SUMMARY
BACKGROUND
Incarcerated persons are disproportionately diagnosed with tuberculosis (TB). California has the second highest inmate population in the United States, but reports the highest number of cases.
OBJECTIVE
To describe the TB epidemiology among incarcerated patients in California.
METHODS
Trends in incidence were assessed using Poisson regression, and trends in percentage were assessed using weighted linear regression. Demographic and clinical characteristics were compared using χ2 or Mann-Whitney U tests.
RESULTS
During 1993–2013, of the 64 090 TB cases reported, 2323 (4%) were correctional facility residents. Incidence in correctional facilities decreased until 2006 (annual per cent change [APC] –12.3%, 95%CI –14.4 to –10.1), but has since stabilized (APC 4.4%, 95%CI –2.1 to 11.4). Compared with state prisoners, federal prisoners were more likely to be male (98%, P = 0.03), persons arriving in the United States within 5 years of diagnosis (62%, P < 0.001), and born in Mexico (88%, P=0.02), whereas local jail inmates were more likely to have a history of substance use (75%, P < 0.001) and homelessness (35%, P < 0.001).
CONCLUSIONS
TB incidence in correctional facilities had steadily declined over the last two decades, but has recently leveled out. To promote further reduction in incidence among diverse incarcerated populations, health departments and correctional facilities should strengthen collaboration by conducting TB risk-based assessments.
Keywords: tuberculosis, prisons, incidence, epidemiology
MYCOBACTERIUM TUBERCULOSIS is spread through the air from person to person, making congregate settings higher-risk environments for tuberculosis (TB) transmission.1 Transmission of TB disease, and reactivation of tuberculous infection, are of specific concern in correctional facilities, where greater concentrations of persons with risk factors for tuberculous infection and TB disease are housed in potentially poorly ventilated or crowded facilities.2 These risk factors, coupled with frequent movement of inmates into and out of facilities, inadequate infection control or delays in diagnosis and treatment, can increase the risk of transmission in these environments. Incidence rates among correctional populations have been shown to be consistently higher than overall TB rates in the United States, and up to eight times higher than among non-correctional populations.3,4 Several outbreaks in correctional facilities have been reported, some resulting in transmission to the community.5–10
California has the highest number of TB cases and the second largest inmate population of any state in the United States, making correctional facilities critical settings for the detection and treatment of TB.11,12 Using the California Department of Public Health (CDPH) TB Registry, we examined trends in incidence and compared demographic and clinical characteristics among correctional TB cases to assess progress in TB control and identify potential areas for improvement.
METHODS
Data sources
The CDPH collects data on all reported TB cases. State law (California Code of Regulations Title 17 §2500) requires health care providers and laboratories to report cases to local health departments. Health departments submit data on cases using a national surveillance report form that collects information on demographic and clinical characteristics and treatment outcomes. Reported cases are matched to the California Office of AIDS registry to identify those co-infected with the human immunodeficiency virus (HIV). Data on all reported cases during 1993–2013 were analyzed. Trend analysis was conducted for this 21-year period based on the completeness and availability of surveillance data. A 10-year period (2000–2009) was selected for comparison of demographic and clinical characteristics among correctional cases because of changes in surveillance variables in 2009.13
To calculate incidence rate, average daily population (ADP) estimates were obtained for federal prisons from the US Federal Bureau of Prisons (unpublished data, US Federal Bureau of Prisons, August 2014), state prisons from the California Department of Corrections and Rehabilitation, and local jails from the California Board of State and Community Corrections; non-correctional population estimates were obtained from the California Department of Finance.14–16
The Centers for Disease Control and Prevention (Atlanta, GA, USA) determined that this project was not research on human subjects and did not require approval by an institutional review board.
Definitions
Cases of TB and correctional facilities were defined according to US National Tuberculosis Surveillance System definitions.13 A correctional case was defined as a patient who was incarcerated at the time of TB diagnosis. To assess infectiousness, we categorized cases into four mutually exclusive categories: 1) sputum acid-fast bacilli (AFB) smear-positive and culture-positive for M. tuberculosis, 2) sputum AFB smear-negative and culture-positive for M. tuberculosis, 3) clinically diagnosed pulmonary cases with negative sputum AFB smear and culture, and 4) extra-pulmonary cases that did not have clinical or laboratory evidence of pulmonary disease.
For all analyses, comparisons were restricted to adult cases, defined as patients aged ≥15 years. Cases residing in juvenile, other types of correctional facilities at diagnosis, or US Immigration and Customs Enforcement detainees were excluded, as population estimates were not available. Incidence rates in 1993 and 1994 could not be calculated because estimates of local jail populations were not available.
A subanalysis of correctional cases diagnosed during 2010–2013 was also conducted to assess changes in surveillance variables. Beginning in 2010, a new variable identifying patients who moved residence while on treatment was collected: patients who moved were categorized as moving ‘in state’, ‘out of state’, or ‘out of country’. Information on the nucleic acid amplification (NAA) test also became available in 2010. We assessed utilization of the NAA test as an initial diagnostic modality by identifying patients who were sputum smear-negative and had an NAA report date before a positive sputum culture date.
