Abstract
The use of ethionamide (ETH) in treating multi-drug resistant tuberculosis is limited by severe side effects. ETH disposition after pulmonary administration in spray dried particles might minimize systemic exposure and side effects.
Methods
Spray dried ETH particles were optimized for performance in a dry powder aerosol generator (DPAG) and exposure chamber. ETH particles were administered by the IV, oral, or pulmonary routes to guinea pigs. ETH appearance in plasma, bronchoalveolar lavage and lung tissues were measured and subjected to non-compartmental pharmacokinetic analysis.
Results
DPAG dispersion of 20% ETH particles gave the highest dose at the exposure chamber ports and fine particle fraction of 72.3%. Pulmonary ETH was absorbed more rapidly and to a greater extent than orally administered drug. At Tmax, ETH concentrations were significantly higher in plasma than lungs from IV dosing, whereas, following insufflation lung concentrations were 5-fold higher than in plasma. AUC(0-t), and CL were similar after IV administration and insufflation. AUC(0-t) after oral administration was 6–7-fold smaller and CL was 6-fold faster. Notably, ETH bioavailability after pulmonary administration was significantly higher (85%) than after oral administration (17%).
Conclusion
Pulmonary ETH delivery would potentially enhance efficacy for TB treatment given the high lung concentrations and bioavailability
Keywords: Tuberculosis, ethionamide, porous particles, bioavailability, pharmacokinetics and pulmonary absorption
1. INTRODUCTION
Tuberculosis (TB) continues to be the cause of the most deaths worldwide due to a single organism, with some sources pairing it to the Human Immunodeficiency Virus (HIV)1 and others indicating that TB has surpassed HIV as a major killer2. The World Health Organization (WHO) estimated that in 2014 more than 9 million people developed TB, and 5% of those patients were infected with multidrug resistant (MDR; resistance against isoniazid and rifampicin) bacterial strains3. Treatment of drug susceptible TB is difficult, requiring 6–9 months of large doses of antibiotics in combination, however treatment of MDR-TB can extend up to 2 years and employs more complex, expensive and poorly tolerated therapeutic regimens4. In 2001, data meta-analysis of 9153 MDR-TB individual patients treated with complex and long regimens in multiple centers reported treatment success in only 54% of these patients5 A successful regimen only appeared in 2010, when a short, standardized treatment regimen based on a fourth generation fluoroquinolone combined with other second-line agents, known as the “Bangladesh Regimen”, achieved a relapse-free cure of 87.9%6. Based on data from this and other similar studies, in May 2016, the WHO announced new recommendations for a 9 to11 month shortened treatment regimen for selected MDR-TB patients7. This regimen has two phases: in the first, intensive phase patients receive a combination of kanamycin, moxifloxacin, prothionamide, clofazimine and pyrazinamide with high-dose isoniazid for 4 to 6 months. In the second, continuation phase patients receive moxifloxacin, clofazimine, pyrazinamide and ethambutol for 5 months. However, this shorter regimen is still associated with significant side effects, with 71% of the patients in the Bangladesh Regimen reporting nausea and vomiting, 12% reporting negative neurological side effects and 6% other miscellaneous side effects, with several patients experiencing more than one of these undesired side effects6.
An alternative approach to decrease the incidence and extent of the side effects to this short regimen is to deliver some of these drugs directly to the lungs to achieve high local drug concentration for extended durations. Such an approach has the possibility of accelerating the onset of drug action, decreasing the dose to achieve the therapeutic effect, which in turn would reduce systemic side effects. Also, it may be possible to exchange some of these drugs with more potent or longer half-lived analogs, which would decrease the dosing frequency. For instance, in the Bangladesh Regimen, prothionamide (PRO) could be replaced by ethionamide (ETH).
ETH was first used in the mid 1950’s for TB treatment and in 1963 it was evaluated with the objective to prevent resistance to isoniazid or to treat isoniazid-resistant MTB (xx). In the United States, ETH is one of the 10 drugs approved by the Food and Drug Administration (FDA) to treat TB8. ETH is on the WHO’s List of Essential Medicines and it is classified as an “oral bacteriostatic second line agent”, Group 4 of drugs to treat MDR-TB9. The 2011 Update of the Guidelines for the Programmatic management of MDR-TB strongly recommends the use of ETH or PRO, as the association of their use with cure was higher than that for cycloserine and PAS10. It is frequently added to drug regimens around the world because it is the only drug in Group 4 that has bactericidal activity against MTB11. However, bactericidal ETH serum concentrations are hard to achieve because of poor tolerability by patients12. Therefore, the use of ETH decreased when PRO, a better tolerated analogue, became available11. Several studies comparing the efficacy and tolerability of ETH and PRO have determined that both compounds are equally effective in treating TB, but that PRO was much better tolerated by the patients than ETH13, 14. PRO is an analogue of ETH, in which the ethyl group is substituted by a propyl molecule at the alpha position. ETH is 2-fold more potent (MIC =0.25 μg/ml) than PRO (MIC = 0.5 μg/ml) against Mycobacterium tuberculosis strain H37Rv and has a longer half-life15, 16. In humans, administration of the same dose (250 mg) of these compounds results in a maximum plasma concentration that is about 1.8 times higher for ETH than for PRO16. The objective of the present study was to evaluate the disposition of ETH after pulmonary administration of spray dried microparticle porous particles (PPs) to guinea pigs and contrast it with that after IV and oral administration. Powder formulations consisting of PPs deliver drug to the lung periphery more efficiently than other powder formulations, avoiding natural clearance mechanisms in the respiratory tract17. We postulate that delivery of ETH by the pulmonary route will increase its efficacy and decrease its toxicity, which can bring it back to the forefront of TB treatments.
2. MATERIALS AND METHODS
ETH and L-leucine were obtained from Spectrum Chemicals & Laboratory Products (Gardena, CA). 1,2 dipalmitoyl-sn-glycero-3-phosphatidylcholine (DPPC) was purchased from Genzyme Pharmaceuticals (Liestal, Switzerland). Carboxy-methyl-cellulose (CMC; MW = 90,000 kDa) was purchased from Sigma-Aldrich (St. Louis, MO). ETH was a yellow powder soluble in ethanol and very sparingly soluble in water. Ethanol USP grade and acetonitrile were purchased from Pharmco Products Inc. (Brookfield, CT). Water from a Millipore Corp. (Billerica, MA) Milli-Q water purification system was used. All other chemicals and reagents used were of pharmaceutical or analytical grade.
