Abstract
Objectives
Abnormalities of lumbopelvic coordination have been suggested to relate to risk of developing low back pain. The objective of this study is to review and summarize the findings of studies that have implemented and reported on lumbopelvic rhythm during trunk forward bending and backward return.
Methods
The PUBMED and CINAHL databases were searched for studies related to LPR using appropriate keywords. The references of each study from the database search were further investigated to identify any missed study.
Results
The findings includes results related to lumbopelvic rhythm, and how it varies due to participant characteristics such as age, gender, and presence of low back pain as well as due to variations in the experimental procedures such as pace of motion, presence of external load, and muscle fatigue.
Conclusion
In general, the magnitude of lumbar contribution is smaller in people with low back pain, in the elderly and females, as well as with greater pace of motion, but is larger with greater external load or back muscle fatigue. The compiled data in this review are expected to serve as a foundation for implementation of this kinematic-based measure in the conduct of future research.
Keywords: Lumbopelvic rhythm, Lumbar spine, Pelvis, Lumbar contribution, Pelvic contribution
Introduction
Low back pain (LBP) is a significant health problem, affecting the well-being of many people each year and imposing a huge economic burden to industries and the healthcare system.1–3 Given the complexity and multifactorial nature of this disorder,4–6 management of LBP inevitably relies on the availability of measures which can help identify at risk individuals, match patients with existing treatments, and monitor the progress of treatments.
The relative pattern of lumbar flexion/extension and pelvic rotation, as the two main contributors to the trunk motion in the sagittal plane, has been used in several earlier studies to verify its capability in differentiating between patients and healthy controls. The suggested premise behind this is that any change in this relative pattern, which for brevity will be called lumbopelvic rhythm (LPR) hereafter, could be an indication of alterations in the synergy between the active and passive contributions of lower back tissues in generating trunk motion. Therefore, changes in LPR could indirectly suggest alterations in neuromuscular control of trunk motion as well as the load (forces and deformations) distribution within the lower back tissues; both of which having an important role in development of LBP.7–9
LPR has been shown to be affected not only by the health condition (i.e. asymptomatic vs. symptomatic or different types of LBP), but also by the personal characteristics (e.g. age, gender) as well as the characteristics of trunk motion task (e.g. pace of motion, load to be lifted). Therefore, better management of LBP using the LPR measure requires an understanding of the potential effects of subject and task characteristics on LPR. Thus, the objective of this review is to summarize the current knowledge about LPR during trunk bending and return in the sagittal plane for groups of individuals with different characteristics, and under different task conditions. This study comes as a continuation of a previous review where we summarized the methods used for kinematic measurement, and characterization approaches for LPR.10 It is expected therefore, that these reviews help in establishing a platform for future study of this concept in LBP research.
Methods
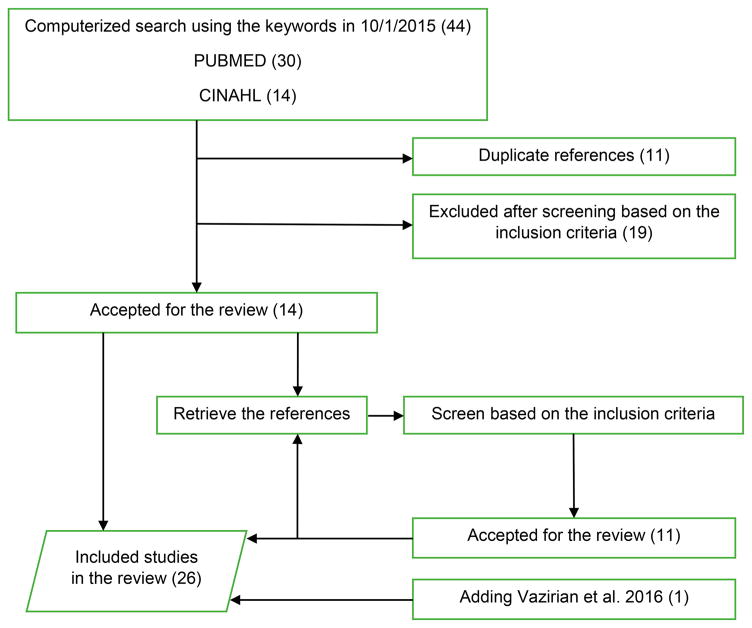
A comprehensive search was conducted to identify all of the relevant studies reporting on LPR. The PUBMED and CINAHL databases were initially searched for articles which had the following keywords in the title or abstract: ‘lumbopelvic rhythm’, ‘lumbo-pelvic rhythm’, ‘lumbar-pelvic rhythm’, ‘spino-pelvic rhythm’, ‘lumbopelvic coordination’, ‘lumbopelvic coordination’, ‘lumbar-pelvic coordination’, and ‘spino-pelvic coordination’. The initial search results were further screened for the following inclusion criteria: (1) original research using in-vivo measurements in human participants, and (2) reporting LPR for trunk motion in the sagittal plane. In addition, references of each identified study were also investigated for identification of any study that was missed in the database search. Finally, a recent study by the authors11 which meets the review inclusion criteria was added to the list of included studies (Fig. 1).