Statistical analysis
Trends in incidence and percentage of cases diagnosed during 1993–2013 were analyzed. Incidence rates for correctional cases per 100 000 inmates were calculated using ADP estimates, and for non-correctional residents by subtracting the sum of the correctional ADP estimates from California population estimates. Trends in incidence were assessed for significance using Poisson regression. Trends in the annual percentage of correctional cases were assessed using linear regression weighted by population size. To examine trends further, we identified joinpoints that best fitted the data using a Monte Carlo permutation test.17 Ninety-five per cent confidence intervals (CIs) for binominal proportions were calculated for incidence rates and for the annual percentage of cases using the Wilson score interval. Bivariate analysis was conducted using the Pearson χ2 test for categorical variables, and the Mann-Whitney U-test for continuous variables; no analysis was performed for categories with fewer than five patients. Reported P values are two sided; P < 0.05 was considered statistically significant. Analyses were conducted using SAS v9.3 (Statistical Analysis System, Cary, NC, USA) and Joinpoint v4.1.1 (National Cancer Institute, Bethesda, MD, USA).
The demographic and clinical characteristics of patients were compared and limited to cases residing in a federal prison, state prison, or local jail during 2000–2009. Cases residing in federal prisons and local jails were compared with cases in state prisons, where the lowest incidence rate was found.
RESULTS
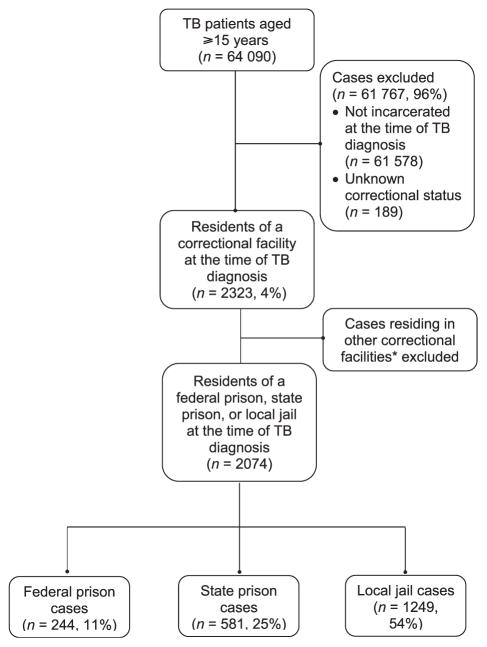
During 1993–2013, 2323 of 64 090 (4%) TB cases were reported in adults incarcerated at diagnosis, 244 (11%) of whom were in federal prisons, 581 (25%) in state prisons, and 1249 (54%) in local jails (Figure 1).
Figure 1.
Classification of TB patients aged ≥15 years who were residents of a correctional facility at the time of diagnosis, California, 1993–2013. *Includes TB cases incarcerated in juvenile, United States Immigration and Customs Enforcement, or other correctional facilities. TB = tuberculosis.
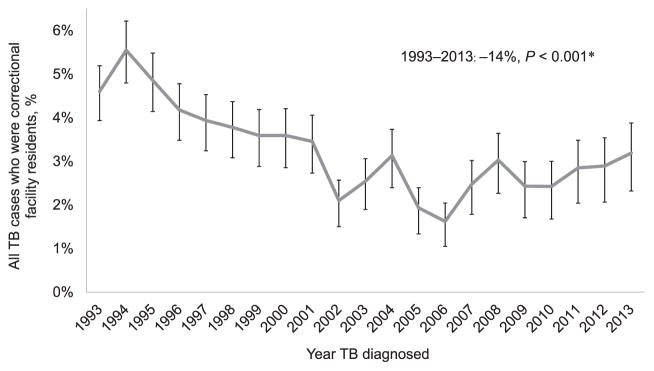
Trends in tuberculosis percentage and incidence rate
The proportion of correctional cases decreased by 14% (P < 0.001, Figure 2) during 1993–2013. Monte Carlo permutation tests identified one join-point in 2006, with a reduction in the proportion of correctional cases diagnosed during 1993–2006 (annual per cent change [APC] −6.3%, 95%CI −8.1 to −4.5), but no change during 2006–2013 (APC 4.6, 95%CI −3.1 to 13.1).
Figure 2.
Trends in the percentage of TB patients aged ≥15 years who were residents of a federal prison, state prison, or local jail at diagnosis, California, 1993–2013. *Per cent change and P values were calculated using weighted linear regression. Ninety-five per cent confidence intervals for binominal proportions were calculated for the annual percentage of cases using the Wilson score interval. TB = tuberculosis.
