Abstract
Public health field services for sexually transmitted infections (STIs) have not adequately evolved to address the expanding scale of the STI problem, its concentration among men who have sex with men, the emergence of new communication technologies and the availability of antiretroviral therapy as a cornerstone of HIV prevention. Field services need to modernize. Modernization should seek to expand field services objectives beyond sex partner STI testing and treatment to include: HIV testing of persons with bacterial STI and their partners, including efforts to promote frequent HIV/STI testing; increased condom access; linkage and relinkage to HIV care and promotion of viral suppression; PrEP promotion; linkage to long acting contraception; and referral for health insurance. Field services programs cannot advance these new objectives while simultaneously doing all of the work they have traditionally done. Modernization will require a willingness to reconsider some longstanding aspects of field services work, including the centrality of face-to-face interviews and field investigations. Health departments seeking to modernize will need to carefully assess their ongoing activities and reorganize to align the use of field services resources with program priorities. In some instances, this may require reorganization to allow staff greater specialization and closer integration with surveillance activities. Adapting programs will require new staff training, improvements in data management systems, and a greater investment in monitoring and evaluation. While modernization is likely to evolve over many years, the time to start is now.
Starting in the 1940s, U.S. health departments began employing outreach staff to increase the evaluation and treatment of the sex partners of persons with syphilis. Originally referred to as contact tracing and subsequently renamed partner notification, partner counseling and referral services and then partner services, the activity has evolved surprisingly little over the last seven decades. Scientific progress - particularly evidence demonstrating the effectiveness of antiretroviral drugs in preventing HIV transmission – has greatly expanded the potential utility of public health outreach. This progress has prompted some health departments to rename their outreach teams using the term field services, in part to reflect the wider array of outcomes they now seek to advance. Field services is now in a state of transition. In this paper we discuss the factors promoting change, the new outcomes that field services might evolve to address, how addressing new outcomes might require modifications in field services procedures to improve efficiency, and how modernization may require changes in public health infrastructure. Many of the changes we propose do not have strong data to support them. However, public health practice typically evolves through a process program implementation and quality improvement, and this reality will likely continue to guide most field services practices in the years to come.
The evolving context of field services
Changes in the focus of STI control
The STIs that public health agencies seek to control have changed since the dawn of post-World War II era. In the 1940s, field services focused on the control of syphilis. The country developed a cadre of professionals, usually called Disease Intervention Specialists (DIS), who interviewed persons with syphilis and sought to ensure their sex partners’ medical evaluation and treatment. In the 1970s, STI programs expanded to include efforts to control gonorrhea1,2, and by 1984 health departments were providing partner services to over 350,000 persons with gonorrhea annually3.
Changes in the science and epidemiology of STI in the 1980s proved beyond field services programs’ capacity to adapt. Physicians described the first cases of AIDS in 19814, and by 1992 over 70,000 cases had been reported to CDC5. Although some health departments applied traditional partner services approaches almost immediately to the new epidemic6, many did not. Concerns about patient confidentiality, the largely untreatable nature of HIV infection in the first 15 years of the epidemic, the social marginalization and widespread bigotry directed against persons with HIV infection and populations at high risk for HIV, particularly men who have sex with men (MSM), and the associated emergence of an increasingly empowered HIV advocacy movement all contributed to public health officials’ reluctance to routinely apply traditional STI control measures to HIV7. This reluctance was reinforced by the organizational structure of public health, which often separated HIV from other STIs. HIV control programs at both the local and federal level failed to consistently integrate partner services8.
Field services also failed to develop a viable response to the emergence of chlamydial infection as a STD control priority. The sheer number of cases presented STI programs with a mismatch between the scale of the STI problem and the resources and methods available to address it. In 2001, while over 80% of all cases of early syphilis in the U.S. received partner services, only approximately one-third of cases of newly diagnosed HIV infection and fewer than 20% of persons with gonorrhea or chlamydial infection were interviewed by DIS9. The system was hidebound by tradition and slow to adapt.
Some of the barriers to applying partner services have diminished over the last decade. Many state and local health departments have integrated HIV and STI programs; public health agencies, including CDC, now advocate the provision of partner services to all persons with newly diagnosed HIV infection10; and the development of expedited partner therapy (EPT) for gonorrhea and chlamydial infection represents an alternative partner management strategy better suited than traditional partner services to the scale of the problem presented by these STIs11. Despite these developments, the system has yet to fully adapt to address the emergence of HIV as the priority STI or the scale and diversity of STIs that affect the public health.
Changes in communication technology and the social organization of sex
The social organization of sex has dramatically changed over the last decade in ways that have undermined the effectiveness of traditional partner services. Starting in the 1990s, the internet began to alter how persons with STIs met their partners, a trend which has accelerated with the advent of geosocial networking applications (GSN apps)12–14. Some health departments have developed protocols allowing DIS to contact persons with STIs and their sex partners via websites or text messages and, to a lesser extent, using GSN apps15–18. However, confidentiality and legal concerns, inadequate DIS training and skill in the use of these technologies, and limitations inherent in electronic communications – which are easily ignored or blocked - have limited the ability of DIS to contact persons with STIs and their partners via the internet and GSN apps. GSN apps are particularly problematic as users do not typically maintain a permanent profile through which they can be contacted, limiting the ability of both index patients (i.e. persons diagnosed with an STI) and DIS to contact potentially exposed partners. The net effect of these changes has been a general sense that it is easier than ever for persons to find anonymous or near anonymous sex partners, and harder than in the past for DIS to identify and communicate with those partners.