Figure 1.
Flow-chart of the literature search to find all relevant studies to LPR.
Results
Twenty-six studies met all of our criteria and were included in the review. The characteristics of participants in each sample and the experimental procedure used in each study are summarized in Table 1.
Table 1.
List of the reviewed studies
| Article | Sample
|
Tasks
|
Group | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Number | Health condition | Age | Gender | Stature | Body mass | Direction | Range of motion | Pace of motion | ||
| Paquet et al.20 | 10 | Low back pain | 41 | FB-BR | As far as possible | Slower than self-selected for normal and self-selected for patients | 1, 2 | |||
| 9 | Healthy | 41 | ||||||||
| Gracovetsky et al.29 | 5 | Healthy | 24 | Male | BR | Up to fully bent posture | Self-selected | 4, 5 | ||
| 5 | Healthy | 24 | Female | |||||||
| 5 | Healthy | 35 | Male | |||||||
| 5 | Healthy | 35 | Female | |||||||
| 5 | Healthy | 45 | Male | |||||||
| 5 | Healthy | 45 | Female | |||||||
| 5 | Healthy | 55 | Male | |||||||
| 5 | Healthy | 55 | Female | |||||||
| Nelson et al.30 | 30 | Healthy | 26 | Female | FB-BR | 90% of maximal FB | Self-selected | 5 | ||
| Esola et al.7 | 14 | Asymptomatic with a history of low back pain | 32 | Male | 182 cm | 83 kg | FB | As far as possible | Self-selected | 3 |
| 6 | Asymptomatic with a history of low back pain | 24 | Female | 163 cm | 56 kg | |||||
| 13 | Healthy | 27 | Male | 177 cm | 78 kg | |||||
| 8 | Healthy | 29 | Female | 166 cm | 63 kg | |||||
| McClure et al.21 | 12 | Asymptomatic with a history of low back pain | 34 | 180 cm | 79 kg | BR | Not instructed | Self-selected | 1, 3 | |
| 12 | Healthy | 29 | 172 cm | 69 kg | ||||||
| Porter and Wilkinson26 | 15 | Patient | 27 | Male | FB- BR | As far as comfortably possible | Self-selected | 2 | ||
| 17 | Healthy | 27 | Male | |||||||
| Tully et al.35 | 13 | Healthy | 26 | Male | 170 cm | FB | Up to touch the floor | Self-selected | 1 | |
| 9 | Healthy | 26 | Female | 170 cm | ||||||
| Granata and Sanford12 | 13 | Healthy | 24 | Male | 171 cm | 77 kg | BR | From 90° to upright | 15, 30 and 60°/second | 1, 5, 6 |
| 5 | Healthy | 24 | Female | 171 cm | 77 kg | |||||
| Lariviere et al.23 | 18 | Healthy | 40 | Male | 175 cm | 74 kg | FB-BR | Fully bent posture | One movement cycle lasted 5.45 seconds | 2 |
| 15 | Healthy | 40 | Female | 172 cm | 62 kg | |||||
| Lee and Wong13 | 20 | Healthy | 20 | Male | 171 cm | 62 kg | FB-BR | As far as possible | Self-selected | 1 |
| Wong and Lee14 | 20 | Healthy | 42 | 170 cm | 71 kg | FB-BR | As far as possible | Self-selected | 1, 2 | |
| 24 | Low back pain | 41 | Male | 172 cm | 69 kg | |||||
| 17 | Low back pain with restricted leg raise | 34 | Male | 174 cm | 71 kg | |||||
| Pal et al.16 | 20 | Healthy | 21 | Male | 180 cm | 77 kg | FB-BR | As far as possible | Self-selected | 1 |
| Thomas and Gibson15 | 8 | Healthy | 27 | Male | FB-BR | With knee flexion, to high, middle and low targets, and with knees extended, to a low target, and as far as possible | With knee flexion, self-selected, and with knees extended, twice the comfortable pace | 1, 4, 6 | ||
