Abstract
PURPOSE:
The purpose of the study was to evaluate the efficacy of silicone rods as frontalis sling for correction of ptosis associated with poor Bell's phenomenon in specific situations.
MATERIALS AND METHODS:
A retrospective interventional case series of 25 eyes of 19 patients who underwent frontalis suspension surgery with silicone rods for ptosis correction from May 2006 to April 2011, was performed. Inclusion criteria included severe ptosis with poor Bell's phenomenon. Patient evaluation included clinical history and other relevant parameters of ptosis measurement. Final outcome measurements included postoperative lid height, lagophthalmos, complications, need for reoperation, and patient satisfaction.
RESULTS:
Mean age at presentation was 25.72 ± 2.2 years. The sex ratio of male: female was 1.11. The causes of ptosis included chronic progressive external ophthalmoplegia (CPEO) in 11 eyes (44%), oculopharyngeal dystrophy in 2 (8%), third cranial nerve palsy in 7 (28%), traumatic in three eyes (12%), and iatrogenic postoperative ptosis (after orbital tumor excision) in two eyes (8%). The postoperative palpebral fissure height and margin reflex distance improved significantly (P = 0.0001). Extrusion of the sling and granuloma formation occurred in two eyes each, and these patients had to undergo sling removal. One patient developed mild exposure keratopathy and was managed conservatively.
CONCLUSION:
Silicone is an effective material for use in frontalis suspension in the management of severe ptosis with poor Bell's phenomenon. The elastic nature of silicone rod makes it an ideal suspensory material for patients with CPEO or third nerve palsy.
Keywords: Bell's phenomenon, frontalis suspension, ptosis, silicone rod
Introduction
Frontalis suspension is the mainstay of surgical management for patients with severe ptosis accompanied by poor levator function. The materials available for this purpose are autogenous and preserved fascia lata, temporalis fascia, deepithelialized strips of skin, orbicularis oculi muscle, palmaris longus tendon, silicone rods, nonabsorbable suture materials (nylon/polypropylene/polyester), and wide porous expanded polytetrafluoroethylene.[1,2] Of these, silicone has the distinct advantage of excellent elasticity enabling good blinking movement, easy adjustability in case of revision, or simple removal of the sling at a later date if warranted.[1,3]
Postoperative lagophthalmos after frontalis suspension surgery is almost universal and predisposes the development of corneal complications in vulnerable patient groups. Clinical findings in patients associated with third cranial nerve palsy, ocular myasthenia gravis (OMG), and chronic progressive external ophthalmoplegia (CPEO) are ptosis, extraocular movement disorders, weak orbicularis action, poor Bell's phenomenon, and poor lid closure.[1,2] These patients are at a higher risk of developing postoperative exposure keratopathy.[2] Postoperative adjustment of eyelid height may also be necessary for progressive conditions such as CPEO and OMG.[1] In view of the above factors, silicone seems to be the ideal material for patients with severe ptosis with poor Bell's phenomenon. This study was undertaken to evaluate the outcome of frontalis sling suspension with silicone rods in these situations in Indian eyes with a review of published literature.
Materials and Methods
Informed consent was obtained from each patient, and the study was in adherence to the tenets of the Declaration of Helsinki. It is a retrospective interventional case series undertaken over a 5-year period in a tertiary eye care institute in South India. Patient evaluation included clinical history, visual acuity, Hirschberg's test, ocular motility, pupillary evaluation, palpebral fissure height (PFH), margin reflex distance (MRD), levator palpebrae superioris (LPS) action, margin crease distance (MCD), lagophthalmos, Bell's phenomenon, fatigability test, Cogan's lid twitch sign, corneal sensation, Schirmer's test, and Ice test. Inclusion criteria were severe ptosis (MRD-1 = 0) and poor (small response) Bell's phenomenon. Bell's phenomenon was evaluated by opening both upper lids by examiners thumb while asking the patient to forcefully close eyes and assessing the direction in which the eyes rotate. Bell's phenomenon was classified into large (=4 mm) and small response (<4 mm) along with the direction of response. The surgery was performed under local infiltrative anesthesia in adults with intravenous sedation and under general anesthesia in children. Frontalis sling was performed using modified Fox Pentagon technique using silicone rod suspension set (Visitec, BD Ophthalmics, New Jersey, USA) [Figure 1]. An identical surgical technique was used by the same surgeon in each patient.
Figure 1.