Changes in the populations affected by STI
HIV and syphilis, the STIs for which field services are typically used in the U.S., are increasingly concentrated in MSM. In 2015, approximately 65% of the 23,872 primary and secondary syphilis cases and 70% of 39,513 new HIV diagnoses in the U.S. occurred among MSM19,20, a group that comprises approximately 2% of the U.S. population21. HIV is increasingly concentrated among young, African American MSM in the southern U.S.22 Although existing data suggest that MSM with STIs notify at least one partner roughly as often as heterosexuals with STIs, as a group, MSM have substantially more partners than heterosexuals. As a result, partner notification efforts, either by patients or by health departments, result in a much smaller proportion of MSM than heterosexual partners being tested and treated23.
In summary, the country confronts an HIV epidemic that is highly concentrated among MSM, particularly young, minority MSM in poorer, more socially conservative parts of the U.S. That epidemic is accompanied by rising rates of bacterial STI, and occurs in the context of sexual networks that are increasingly formed via electronic communications which facilitate anonymous or near anonymous sex and which often leave very limited or no permanent records. In this situation, the utility of traditional partner notification tools, which rely heavily on face-to-face interviews and field investigation, is uncertain. We do not favor abandoning efforts to identify, test and treat the sex partners of persons with HIV/STI. However, the contemporary epidemiology of HIV/STI in the U.S. and the context in which transmission occurs requires us to fundamentally rethink how we approach outreach to persons with HIV/STI.
New opportunities: expanding and goals of field services
The problems we face are serious and will not be easily overcome, but we are not bereft of effective interventions or promising opportunities. We have good evidence that condoms prevent the transmission of a wide array of STIs24, that people who test HIV positive change their behavior to protect their sex partners25,26, and that antiretroviral medications, if taken consistently by persons with HIV infection or persons at risk for HIV infection, reduces the risk of HIV transmission by over 90%27,28. The U.S. National HIV/AIDS Strategy is focused on the use of HIV testing, treatment and pre-exposure prophylaxis (PrEP) to control the HIV epidemic29. This focus should prompt public health programs to reconsider the goals of field services. Tables 1 and 2 present program outcomes and associated evaluation metrics that health departments should consider integrating into field services programs.
Table 1.
Expanded field services outcomes and changes in public health infrastructure, policy and procedures that may be required to institute change
| Field Services Outcomes | Potential Areas for change in procedures | Potential changes in policy, training and infrastructure |
|---|---|---|
| Partner notification, testing and treatment |
|
|
| HIV testing and retesting of index cases with STIs and high-risk partners of persons with HIV/STI |
|
|
| Increase condom use |
|
|
| Referral for PrEP |
|
|
| Linkage to HIV care |
|
|
| Relinkage to HIV care |
|
|
| Increase use of effective contraception |
|
|
| Referral for health insurance |
|
|
Table 2.
Expanded field services outcomes, populations in which outcomes should be measured and program evaluation metrics
| Field Services Outcomes | Populations in which outcome may be relevant | Proposed Program Evaluation Metrics |
|---|---|---|
| Partner notification, testing and treatment | Newly diagnosed HIV infection Bacterial STI HIV-infected index patients and partners who are out of care |
|
| HIV testing and retesting | Index cases with bacterial STIs Partners of index cases receiving STI partner services |
|
| Increase condom use | Index cases and partners receiving HIV or STI partner services |
|
| Referral for PrEP | Index cases at high risk for HIV receiving STI partner services+ Sex partners of persons with HIV or early syphilis |
|
| Linkage to HIV care | Index cases receiving HIV partner services |
|
| Relinkage to HIV care | Index cases receiving STI partner services who are found to be out of care, partners of persons receiving partner services found to be out of care |
|
| Increase use of effective contraception | Women receiving partner services and female partners of persons receiving partner services who do not desire pregnancy and are not using long-acting contraception |
|
| Referral for health insurance | Uninsured persons (index cases ore partners) identified through partner services |
|
Outcomes should be evaluated using verified (confirmed by DIS) and unverified dispositions (index patient report alone). Also, timing of partner HIV notification and testing relative to index patient interview should ideally be measured to define notification and testing occurring prior to PS intervention. Outcomes best evaluated as indices (events per index case receiving PS)
PrEP referral should ideally be guided by local epidemiology on HIV risks. Throughout the U.S., persons with an HIV-infected sex partner who is not on antiretrovirals, MSM with early syphilis or rectal gonorrhea and MSM who use methamphetamine are at high risk for HIV and should be offered PrEP.