| 8 | Healthy | 26 | Female | |||||||
| van Wingerden et al.24 | 29 | Low back pain with pelvic girdle pain | 33 | Female | FB-BR | As far as possible | Moderate pace | 2 | ||
| 22 | Low back pain | 36 | Female | |||||||
| 53 | Healthy | 25 | Female | |||||||
| Silfies et al.22 | 23 | Healthy | 39 | Male | 170 cm | 73 kg | FB-BR | To reach a target in front of the participant’s trunk | 3 seconds reaching and 3 seconds returning | 2 |
| 12 | Healthy | 39 | Female | 170 cm | 73 kg | |||||
| 11 | Low back pain | 41 | Male | 180 cm | 85 kg | |||||
| 19 | Low back pain | 41 | Female | 180 cm | 85 kg | |||||
| Kim et al.25 | 16 | Healthy | 24 | 169 cm | 61 kg | FB-BR | Fully flexed position, then to the initial position | 3 seconds bending, 3 seconds returning | 2 | |
| 17 | Low back pain (lumbar flexion with rotation syndrome) | 23 | 173 cm | 67 kg | ||||||
| 14 | Low back pain (lumbar extension with rotation syndrome) | 24 | 169 cm | 65 kg | ||||||
| Hasebe et al.19 | 18 | Healthy | 36 | Male | 171 cm | 67 kg | FB | To touch toes | Self-selected | 1 |
| Hu et al.32 | 12 | Healthy | 26 | Male | 172 cm | 77 kg | BR | Full flexion to upright | Self-selected | 5 |
| Iwasaki et al.31 | 16 | Healthy | 22 | Male | BR | Not instructed | Self-selected | 5 | ||
| 10 | Healthy | 22 | Female | |||||||
| Lariviere et al.23 | 10 | Healthy | 26 | Male | 180 cm | 80 kg | FB-BR | As far as possible | 4 seconds bending and 4 seconds returning | 2 |
| 10 | Healthy | 27 | Female | 168 cm | 65 kg | |||||
| Phillips et al.33 | 6 | Healthy | 27 | Male | 179 cm | 79 kg | FB | To touch toes | As fast as possible, and Metronome 60 beats/minute | 5, 7 |
| 6 | Healthy | 27 | Female | 166 cm | 62 kg | |||||
| Tafazzol et al.9 | 8 | Healthy | 25 | Male | 181 cm | 80 kg | FB-BR | To their maximum voluntary bending | Self-selected | 1 |
| Hu and Ning8 | 13 | Healthy | 27 | Male | 175 cm | 69 kg | FB-BR | To 40 cm from the center of ankles | Self-selected | 5, 7 |
| Hu and Ning34 | 15 | Healthy | 26 | Male | 173 cm | 77 kg | FB-BR | To 40 cm from the center of ankles | Self-selected | 7 |
| Pries et al.27 | 134 | Healthy | 38 | Male | 180 cm | 75 kg | FB | As far as possible | Self-selected | 4 |
| 175 | Healthy | 38 | Female | 167 cm | 61 kg | |||||
| Vazirian et al.11 | 6 | Healthy | 25 | Male | 178 cm | 79 kg | FB-BR | As far as possible | Self-selected, and as fast as possible | 4, 6 |
| 6 | Healthy | 25 | Female | 165 cm | 61 kg | |||||
| 6 | Healthy | 35 | Male | 173 cm | 81 kg | |||||
| 6 | Healthy | 35 | Female | 167 cm | 65 kg | |||||
| 6 | Healthy | 45 | Male | 180 cm | 88 kg | |||||
| 6 | Healthy | 45 | Female | 166 cm | 71 kg | |||||
| 6 | Healthy | 55 | Male | 181 cm | 85 kg | |||||
| 6 | Healthy | 55 | Female | 164 cm | 71 kg | |||||
| 6 | Healthy | 65 | Male | 178 cm | 84 kg | |||||
| 6 | Healthy | 65 | Female | 165 cm | 65 kg | |||||
Letter codes under Tasks column denote: FB: forward bending, BR: backward return.