2.1. Formulation of Ethionamide Porous Particles
ETH PPs were manufactured as described previously18, 19 by spray-drying (LabPlant, Model SD-06) a water/ethanol solution containing different proportions of ETH, L-leucine and DPPC. In order to increase the residence time of a standing aerosol cloud of ETH PPs in a dispersion chamber, three different formulations of PPs were prepared with three different compositions of ETH (50%, 20% and 5%), leucine and DPPC as follows (50:40:10 w/w; 20:70:10 w/w; and 5:90:5 w/w).
2.2. Characterization of Ethionamide Porous Particles
The dry particles were viewed using scanning electron microscopy (SEM). A LEO 982 field emission scanning electron microscope (Carl Zeiss, Inc., Thornwood, NY) was operated at 2 kV with a filament current of about 0.5 mA. Powder samples were prepared by deposition on a double coated carbon conductive tape tab (Ted Pella Inc., Redding, CA) mounted on a pin mount and dusted. The sample was then coated with a Platinum/Palladium layer with a Cressington Scientific Instruments Inc. (Watford, UK) 208HR sputter coater, operated for 60 s at a sputtering current of 40 mA.
An eight-stage Andersen non-viable 1ACFM cascade impactor (ACI) (Copley Scientific Limited, Nottingham, UK) was used to determine the mass median aerodynamic diameter (MMAD) and the fine particle fraction (FPF) of the total dose of powder less than or equal to an effective cut-off aerodynamic diameter of 5.8 μm (FPF5.8) and 3.3 μm (FPF3.3) relevant to humans and laboratory animals, respectively.
2.3. Performance of Ethionamide Porous Particles in a dry powder aerosol generator (DPAG)
A custom-made nose-only exposure chamber and dry powder aerosol generator (DPAG, Patent US 8,205,612 B2) was developed with the purpose of generating and delivering dry powder aerosol from PP formulations to guinea pigs. The percentage of the nominal dose of ETH PPs delivered at each port of the DPAG was evaluated, by a method described previously20, as follows: Approximately 50 mg of ETH PPs (nominal dose) were loaded in the main chamber of the DPAG and cotton balls of similar sizes were snuggly placed to cover each port and the DPAG was actuated for 5 minutes to aerosolize the ETH PPs. The cotton balls were the carefully taken out of the ports and each cotton ball was placed in a beaker, where ETH was extracted into 10 ml of methanol and the concentration determined by UV spectrophotometry from a standard curve constructed using known amounts of ETH PPs. The % of nominal dose of PPs delivered at each port was determined dividing the amount of ETH PPs deposited at each port (calculated by correcting with the ETH content in each formulation) by the nominal dose loaded in the chamber of the DPAG.
The aerodynamic performance of ETH PPs in the DPAG was evaluated as a means of estimating the respirable dose that would be delivered to each animal in the chamber. A Marple Personal Cascade Impactor (Series 290, Westech Instruments, Inc., Marietta, GA) was employed to determine the mass median aerodynamic diameter (MMAD) and fine particle fraction (FPF) delivered to each port of the chamber following dispersion of ETH PPs. Most importantly, it was calculated the FPF of the % of nominal dose of PPs delivered at each port of the DPAG less than or equal to an effective cut-off aerodynamic diameter of 3.5 μm (FPF3.5) and 0.52 μm (FPF0.52) as they are relevant to the nose and alveoli of guinea pigs, respectively21, 22. The impactor was coupled to a vacuum pump calibrated at 2 L/min to mimic the breathing of a guinea pig. To calculate the dose delivered, approximately 60 mg of ETH PPs were deposited on top of the chamber propeller and the chamber was actuated for 5 minutes at a fixed speed and the powder dispersion aided with air from an external source (DPAG, Patent US 8,205,612 B2). After powder dispersion, the amount of ETH deposited in the stages of the impactor were determined by rinsing them thoroughly with methanol and the ETH concentration calculated by UV spectrophotometric analysis of the samples at 290 nm.
2.4. Pharmacokinetic studies
2.4.1. Animals
Specific-pathogen free, male Dunkin-Hartley guinea pigs (Hilltop Lab Animals, Inc., Scottdale, PA, USA) weighing (383.6 ± 28.4 g) were housed individually in a constant temperature environment of 22°C on a 12 h light/dark cycle. Animals were allowed access to water and food ad libitum. The day before the study, each animal underwent cannulation of the right external jugular vein for continuous blood sampling and allowed to recover overnight. All animal procedures were approved by the Institutional Animal Care and Use Committee (IACUC) of the University of North Carolina at Chapel Hill in accordance with “Principles of Laboratory Animal Care” (NIH publication #85–23, revised in 1985).
2.4.2. Treatments
Animals were divided into 4 groups receiving different ETH formulations (table 1): solution, suspension or dry powder, delivered by different routes (IV, oral, pulmonary). For IV administration, ETH drug substance was dissolved in pure ethanol and vortexed for ~1 min until completely dissolved. For oral administration, pure ETH was suspended in 1.25% CMC and distilled water by mortar and pestle followed by vortexing. ETH was administered intravenously to animals as a solution by the cannula implanted at the jugular and orally as a suspension to animals using an oral gavage needle. For the insufflation procedure, each animal was anesthetized by intraperitoneal injection of ketamine (50 mg/kg) and xylazine (5 mg/kg). The animal was then intubated with the help of a laryngoscope and ETH-PPs were administered with a small dry powder insufflator (Penn Century, Wyndmoor, PA) directly into the animal’s airways. The insufflator was removed and each animal was held in an upright position for 1–3 min. The animal was then placed at ~30° incline with a h eating pad underneath to prevent hypothermia. The animal’s breathing was monitored continuously until recovery from anesthesia. Dosing of animals with ETH-PPs by passive inhalation was conducted by placing conscious animals in the ports of a custom-made nose-only dry powder aerosol generator (DPAG) and dispersing 360 mg of powder inside the chamber for 1 h so that animal would inhale powder only through the nose. After dosing, blood samples (0.3 ml) were collected from each animal into heparinized tubes at 0, 0.08, 0.25, 0.5, 0.75, 1, 1.5, 2, 3, and 4 h. Sterile heparinized saline solution was used to replace the blood volume lost through sample collection. Plasma was separated and stored at −80°C until analysis.
Table 1.