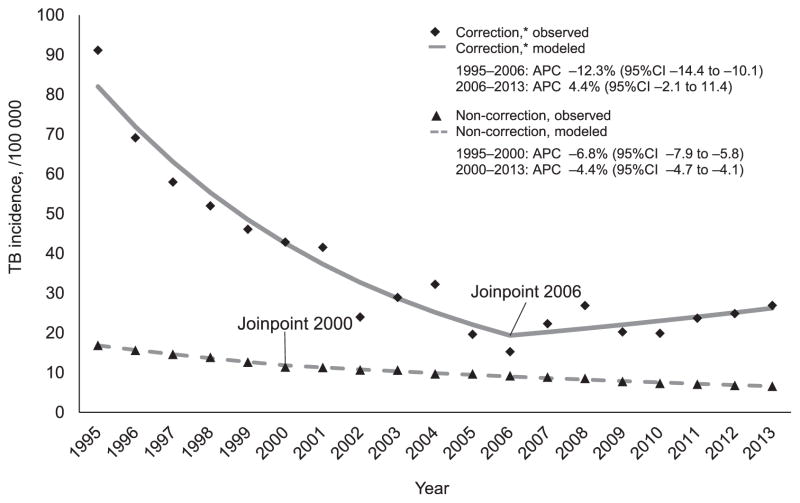
TB incidence decreased by 77% (95%CI −86 to −65%) among correctional populations and by 60% (95%CI –62 to –58) among non-correctional populations during 1995–2013. Permutation analysis identified one joinpoint in correctional incidence in 2006 and one joinpoint in non-correctional incidence in 2000 (Figure 3). Similar to proportional trends, correctional incidence decreased during 1995–2006 (APC −12.3%, 95%CI −14.4 to −10.1), but did not change during 2006–2013 (APC 4.4%, 95%CI −2.1 to 11.4). Incidence among non-correctional populations decreased during 1995–2000 (APC −6.8%, 95%CI −7.9 to −5.8) and during 2000–2013 (APC −4.4%, 95%CI −4.7 to −4.1).
Figure 3.
TB incidence trends by residence at the time of diagnosis, California, 1995–2013. APC and 95%CIs were calculated using the Monte Carlo permutation test. *Residents of a federal prison, state prison, or local jail at the time of diagnosis. TB =tuberculosis; APC = annual per cent change; CI = confidence interval.
Incidence in each correctional facility also declined; it decreased by 23% (95%CI −56 to 36) in federal prisons, 97% (95%CI −99 to −93) in state prisons, 78% (95%CI −85 to −66) in local jails, and 60% (95%CI−62 to−58) in non-correctional populations. The number of cases, population estimates, and incidence rates are reported in Appendix Table A.*
Demographic characteristics of TB cases
Among correctional cases, more than half (53%) were foreign-born patients, primarily originating from Mexico (76%). Compared with state prisons, federal prisons had higher proportions of cases that were male (98% vs. 92%, P = 0.03), younger adults (median 32 vs. 39 years, P < 0.001), Hispanics (86% vs. 54%, P < 0.001), and foreign-born persons (82% vs. 28%, P < 0.001) (Table 1). Among the foreign-born, patients diagnosed in a federal prison were more likely than those diagnosed in state prisons to be from Mexico (88% vs. 71%, P = 0.02) and to have arrived in the United States within 5 years of diagnosis (62% vs. 13%, P < 0.001). Cases in federal prisons were also less likely to consume excessive amounts of alcohol (30% vs. 51%, P < 0.001), inject drugs (10% vs. 22%, P = 0.01), or use non-injected drugs (38% vs. 51%, P = 0.04).
Table 1.
Comparison of demographic and social characteristics of tuberculosis patients aged ≥15 years who were correctional residents at diagnosis, California, 2000–2009
| State prison (n = 134) | Federal prison (n = 131) | P value* | Local jail (n = 434) | P value† | |
|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | |||
| Demographic characteristics | |||||
| Male | 123 (92) | 128 (98) | 0.03 | 397 (91) | 0.91 |
| Age, years, median [IQR] | 39 [32–47] | 32 [24–38] | <0.001 | 38 [28–46] | 0.12 |
| Race/ethnicity | |||||
| White | 21 (16) | 6 (5) | 0.002 | 61 (14) | 0.64 |
| Black | 29 (22) | 4 (3) | <0.001 | 89 (21) | 0.77 |
| Hispanic | 72 (54) | 113 (86) | <0.001 | 239 (55) | 0.79 |
| Asian | 7 (5) | 7 (5) | 0.97 | 40 (9) | 0.14 |
| Other, multiple, or missing‡ | 5 (4) | 1 (1) | — | 5 (1) | — |
| Born outside of the US§ | 38 (28) | 108 (82) | <0.001 | 223 (51) | <0.001 |
| Mexico¶ | 27 (71) | 95 (88) | 0.02 | 159 (71) | 0.98 |
| Arrived in US within 5 years of TB diagnosis# | 5 (16) | 64 (62) | <0.001 | 67 (32) | 0.03 |
| Social characteristics | |||||
| Any substance use** | 67 (59) | 66 (52) | 0.23 | 311 (75) | <0.01 |
| Excessive alcohol use†† | 56 (51) | 38 (30) | <0.001 | 222 (56) | 0.38 |
| Injection drug use‡‡ | 23 (22) | 13 (10) | 0.01 | 56 (14) | 0.06 |
| Non-injection drug use§§ | 54 (51) | 48 (38) | 0.04 | 192 (48) | 0.53 |
| Homeless in the previous year¶¶ | 14 (12) | 8 (6) | 0.12 | 145 (34) | <0.001 |
χ2 analysis comparing demographic characteristics among patients residing in state prisons vs. federal prisons.