Number codes under Group column denote study of LPR are related to (1) healthy control population,( 2) current LBP, (3) history of LBP, (4) age/gender, (5) handling of external load, (6) motion pace and (7) muscle fatigue. See summary of results for details.
During the review process, we noted that the LPR has been generally studied from two main perspectives that included (1) magnitude, and (2) timing of lumbar and pelvic contributions to trunk motion. Hence, in the following sections, the findings of the reviewed studies have been summarized based on if the focus was the magnitude or the timing aspects of LPR. The summary has been organized by first reporting findings from studies involving only asymptomatic people with no history of LBP, followed by findings from studies involving individuals with a current or a past episode LBP. Thereafter, reports of changes in LPR due to differences in the characteristics of participant samples and experimental procedures are summarized.
LPR in asymptomatic people with no history of LBP
Findings from reports of the timing of lumbar and pelvic motions can be categorized into (1) simultaneous motion of the lumbar spine and pelvis with no delay,12–14 (2) simultaneous motion of the lumbar spine and pelvis with a delay,15,16 and (3) sequential motion of the lumbar spine and pelvis.17,18 Early studies of the kinematics of the lumbar spine and pelvis in asymptomatic individuals suggested a sequential contribution to the trunk motion;17,18 a suggestion that was not supported by any of the studies included in the current review. For the forward bending task, Lee and Wong,13 and Wong and Lee14 reported a zero phase delay between lumbar and pelvic motions. In contrast, Pal et al.16 reported that the initiation of motion and maximum angular velocity of the lumbar spine occurred, respectively, 9.9 and 13.3% of task duration earlier than the time of corresponding events for the pelvis. Thomas and Gibson15 also reported that the initiation of lumbar motion was 48.9 milliseconds ahead of the pelvic motion.
For the backward return task, Granata and Sanford12 reported simultaneous lumbar and pelvic motions based on the observation that the plot of lumbar motion compared to pelvic motion had no near horizontal or vertical segment. Similarly, Lee and Wong13 and Wong and Lee14 reported a zero phase delay between the lumbar and pelvic motions during the backward return. Pal et al.16 however, reported that the motion onset and peak velocity of the pelvis occurred, respectively, 4.7 and 5.2% of the task duration earlier than the corresponding time events for the lumbar spine during the backward return. Similar observations to those by Pal et al.16 have been reported by Thomas and Gibson15 with the pelvic motion reported to start 63 milliseconds ahead of the lumbar motion but only for the backward return from a middle and low height target. For the backward return started from a high height target (i.e. small trunk flexion), the same authors observed no phase difference. Such findings were consistent with the results from Lee and Wong,13 Wong and Lee,14 and Granata and Sanford.12
For the magnitude aspects of LPR, the general observation in the studies reviewed was that the lumbar contribution to forward bending is dominant in the early stage of the trunk motion, whereas the pelvic contribution gradually increases and becomes dominant toward the end range of the trunk motion.7,9,13,16,19,20 Thomas and Gibson15 reported larger lumbar contribution during the second quartile than the first quartile of forward bending. The reported lumbar to pelvic contribution ratios in their study were 1.8:1 and 1.6:1, respectively.
Inversely, it was reported that the early stage of backward return was accomplished primarily by pelvic motion, whereas the late stage of the backward return was accomplished primarily by lumbar spine motion.9,12,13,16,20,21 The only exception to this general observation was a study by Pal et al.,16 wherein equal contributions from the lumbar spine and pelvis were reported throughout the middle and late stages of backward return.
LPR and current episode of LBP
There is no consensus in the reports of differences in the timing aspect of LPR between people with and without a current episode of LBP. Wong and Lee14 reported that participants with LBP, similar to asymptomatic participants, demonstrated a simultaneous lumbar and pelvic motion both in forward bending and backward return. Paquet et al.20 similarly suggested no significant difference in the timing of lumbar relative to pelvic coordination between people with LBP versus people without current LBP. Paquet et al.20 further divided their LBP group into two subgroups and found that those who had significantly more in-phase lumbar and pelvic motion than the control group used pelvic motion for the earlier stage of the forward bending, and the terminal stage of the backward return. In another study, Silfies et al.22 observed that patients with LBP had a higher mean relative phase between the lumbar spine and pelvis than the control group in forward bending and backward return (i.e. more sequential motion).