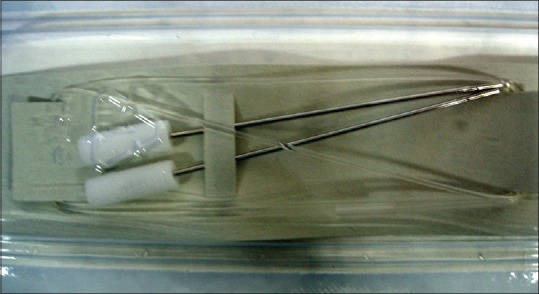
Commercially available silicone frontalis suspension set (Visitec, BD Ophthalmics, New Jersey, USA)
A sterile pen was used to mark 2 mm above the lash line parallel to the level of lateral and medial limbus; the natural or desired eyelid crease; just above the lateral and medial ends of the brows and around 1 cm above the brow on the forehead in the pupillary axis. Subcutaneous infiltration of local anesthetic (1:1 mixture of 2% lidocaine with 1:100,000 epinephrine and 0.5% bupivacaine) was injected at the markings. Stab incisions were made along the markings with number 11 Bard-Parker blade. We used half of the sling with the attached needle for each eye. The needle was passed from the forehead incision down to exit above the brow. Then, it was passed behind the orbital septum to exit just above the lid margin, then through the pretarsal tissues. The direction of the needle was reversed and passed deep to the septum to exit above the brow. Finally, the needle was taken out from the forehead incision. The needle was detached, and both ends of the silicone rod were passed through the sleeve supplied with the set [Figure 2].
Figure 2.

Frontalis suspension using Fox Pentagon technique showing the path of the sling from forehead followed by brow, lid margin, and reverse
When under local anesthesia, the patients were made to sit up. The sling was tightened until the upper eyelid margin was at the pupil or just above it (MRD-1: 0 to + 1) after negating the frontalis action by pressure over suprabrow area by the assistant's thumb. In patients under general anesthesia, the sling was tightened till the visual axis was just clear (MRD-1: +1 to + 2), as opposed to the normal practice of leaving the lid margin at the superior limbus. Undercorrection was achieved by negating frontalis overaction by pressure over suprabrow in patients under local anesthesia, while in patients under general anesthesia with the aid of muscle relaxants. The ends of the rod were cut long and buried. The forehead incision was sutured in two layers while the rest of the stab incisions were left unsutured as they heal rapidly. A single frost suture was passed through the lower lids and kept in place for 48 h. Cold compresses and copious lubricating eye drops were started following removal of the eye patch after 2 hours. Topical antibiotic ointment was prescribed for 2 weeks with gel preparation to be instilled daily at night for long-term use. Preoperative vision, MRD-1, and PFH were compared with the outcome measurements of postoperative MRD-1, PFH. Corneal involvement after fluorescein staining, complications, lagophthalmos, need for reoperation, and patient satisfaction were noted. Statistical analysis was carried out using the Statistical package for social sciences version 16 (SPSS Inc., Chicago, IL, USA) and Microsoft (R) Office Excel 2010. Paired t-test was used for comparison of continuous variables. All statistical tests were found to be at a 5% level of significance.
Results
There were 25 (13 unilateral and six bilateral) eyes of 19 patients included in the study. The male: female ratio was 1.11. Mean age at presentation was 25.72 ± 2.2 years. Follow-up period ranged from 6 weeks to 36 months. The family history of ptosis was present in one patient of CPEO and one of oculopharyngeal dystrophy. The patients in this study included 11 eyes (44%) with CPEO, two eyes (8%) with oculopharyngeal dystrophy, seven eyes (28%) with third cranial nerve palsy, three eyes (12%) with traumatic ptosis, and two eyes (8%) with iatrogenic traumatic ptosis after excision of orbital tumors.
The preoperative LPS action was poor (<4 mm in 19 eyes) to fair (5–7 mm in 6 eyes) in all the patients. The pre- and post-operative MRD-1 and PFH are summarized in Table 1. PFH and MRD-1 improved significantly with a P = 0.0001 following surgery. Postoperative lagophthalmos was absent in six eyes, and mild lagophthalmos of (<2 mm) was present in 19 eyes. The postoperative lid contour was fair in nine eyes and good in 16 eyes. Complications were noted in five patients, two sling exposure, and two granuloma formation, [Figure 3] who underwent removal of the slings. On microbiological examination of the removed slings, no growth of any organisms was identified. One patient with history of having undergone excision of a recurrent lacrimal gland lesion developed mild superficial punctate keratopathy following sling surgery with decrease in vision by one line (20/30 from 20/20-Jaeger). She was managed conservatively with copious lubricants and was happy with the surgical outcome [Figure 4]. Thirteen (76%) patients in our series expressed complete satisfaction with the surgical correction while 2 (8%) patients did not share the same sentiments. Satisfaction levels of four patients could not be commented on due to inadequate documentation.