χ2 analysis comparing demographic characteristics among patients residing in state prisons vs. local jails.
Small numbers in American Indian/Alaska Native, Native Hawaiian/Other Pacific Islander, multiple races, or unknown/missing races are grouped together.
Analysis of patients with a known country of origin (federal prison, n = 131; state prison, n =128; local jail, n = 428).
Analysis of patients who were born outside of the United States and had a known country of origin (federal prison, n =108; state prison, n =38; local jail, n = 223).
Analysis of patients who were born outside of the United States and had a known date of arrival (federal prison, n =104; state prison, n =31; local jail, n =211).
Analysis of patients with a known history of substance use, defined as any reported history of injection drug use, non-injection drug use, or excessive alcohol use in the year prior to TB diagnosis (federal prison, n = 128; state prison, n = 113; local jail, n = 415).
Analysis of patients with a known history of excessive alcohol use in the year before TB diagnosis (federal prison, n =126; state prison, n =109; local jail, n = 222).
Analysis of patients with a known history of injection drug use in the year before TB diagnosis (federal prison, n =126; state prison, n =104; local jail, n =389).
Analysis of patients with a known history of non-injection drug use in the year prior to TB diagnosis (federal prison, n =127; state prison, n =105; local jail, n = 192).
Analysis of patients with a known history of homelessness at any time during the year before TB diagnosis (federal prison, n =128; state prison, n =118; local jail, n = 421).
IQR = interquartile range; TB = tuberculosis.
Compared with state prisons, local jails had higher proportions of foreign-born persons (51% vs. 28%, P < 0.001) and patients arriving in the United States within 5 years of diagnosis (32% vs. 13%, P =0.03). Cases in local jails were also more likely to have a history of substance use (75% vs. 59%, P <0.01) and homelessness (34% vs. 12%, P < 0.001).
Clinical characteristics and treatment outcomes of tuberculosis cases
Compared with state prisons, federal prisons had higher proportions of cases with pulmonary TB (90% vs. 72%, P <0.001), but lower proportions of patients with HIV/AIDS (acquired immune-deficiency syndrome) (5% vs. 12%, P =0.03; Table 2). Federal prison cases also had lower treatment completion rates (53% vs. 67%, P = 0.02), with a higher proportion of cases reported as lost to follow-up (20% vs. 8%, P =0.04).
Table 2.
Clinical characteristics and treatment outcomes of TB patients aged ≥15 years who were correctional residents at diagnosis, California, 2000–2009
| Clinical characteristics | State prison (n = 134) | Federal prison (n = 131) | P value* | Local jail (n = 434) | P value† |
|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | |||
| Previous diagnosis of TB‡ | 5 (4) | 5 (4) | 1.0 | 24 (6) | 0.43 |
| TB skin test | |||||
| Positive | 97 (72) | 85 (65) | 0.18 | 325 (75) | 0.56 |
| Negative or not done | 37 (28) | 44 (34) | 0.29 | 99 (23) | 0.25 |
| Unknown | 0 | 2 (2) | — | 10 (2) | — |
| TB site of disease | |||||
| Pulmonary | 97 (72) | 118 (90) | <0.001 | 397 (91) | <0.001 |
| Extra-pulmonary | 26 (19) | 7 (5) | <0.001 | 21 (5) | <0.001 |
| Both | 11 (8) | 6 (5) | 0.23 | 16 (4) | 0.03 |
| Infectiousness | |||||
| Sputum culture+, smear+ | 49 (37) | 44 (34) | 0.61 | 198 (46) | 0.06 |
| Sputum culture+, smear− | 40 (30) | 45 (34) | 0.43 | 142 (33) | 0.53 |
| Pulmonary clinical diagnosis | 19 (14) | 35 (27) | 0.01 | 73 (17) | 0.47 |
| Extra-pulmonary TB | 26 (19) | 7 (5) | <0.001 | 21 (5) | <0.001 |
| Abnormal chest X-ray§ | |||||
| Cavitary | 26 (24) | 30 (24) | 0.98 | 60 (15) | 0.02 |
| Non-cavitary TB | 73 (68) | 92 (74) | 0.27 | 331 (80) | <0.01 |
| Non-cavitary, not TB | 9 (8) | 2 (2) | — | 22 (5) | 0.24 |
| HIV/AIDS-positive¶ | 16 (12) | 6 (5) | 0.03 | 29 (7) | 0.05 |
| Pan-susceptible TB# | 59 (87) | 73 (86) | 0.87 | 278 (89) | 0.58 |
| Treatment outcome** | |||||
| Completed | 87 (67) | 68 (53) | 0.02 | 323 (76) | 0.06 |
| Moved | 25 (19) | 26 (20) | 0.85 | 49 (11) | 0.02 |
| Lost | 10 (8) | 26 (20) | <0.01 | 38 (9) | 0.68 |
| Died | 4 (3) | 0 | — | 5 (1) | — |
| Refused/other | 3 (2) | 8 (6) | — | 11 (3) | — |
χ2 analysis comparing demographic characteristics among patients residing in state prisons vs. federal prisons.