Condom use should ideally be monitored at the population-level using sentinel (e.g. STD clinic data) and population-based (e.g. National HIV Behavioral Surveillance, Behavioral Risk Factor Surveillance) surveillance sources of data.
DIS should ask all HIV-infected persons contacted through partner services if they have an HIV medical provider, when they last saw that provider, when they are scheduled to see their provider next, and if they are taking ART. Persons without a medical provider or with no follow-up planned should be relinked to care. Public health programs should seek to promote universal ART use through partner services.
HIV Testing
At least among MSM, few if any risk factors are as consistently associated with testing HIV positive as having a bacterial STI30–32s. Although CDC recommends that all persons with bacterial STIs be tested for HIV infection33s, only approximately half of persons with gonorrhea test for HIV near the time of their diagnosis34s. Testing rates are particularly low among persons tested outside of STD clinics and other clinical sites that focus on sexual health35s. Australian data demonstrate that text message reminders can increase testing rates, and mathematical models suggest that increasing testing frequency can diminish HIV transmission36,37s. These data provide a strong rationale for integrating the promotion of HIV testing into field services programs. Such efforts should seek to increase the proportion of persons with STIs who test for HIV, and to promote more frequent HIV/STI testing among persons at high risk for HIV/STI. An effort to integrate HIV testing into partner services for gonorrhea and chlamydial infection among MSM in WA State demonstrated that such efforts increase HIV testing among both index patients and their partners35,38s.
PrEP referral
Being diagnosed with a bacterial STI is associated with future HIV acquisition among MSM39–41s. This association is particularly strong among MSM with early syphilis and rectal gonorrhea. PrEP guidelines specifically identify the occurrence of STI as an indication for PrEP42,43s. Because STIs are reportable, they may represent a means through which health departments can promote population-based PrEP use in an identifiable high risk population. Such efforts are greatly facilitated by STI case-reporting that includes gender of sex partners, which is routine in some states, including Washington and Florida. Since 2014, our HIV/STD program in Seattle has integrated PrEP referral into partner services for MSM with bacterial STIs. Initial evaluation of this effort suggests that roughly one in four men accept PrEP referrals, with many initiating PrEP in our STD clinic44s. Of note, our STD clinic’s PrEP program relies on field services staff to organize patient’s receipt of medication and follow-up.
Initial linkage to HIV care
CDC now promotes population-based HIV partner services10. Such services use HIV surveillance data to identify persons with newly diagnosed HIV infection and refer them to field services for investigation. Traditionally, these investigations have focused on partner notification and testing, and have not explicitly identified linkage to care as an outcome for which field services staff are accountable. Since 2006, Public Health Seattle-King County (PHSKC) has defined linkage to care as the responsibility of DIS providing HIV partner services, and has measured linkage to care as an explicit investigation outcome. DIS offer all persons with newly diagnosed HIV an opportunity to see a medical provider at our STD clinic for laboratory testing (i.e. CD4 lymphocyte count and HIV RNA testing), counseling and assistance linking to ongoing medical care. Patients can typically see a provider within 48 hours. We believe that this effort, which marries partner services and linkage to care, has been instrumental in allowing us to consistently link approximately 95% of persons with newly diagnosed HIV to care within 3 months of HIV diagnosis45s. The New York City field services program has also associated receipt of partner services with successful linkage to care46s.
Relinkage to care
The occurrence of a bacterial STI is an opportunity to assess engagement in care and viral suppression in persons with a prior HIV diagnosis, to relink persons with HIV to care and to promote the use of antiretroviral therapy (ART). This should be a routine, measured effort in STD clinics and among persons receiving field services. Several states currently link STD and HIV surveillance data to identify persons with bacterial STIs who have previously diagnosed HIV infection. This is typically undertaken for purposes of partner notification and testing, though the effectiveness of these efforts, which often affect persons who serosort and who are virologically suppressed, is uncertain. On the other hand, linking STI and HIV surveillance databases or giving DIS access to HIV surveillance data that include viral load results, it is possible to identify HIV-infected persons who are not virally suppressed. Prioritizing these persons for field services with the goals of helping them relink to HIV care and treatment, and assisting their partners with HIV/STI testing and linkage to HIV care or PrEP, could be a more effective use of resources.
STI partner services are only one activity though which field services teams may use surveillance data to relink out of care persons with HIV care or promote the use of ART. CDC recently dubbed this activity “Data-to-Care”.47s DIS, who are accustomed to performing outreach, have or could have access to HIV surveillance data, and are trained in field investigation, are well poised to undertake this work. However, initial Data-to-Care efforts, which have typically relied on surveillance data to identify persons thought to be out of care, have met with limited success, in large measure because many persons thought to be out of care have migrated out of the area where they were diagnosed or are incorrectly classified as unsuppressed based on incomplete surveillance data48–50s. The limitations affecting early Data-to-Care efforts in no way diminish the importance of increasing population-level viral suppression, but they do highlight the need to develop a variety of means for identifying HIV-infected persons who are inadequately treated. With that idea in mind, HIV/STI programs, including field services programs, should seek to integrate relinkage into all work undertaken with HIV-infected persons.