Summary of treatments employed to evaluate the disposition of Ethionamide in guinea pigs.
| Treatment | Formulation | Dose (mg/kg) | Route of administration | # Animals (Tmin) | # Animals (Tmax) |
|---|---|---|---|---|---|
| IV | Solution | 6 | IV | 8 | 4 |
| Oral | Suspension | 6 | Oral | 8 | 5 |
| Insufflation | Dry powder (PPs) | 6 | Pulmonary (Insufflation) | 8 | 6 |
| Passive Inhalation | Dry powder (PPs) | * | Pulmonary (Passive inhalation) | 4 | – |
5 mg/kg, estimated from PK parameters (area under the curve, dose and bioavailability) calculated for IV and insufflation groups, the drug load in the ETH-PPs (20%), the fine particle fraction in that particular batch (FPF<0.52 μm = 27.37% at 2 L/min using a Marple personal cascade impactor), the average weight of the animals (0.38 kg) in that treatment group. The number of animals in each treatment group was selected based on similar studies previously performed by our group.
2.4.3. Evaluation of local Ethionamide concentrations
After collection of the last blood sample, animals were anesthetized and euthanized by exsanguination. The amount of ETH remaining in the airways was determined by measuring ETH concentrations in bronchoalveolar lavage (BAL) fluid. The lungs of each animal were lavaged by instilling 5 ml of sterile saline and slowly withdrawing the fluid. An aliquot of the BAL fluid was placed in a microcentrifuge tube and immediately centrifuged for 10 min at 12,000 rpm. The BAL supernatant was separated from the pellet (i.e., cellular constituents) and both were stored at -80°C until later analysis. After BAL was performed, the trachea and lungs were resected and stored with the BAL components until analysis.
After completing animals in the 4 treatment groups and the time to reach maximal ETH plasma concentrations (Tmax) was calculated, another group of animals from each treatment received the respective ETH formulations, with the purpose to determine local ETH concentrations. However, these animals were euthanized at Tmax as described above, BAL performed and lung and trachea collected and stored until analysis.
2.4.4 Determination of Ethionamide concentration in biological samples
ETH concentrations in plasma, BAL, and tissue samples were determined using a validated HPLC method23. ETH concentrations in the standard curve ranged from 0.2 to 10 mg/ml and the absolute recovery of ETH was approximately 91%. The within-day precision (coefficient of variation [CV]) of quality control samples was 0.36 to 6.39%, and the overall validation precision was 0.81 to 4.66%.
2.4.5 Pharmacokinetic analysis
ETH plasma concentration-time profiles from 0–4 hours following oral, IV and pulmonary ETH administration for all animals were subjected to non-compartmental pharmacokinetic analysis using WinNonlin (Pharsight Corporation, Mountain View, CA). The following pharmacokinetic parameters were determined: area under the curve (AUC(0-t)), apparent total body clearance (CL), mean residence time (MRT), elimination rate constant (K), and half-life (t1/2). Maximum ETH concentrations (Cmax) and time to achieve the maximum ETH concentration (Tmax) were obtained from the non-fitted plasma versus time profiles for each individual animal. The following equation was used to calculate bioavailability:
Where AUC lung, oral,IV is the area under the curve after pulmonary, oral or IV administration and D is the dose delivered (6 mg/kg) by each of these routes.
2.5 Statistical analysis
ETH plasma concentration versus time profiles, ETH concentrations in BAL and tissue data as well as PK parameter of disposition were statistically analyzed using a one-way analysis of variance (ANOVA) and least-squares significant differences multiple comparison method (i.e., Tukey’s). A probability level of 5% (p<0.05) was considered to be statistically significant.
3. RESULTS
3.1. Physicochemical characteristics of Ethionamide Porous Particles
Regardless of the %ETH in the formulation, all spray-dried ETH PPs were very porous spherical particle structures constructed of thin walled layers as shown by the scanning electron micrograph (figure 1). However, the MMAD, GSD and FPF as determined by impaction were different: MMAD and GSD of 50%ETH PPs was larger (4.94 μm and 1.53, respectively) than those of 20%ETH PPs (4.01 μm and 1.07, respectively), whereas the FPF5.8 and FPF3.3 were lower for the 50% ETH PPs (55.58% and 9.49%, respectively) than for the 20%ETH PPs (77.95% and 26.31%, respectively).
Figure 1.
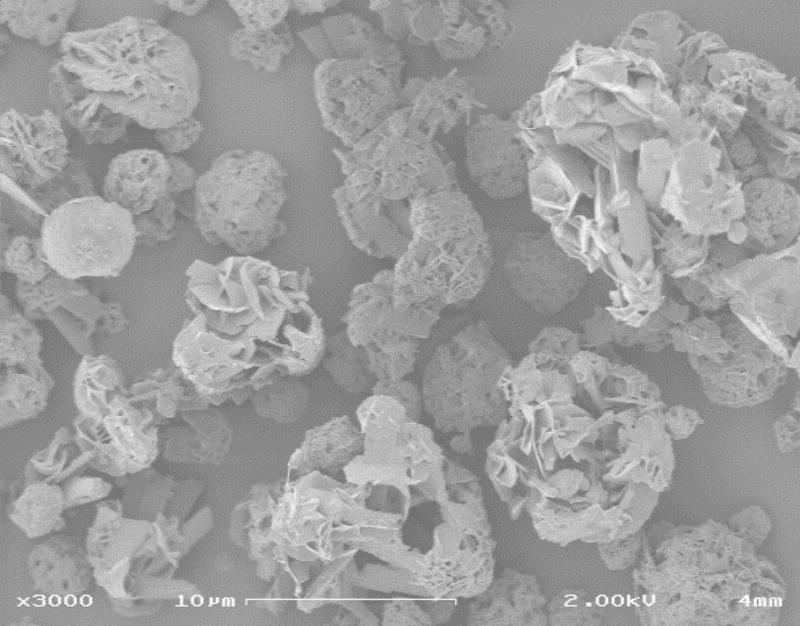
SEM micrograph of spray dried ETH PPs. Bar = 10 μm. This micrograph corresponds to PPs containing 50% ETH, but the morphology of PPs containing 20% ETH is similar and therefore not shown.
3.2. Performance of Ethionamide Porous Particles in a dry powder aerosol generator
Dispersion of PPs containing 20% ETH resulted in a 2-fold higher percentage of the nominal dose (18.35±2.66%) delivered to the ports of the DPAG and was significantly higher (p<0.05) than those resulting from the dispersion of PPs containing either 50% or 5% ETH (8.86±1.17% and 9.42±0.83%, respectively). Due to the low percentage of the dose delivered to the ports of the DPAG and the small drug content, the 5% ETH PPs formulation was not considered further, as it was unlikely that their pulmonary administration to animals would yield therapeutic drug levels.