χ2 analysis comparing demographic characteristics among patients residing in state prisons vs. local jails.
Analysis of patients with data on history of previous TB diagnosis (federal prison, n = 129; state prison, n = 129; local jail, n = 427).
Analysis of patients with pulmonary TB and chest X-ray results (federal prison, n = 124; state prison, n = 108; local jail, n = 413).
Analysis of patients matched to the California HIV/AIDS Registry.
Analysis of patients with culture-positive TB and drug susceptibility results for isoniazid, rifampin, pyrazinamide, and ethambutol (federal prison, n = 85; state prison, n = 68; local jail, n = 312).
Analysis of patients with treatment outcome data (federal prison, n = 128; state prison, n = 129; local jail, n = 426).
TB = tuberculosis; HIV = human immunodeficiency virus; AIDS = acquired immunodeficiency syndrome.
Compared with state prisons, local jails had significantly higher proportions of cases with pulmonary TB (91% vs. 72%, P < 0.001), but lower proportions of cases with cavitary lesions on chest radiography (15% vs. 24%, P = 0.02), patients with HIV/AIDS (7% vs. 12%, P = 0.05), and patients reported as having ‘moved’ as a reason for treatment interruption (11% vs. 19%, P = 0.02). A lower percentage of correctional cases overall than non-correctional cases completed treatment (478/683, 70% vs. 22 495/26 070, 86%; P < 0.001).
Sub-analysis of correctional cases diagnosed during 2010–2013
During 2010–2013, 286/8593 (3%) cases were reported in adults incarcerated at diagnosis. Compared with non-correctional cases, correctional cases had lower treatment completion rates (205/286, 72% vs. 6708/8279, 81%; P < 0.001) and higher rates of movement while on treatment (120/279, 42% vs. 611/7879, 7%; P < 0.001). Treatment completion was low among both correctional and non-correctional cases who moved while on treatment (64/120, 53% vs. 290/611, 47%; P = 0.27). Of 120 correctional cases who moved while on treatment, 58 (48%) moved within California, 50 (42%) moved out of the United States, and 12 (10%) moved to another state in the United States. Of the 50 patients who moved out of the United States, 48 (96%) were referred to international health agencies.
There was no significant difference in utilization of the NAA test between correctional and non-correctional cases (144/285, 51% vs. 3759/8280, 45%; P=0.09) or as an initial diagnostic modality for sputum smear-negative cases (17/29, 59% vs. 413/646, 64%; P=0.56).
DISCUSSION
TB incidence in California has decreased significantly in both correctional and non-correctional populations over the last two decades. However, incidence in correctional facilities began leveling out in 2006, despite continued decreases among non-incarcerated populations. Overall, incarcerated patients in California continue to have TB incidence rates three to four times higher than non-incarcerated populations (Appendix Table A).
It should be noted that the most substantial decrease in incidence among correctional populations has been in state prisons which, in 2012 and 2013, had lower incidence rates than non-incarcerated populations. Although the cause of these reductions has not been determined, enhanced control policies for diagnosing and treating TB were implemented in 1993, which may have led to lower transmission in the state prison system.18 This decline may also have been supplemented by improvements in diagnosing TB upon entry to local jails, where an inmate may be initially incarcerated before arriving at a state prison. We also found that inmates of state prisons were more likely to have HIV coinfection. This population may be screened for TB more often and may be less likely to progress to infectious TB with the availability of antiretroviral therapy.
There were also differences in the demographic and clinical characteristics of cases residing in correctional institutions that may explain some of the varying incidence rates observed. State prison cases were more likely to be US-born, with non-infectious, extra-pulmonary TB, than federal prison or local jail cases. Foreign-born populations are likely of particular importance in federal prisons, where cases are more likely to be persons born in Mexico who arrived in the United States within 5 years of diagnosis. The proportion of incarcerated Hispanic TB patients has been increasing since 2003.19 This population is less likely to be insured or to regularly access public health services, where they could be screened and treated for TB.20 Likewise, local jail cases were more likely to be persons with a history of substance use and homelessness—populations that may also infrequently access public health services. Higher incidence rates among these at-risk populations may be an indication of successful screening upon entry to correctional facilities. Our findings highlight potentially meaningful differences between inmate populations. In addition to infection control policies, correctional TB control policies may benefit from considering population risk factors.2
Our analysis also found that patients diagnosed in a correctional facility were less likely to complete treatment than non-correctional patients. Similar findings have been reported elsewhere among specific subpopulations at risk for incomplete treatment.21 Current data on treatment outcome do not distinguish between patients incarcerated for the duration of treatment and those who have been released from custody while on treatment. There are also no data to differentiate patients who moved between correctional facilities from those who were paroled to the community. Of the available data, correctional cases were more likely to move while on treatment than non-correctional cases, a factor that may contribute to lower treatment completion rates. These results are consistent with findings showing that patients who move are less likely to complete treatment.22 Our analysis reveals potential limitations in assessing treatment outcomes using surveillance data, and highlights the need for better coordination of care between correctional facilities, state and local health jurisdictions, and international TB partners, especially upon parole.