Contraception
Although much of our focus is on MSM, STI remain a critical women’s health concern. Noncontracepting women with STIs have an extremely high risk for unintended pregnancy51s. While simply referring noncontracepting women with STIs to family planning is ineffective51s, the development and expanded availability of safe, long-acting contraception should prompt renewed efforts to integrate family planning and STI related outreach. Such efforts are likely to require a combination of active referral, patient navigation, and direct provision of services rather than just dissemination of information.
Revising field services procedures
Field services staff are busy. Absent a large infusion of new funds, DIS cannot undertake the work we describe above and continue doing all of their current work. In particular, focusing on linkage and relinkage to care and PrEP requires DIS to follow-up with patients, a process that is often time consuming. However, it’s not clear that all of the work DIS currently do is a high priority, or that all of the methods DIS currently employ represent an ideal balance between productivity and efficiency. Traditional partner services emphasize a model of investigation developed decades ago to control syphilis. The value of this approach needs to be challenged as field services staff develop a more variable approach to intervention based on the population affected, the STI being investigated, and the objectives of the investigation.
Telephone interviews and field investigations
Most field services programs emphasize the rapid initiation and completion of investigations, face-to-face interviews with index patients and partners, and field investigations (i.e. going to a patient or partner’s home, place of work, or other locations to conduct interviews). This approach is time-consuming and costly, and it is uncertain how much such efforts improve outcomes over those achievable with less labor intensive efforts. In King County, we conduct most partner notification interviews, including interviews for HIV infection and syphilis, by telephone. DIS interview STD clinic patients face-to-face and field investigations are reserved for persons who DIS cannot reach by telephone. Analyzing program outcomes, we found that face-to-face interviews were associated with more partners of persons with HIV and early syphilis being named and tested, but the benefits of face-to-face interviews on the more critical outcomes of new case identification were mixed. Face-to-face interviews were associated with greater HIV case-finding, but no increase in the number of partners diagnosed and treated for syphilis (i.e. the brought to treatment index)52s. New York City recently reported changing their HIV partner services procedures to allow DIS to interview partners of persons with HIV via telephone or Face Time, a change that facilitated a very large increase in the number of persons their program was able to serve53s. Telephone-based partner services have also been successfully employed for chlamydial infection in Sweden54s.
Additional data on the relative value of face-to-face vs. telephone interviews are needed. However, given the competing demands on field services staff, programs should reconsider procedures that require immediate initiation of field investigations and experiment with more flexible, less labor intensive models of work. These might be pilot tested in persons with syphilis who are HIV positive and virally suppressed, and expanded based on experience.
Text messaging and the use of geosocial networking apps
Field services programs need to be able to text message patients and partners. The primary barrier to this innovation is concern related to confidentiality. However, this concern should not be a barrier to texting messages that do not contain personal health information (PHI); communication of non-PHI is not governed by the Health Insurance Portability and Accountability Act (HIPAA). Ideally, DIS would be able to send a series of text messages to patients and their partners with increasing levels of personal information sent to persons who do not respond to initial messages. DIS also need to develop means to identify and contact partners that index patients meet using GSN apps. Many departments forbid DIS from accessing apps, and relatively few DIS have experience using them in their work. Developing and disseminating approaches using apps to identify and contact partners is critical to successful field services modernization. CDC’s toolkit on the use of new technologies for partner services is an excellent resource for field services programs interested in expanding their use of new communication technologies55s.
Timeliness of investigation
Many field services programs place a premium on the rapid initiation and completion of cases. Rapidly initiating STI cases that are highly infectious is important. However, for non-acute HIV infection the emphasis on timeliness should be balanced by recognition of the fact that most persons diagnosed with HIV have been infected for months to years. Their daily risk of transmitting HIV is typically low. As a result, there is usually no urgency to initiate a field investigation in the first days following report of a case, and no urgency to close the case. Moreover, ensuring linkage to care is more important than rapidly closing cases. In King County, our practice is to make multiple attempts at contacting persons with HIV by telephone before initiating field investigations. We leave cases open until DIS confirm that patients have successfully linked to care, or until a team that includes the DIS supervisor, surveillance staff, and program leadership agree that additional efforts to achieve linkage are futile.
Non-investigatory work
Many programs expend significant DIS resources giving patients face-to-face HIV/STI test results. Requiring patients to return to STD clinics to receive results is an antiquated practice that imposes significant burden on patients and clinics, is inconsistent with standards of care in other healthcare organizations, creates a disparity in healthcare quality for the mostly uninsured and otherwise vulnerable patients who seek care in STD clinics, and should be abandoned. Allowing patients to receive results by telephone or via the internet increases receipt of results, saves staff time and improves patient satisfaction56,57s. Of note, we routinely give patients HIV positive test results by telephone and, more recently, have begun giving these results via a portal that allows patients to access their electronic medical record. We have never encountered problems with this practice; all HIV positive patients are offered face-to-face post-test counseling, including counseling with an HIV medical provider.