The emitted dose collected in the different stages of the Marple Personal Cascade Impactor attached to the port of the DPAG was 2-fold higher after dispersion of PPs containing 20% ETH (11.68%) compared to those containing 50% ETH (6.32%). The MMAD and GSD of 20% ETH PPs were smaller (2.89 μm and 2.41, respectively) than that corresponding to 50% ETH PPs (4.85 μm and 2.66, respectively). Most importantly, FPF3.5 and FPF0.52 where higher in the 20% ETH PPs (72.3% and 43.9%, respectively), than those of 50% ETH PPs (64.3% and 19.7%, respectively). This difference in the FPF3.5 and FPF0.52 has important implications for administration of ETH PPs by passive inhalation studies in the guinea pig model as only particles in the 0.7–3.0 μm range could have a therapeutic effect21, 22. Therefore, the 20% ETH LPP formulation was selected for subsequent animal studies.
3.3. Pharmacokinetic studies
Figure 2 shows mean ETH plasma concentration vs. time curves after dosing IV, oral, and pulmonary treatments (insufflation and nose-only exposure) to guinea pigs. As expected after IV administration, ETH plasma concentrations at 0.083, 0.25, and 0.5 h were significantly higher (p<0.05) than those receiving the same dose by oral administration. Remarkably, ETH plasma concentrations in animals dosed with ETH-PPs by insufflation at these times were similar (p>0.05) to the IV dosed animals and significantly higher (p>0.05) than orally dosed animals, indicating immediate absorption of ETH from the lungs. At 1 hour post-dosing, ETH plasma concentrations were similar for all treatment groups until the end of the study. ETH plasma concentrations in animals dosed by passive inhalation in the DPAG were similar to those of animals dosed orally throughout the study. The ETH dose received by animals dosed by passive inhalation was approximately 5 mg/kg. This dose was calculated using the drug load in the ETH-PPs (20%), the fine particle fraction in that particular batch (FPF<0.52 μm = 27.37% at 2 L/min using a Marple personal cascade impactor), the average weight of the animals (0.38 kg) in that treatment group, the AUC obtained after passive inhalation of ETH PPs and the pulmonary bioavailability obtained after insufflation.
Figure 2.

AVERAGE plasma concentration versus time curves (log scale) for all treatments administered by various routes and with different doses. Treatments include: intravenous ethionamide USP (IV; 6 mg/kg), oral ethionamide USP (Oral; 6 mg/kg), ethionamide large porous particles (ETH-PPs; 6 mg/kg), and ethionamide large porous particles delivered by nose-only exposure (ETH-PPs; 5 mg/kg). * = IV different from oral (P<0.05); # = insufflation different from oral (P<0.05). (Average ± standard deviation, n = 4–8).
Local ETH concentrations in lungs, trachea, BAL pellet and supernatant at the time of maximum concentration (Tmax) and at the end of the study (Tmin) are presented in table 2. For ETH levels at Tmax, two types of comparisons were performed (table 2): (1) between fluids (plasma and BAL supernatant/pellet) and tissues within the same route of administration (denoted by a numerical superscript); and (2) between different routes of administration within the same fluid/tissue (denoted by a letter superscript). As expected in animals receiving ETH by the IV route, the highest concentrations were observed in plasma, with higher ETH concentrations in lungs and trachea (well perfused organs), than in BAL components. In contrast, animals dosed by insufflation exhibited the highest ETH concentrations in lungs and trachea which were 5- and 7-fold as those in plasma, followed by those in BAL supernatant, which were also 3-fold higher than those in plasma. Despite of the large variability observed in ETH concentrations among trachea and lung tissues of animals receiving ETH by the oral route, these concentrations were significantly higher than those observed in BAL components and in plasma. Comparison of ETH concentrations in lung tissue and BAL pellet samples indicated that animals dosed by insufflation exhibited significantly higher concentrations than animals dosed orally. Likewise, significantly higher (>10-fold) ETH concentrations were observed in the trachea and BAL supernatant of animals dosed by the pulmonary route than by any other treatment. ETH levels in plasma and BAL were mostly undetectable in animals of all treatment groups at the end of the study period (Tmin, table 2).
Table 2.
Ethionamide concentration in individual components of BAL, lung and trachea tissues at various times after dose administration (Average ± standard deviation, n = 4–8).
| Time/Treatment | Cmax Plasma (μg/ml) |
Trachea (μg/g) |
BAL supernatant (μg/ml) |
BAL pellet (μg/ml) |
Lungs (μg/g) |
|---|---|---|---|---|---|
| Tmax | |||||
| IV (0.083 h) |
5.85 ± 1.611; a | 2.69 ± 0.592; b | 0.75 ± 0.373; b | 0.04 ± 0.033; a,b | 4.08 ± 0.622; a,b |
| Oral (0.39 h) |
0.21 ± 0.071; b | 0.95 ± 0.621; b | 0.03 ± 0.052; b | 0.00 ± 0.002; b | 0.85 ± 1.041; b |
| ETH-PPs (insufflation) (0.083 h) |
3.37 ± 0.871, 2; b | 23.29 ± 9.881; a | 9.15 ± 6.152, 3; a | 0.47 ± 0.473; a | 18.50 ± 15.721, 2; a |
| At Tmin | |||||
| IV | 0.00 ± 0.01 | 0.00 ± 0.00 | 0.00 ± 0.00 | 0.00 ± 0.00 | 0.00 ± 0.00 |
| Oral | 0.01 ± 0.02 | 0.00 ± 0.00 | 0.00 ± 0.00 | 0.00 ± 0.00 | 0.05 ± 0.04 |
| ETH-PPs | 0.01 ± 0.01 | 0.03 ± 0.04 | 0.00 ± 0.00 | 0.01 ± 0.02 | 0.02 ± 0.04 |
Comparisons between fluids (plasma and BAL supernatant/pellet) and tissues within the same route of administration. Numeric superscripts show the relative ranks of values (starting from the highest values). When the means are not significantly different, the same numeric superscript is used.
Comparisons between different routes of administration within the same fluid/tissue. When the means are not significantly different, the same letter superscript is used.
