demonstrated low-grade listhesis, with a 3-point and 5-point reduction in VAS respectively. One patient who was unable to return to the collision sport of football (patient #2) was able to return to basketball at a competitive level. To our knowledge, no patients have required any further surgical interventions.
There are several limitations to our study, including the retrospective nature of this case series. Although there was a high rate of agreement between raters, no advanced imaging was used to determine true boney defect healing. The follow-up period is also brief, averaging just under 11 months. Longer-term study will is needed to judge the durability or success of this procedure with time.
Conclusions
Pediatric patients treated surgically with the indirect pars repair technique described, appear to achieve satisfactory mid-term results. A high percentage of patients returned to a competitive sporting activity level and had defect healing on follow-up radiographs. This technique appears safe with no complications observed in this case series. Further study and longer-term follow-up within this group is needed to determine the surgical durability of this procedure.
Acknowledgements
None.
Ethical Statement: Cleveland Clinic Institutional Review Board (IRB) approval of was granted for our study (IRB # 16-728).
Footnotes
Conflicts of Interest: RC Goodwin paid consultant for Stryker. The other authors have no conflicts of interest to declare.
References
- 1.Fredrickson BE, Baker D, McHolick WJ, et al. The natural history of spondylolysis and spondylolisthesis. J Bone Joint Surg Am 1984;66:699-707. 10.2106/00004623-198466050-00008 [DOI] [PubMed] [Google Scholar]
- 2.Kalichman L, Kim DH, Li L, et al. Spondylolysis and spondylolisthesis: prevalence and association with low back pain in the adult community-based population. Spine (Phila Pa 1976) 2009;34:199-205. 10.1097/BRS.0b013e31818edcfd [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Klein G, Mehlman CT, McCarty M. Nonoperative treatment of spondylolysis and grade I spondylolisthesis in children and young adults: a meta-analysis of observational studies. J Pediatr Orthop 2009;29:146-56. 10.1097/BPO.0b013e3181977fc5 [DOI] [PubMed] [Google Scholar]
- 4.Beutler WJ, Fredrickson BE, Murtland A, et al. D. The natural history of spondylolysis and spondylolisthesis: 45-year follow-up evaluation. Spine (Phila Pa 1976) 2003;28:1027-35; discussion 1035. 10.1097/01.BRS.0000061992.98108.A0 [DOI] [PubMed] [Google Scholar]
- 5.Bouras T, Korovessis P. Management of spondylolysis and low-grade spondylolisthesis in fine athletes. A comprehensive review. Eur J Orthop Surg Traumatol 2015;25 Suppl 1:S167-75. 10.1007/s00590-014-1560-7 [DOI] [PubMed] [Google Scholar]
- 6.Randolph JJ. Online Kappa Calculator. 2008; Available online: http://justusrandolph.net/kappa/, accessed 06/03, 2016.
- 7.Kimura M. My method of filing the lesion with spongy bone in spondylolysis and spondylolistesis. Seikei Geka 1968;19:285-96. [PubMed] [Google Scholar]
- 8.Buck JE. Direct repair of the defect in spondylolisthesis. Preliminary report. J Bone Joint Surg Br 1970;52:432-7. [PubMed] [Google Scholar]
- 9.de Bodman C, Bergerault F, de Courtivron B, et al. Lumbo-sacral motion conserved after isthmic reconstruction: long-term results. J Child Orthop 2014;8:97-103. 10.1007/s11832-014-0560-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Morscher E, Gerber B, Fasel J. Surgical treatment of spondylolisthesis by bone grafting and direct stabilization of spondylolysis by means of a hook screw. Arch Orthop Trauma Surg 1984;103:175-8. 10.1007/BF00435550 [DOI] [PubMed] [Google Scholar]
- 11.Tokuhashi Y, Matsuzaki H. Repair of defects in spondylolysis by segmental pedicular screw hook fixation. A preliminary report. Spine (Phila Pa 1976) 1996;21:2041-5. 10.1097/00007632-199609010-00023 [DOI] [PubMed] [Google Scholar]