Cluster investigations and social network interventions
Many field services programs have DIS seek to identify the nonsexual contacts of persons with STIs through “cluster investigations” designed to test persons in the same social network as persons with identified STIs or the partners of persons with STIs. Past evaluations have found that HIV and STI test positivity among nonsexual contacts is substantially lower than that observed in sex partners58s, though such efforts have sometimes been effective, particularly in areas with a very high STI incidence59s. DIS have also been successful in coordinating a peer referral program in which methamphetamine using and Black MSM were asked to refer members of their social network for HIV/STI testing60s. While social network-based strategies have sometimes been effective, the contemporary effectiveness of cluster investigations is uncertain and the practice merits reevaluation to identify when it is useful, and when it should be abandoned to allow DIS to undertake higher priority work.
Developing an infrastructure to modernize field services
Integrating new outcomes into field services will require substantial changes in how DIS do their work, including changes in DIS protocols, data collection records and databases; new training; and better integration of field services with public health surveillance and the wider health care system.
Prioritizing change
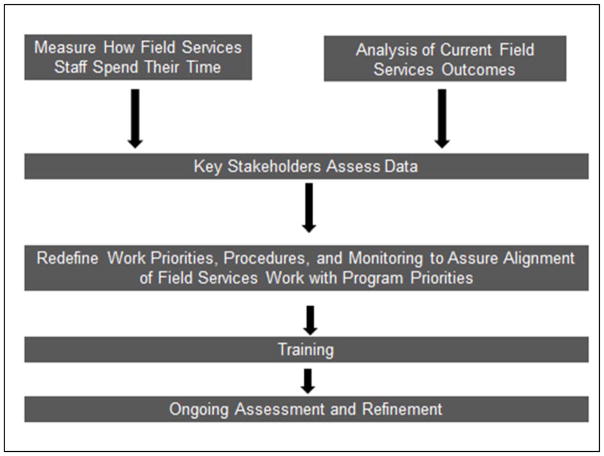
We recognize that virtually no field services program can simultaneously integrate all of the new outcomes we identify in table 1. Thus, as a first step, programs should identify which new outcomes are priorities. Because taking on new work requires some combination of new resources, greater efficiency, and discontinuation of lower priority work, programs should initially seek to define the quantity and outcomes of their current work (i.e. the number and percent of persons with each STI receiving partner services and the dispositions for these cases) and how DIS spend their time (figure 1). Common components of DIS work that most programs will want to measure include initial investigation of laboratory reports, confirming index patient treatment, telephone and online investigation, field investigation, documentation, performing HIV tests, and giving test results. These different activities should be evaluated for each STD. In some areas, portions of this work are carried out by non-DIS staff. Since this work represents an investment of disease investigation resources, it should be included in the assessment of how staff spends their time. (An instrument to evaluate how DIS spend their time is available through the University of Washington Public Health Capacity Building Center.) Programs should use these data to assess the extent to which current activities are aligned with program priorities. This assessment, along with federal priorities, should guide program changes. Defining field services priorities should include a process of shared decision-making between state and local health departments, and include program leadership and the field services team.
Figure 1.
Process for evaluating and modifying field services to align work with program priorities
Table 3 presents an example of how work might be prioritized based on the STI, population served, and the goals field services seek to advance. Different jurisdictions will order these priorities differently based on local objectives, funding streams, epidemiologic context and experience. However, all programs should seek to develop an explicit list of priorities and objectives.
Table 3.
Example of field services priorities, approaches to investigation+ and goals
| Population in order of priority | Approach | Goals* |
|---|---|---|
| Tier 1 | ||
| Syphilis in pregnant women | High intensity PS** | Index patient (IP) and partner treatment, Prevention congenital syphilis |
| Acute HIV infection | High intensity PS | Partner testing, Partner PrEP or PEP, Immediate initiation antiretroviral therapy (ART) (<48 hours) |
| Bacterial STI in HIV+ unsuppressed persons | High intensity PS | Relinkage to care/initiation antiretroviral therapy (ART), Partner testing and PrEP |
| Tier 2 | ||
| New HIV infection | Intermediate intensity PS** | Linkage to care (goal <7 days), Partner testing Partner PrEP |
| Investigation of HIV+ persons known to be in-jurisdiction and not virally suppressed | Intermediate intensity PS | Relinkage to HIV care, Partner HIV testing and PrEP |
| Complicated syphilis++ | Care coordination (as needed) – intermediate intensity PS | Treatment – prevent long-term sequelae, PrEP (HIV−), ART (HIV+), partner testing, treatment and possible PrEP |
| Tier 3 | ||
| Antimicrobial resistant gonorrhea (GC) | Intermediate intensity PS** | Treatment of IP and partners |
| Early syphilis in women and men who have sex with women only (MSW) | Intermediate intensity PS | Treatment of IP and partners, Identification of pregnant women with syphilis, Long acting contraception (LARC) promotion, HIV testing, PrEP referral (depends on local epidemiology) |
| GC or chlamydia (CT) in untreated pregnant women++ | Intermediate intensity PS | Treatment of IP and partners |
| Early syphilis in MSM and transgender persons who have sex with men | Lower intensity PS** (consider follow-up to ensure PrEP linkage) | HIV testing, Screening for complicated syphilis, Treatment of IP and partners, PrEP promotion |
| Surveillance-based investigation of HIV+ persons who are not virally suppressed | Intermediate intensity PS | Relinkage to HIV care, Partner HIV testing and PrEP |
| Tier 4 | ||
| Random sample heterosexual GC/CT*** | Lower intensity PS | Evaluation of EPT uptake, Partner treatment (EPT), LARC promotion |
| GC in MSM and transgender persons | Lower intensity PS (Intermediate intensity to promote PrEP in rectal GC) | HIV testing, Treatment of case and partners, PrEP promotion |
| GC in women and MSW only | Lower intensity PS | EPT, LARC promotion, PrEP promotion (depends on local epidemiology) |
| Tier 5 | ||
| CT in MSM and transgender persons | Lower intensity PS | HIV testing, Treatment of case and partners, PrEP promotion |
| CT in women and MSW only | Lower intensity PS | EPT, LARC promotion |
High intensity PS involve early initiation of field investigations. Intermediate intensity PS includes initial efforts to contact IPs by telephone or text message, with field investigation limited to cases that cannot be reached via telephone or text message. Lower intensity PS involves efforts to reach IPs and partners only via telephone and text message.