The PK parameters that characterize the disposition of ETH after administration by the different routes are reported in table 3. As expected from the similarity in the plasma concentration versus time profiles, AUC(0-t), CL, MRT, and Tmax were also similar (p<0.05) between animals dosed IV and by insufflation, indicating similar disposition of ETH by both routes of administration. However Cmax was significantly higher in IV dosed animals than in those receiving ETH by insufflation. AUC after oral administration of ETH was 6–7-fold smaller than that after IV or pulmonary administration. Tmax indicated that, in the guinea pig, ETH was absorbed 5-times faster after pulmonary administration than after oral administration and was cleared (CL) significantly faster (6-fold) after oral administration than after IV or pulmonary administration. Most notably, ETH bioavailability after pulmonary administration was 85% with respect to IV administration, whereas the oral bioavailability was only 17%.
Table 3.
Pharmacokinetic parameters obtained by non-compartmental analysis after administration of the various treatments of Ethionamide by the different routes (Mean ± S.D.; n = 6–8).
| Treatments | |||
|---|---|---|---|
| Parameter | IV (6 mg/kg) |
Oral (6 mg/kg) |
ETH-PPs (6 mg/kg) |
| AUC (0-t) (μg h/ml) | 1.60 ± 0.391 | 0.21 ± 0.132 | 1.34 ± 0.121 |
| CL (ml/h/kg) | 3.93 ± 0.952 | 26.46 ± 12.811 | 4.40 ± 0.382 |
| K (h−1) | 1.45 ± 0.27 | 1.10 ± 0.55 | 1.77 ± 1.41 |
| t1/2 (h) | 0.49 ± 0.08 | 0.79 ± 0.40 | 0.75 ± 0.57 |
| MRT (h) | 0.41 ± 0.072 | 0.92 ± 0.251 | 0.43 ± 0.152 |
| Cmax (μg/ml) | 5.03 ± 0.901 | 0.19 ± 0.083 | 3.71 ± 0.602 |
| Tmax (h) | 0.08 ± 0.002 | 0.39 ± 0.211 | 0.08 ± 0.002 |
| F (0-∞) | 1.00 ± 0.001 | 0.17 ± 0.123 | 0.85 ± 0.072 |
AUC(0-t) = area under the curve, K = elimination rate constant; t1/2 = half-life; MRT = mean residence time; CL = clearance; Cmax = maximum concentration; Tmax = time to reach Cmax; F(0-∞) = bioavailability.
Numeric superscripts show the relative ranks of values (starting from the highest values).
When the means are not significantly different, the same superscript is used.
4. DISCUSSION
The global spread of strains of Mycobacterium tuberculosis (MTB) with resistance to the most effective anti-TB drugs (rifampicin and isoniazid), defined as MDR-TB, has been a challenging hurdle to the global TB control. Further, the increasing incidence of extensively (resistance to more than the two first line drugs, rifampicin and isoniazid) and totally drug resistant TB is a global health emergency. The therapeutic regimen for the management of patients with MDR-TB usually consists of 4 or more drugs and is based on the susceptibility of the isolated bacteria. In general, these regimens follow national treatment guidelines in line with WHO-recommended standards but their composition is influenced by the efficacy of the drugs, the treatment strategy, possible adverse effects and the cost of treatment24. Thus, even though ETH is more potent and has a longer half-life, the inclusion of PRO in these regimens is favored over ETH with the purpose of reducing the severe adverse effects of the treatment25. Since the main adverse effects associated with the use of ETH are gastrointestinal, it is postulated that administration of ETH by the pulmonary route would decrease its toxicity and increase its efficacy because higher local drug concentration could be achieved at the site of MTB infection.
Previous studies have demonstrated that PPs are more efficiently delivered to the lung periphery (the major site of MTB infection) than smaller solid particles with the same mass, because their site of their deposition in the lungs is determined by their aerodynamic, rather than their geometric diameter26. In this study, ETH PPs were manufactured with same procedure (spray drying) and materials (leucine and DPPC) that we have used successfully with other anti-TB drugs (rifampicin, capreomycin and PA-824)27–30. The previous studies demonstrated that the antimicrobial activity of these antibiotics was not affected by the process of spray drying. This determination was not performed for ETH PPs since similar conditions were used for their manufacture. However, since the drug was recovered intact following delivery and there was no evidence of degradation during in-vitro characterization (dose and aerodynamic particle size distribution measurement), there is no reason to believe that its chemical composition was affected by spray drying. Therefore, it is unlikely that its activity was affected by spray drying but this requires confirmation by determining the minimum inhibitory concentration for MTB.
In the present study, three different formulations of ETH PPs were prepared by varying the percentages of ETH (5–50%), leucine (40–90%) and DPPC (5–10%) to maximize the respirable fraction (FPF) that could be delivered to the alveoli of guinea pigs using the DPAG. Leucine is a non-polar amino acid that has weak surfactant properties and low aqueous solubility, whereas DPPC is a phospholipid that also has surfactant properties. The use of leucine in the formulation of inhalable particles has been reported to increase significantly the respirable fraction, as it enhances the flowability and dispersibility of the dry powder31. Inclusion of DPPC (up to 60%) in PPs formulation has shown to decrease particle density, but this decrease is accompanied by an increase in particle size32. However, at 10% or less DPPC content with respect to leucine, no increase in particle size was observed33. Thus, while formulating the ETH PPs, the maximum proportions of ETH and DPPC that were considered were 50% and 10%, respectively.
Evaluation of the performance of the three ETH PPs formulation in the DPAG determined that dispersion of the PPs containing 20% ETH achieved the highest percentage (18.35%) of the nominal dose delivered at the ports of the DAPG and the highest respirable fraction relevant to guinea pigs (FPF0.52). It is likely that the highest respirable fraction in that powder resulted in the highest percentage of the nominal dose delivered at the ports of the DAPG. The higher respirable fraction in the 20% ETH PPs is probably due to the higher percentage of leucine in this formulation (70%), compared to the percentage in the 50% ETH PPs formulation (40%)34, 35.