In general, it has been suggested that in the presence of LBP the lumbar contribution in forward bending and backward return decreases.20,23–26 Lariviere et al.23 reported that the lumbar contribution was significantly smaller in people with LBP compared to people without LBP. They further noticed that such differences were not affected by the presence of a 12 kg external load. Porter and Wilkinson26 also reported a smaller lumbar contribution in people with chronic LBP compared to people without LBP. However, this occurred only during the early stage of the forward bending (0–15°).
van Wingerden et al.24 compared the lumbar and pelvic contribution between a group of patients with LBP and a group of pelvic girdle pain patients. The investigators observed that patients with LBP tended to maintain a lordosis (less lumbar motion) during forward bending. In contrast, the pelvic girdle pain patients displayed lumbar motion in the initial phase of forward bending. However, a higher lumbar contribution was reported for both patient groups as compared to controls toward the end range of forward bending.
A similar study was conducted by Kim et al.25 wherein the investigators compared the LPR between two subgroups of LBP patients; patients with lumbar flexion with rotation syndrome, and patients with lumbar extension with rotation syndrome, and a control group. The group with lumbar flexion with rotation syndrome showed less pelvic and excessive lumbar motion compared to the control group. The group with lumbar extension with rotation syndrome showed more pelvic and less lumbar motion than the control group. The reported patterns were observed during both forward bending and backward return.
LPR and history of LBP
The differences in LPR of people with a history of LBP compared to those without a history of LBP have been investigated in two studies. The goal of the two studies was to understand the reason why asymptomatic people with a history of LBP are susceptible to a recurrence of LBP. The participants with a history of LBP were reported to have a smaller lumbar contribution during the middle stage of forward bending (30–60°) compared to participants without a history of LBP as reflected in the reported lumbar to pelvic ratios of 0.72:1 compared to 1.06:1.7 During the early stage of backward return though, the lumbar contribution was reported to be larger in people with a history of LBP compared to those without a history of LBP.21
LPR and age and gender
Pries et al.27 reported a smaller lumbar and larger pelvic contribution to trunk motion at the end range of trunk forward bending in older individuals compared to younger individuals, as well as in females compared to the males. Vazirian et al.11 studied the differences in the lumbar contribution in four quartiles of forward bending and backward return between five age groups spanning from 20 to 70 years old. The investigators reported a smaller lumbar contribution in the groups older than 50 years, in the males and females, as well as a smaller lumbar contribution in females versus males in all of the quarters of forward bending and backward return. However, Thomas and Gibson15 observed no effect of gender on the magnitudes of lumbar and pelvic contribution in forward bending and backward return. For the backward return task, Lariviere et al.28 reported larger contribution from the lumbar spine in males compared to females. Gracovetsky et al.29 reported that older participants experienced a smaller lumbar contribution throughout the backward return compared to younger participants.
LPR and external load
In general, the lumbar and pelvic motions during forward bending in the presence of external load has been reported to become more synchronous.8,30 For the backward return, however, the reports about the timing of lumbar and pelvic contributions are inconsistent. Nelson et al.30 reported a relatively sequential pattern of lumbar and pelvic motions with the lumbar motion being ahead of the pelvic, when lifting a 9.5 kg load. Similarly, Iwasaki et al.31 observed that compared to a no load condition, the initiation of lumbar motion was delayed when lifting an external load that was 20% of the participant’s body weight. Hu et al.32 found out that compared to lifting no load, lifting a 9 kilogram weight from the ground reduced the mean relative phase between the lumbar spine and pelvis (i.e. the lumbar and pelvic motions became more synchronous except during the first quartile of backward return). There have also been reports of simultaneous lumbar and pelvic motions during the backward return in the presence of load.8,12
For the forward bending task, an increase of approximately 10% in the lumbar contribution was reported by Phillips et al.33 for different stages of a fast forward bending task with added weight (~11 kg) to the trunk. For the backward return task, investigators report either no effect29 or an increase in the lumbar contribution12 due to the external load. Granata and Sanford12 reported an increase of approximately 1.3 in the ratio of lumbar to pelvic contribution when the external load increased from 0.1 to 10 kg in backward return. However, Gracovetsky et al.29 reported no effect of external load on the lumbar and pelvic contribution during the early stage of backward return (i.e. up to 60° of the trunk motion) even with heavy loads up to 45 kg.