Referral for assistance obtaining insurance is a potential goal in all populations.
Neuro, ocular or otosyphilis
High intensity PS should be used in cases with elevated minimum inhibitory concentrations to ceftriaxone. Selected jurisdictions are using high-intensity PS for infections with Neisseria gonorrhoeae with decreased susceptibility to cefixime or azithromycin.
Prioritization of untreated persons with gonorrhea or chlamydial infection should not necessarily prompt programs to allocate resources to define the treatment status of all reported cases.
Undertaken to evaluate chlamydial control programs, particularly the use of expedited partner therapy11.
Program organization
In most programs, DIS are generalists, variously working cases of HIV and syphilis and performing other tasks as needed. As the portfolio of DIS work expands, this approach merits reconsideration. Not all DIS have the same skills or interests, and programs need to deploy their staff to advance priority goals and capitalize on each team member’s strengths. The practice of assigning all DIS to all tasks also poses a risk of sacrificing priority work in order to complete urgent work; DIS based in clinics frequently interrupt work to perform HIV tests or give test results and, as a result, neglect the program’s most important objectives. In King County, within our field services program, we have separate teams that focus on initial HIV case investigation (i.e. surveillance investigation, partner services and linkage to care), syphilis, gonorrhea and chlamydia in MSM and transgender persons, PrEP coordination, gonorrhea and chlamydial in cis-gender women and cis-gender men who have sex with women only, and relinkage to HIV care. We believe that this more specialized approach is better suited to mid-to-large programs that use DIS to advance diverse outcomes.
Training
DIS will need training to take on new work. CDC promotes DIS training through an online course, Passport for Partner Services, as well as through DIS Training Centers (DTCs). It is also developing a DIS certification program which will likely be integrated with new training efforts. These are valuable resources and positive developments which should facilitate field services modernization. However, the resources allocated to the DTCs are too meager to rapidly train all DIS in new procedures and, because successful programs will be heterogeneous as they adapt to local circumstances, national training cannot completely prepare field services staff for their jobs. Some state and local health departments already operate substantial training programs, and DIS have always learned much of their work on the job from one another. Thus, to prepare DIS for the future, we need a combination of improved federally funded national training and locally developed training that includes peer mentorship. Finally, modernization should not wait for national trainings. These might be a long time coming. Programs should identify priority areas for change and get started, learning as they go.
Data access, collection and management
Data collection instruments and associated data management systems play a central role in promoting program priorities, adherence to protocol and program monitoring. Ideally, these systems also help DIS succeed in their work, facilitating the organization and accessibility of information. As a result, promoting new objectives will require changes in data collection instruments and databases. For many programs, these changes present a substantial obstacle to change. Local health departments often rely on statewide field services databases that are maintained by information technology offices which are not directly accountable to HIV/STI programs and are minimally responsive to programmatic needs. Altering databases is often difficult and occurs slowly. These barriers are particularly problematic when developing new bodies of work, which inevitably involves serial refinements in data collection as staff develop and modify program procedures. Depending on local circumstances, departments should consider developing supplemental field services databases in simple, readily available programs (e.g. Microsoft Access, Research Electronic Data Capture [REDCap]) that are locally controlled and that can be rapidly changed. Once program procedures are well-developed, data elements can be incorporated into centrally managed databases.
Access to data, particularly data related to HIV, represents a particularly important problem. In many areas, DIS do not have access to HIV surveillance data, particularly viral load data. This needs to change. As discussed above, DIS can and should play an important role in promoting engagement with HIV care, but they cannot do that without access to HIV surveillance data. The integrity of surveillance data, and the privacy of persons with HIV needs to be protected, but legitimate concerns related to these issues should not be a barrier to DIS accessing surveillance data.