The formulation containing 20% ETH was selected for use in animal studies despite the higher drug content observed for the formulation containing 50% ETH. This may be explained by estimates of the fraction of the nominal dose delivered to the port (18.35%) and the respirable fraction corresponding to guinea pigs (FPF0.52 = 43.9%) predicting that animals would inhale more than 4-fold more ETH with the 20% formulation than with the 50% formulation. Therefore, the immediate absorption of ETH after pulmonary administration of ETH PPs (Tmax = 0.089 h, or 5 minutes) may be attributed to the large FPF of this optimized formulation being deposited directly in the alveoli of animals. Even though very rapid absorption of several compounds has been reported after their pulmonary administration, ETH concentrations in plasma after pulmonary administration were remarkably similar to those after IV administration. This may be explained by the larger surface area for absorption in the alveolar region together with the small molecular weight of ETH and partition coefficient (log P) of 0.705 allowing it to cross the thin barrier from the alveoli to the capillary blood supply very rapidly. In contrast, the absorption of ETH from the GI tract of the guinea pig appears to be slightly delayed (Tmax = 0.39 h), limited and variable. Despite limited reports of rapid and complete ETH absorption when administered to humans36, a larger number of studies describe the pattern of ETH absorption as “erratic” and that delayed absorption is typically common23, 25, 37. The Tmax in healthy volunteers is reported to be between 1.02 h and 2.6 h depending on the formulation (film or enteric coated tablet) and co-administration of food or antacids23, 38–40.
The disposition of ETH in the guinea pig after oral administration has been published in a small number of papers of the seminal work of Dickinson and Mitchison, where large doses (10–320 mg/kg) were administered41–44, but there are no reports of pulmonary delivery of ETH powders to guinea pigs or humans. The dose of ETH in the present study (6 mg/kg) was selected for direct comparison with the pharmacokinetic studies using oral administration performed in volunteers by Auclair et al.23 and Zhu et al.38, which indicated that this dose appeared to be the minimum required to achieve serum concentrations above the MIC = 0.25 μg/ml15. In the present study, while IV and pulmonary administration of this dose did achieve plasma concentrations significantly above MIC (Cmax of 5.85 μg/ml and 3.37 μg/ml, respectively), oral administration did not do so at any time during the study (Cmax = 0.21 μg/ml). These differences can be noted when comparing the Cmax of early studies in guinea pigs and those from humans. In guinea pigs, Cmax of less than 1.0 and 5 μg/ml were recorded for doses of 10 and 40 mg/kg, respectively41, 42; whereas for healthy volunteers, the Cmax recorded for a dose of approximately 6 mg/kg is between 2.16 and 2.3 μg/ml23, 25, 38, 39. This may result from a species difference in enzyme expression and/or activity and, consequently, metabolism. In man, ETH is extensively metabolized in the liver, where 6 metabolites have been isolated to date39. The first step in ETH metabolism is transformation to sulphoxide metabolites, which have antimicrobial activity, by Flavin-containing-monooxygenases (FMO)25. From the five functional FMOs, the isoforms 1, 2 and 3 are implicated in the metabolism of ETH: FMO1 is primarily expressed in liver, kidney and intestine; FMO2 is the major isoform in the lungs and FMO3 is the primary FMO in the liver45. There are no reports of the expression and localization of FMOs in the guinea pig but it is plausible that they would be located in the same organs as in man. If so they would have different activities as has been reported with other liver enzymes46. Therefore, the lower ETH concentrations in plasma after oral administration in the guinea pig may be due to its “erratic” absorption and extensive metabolism in intestine and liver.
In addition to the immediate absorption and higher plasma concentrations due to lack of ETH metabolism in the lungs, there are three additional advantages of delivering ETH by the pulmonary route: (1) The achievement of higher local concentrations at the site of MTB infection; (2) Smaller variability in the overall disposition; and (3) the similarity of its corresponding PK parameters (AUC(0-t), CL, MRT) to those after IV administration.
ETH concentrations in the trachea, BAL and lungs of animals dosed by insufflation were several fold higher at Tmax than those after oral administration and MIC. Thus, more drug would be available to kill MTB at the site of infection. Local ETH concentrations were not determined in animals dosed by passive inhalation, but the resulting plasma concentrations were similar to those after oral administration. These lower concentrations may be explained by the breathing parameters of guinea pigs, rather than limited absorption and extensive metabolism such as in the oral route. The dose that guinea pigs can inhale by passive administration was limited to the amount that the animal could breathe through its nose and the fraction of the dose that could can be inhaled by the nose, which is limited by the cutoff diameter of particles47.
There was considerable inter-animal variability in the calculation of PK parameters for the different treatments, but the coefficient of variation (CV%) was significantly smaller after pulmonary administration (CV% = 8–16%) than after oral administration (CV%= 42–62%). This fairly larger variability in PK parameters after oral administration of ETH has been also observed in humans (healthy and TB-infected)23, 38. Nevertheless, pulmonary delivery of ETH resulted in a 7-fold larger AUC(0-t) and the drug being cleared 6-fold less than after oral delivery. Notably, the similarity of AUC(0-t) resulted in a much higher bioavailability (85%) than that after oral administration (17%). Thus, with the higher local concentrations achieved in the lungs and the higher bioavailability after pulmonary administration compared to those obtained orally, it may be possible to reduce the dose of ETH required for the treatment of MDR-TB.
Efficacy studies with inhaled ETH, alone or in combination are required to confirm its effectiveness in treating MDR-TB. However, the results of the present study have the potential to inform existing treatment regimens. A possible application of the findings of the present study could be that the formulation and route of administration for ETH could be switched form a tablet/suspension administered orally to a dry powder formulation administered by inhalation in currently used regimens such as the “Bangladesh Regimen”. Pulmonary administration of ETH is likely to decrease significantly or even eliminate the high frequency of gastrointestinal side effects caused by the oral administration of ETH. Pulmonary administration can also avoid the first pass metabolism of ETH, which is suspected to contribute to the large intra-subject variability observed after oral administration to patients23, 38 that we also observed in guinea pigs. Lastly, pulmonary administration of ETH is likely to achieve bactericidal levels at the primary site of infection, with a potentially reduced dose. However, more detailed PK studies are required to evaluate the use of reduced doses by inhalation, or the dosing frequency to achieve the desired effect. Nevertheless, pulmonary delivery of ETH can be a prime candidate for use in individualized MDR-TB regimens9, whenever these are possible.
5. CONCLUSION
The results of this study suggest that administration of ETH by the pulmonary route may enhance its efficacy as indicated by the higher concentrations achieved in the lungs, trachea and BAL of guinea pigs and also by the significantly higher bioavailability. Thus, it is plausible that the higher bioavailability may allow administration of smaller doses to achieve the same effects observed by other routes of administration, which in turn could decrease the incidence of adverse effects. The advantages of this approach would allow reconsideration of the role of ETH in TB therapy.
Acknowledgments
This work was supported by a grant (5 U01 61336) from the National Institutes of Health/NIAID.