These findings are subject to limitations. First, because of unavailable population estimates, cases among persons residing in juvenile or other types of correctional facilities, accounting for 11% of correctional cases, were excluded from the analysis. Second, incidence rates were calculated using ADP estimates. These population estimates were available for all three correctional populations, but could disproportionately overestimate incidence in facilities with large variations in population size or short durations of incarceration. Third, current surveillance methods do not distinguish TB diagnosis upon entry from diagnosis during incarceration, making it difficult to assess for transmission that may be occurring within correctional facilities. Finally, there are currently no systematic methods for measuring the impact of the duration of stay or policy differences on TB control efforts.
Focused strategies may be necessary to ensure incidence continues to decline among inmate populations. The NAA test can detect M. tuberculosis bacteria in a specimen weeks earlier than culture-based methods, and is recommended for patients with suspected pulmonary disease.23,24 Increasing the utilization of early diagnostic methods, such as the NAA test, could prevent the need for labor-intensive contact investigations. TB programs should also focus on ensuring continuity of care across multiple jurisdictions. Strengthening collaborations, including data sharing between correctional facilities, law enforcement, and TB programs, could allow improved coordination of care among responsible parties after inmate release.
Finally, collaborations with the California Correctional Health Care Services revealed that up to 75% of state prison cases were diagnosed more than 6 months after entry, suggesting that most TB disease is due to reactivation of latent tuberculous infection (K Lucas, personal communication, August 2016). Tuberculous infection has been successfully treated using the 3-month, 12-dose isoniazid-rifapentine regimen in various settings, including correctional facilities, in which equal or higher treatment completion rates have been achieved compared with those in clinical trials.25–27 Utilizing shorter treatment regimens can increase treatment completion for tuberculous infection and prevent progression to infectious TB, reducing the number of patients requiring coordination of care upon release.28,29 Given the high rate of movement among correctional cases, TB programs and correctional facilities should focus on increasing treatment for tuberculous infection using shorter regimens among current and former inmates. Successful treatment of tuberculous infection provides an opportunity to improve outcomes and prevent future progression to TB disease in correctional facilities and the community.
Acknowledgments
The authors wish to thank J Mohle-Boetani, C Wheeler, and K Lucas, California Correctional Health Care Services, Elk Grove, CA, USA, and G Schecter, California Department of Public Health, Sacramento, CA, USA, for their feedback in developing this manuscript; M Ehman for consultation on Joinpoint analysis; J Westenhouse and the California Tuberculosis Control Branch Registry for data quality assurance and database preparation.
This study was supported by the Grant or Cooperative Agreement Number U52PS004656 funded by the Centers for Disease Control and Prevention (CDC), Atlanta, GA, USA. The contents of this manuscript are solely the responsibility of the authors and do not necessarily represent the official views of the CDC, the Department of Health and Human Services, Washington DC, USA, or the California Department of Public Health.
APPENDIX
Table A.
TB cases among correction and non-correctional populations by residence at the time of diagnosis, California, 1993–2013
| Year | TB cases | ||||
|---|---|---|---|---|---|
|
| |||||
| Non-corrections | Corrections† | Federal prisons | State prisons | Local jails | |
| n/N (rate per 100 000*) | n/N (rate per 100 000*) | n/N (rate per 100 000*) | n/N (rate per 100 000*) | n/N (rate per 100 000*) | |
| 1993 | 4 371/NA (NA) | 197/NA (NA) | 4/6 560 (61) | 106/119 951 (88) | 87/NA (NA) |
| 1994 | 4 079/NA (NA) | 222/NA (NA) | 5/7 279 (69) | 64/125 605 (51) | 153/NA (NA) |
| 1995 | 4 016/23 835 341 (17) | 192/210 711 (91) | 5/7 350 (68) | 71/135 133 (53) | 116/68 228 (170) |
| 1996 | 3 749/24 044 792 (16) | 154/222 868 (69) | 6/6 709 (89) | 63/145 565 (43) | 85/70 594 (120) |
| 1997 | 3 569/24 457 777 (15) | 138/238 122 (58) | 3/6 876 (44) | 41/155 276 (26) | 94/75 970 (124) |