Monitoring and evaluation
Successful programs require ongoing monitoring and evaluation that integrates the work of epidemiologists with field services staff and supervisors. However, many field services programs have virtually no epidemiologic support. Success requires that some funding be allocated for program evaluation. Where data analytic capacity is very limited, health departments should explore contracting with academic or other partners for services. While such efforts require safeguards around data security, the need for such safeguards should not be a major impediment to forming new collaborative relationships.
Improving information dissemination
Many of the changes in field services we propose have been at least partially initiated in many health departments. There is an urgent need for field services programs to more rigorously evaluate their programs and publish their findings. CDC’s recent provision of supplemental funding to selected STD programs to more thoroughly evaluate their field services programs (CDC-RFA-PS15-1511), and efforts to promote the integration of HIV surveillance and prevention programs (CDC-RFA-PS18-1802) are important efforts to promote this change. Additional efforts of this type, which should ideally include greater partnerships with academic collaborators, are needed.
Conclusions
Changes in the epidemiology of STI, the social organization of sex, and the interventions available to prevent HIV/STI require a fundamental reorganization of field services in the U.S. That organization will require health departments to clearly establish their priorities and undertake new work while diminishing their investment in bodies of work and procedures that are relatively low yield. In many instances, success will also require changing the field services infrastructure, including the organization of field services teams, how those teams interact with surveillance and epidemiology units, how they collect and access data, and how they train staff. Progress is likely to be uneven, and different areas will prioritize different activities. To us, the most pressing need is to get started, to identify local priorities and establish plans for change, plans that take on the daunting challenges we all face and capitalize on scientific innovations to advance the public’s health.
Supplementary Material
Acknowledgments
Funding: Research reported in this publication was supported in part by NIAID, NCI, NIMH, NIDA, NICHD, NHLBI, NIA, NIGMS, NIDDK of the National Institutes of Health under award number AI027757, and by CDC H25PS004364 and CDC H25PS005108.
References
- 1.Henderson RH. Control of sexually transmitted diseases in the United States-A federal perspective. Br J Vener Dis. 1977;53(4):211–215. doi: 10.1136/sti.53.4.211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Peterman TA, O’Connor K, Bradley HM, Torrone EA, Bernstein KT. Gonorrhea Control, United States, 1972–2015, A Narrative Review. Sex Transm Dis. 2016;43(12):725–730. doi: 10.1097/OLQ.0000000000000515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention. Sexually Transmitted Disease Statistics 1984. Atlanta, GA: Dec, 1985. p. 134. [Google Scholar]
- 4.Gottlieb MS, Schroff R, Schanker HM, et al. Pneumocystis carinii pneumonia and mucosal candidiasis in previously healthy homosexual men: evidence of a new acquired cellular immunodeficiency. N Engl J Med. 1981;305(24):1425–1431. doi: 10.1056/NEJM198112103052401. [DOI] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention. HIV Surveillance - Epidemiology of HIV Infection. 2013. [Google Scholar]
- 6.Leads from the MMWR. Partner notification for preventing human immunodeficiency virus (HIV) infection--Colorado, Idaho, South Carolina, Virginia. Jama. 1988;260(5):613–615. [PubMed] [Google Scholar]
- 7.Bayer R, Fairchild AL. Changing the paradigm for HIV testing--the end of exceptionalism. N Engl J Med. 2006;355(7):647–649. doi: 10.1056/NEJMp068153. [DOI] [PubMed] [Google Scholar]
- 8.Potterat JJ. Partner notification for HIV: running out of excuses. Sex Transm Dis. 2003;30(1):89–90. doi: 10.1097/00007435-200301000-00017. [DOI] [PubMed] [Google Scholar]
- 9.Golden MR, Hogben M, Handsfield HH, St Lawrence JS, Potterat JJ, Holmes KK. Partner notification for HIV and STD in the United States: low coverage for gonorrhea, chlamydial infection, and HIV. Sex Transm Dis. 2003;30(6):490–496. doi: 10.1097/00007435-200306000-00004. [DOI] [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention. Recommendations for partner services programs for HIV infection, syphilis, gonorrhea and chlamydial infection. MMWR. 2008:57. [PubMed] [Google Scholar]
- 11.Golden MR, Kerani RP, Stenger M, et al. Uptake and Population-Level Impact of Expedited Partner Therapy (EPT) on Chlamydia trachomatis and Neisseria gonorrhoeae: The Washington State Community-Level Randomized Trial of EPT. PLoS Med. 2015;12(1):e1001777. doi: 10.1371/journal.pmed.1001777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McFarlane M, Bull SS, Rietmeijer CA. The Internet as a newly emerging risk environment for sexually transmitted diseases. Jama. 2000;284(4):443–446. doi: 10.1001/jama.284.4.443. [DOI] [PubMed] [Google Scholar]