Table 1.
Pre- and post-operative margin reflex distance 1 and palpebral fissure height following frontalis sling with silicone rods
| Preoperative | Postoperative | Paired correlation | Paired simple test mean difference | P | |
|---|---|---|---|---|---|
| PFH | 3.75±2.64 | 7.37±1.95 | 0.474 | 0.495 | 0.0001 |
| MRD-1 | −1.84±1.4 | 1.68±1.26 | 0.042 | 0.369 | 0.0001 |
PFH = Palpebral fissure height, MRD = Margin reflex distance
Figure 3.

Granuloma due to sling on the right forehead at the site of incision
Figure 4.
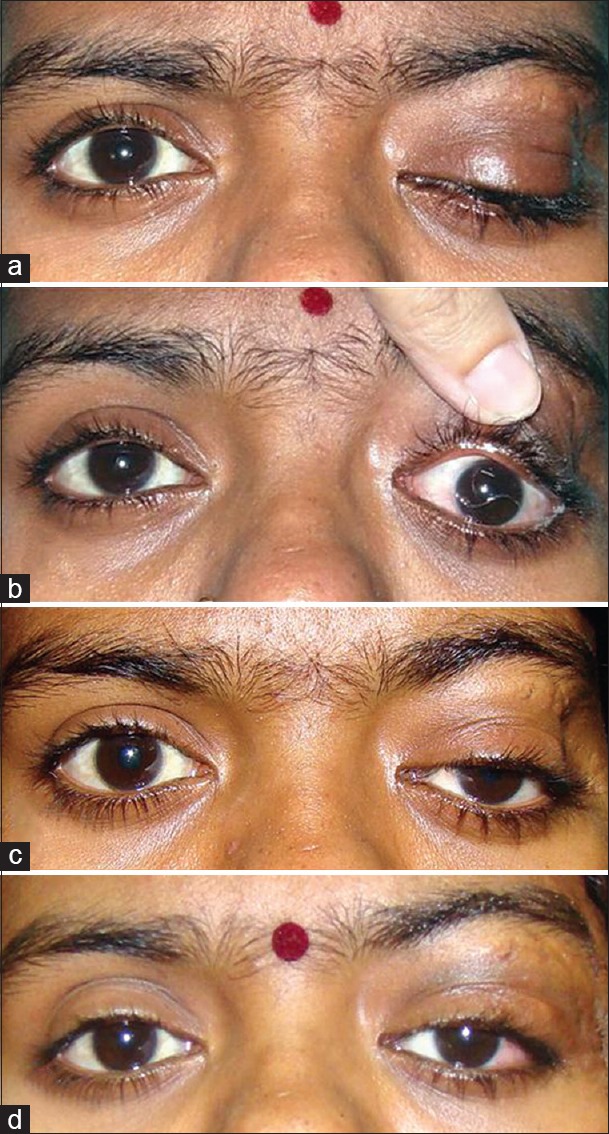
(a and b) Severe ptosis and dystopia due to recurrent lacrimal gland tumor. (c) Residual ptosis after excision of orbital lesion. (d) Following correction of ptosis (note the left frontalis overaction)
Discussion
Bell's phenomenon, named after Sir Charles Bell, is the ability to produce an upward movement of the eye with the oculocephalic maneuver wherein the eyes typically roll upward and outward on the closure of the eyelids [Figure 5].[4] It is considered to be protective, as the risk of exposure keratitis is reduced in the presence of positive Bell's phenomenon, whereas in patients with poor Bell's phenomenon, chances of serious corneal exposure leading to dryness and ulceration are high if lagophthalmos ensues following lid surgery.[5]
Figure 5.