LPR and trunk pace
Increasing the pace while lifting a load has been suggested to reduce the sequential nature of the pelvic and lumbar motions.12 For the forward bending task, Thomas and Gibson15 observed that increasing the pace of the trunk motion, in contrast to presence of external load, was associated with a reduction in the lumbar contribution. Granata and Sanford12 similarly reported a reduction in the total lumbar contribution with increasing the pace in backward return, but only in the presence of an external load.
LPR and fatigue
Hu and Ning34 reported that with a 9 kg weight, the mean relative phase of the lumbar spine and pelvis was reduced by ~0.05 rad (i.e. became more in phase) due to the erector spinae muscle fatigue in backward return. By further dividing the total lifting duration into four intervals, Hu and Ning observed that the relative phase became lower due to fatigue in all except the first interval of the backward return. In another study, the same investigators also noted that fatigue resulted in an increased lumbar contribution during both the forward bending and backward return tasks. Finally, while not involving a specific trunk muscle fatiguing protocol, Phillips et al.33 reported an increased lumbar contribution at different stages of fast forward bending following a 45-minute brisk treadmill walk while carrying body armor.
Conclusion
There is a general consensus among the reviewed studies that the lumbar contribution is predominant during the early stages of forward bending as well as later stages of backward return; a contribution that decreases at larger trunk flexion angles. In contrast to increasing the pace of trunk motion, the presence of external load was reported to delay and increase the lumbar contribution in backward return. The lumbar contribution has been reported to reduce with aging and to be less (or equal) among females as compared to males in forward bending and backward return. In contrast to healthy individuals, asymptomatic people with a history of LBP have a smaller lumbar contribution during the middle stage of forward bending, and a larger lumbar contribution during early stages of backward return. Different reports of timing and magnitude of lumbar and pelvic contribution to trunk motion have been reported for people in a current episode of LBP. Given the complexity and multifactorial nature of LBP, these differences could have been in part due to the heterogeneity in the populations of patients with LBP in the reviewed studies. Depending on the source of LBP, similar, larger, or smaller lumbar contribution have been reported among people in an episode of LBP compared to those not in an episode of LBP. Another potential source of variability in the results of the reviewed studies, could be the differences in methods used to measure the motion, and approaches used to characterize the LPR.10
Acknowledgments
Funding This work was supported in part by a funding from the Centers for Disease Control and Prevention (R21OH010195) and a funding from the National Institute of Child Health and Development/National Center for Medical Rehabilitation Research (R01 HD047709).
Footnotes
Disclaimer statements
Contributors None.
Conflicts of interest The authors report no conflicts of interest.
Ethics approval None.
ORCiD
Milad Vazirian, http://orcid.org/0000-0001-6771-5148
Linda R. Van Dillen, http://orcid.org/0000-0002-3845-4783
References
- 1.Hoy D, Brooks P, Blyth F, Buchbinder R. The epidemiology of low back pain. Best Pract Res Clin Rheumatol. 2010;24(6):769–81. doi: 10.1016/j.berh.2010.10.002. [DOI] [PubMed] [Google Scholar]
- 2.Hoy D, Bain C, Williams G, March L, Brooks P, Blyth F, et al. A systematic review of the global prevalence of low back pain. Arthritis Rheum. 2012;64(6):2028–37. doi: 10.1002/art.34347. [DOI] [PubMed] [Google Scholar]