| 1998 | 3 447/24 860 872 (14) | 128/246 353 (52) | 15/8 490 (177) | 36/159 563 (23) | 77/78 300 (98) |
| 1999 | 3 208/25 387 327 (13) | 113/245 254 (46) | 9/9 211 (98) | 26/160 970 (16) | 78/75 073 (104) |
| 2000 | 2 966/26 004 576 (11) | 105/245 140 (43) | 16/10 145 (158) | 26/161 567 (16) | 63/73 428 (86) |
| 2001 | 2 980/26 413 965 (11) | 101/243 118 (42) | 22/10 916 (202) | 22/160 000 (14) | 57/72 202 (79) |
| 2002 | 2 859/26 771 018 (11) | 59/246 033 (24) | 12/11 918 (101) | 12/158 682 (8) | 35/75 433 (46) |
| 2003 | 2 889/27 163 451 (11) | 72/249 178 (29) | 13/13 390 (97) | 11/160 772 (7) | 48/75 016 (64) |
| 2004 | 2 664/27 509 699 (10) | 82/254 676 (32) | 16/13 762 (116) | 17/163 346 (10) | 49/77 568 (63) |
| 2005 | 2 682/27 774 971 (10) | 51/259 783 (20) | 8/14 630 (55) | 13/164 392 (8) | 30/80 761 (37) |
| 2006 | 2 576/28 067 563 (9) | 41/268 790 (15) | 5/16 075 (31) | 8/171 340 (5) | 28/81 375 (34) |
| 2007 | 2 515/28 401 095 (9) | 61/273 823 (22) | 17/17 241 (99) | 7/172 582 (4) | 37/84 000 (44) |
| 2008 | 2 459/28 749 434 (9) | 73/271 657 (27) | 14/17 423 (80) | 10/171 264 (6) | 49/82 970 (59) |
| 2009 | 2 269/29 153 927 (8) | 54/267 099 (20) | 8/17 214 (47) | 8/168 286 (5) | 38/81 599 (47) |
| 2010 | 2 142/29 448 826 (7) | 51/256 415 (20) | 15/17 322 (87) | 17/165 747 (10) | 19/73 346 (26) |
| 2011 | 2 101/29 753 023 (7) | 59/249 091 (24) | 11/18 193 (61) | 14/160 071 (9) | 34/70 827 (48) |
| 2012 | 2 036/30 075 534 (7) | 58/233 529 (25) | 24/18 875 (127) | 4/136 783 (3) | 30/77 871 (39) |
| 2013 | 2 001/30 390 718 (7) | 63/234 102 (27) | 16/19 140 (84) | 5/133 217 (4) | 42/81 745 (51) |
TB case incidence rates per 100 000 population were calculated from estimates of California resident and institutional populations.14–16
The number of correctional cases presented includes TB cases incarcerated in a federal prison, state prison, or local jail; cases residing in a juvenile, United States Immigration and Customs Enforcement, or other correctional facility have been excluded.
NA = not available; TB = tuberculosis.
Footnotes
The appendix is available in the online version of this article, at http://www.ingentaconnect.com/content/iuatld/ijtld/2017/00000021/00000008/art00015.
Conflicts of interest: none declared.
References
- 1.World Health Organization. WHO policy on TB infection control in health-care facilities, congregate settings and households. Geneva, Switzerland: WHO; 2009. WHO/HTM/TB/2009.419. [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. Prevention and Control of Tuberculosis in Correctional and Detention Facilities: Recommendations from CDC. MMWR Morb Mortal Wkly Rep. 2006;55:1–44. [Google Scholar]
- 3.Macneil JR, Lobato MN, Moore M. An unanswered health disparity: tuberculosis among correctional inmates, 1993 through 2003. Am J Public Health. 2005;95:1800–1805. doi: 10.2105/AJPH.2004.055442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lambert LA, Armstrong LR, Lobato MN, Ho C, France AM, Haddad MB. Tuberculosis in jails and prisons: United States, 2002–2013. Am J Public Health. 2016;106:2231–2237. doi: 10.2105/AJPH.2016.303423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mohle-Boetani JC, Miguelino V, Dewsnup D, et al. Outbreak in a housing unit for human immunodeficiency virus–infected patients in a correctional facility: transmission risk factors and effective outbreak control. Clin Infect Dis. 2002;34:668–676. doi: 10.1086/338815. [DOI] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention. Tuberculosis outbreaks in prison housing units for HIV-infected inmates—California, 1995–1996. MMWR Morb Mortal Wkly Rep. 1999;48:79–82. [PubMed] [Google Scholar]
- 7.Valway SE, Richards SB, Kovacovich J, Greifinger RB, Crawford JT, Dooley SW. Outbreak of multidrug-resistant tuberculosis in a New York State prison, 1991. Am J Epidemiol. 1994;140:113–122. doi: 10.1093/oxfordjournals.aje.a117222. [DOI] [PubMed] [Google Scholar]
- 8.Bur S, Golub J, Armstrong J, et al. Evaluation of an extensive tuberculosis contact investigation in an urban community and jail. Int J Tuberc Lung Dis. 2003;7(Suppl 3):S417–S423. [PubMed] [Google Scholar]
- 9.Jones TF, Woodley CL, Fountain FF, Schaffner W. Increased incidence of the outbreak strain of Mycobacterium tuberculosis in the surrounding community after an outbreak in a jail. South Med J. 2003;96:155–157. doi: 10.1097/01.SMJ.0000053678.62096.6F. [DOI] [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention. Tuberculosis transmission in multiple correctional facilities—Kansas, 2002–2003. MMWR Morb Mortal Wkly Rep. 2004;53:734–738. [PubMed] [Google Scholar]