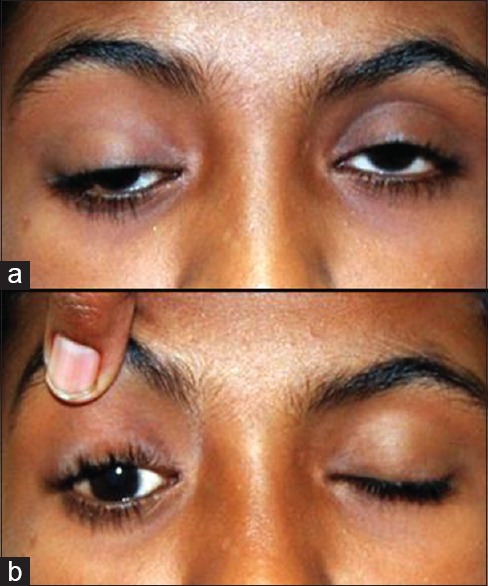
A patient of third nerve palsy showing right eye severe ptosis with hypotropia and poor Bell's phenomenon in right eye
Bell's phenomenon is an important consideration in the management of neurogenic and myogenic ptosis as it may be reduced or absent.[6] In patients with poor Bell's phenomenon, ptosis correction should be approached with caution as it may lead to serious corneal complications due to exposure.[4] Correction of ptosis in patients with CPEO, third cranial nerve palsy, and OMG with the limitation of extraocular movements and poor Bell's phenomenon is fraught with that risk. In fact, many still believe that any surgical intervention is contraindicated in these groups of patients as postoperative lagophthalmos would subject them to an unacceptably high risk of developing exposure keratopathy.
Moss had reported the limited role of ptosis prosthesis (crutches) as a conservative modality of treatment for ptosis [Figure 6].[7] It is still widely prescribed for these groups of patients by many ophthalmologists. However, it should be kept in mind while prescribing crutch glasses that they can lead to skin erosion and infection. Crutch glasses interfere with the normal blink reflex hence is actually contraindicated in patients with poor Bell's phenomenon and dry eyes. Although a combination of spectacle mounted crutch glasses and moisture chamber has been tried for the management of progressive external ophthalmoplegia, surgical correction in the form of frontalis suspension deploying silicone rods remains the definitive and most effective treatment of visually debilitating ptosis.[8]
Figure 6.

Conservative modality of treating ptosis: Crutch glasses to be avoided in our set of patients
Doherty et al. recommend that surgical intervention in these patients should be aimed at obtaining a clear visual axis while minimizing the risk of corneal exposure.[9] For our study, we selected patients with severe ptosis with obscured visual axis. We also consciously undercorrected these patients, which in turn led to nominal postoperative lagophthalmos thereby minimizing the risk of corneal exposure [Figure 7].
Figure 7.

(a) Bilateral myogenic ptosis in a case of chronic progressive external ophthalmoplegia. (b) Postoperative lid height at rest (undercorrection). (c) Lid height after frontalis action with clearing of the visual axis. (d) Postoperative normal lid closure: No lagophthalmos seen
Postoperative PFH was found to be significantly enhanced in these patients leading to the clearing of the visual axis. Johnson and Kuwabara proposed a surgical guideline recommending frontalis suspension if levator function was <8 mm in patients with oculopharyngeal dystrophy.[10]
Complications involving the cornea, such as corneal exposure, keratitis, and ulcer following frontalis sling, have been reported, which however, can be treated effectively.[9] In our study, corneal exposure due to lagophthalmos was treated with lubricants in the initial postoperative period as recommended.[1] While the rest of the group as such did not report any serious corneal complications, one patient developed mild scarring of the cornea following exposure keratopathy in our study.
Two eyes each developed sling granuloma and exposure following surgery which subsequently underwent removal. Recurrence of ptosis is a known complication of silicone sling usage, and all the patients were counseled about the same before surgery.[11] Sling migrations have also been reported but were not seen in our study.
Lelli et al. found the need to revise or replace 39% of slings while in our study, only 4 eyes (16%) of the slings needed removal.[1] Silicone being a foreign material can become infected.[12] Bilateral Candida and atypical mycobacterial infection after frontalis sling suspension with silicone rod have been reported.[13,14] Tuberculosis is an endemic disease in India, and it should be kept as a differential diagnosis when patients with silicone sling develop granuloma. The exposed slings and granuloma material were sent for microbiological assay but did not show any organism. Postoperative diplopia may occur in patients of CPEO and third nerve palsy[2] and should be ruled out during preoperative assessment. If present, these patients may be offered unilateral ptosis correction to avoid diplopia.
In our study, all the patients in the neurogenic ptosis group achieved satisfactory outcome following surgery.
The drawback of our study stems from its retrospective design. Inadequate documentation of patient satisfaction is a case in point. We did not compare the result of frontalis suspension using different materials as we felt it would subject this group of patients to unnecessary risk.