- 3.Hoy D, March L, Brooks P, Blyth F, Woolf A, Bain C, et al. The global burden of low back pain: estimates from the Global Burden of Disease 2010 study. Ann Rheum Dis. 2014;73(6):968–74. doi: 10.1136/annrheumdis-2013-204428. [DOI] [PubMed] [Google Scholar]
- 4.Deyo RA, Weinstein JN. Low back pain. N Engl J Med. 2001;344(5):363–70. doi: 10.1056/NEJM200102013440508. [DOI] [PubMed] [Google Scholar]
- 5.Veizi E, Hayek S. Interventional therapies for chronic low back pain. Neuromodulation. 2014;17(Suppl 2):31–45. doi: 10.1111/ner.12250. [DOI] [PubMed] [Google Scholar]
- 6.Salzberg L. The physiology of low back pain. Prim Care. 2012;39(3):487–98. doi: 10.1016/j.pop.2012.06.014. [DOI] [PubMed] [Google Scholar]
- 7.Esola MA, McClure PW, Fitzgerald GK, Siegler S. Analysis of lumbar spine and hip motion during forward bending in subjects with and without a history of low back pain. Spine (Phila Pa 1976) 1996;21(1):71–78. doi: 10.1097/00007632-199601010-00017. [DOI] [PubMed] [Google Scholar]
- 8.Hu B, Ning X. The changes of trunk motion rhythm and spinal loading during trunk flexion and extension motions caused by lumbar muscle fatigue. Ann Biomed Eng. 2015;43:2112–9. doi: 10.1007/s10439-015-1248-0. [DOI] [PubMed] [Google Scholar]
- 9.Tafazzol A, Arjmand N, Shirazi-Adl A, Parnianpour M. Lumbopelvic rhythm during forward and backward sagittal trunk rotations: Combined in vivo measurement with inertial tracking device and biomechanical modeling. Clin Biomech (Bristol, Avon) 2014;29(1):7–13. doi: 10.1016/j.clinbiomech.2013.10.021. [DOI] [PubMed] [Google Scholar]
- 10.Vazirian M, Van Dillen LR, Bazrgari B. Lumbopelvic rhythm during trunk motion in the sagittal plane: A review of the kinematic measurement methods and characterization approaches. Phys Ther Rehabil. 2016;3:1–9. doi: 10.7243/2055-2386-3-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vazirian M, Shojaei I, Bazrgari B, Agarwal A. Lumbar contribution to the trunk forward bending and backward return; age-related differences. Ergonomics. 2016:1–26. doi: 10.1080/00140139.2016.1237676. [DOI] [PubMed] [Google Scholar]
- 12.Granata KP, Sanford AH. Lumbar-pelvic coordination is influenced by lifting task parameters. Spine (Phila Pa 1976) 2000;25(11):1413–18. doi: 10.1097/00007632-200006010-00014. [DOI] [PubMed] [Google Scholar]
- 13.Lee RY, Wong TK. Relationship between the movements of the lumbar spine and hip. Hum Mov Sci. 2002;21(4):481–94. doi: 10.1016/s0167-9457(02)00117-3. [DOI] [PubMed] [Google Scholar]
- 14.Wong TK, Lee RY. Effects of low back pain on the relationship between the movements of the lumbar spine and hip. Hum Mov Sci. 2004;23(1):21–34. doi: 10.1016/j.humov.2004.03.004. [DOI] [PubMed] [Google Scholar]
- 15.Thomas JS, Gibson GE. Coordination and timing of spine and hip joints during full body reaching tasks. Hum Mov Sci. 2007;26(1):124–40. doi: 10.1016/j.humov.2006.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pal P, Milosavljevic S, Sole G, Johnson G. Hip and lumbar continuous motion characteristics during flexion and return in young healthy males. Eur Spine J. 2007;16(6):741–7. doi: 10.1007/s00586-006-0200-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Farfan HF. Muscular mechanism of the lumbar spine and the position of power and efficiency. Orthop Clin North Am. 1975;6(1):135–44. [PubMed] [Google Scholar]
- 18.Davis PR, Troup JD, Burnard JH. Movements of the thoracic and lumbar spine when lifting: a chrono-cyclophotographic study. J Anat. 1965;99:13–26. [PMC free article] [PubMed] [Google Scholar]
- 19.Hasebe K, Sairyo K, Hada Y, Dezawa A, Okubo Y, Kaneoka K, et al. Spino-pelvic-rhythm with forward trunk bending in normal subjects without low back pain. Eur J Orthop Surg Traumatol. 2014;24(Suppl 1):S193–S199. doi: 10.1007/s00590-013-1303-1. [DOI] [PubMed] [Google Scholar]
- 20.Paquet N, Malouin F, Richards CL. Hip-spine movement interaction and muscle activation patterns during sagittal trunk movements in low back pain patients. Spine (Phila Pa 1976) 1994;19(5):596–603. doi: 10.1097/00007632-199403000-00016. [DOI] [PubMed] [Google Scholar]