- 11.Centers for Disease Control and Prevention. Reported tuberculosis in the United States, 2014. Atlanta, GA, USA: US Department of Health and Human Services, CDC; 2015. [Google Scholar]
- 12.Bureau of Justice Statistics. Correctional populations in the United States, 2013. Washington DC, USA: US Department of Justice, BJS; 2014. [Google Scholar]
- 13.Centers for Disease Control and Prevention. CDC tuberculosis surveillance data training: report of verified case of tuberculosis (RVCT) instruction manual. Atlanta, GA, USA: US Department of Health and Human Services, CDC; 2009. [Google Scholar]
- 14.California Department of Corrections and Rehabilitation. Average daily prison population report archive. Sacramento, CA, USA: California Department of Corrections and Rehabilitation; 2017. [Accessed April 2017]. http://www.cdcr.ca.gov/reports_research/offender_information_services_branch/Annual/Ipop2Archive.html. [Google Scholar]
- 15.California Board of State and Community Corrections. Jail profile survey—online query. Sacramento, CA, USA: BSCC; 2017. [Accessed April 2017]. https://app.bscc.ca.gov/joq//jps/QuerySelection.asp. [Google Scholar]
- 16.California Department of Finance. E-8 historical population and housing estimates for cities, counties, and the state, 2000–2010. Sacramento, CA, USA: California Department of Finance; 2012. [Google Scholar]
- 17.Kim H, Fay M, Feuer E, Midthune D. Permutation Tests for joinpoint regression with applications to cancer rates. Stat Med. 2000;19:335–351. doi: 10.1002/(sici)1097-0258(20000215)19:3<335::aid-sim336>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 18.State of California Legislative Information. Examination of inmates and wards for tuberculosis. Sacramento, CA, USA: California Legislative Information; 1993. California Penal Code. [Google Scholar]
- 19.Mindra G, Wortham JM, Haddad MB, Salinas JL, Powell KM, Armstrong LR. Tuberculosis among incarcerated Hispanic persons in the United States, 1993–2014. J Immigr Minor Heal. 2016 Nov 29; doi: 10.1007/s10903-016-0534-8. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Davidow AL, Katz D, Ghosh S, et al. Preventing infectious pulmonary tuberculosis among foreign-born residents of the United States. Am J Public Health. 2015;105:81–88. doi: 10.2105/AJPH.2015.302662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mitruka K, Winston CA, Navin TR. Predictors of failure in timely tuberculosis treatment completion, United States. Int J Tuberc Lung Dis. 2012;16:1075–1082. doi: 10.5588/ijtld.11.0814. [DOI] [PubMed] [Google Scholar]
- 22.Cummings KC, Mohle-Boetani JC, Royce SE, Chin DP. Movement of tuberculosis patients and the failure to complete antituberculosis treatment. Am J Respir Crit Care Med. 1998;157:1249–1252. doi: 10.1164/ajrccm.157.4.9708058. [DOI] [PubMed] [Google Scholar]
- 23.Moore DF, Guzman JA, Mikhail LT. Reduction in turnaround time for laboratory diagnosis of pulmonary tuberculosis by routine use of a nucleic acid amplification test. Diagn Microbiol Infect Dis. 2005;52:247–254. doi: 10.1016/j.diagmicrobio.2005.02.014. [DOI] [PubMed] [Google Scholar]
- 24.Centers for Disease Control and Prevention. Updated guidelines for the use of nucleic acid amplification tests in the diagnosis of tuberculosis. Morb Mortal Wkly Rep. 2009;58:7–10. [PubMed] [Google Scholar]
- 25.Juarez-Reyes M, Gallivan M, Chyorny A, O’Keeffe L, Shah N. Completion rate and side effect profile of three months isoniazid and rifapentine treatment for latent tuberculosis infection in an urban county jail. Open Forum Infect Dis. 2016;3:ofv220. doi: 10.1093/ofid/ofv220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Federal Bureau of Prisons. Isoniazid-rifapentine treatment for latent TB infection: addendum to ‘management of tuberculosis’. Washington DC, USA: FBOP; 2014. [Accessed April 2017]. http://www.bop.gov/resources/pdfs/latent_TB_infection.pdf. [Google Scholar]
- 27.Sterling TR, Villarino ME, Borisov AS, et al. Three months of rifapentine and isoniazid for latent tuberculosis infection. N Engl J Med. 2011;365:2155–2166. doi: 10.1056/NEJMoa1104875. [DOI] [PubMed] [Google Scholar]
- 28.Centers for Disease Control and Prevention. Recommendations for use of an isoniazid-rifapentine regimen with direct observation to treat latent Mycobacterium tuberculosis infection. Morb Mortal Wkly Rep. 2011;60:1650–1653. [PubMed] [Google Scholar]
- 29.US Preventive Services Task Force. Screening for latent tuberculosis infection in adults. J Am Med Assoc. 2016;316:962–969. [Google Scholar]