- 12.Kakiuchi M. Repair of the defect in spondylolysis. Durable fixation with pedicle screws and laminar hooks. J Bone Joint Surg Am 1997;79:818-25. 10.2106/00004623-199706000-00003 [DOI] [PubMed] [Google Scholar]
- 13.Dai LY, Jia LS, Yuan W, et al. Direct repair of defect in lumbar spondylolysis and mild isthmic spondylolisthesis by bone grafting, with or without facet joint fusion. Eur Spine J 2001;10:78-83. 10.1007/s005860000205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Deguchi M, Rapoff AJ, Zdeblick TA. Biomechanical comparison of spondylolysis fixation techniques. Spine (Phila Pa 1976) 1999;24:328-33. 10.1097/00007632-199902150-00004 [DOI] [PubMed] [Google Scholar]
- 15.Ulibarri JA, Anderson PA, Escarcega T, et al. Biomechanical and clinical evaluation of a novel technique for surgical repair of spondylolysis in adolescents. Spine (Phila Pa 1976) 2006;31:2067-72. 10.1097/01.brs.0000231777.24270.2b [DOI] [PubMed] [Google Scholar]
- 16.Roca J, Iborra M, Cavanilles-Walker JM, et al. Direct repair of spondylolysis using a new pedicle screw hook fixation: clinical and CT-assessed study: an analysis of 19 patients. J Spinal Disord Tech 2005;18 Suppl:S82-9. 10.1097/01.bsd.0000123425.12852.3c [DOI] [PubMed] [Google Scholar]
- 17.Fan J, Yu GR, Liu F, et al. Direct repair of spondylolysis by TSRH's hook plus screw fixation and bone grafting: biomechanical study and clinical report. Arch Orthop Trauma Surg 2010;130:209-15. 10.1007/s00402-009-0897-6 [DOI] [PubMed] [Google Scholar]
- 18.Chung CH, Chiu HM, Wang SJ, et al. Direct repair of multiple levels lumbar spondylolysis by pedicle screw laminar hook and bone grafting: clinical, CT, and MRI-assessed study. J Spinal Disord Tech 2007;20:399-402. 10.1097/01.bsd.0000211253.67576.90 [DOI] [PubMed] [Google Scholar]
- 19.Hersh DS, Kim YH, Razi A. Multi-level spondylolysis. Bull NYU Hosp Jt Dis 2011;69:339-43. [PubMed] [Google Scholar]
- 20.Liu X, Wang L, Yuan S, et al. Multiple-level lumbar spondylolysis and spondylolisthesis. J Neurosurg Spine 2015;22:283-7. 10.3171/2014.10.SPINE14415 [DOI] [PubMed] [Google Scholar]
- 21.Jones TR, Rao RD. Adult isthmic spondylolisthesis. J Am Acad Orthop Surg 2009;17:609-17. 10.5435/00124635-200910000-00003 [DOI] [PubMed] [Google Scholar]
- 22.Rajaee SS, Bae HW, Kanim LE, et al. Spinal fusion in the United States: analysis of trends from 1998 to 2008. Spine (Phila Pa 1976) 2012;37:67-76. 10.1097/BRS.0b013e31820cccfb [DOI] [PubMed] [Google Scholar]
- 23.Ye YP, Xu H, Chen D. Comparison between posterior lumbar interbody fusion and posterolateral fusion with transpedicular screw fixation for isthmic spondylolithesis: a meta-analysis. Arch Orthop Trauma Surg 2013;133:1649-55. 10.1007/s00402-013-1868-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Johnson GV, Thompson AG. The Scott wiring technique for direct repair of lumbar spondylolysis. J Bone Joint Surg Br 1992;74:426-30. [DOI] [PubMed] [Google Scholar]
- 25.Giudici F, Minoia L, Archetti M, et al. Long-term results of the direct repair of spondylolisthesis. Eur Spine J 2011;20 Suppl 1:S115-20. 10.1007/s00586-011-1759-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Westacott DJ, Cooke SJ. Functional outcome following direct repair or intervertebral fusion for adolescent spondylolysis: a systematic review. J Pediatr Orthop B 2012;21:596-601. 10.1097/BPB.0b013e328355393d [DOI] [PubMed] [Google Scholar]
- 27.Snyder LA, Shufflebarger H, O'Brien MF, et al. Spondylolysis outcomes in adolescents after direct screw repair of the pars interarticularis. J Neurosurg Spine 2014;21:329-33. 10.3171/2014.5.SPINE13772 [DOI] [PubMed] [Google Scholar]
- 28.Karatas AF, Dede O, Atanda AA, et al. Comparison of Direct Pars Repair Techniques of Spondylolysis in Pediatric and Adolescent Patients: Pars Compression Screw versus Pedicle Screw-Rod-Hook. Clin Spine Surg 2016;29:272-80. [DOI] [PubMed] [Google Scholar]