- 21.McClure PW, Esola M, Schreier R, Siegler S. Kinematic analysis of lumbar and hip motion while rising from a forward, flexed position in patients with and without a history of low back pain. Spine (Phila Pa 1976) 1997;22(5):552–8. doi: 10.1097/00007632-199703010-00019. [DOI] [PubMed] [Google Scholar]
- 22.Silfies SP, Bhattacharya A, Biely S, Smith SS, Giszter S. Trunk control during standing reach: a dynamical system analysis of movement strategies in patients with mechanical low back pain. Gait Posture. 2009;29(3):370–6. doi: 10.1016/j.gaitpost.2008.10.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lariviere C, Gagnon D, Loisel P. The effect of load on the coordination of the trunk for subjects with and without chronic low back pain during flexion-extension and lateral bending tasks. Clin Biomech (Bristol, Avon) 2000;15(6):407–16. doi: 10.1016/s0268-0033(00)00006-1. [DOI] [PubMed] [Google Scholar]
- 24.van Wingerden JP, Vleeming A, Ronchetti I. Differences in standing and forward bending in women with chronic low back or pelvic girdle pain: indications for physical compensation strategies. Spine (Phila Pa 1976) 2008;33(11):E334–E341. doi: 10.1097/BRS.0b013e318170fcf6. [DOI] [PubMed] [Google Scholar]
- 25.Kim MH, Yi C-H, Kwon O-Y, Cho S-H, Cynn H-S, Kim Y-H, et al. Comparison of lumbopelvic rhythm and flexion-relaxation response between 2 different low back pain subtypes. Spine (Phila Pa 1976) 2013;38(15):1260–7. doi: 10.1097/BRS.0b013e318291b502. [DOI] [PubMed] [Google Scholar]
- 26.Porter JL, Wilkinson A. Lumbar-hip flexion motion. A comparative study between asymptomatic and chronic low back pain in 18- to 36-year-old men. Spine (Phila Pa 1976) 1997;22(13):1508–13. doi: 10.1097/00007632-199707010-00017. discussion 1513–4. [DOI] [PubMed] [Google Scholar]
- 27.Pries E, Dreischarf M, Bashkuev M, Putzier M, Schmidt H. The effects of age and gender on the lumbopelvic rhythm in the sagittal plane in 309 subjects. J Biomech. 2015;48:3080–7. doi: 10.1016/j.jbiomech.2015.07.030. [DOI] [PubMed] [Google Scholar]
- 28.Lariviere C, Caron J-M, Preuss R, Mecheri H. The effect of different lumbar belt designs on the lumbopelvic rhythm in healthy subjects. BMC Musculoskelet Disord. 2014;15:307. doi: 10.1186/1471-2474-15-307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gracovetsky S, Newman N, Pawlowsky M, Lanzo V, Davey B, Robinson L. A database for estimating normal spinal motion derived from noninvasive measurements. Spine (Phila Pa 1976) 1995;20(9):1036–46. doi: 10.1097/00007632-199505000-00010. [DOI] [PubMed] [Google Scholar]
- 30.Nelson JM, Walmsley RP, Stevenson JM. Relative lumbar and pelvic motion during loaded spinal flexion/extension. Spine (Phila Pa 1976) 1995;20(2):199–204. doi: 10.1097/00007632-199501150-00013. [DOI] [PubMed] [Google Scholar]
- 31.Iwasaki R, Yokoyama G, Kawabata S, Suzuki T. Lumbar extension during stoop lifting is delayed by the load and hamstring tightness. J Phys Ther Sci. 2014;26(1):57–61. doi: 10.1589/jpts.26.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hu B, Ning X, Nussbaum MA. The influence of hand load on lumbar-pelvic coordination during lifting task. Human Factors and Ergonomics Society 58th Annual Meeting; 2014. [Google Scholar]
- 33.Phillips M, Bazrgari B, Shapiro R. The effects of military body armour on the lower back and knee mechanics during toe-touch and two-legged squat tasks. Ergonomics. 2015;58:492–503. doi: 10.1080/00140139.2014.970589. [DOI] [PubMed] [Google Scholar]
- 34.Hu B, Ning X. The influence of lumbar extensor muscle fatigue on lumbar-pelvic coordination during weight lifting. Ergonomics. 2015;58:1424–32. doi: 10.1080/00140139.2015.1005173. [DOI] [PubMed] [Google Scholar]
- 35.Tully EA, Wagh P, Galea MP. Lumbofemoral rhythm during hip flexion in young adults and children. Spine. 2002;27:E432–40. doi: 10.1097/00007632-200210150-00013. [DOI] [PubMed] [Google Scholar]