GLOSSARY OF TERMS
- 1ACFM
1 Actual cubic feet per minute
- ACI
Andersen Cascade Impactor
- AUC
Area under the Curve
- BAL
Broncho-Alveolar Lavage
- CL
Apparent Total Body Clearance
- Cmax
Maximum ethionamide plasma concentration
- CMC
Carboxy-methyl-cellulose
- CV%
Coefficient of Variation
- DPAG
Dry Powder Aerosol Generator
- DPPC
1,2 dipalmitoyl-sn-glycero-3-phosphatidylcholine
- ETH
Ethionamide
- FPF
Fine Particle Fraction
- FMO
Flavin-containing-monooxygenases
- GSD
Geometric Standard Deviation
- HIV
Human Immunodeficiency Virus
- HPLC
High Performance Liquid Chromatography
- IV
Intravenous
- K
Elimination rate constant
- MIC
Minimum Inhibitory Concentration
- MDR
Multi-Drug Resistant
- MMAD
Mass Median Aerodynamic Diameter
- MRT
Mean Residence Time
- MTB
Mycobacterium tuberculosis
- MW
Molecular weight
- PK
Pharmacokinetic
- PPs
Porous Particles
- PRO
Prothionamide
- SEM
Scanning Electron Microscopy
- t1/2
Half-life
- TB
Tuberculosis
- Tmax
Time to reach maximum ethionamide plasma concentration
- Tmin
Time to reach minimum ethionamide plasma concentration
- USP
United States Pharmacopeia
- UV
Ultra Violet
- WHO
World Health Organization
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
7.0 REFERENCES
- 1.O’Connor G, Gleeson LE, Fagan-Murphy A, Cryan SA, O’Sullivan MP, Keane J. Sharpening nature’s tools for efficient tuberculosis control: A review of the potential role and development of host-directed therapies and strategies for targeted respiratory delivery. Advanced drug delivery reviews. 2016;102:33–54. doi: 10.1016/j.addr.2016.04.024. [DOI] [PubMed] [Google Scholar]
- 2.Dooley KE, Phillips PP, Nahid P, Hoelscher M. Challenges in the clinical assessment of novel tuberculosis drugs. Advanced drug delivery reviews. 2016;102:116–22. doi: 10.1016/j.addr.2016.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.WHO. WHO Global Tuberculosis Report 2015. WHO; Geneva, Switzerland: 2015. [Google Scholar]
- 4.Hoagland DT, Liu J, Lee RB, Lee RE. New agents for the treatment of drug-resistant Mycobacterium tuberculosis. Advanced drug delivery reviews. 2016;102:55–72. doi: 10.1016/j.addr.2016.04.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Marais BJ. The global tuberculosis situation and the inexorable rise of drug-resistant disease. Advanced drug delivery reviews. 2016;102:3–9. doi: 10.1016/j.addr.2016.01.021. [DOI] [PubMed] [Google Scholar]
- 6.Van Deun A, Maug AK, Salim MA, Das PK, Sarker MR, Daru P, Rieder HL. Short, highly effective, and inexpensive standardized treatment of multidrug-resistant tuberculosis. Am J Respir Crit Care Med. 2010;182(5):684–92. doi: 10.1164/rccm.201001-0077OC. [DOI] [PubMed] [Google Scholar]
- 7.WHO, W. H. O. The shorter MDR-TB regimen. WHO; Geneva, Switzerland: 2016. http://www.who.int/tb/Short_MDR_regimen_factsheet.pdf. [Google Scholar]
- 8.CDC, C. f. D. C. a. P. Treatment of Tuberculosis. Morbidity and Mortality Weekly Report 2003. 52(RR-11):1–81. [PubMed] [Google Scholar]
- 9.WHO, W. H. O. Treatment of Tuberculosis Guidelines. WHO, World Health Organization; Geneva, Switzerland: 2010. [PubMed] [Google Scholar]
- 10.WHO, W. H. O. Guidelines for the programmatic management of drug-resistant tuberculosis. WHO, World Health Organization; Geneva, Switzerland: 2011. [PubMed] [Google Scholar]
- 11.Dooley KE, Mitnick CD, Ann DeGroote M, Obuku E, Belitsky V, Hamilton CD, Makhene M, Shah S, Brust JC, Durakovic N, Nuermberger E. Old drugs, new purpose: retooling existing drugs for optimized treatment of resistant tuberculosis. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America. 2012;55(4):572–81. doi: 10.1093/cid/cis487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mitnick CD, McGee B, Peloquin CA. Tuberculosis pharmacotherapy: strategies to optimize patient care. Expert opinion on pharmacotherapy. 2009;10(3):381–401. doi: 10.1517/14656560802694564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.BTA, B. T. A. A comparison of the toxicity of prothionamide and ethionamide: a report from the research committee of the British Tuberculosis Association. Tubercle. 1968;49(2):125–35. [PubMed] [Google Scholar]
- 14.Gupta D, Mital OP, Agarwal MC, Kansal HM, Nath S. A comparison of therapeutic efficacy and toxicity of ethionamide and prothionamide in Indian patients. J Indian Med Assoc. 1977;68(2):25–9. [PubMed] [Google Scholar]
- 15.Ethionamide. Tuberculosis. 2008;88(2):106–108. doi: 10.1016/S1472-9792(08)70009-X. [DOI] [PubMed] [Google Scholar]
- 16.Prothionamide. Tuberculosis. 2008;88(2):139–140. doi: 10.1016/S1472-9792(08)70020-9. [DOI] [PubMed] [Google Scholar]
- 17.Ibrahim M, Garcia-Contreras L. Mechanisms of absorption and elimination of drugs administered by inhalation. Therapeutic delivery. 2013;4(8):1027–45. doi: 10.4155/tde.13.67. [DOI] [PubMed] [Google Scholar]
- 18.Garcia-Contreras L, Fiegel J, Telko MJ, Elbert K, Hawi A, Thomas M, VerBerkmoes J, Germishuizen WA, Fourie PB, Hickey AJ, Edwards D. Inhaled large porous particles of capreomycin for treatment of tuberculosis in a guinea pig model. Antimicrobial agents and chemotherapy. 2007;51(8):2830–6. doi: 10.1128/AAC.01164-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sung JC, Garcia-Contreras L, Verberkmoes JL, Peloquin CA, Elbert KJ, Hickey AJ, Edwards DA. Dry powder nitroimidazopyran antibiotic PA-824 aerosol for inhalation. Antimicrobial agents and chemotherapy. 2009;53(4):1338–43. doi: 10.1128/AAC.01389-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kaur J, Muttil P, Verma RK, Kumar K, Yadav AB, Sharma R, Misra A. A hand-held apparatus for “nose-only” exposure of mice to inhalable microparticles as a dry powder inhalation targeting lung and airway macrophages. European journal of pharmaceutical sciences : official journal of the European Federation for Pharmaceutical Sciences. 2008;34(1):56–65. doi: 10.1016/j.ejps.2008.02.008. [DOI] [PubMed] [Google Scholar]