- 13.Beymer MR, Weiss RE, Bolan RK, et al. Sex on demand: geosocial networking phone apps and risk of sexually transmitted infections among a cross-sectional sample of men who have sex with men in Los Angeles County. Sex Transm Infect. 2014;90(7):567–572. doi: 10.1136/sextrans-2013-051494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hull P, Mao L, Prestage G, Zablotska I, de Wit J, Holt M. The use of mobile phone apps by Australian gay and bisexual men to meet sex partners: an analysis of sex-seeking repertoires and risks for HIV and STIs using behavioural surveillance data. Sex Transm Infect. 2016 doi: 10.1136/sextrans-2015-052325. [DOI] [PubMed] [Google Scholar]
- 15.Klausner JD, Wolf W, Fischer-Ponce L, Zolt I, Katz MH. Tracing a syphilis outbreak through cyberspace. Jama. 2000;284(4):447–449. doi: 10.1001/jama.284.4.447. [DOI] [PubMed] [Google Scholar]
- 16.Udeagu CC, Bocour A, Shah S, Ramos Y, Gutierrez R, Shepard CW. Bringing HIV partner services into the age of social media and mobile connectivity. Sex Transm Dis. 2014;41(10):631–636. doi: 10.1097/OLQ.0000000000000181. [DOI] [PubMed] [Google Scholar]
- 17.Hightow-Weidman L, Beagle S, Pike E, et al. “No one’s at home and they won’t pick up the phone”: using the Internet and text messaging to enhance partner services in North Carolina. Sex Transm Dis. 2014;41(2):143–148. doi: 10.1097/OLQ.0000000000000087. [DOI] [PubMed] [Google Scholar]
- 18.Kachur R, Adelson S, Firenze K, Herrera M. Reaching patients and their partners through mobile: text messaging for case management and partner notification. Sex Transm Dis. 2011;38(2):149–150. doi: 10.1097/OLQ.0b013e3182036bab. [DOI] [PubMed] [Google Scholar]
- 19.Centers for Disease Control and Prevention. Sexually Transmitted Disease Surveillance 2015. Atlanta: CDC; Nov, 2016. 2014. [Google Scholar]
- 20.HIV/AIDS Epidemiology Unit PHSKC, and the Infectious Disease Assessment Unit Washington State Department of Health. HIV/AIDS Epidemiology Report 2015. http://www.kingcounty.gov/depts/health/communicable-diseases/hiv-std/patients/epidemiology/annual-reports.aspx.
- 21.Purcell DW, Johnson CH, Lansky A, et al. Estimating the population size of men who have sex with men in the United States to obtain HIV and syphilis rates. The open AIDS journal. 2012;6:98–107. doi: 10.2174/1874613601206010098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Seth P, Walker T, Hollis N, et al. HIV testing and service delivery among Blacks or African Americans--61 health department jurisdictions, United States, 2013. MMWR Morb Mortal Wkly Rep. 2015;64(4):87–90. [PMC free article] [PubMed] [Google Scholar]
- 23.Menza TW, De Lore JS, Fleming M, Golden MR. Partner notification for gonococcal and chlamydial infections in men who have sex with men: success is underestimated by traditional disposition codes. Sex Transm Dis. 2008;35(1):84–90. doi: 10.1097/OLQ.0b013e31814fb125. [DOI] [PubMed] [Google Scholar]
- 24.Steiner MJ, Warner L, Stone KM, Cates W. Condoms and other barrier methods for prevention of STD/HIV infection and pregnancy. In: Holmes KK, Sparling PF, Stamm WE, et al., editors. Sexually Transmitted Diseases. 4. New York: McGraw Hill; 2008. [Google Scholar]
- 25.Marks G, Crepaz N, Senterfitt JW, Janssen RS. Meta-analysis of high-risk sexual behavior in persons aware and unaware they are infected with HIV in the United States: implications for HIV prevention programs. J Acquir Immune Defic Syndr. 2005;39(4):446–453. doi: 10.1097/01.qai.0000151079.33935.79. [DOI] [PubMed] [Google Scholar]
- 26.Khosropour CM, Dombrowski JC, Kerani RP, Katz DA, Barbee LA, Golden MR. Changes in Condomless Sex and Serosorting Among Men Who Have Sex With Men After HIV Diagnosis. J Acquir Immune Defic Syndr. 2016;73(4):475–481. doi: 10.1097/QAI.0000000000001128. [DOI] [PubMed] [Google Scholar]
- 27.Cohen MS, Chen YQ, McCauley M, et al. Prevention of HIV-1 infection with early antiretroviral therapy. N Engl J Med. 2011;365(6):493–505. doi: 10.1056/NEJMoa1105243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dai JY, Gilbert PB, Hughes JP, Brown ER. Estimating the efficacy of preexposure prophylaxis for HIV prevention among participants with a threshold level of drug concentration. Am J Epidemiol. 2013;177(3):256–263. doi: 10.1093/aje/kws324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.White House Office on AIDS. National HIV/AIDS Strategy for the United States: Updated to 2020. Jul, 2015. [Google Scholar]
- 30.Wasserheit JN. Epidemiological synergy. Interrelationships between human immunodeficiency virus infection and other sexually transmitted diseases. Sex Transm Dis. 1992;19(2):61–77. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.