Conclusion
Ptosis correction is a challenge in patients with poor Bell's phenomenon. This is an original study documenting the efficacy of silicone sling for these groups of patients from the Indian subcontinent. The outcome of frontalis suspension with silicone rods is satisfactory, and complications were few in our study. These patients should be monitored closely following surgery to tackle any corneal or sling-related complications. Frontalis suspension surgery with silicone rods is safe and effective option and is undoubtedly the material of choice for correction of severe neurogenic or myogenic ptosis in patients with poor Bell's phenomenon.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Lelli GJ, Jr, Musch DC, Frueh BR, Nelson CC. Outcomes in silicone rod frontalis suspension surgery for high-risk noncongenital blepharoptosis. Ophthal Plast Reconstr Surg. 2009;25:361–5. doi: 10.1097/IOP.0b013e3181b3b183. [DOI] [PubMed] [Google Scholar]
- 2.Bernardini FP, de Conciliis C, Devoto MH. Frontalis suspension sling using a silicone rod in patients affected by myogenic blepharoptosis. Orbit. 2002;21:195–8. doi: 10.1076/orbi.21.3.195.7171. [DOI] [PubMed] [Google Scholar]
- 3.Ahn J, Kim NJ, Choung HK, Hwang SW, Sung M, Lee MJ, et al. Frontalis sling operation using silicone rod for the correction of ptosis in chronic progressive external ophthalmoplegia. Br J Ophthalmol. 2008;92:1685–8. doi: 10.1136/bjo.2008.144816. [DOI] [PubMed] [Google Scholar]
- 4.Brodsky MC, editor. Pediatric Neuro-Ophthalmology. 2nd ed. New York: Springer; 2010. Complex ocular motor disorders in children; pp. 349–57. [Google Scholar]
- 5.Brodsky MC, editor. Pediatric Neuro-Ophthalmology. 2nd ed. New York: Springer; 2010. Ocular motor nerve palsies in children; p. 270. [Google Scholar]
- 6.Olver JM, Collin JR. Management of neurogenic and myogenic ptosis. In: Naugle TC, Hesse RJ, Fry CL, editors. Diagnosis and Management of Oculoplastic and Orbital Disorders: New Orleans Academy of Ophthalmology. New York: Kugler Publications; 1995. p. 29. [Google Scholar]
- 7.Moss HL. Prosthesis for blepharoptosis and blepharospasm. J Am Optom Assoc. 1982;53:661–7. [PubMed] [Google Scholar]
- 8.Cohen JM, Waiss B. Combination ptosis crutch and moisture chamber for management of progressive external ophthalmoplegia. J Am Optom Assoc. 1997;68:663–7. [PubMed] [Google Scholar]
- 9.Doherty M, Winterton R, Griffiths PG. Eyelid surgery in ocular myopathies. Orbit. 2013;32:12–5. doi: 10.3109/01676830.2012.736599. [DOI] [PubMed] [Google Scholar]
- 10.Johnson CC, Kuwabara T. Oculopharyngeal muscular dystrophy. Am J Ophthalmol. 1974;77:872–9. doi: 10.1016/0002-9394(74)90392-4. [DOI] [PubMed] [Google Scholar]
- 11.Carter SR, Meecham WJ, Seiff SR. Silicone frontalis slings for the correction of blepharoptosis: Indications and efficacy. Ophthalmology. 1996;103:623–30. doi: 10.1016/s0161-6420(96)30643-x. [DOI] [PubMed] [Google Scholar]
- 12.Lane CM, Collin JR. Treatment of ptosis in chronic progressive external ophthalmoplegia. Br J Ophthalmol. 1987;71:290–4. doi: 10.1136/bjo.71.4.290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Davies BW, Bratton EM, Durairaj VD, Hink EM. Bilateral Candida and atypical mycobacterial infection after frontalis sling suspension with silicone rod to correct congenital ptosis. Ophthal Plast Reconstr Surg. 2013;29:e111–3. doi: 10.1097/IOP.0b013e318281eb1f. [DOI] [PubMed] [Google Scholar]
- 14.Walang B, Rath S, Sharma S. Nontuberculous mycobacterial infection after frontalis sling surgery using silicone rod. J Ophthalmic Inflamm Infect. 2012;2:219–21. doi: 10.1007/s12348-012-0073-y. [DOI] [PMC free article] [PubMed] [Google Scholar]