- 21.Schum M, Yeh HC. Theoretical evaluation of aerosol deposition in anatomical models of mammalian lung airways. Bulletin of mathematical biology. 1980;42(1):1–15. doi: 10.1007/BF02462363. [DOI] [PubMed] [Google Scholar]
- 22.Stokinger HE, Steadman LT, Wilson HB, Sylvester GE, Dziuba S, Labelle CW. Lobar deposition and retention of inhaled insoluble particulates. AMA archives of industrial hygiene and occupational medicine. 1951;4(4):346–53. [PubMed] [Google Scholar]
- 23.Auclair B, Nix DE, Adam RD, James GT, Peloquin CA. Pharmacokinetics of ethionamide administered under fasting conditions or with orange juice, food, or antacids. Antimicrob Agents Chemother. 2001;45(3):810–4. doi: 10.1128/AAC.45.3.810-814.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.WHO, W. H. O. Companion handbook to the WHO guidelines for the programmatic management of drug-resistant tuberculosis. WHO, World Health Organization; Geneva, Switzerland: 2014. [PubMed] [Google Scholar]
- 25.Thee S, Garcia-Prats AJ, Donald PR, Hesseling AC, Schaaf HS. A review of the use of ethionamide and prothionamide in childhood tuberculosis. Tuberculosis (Edinb) 2016;97:126–36. doi: 10.1016/j.tube.2015.09.007. [DOI] [PubMed] [Google Scholar]
- 26.Susan Hoe SM, Boraey Mohammed, Ivey James, Shamsaddini-Shahrbabak Abouzar, Finlay Warren, Vehring Reinhard. Substitution of L-Leucine with D-Leucine in spray-dried respirable powders for control of Pseudomonas aeruginosa infection. International Society for Aerosols (ISAM) 2013 [Google Scholar]
- 27.Edwards DA, Hanes J, Caponetti G, Hrkach J, Ben-Jebria A, Eskew ML, Mintzes J, Deaver D, Lotan N, Langer R. Large porous particles for pulmonary drug delivery. Science. 1997;276(5320):1868–71. doi: 10.1126/science.276.5320.1868. [DOI] [PubMed] [Google Scholar]
- 28.Garcia-Contreras L, Muttil P, Fallon JK, Kabadi M, Gerety R, Hickey AJ. Pharmacokinetics of sequential doses of capreomycin powder for inhalation in guinea pigs. Antimicrobial agents and chemotherapy. 2012;56(5):2612–8. doi: 10.1128/AAC.06145-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Garcia-Contreras L, Sung JC, Muttil P, Padilla D, Telko M, Verberkmoes JL, Elbert KJ, Hickey AJ, Edwards DA. Dry powder PA-824 aerosols for treatment of tuberculosis in guinea pigs. Antimicrobial agents and chemotherapy. 2010;54(4):1436–42. doi: 10.1128/AAC.01471-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sung JC, Padilla DJ, Garcia-Contreras L, Verberkmoes JL, Durbin D, Peloquin CA, Elbert KJ, Hickey AJ, Edwards DA. Formulation and pharmacokinetics of self-assembled rifampicin nanoparticle systems for pulmonary delivery. Pharmaceutical research. 2009;26(8):1847–55. doi: 10.1007/s11095-009-9894-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Vehring R. Pharmaceutical particle engineering via spray drying. Pharmaceutical research. 2008;25(5):999–1022. doi: 10.1007/s11095-007-9475-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Vanbever R, Mintzes JD, Wang J, Nice J, Chen D, Batycky R, Langer R, Edwards DA. Formulation and physical characterization of large porous particles for inhalation. Pharm Res. 1999;16(11):1735–42. doi: 10.1023/a:1018910200420. [DOI] [PubMed] [Google Scholar]
- 33.Gervelas C, Serandour AL, Geiger S, Grillon G, Fritsch P, Taulelle C, Le Gall B, Benech H, Deverre JR, Fattal E, Tsapis N. Direct lung delivery of a dry powder formulation of DTPA with improved aerosolization properties: effect on lung and systemic decorporation of plutonium. J Control Release. 2007;118(1):78–86. doi: 10.1016/j.jconrel.2006.11.027. [DOI] [PubMed] [Google Scholar]
- 34.Lechuga-Ballesteros D, Charan C, Stults CL, Stevenson CL, Miller DP, Vehring R, Tep V, Kuo MC. Trileucine improves aerosol performance and stability of spray-dried powders for inhalation. Journal of pharmaceutical sciences. 2008;97(1):287–302. doi: 10.1002/jps.21078. [DOI] [PubMed] [Google Scholar]
- 35.Lucas P, Anderson K, Potter UJ, Staniforth JN. Enhancement of small particle size dry powder aerosol formulations using an ultra low density additive. Pharm Res. 1999;16(10):1643–7. doi: 10.1023/a:1011981326827. [DOI] [PubMed] [Google Scholar]
- 36.Arbex MA, Varella M, Siqueira HR, Mello FA. Antituberculosis drugs: drug interactions, adverse effects, and use in special situations. Part 2: second line drugs. J Bras Pneumol. 2010;36(5):641–56. doi: 10.1590/s1806-37132010000500017. [DOI] [PubMed] [Google Scholar]
- 37.Peloquin CA. Therapeutic drug monitoring in the treatment of tuberculosis. Drugs. 2002;62(15):2169–83. doi: 10.2165/00003495-200262150-00001. [DOI] [PubMed] [Google Scholar]
- 38.Zhu M, Namdar R, Stambaugh JJ, Starke JR, Bulpitt AE, B SE, Peloquin CA. Population pharmacokinetics of ethionamide in patients with tuberculosis. Tuberculosis (Edinb) 2002;82(2–3):91–6. doi: 10.1054/tube.2002.0330. [DOI] [PubMed] [Google Scholar]
- 39.Pfizer WPI. Prescribing information. Pfizer, Wyeth Pharmaceuticals Inc.; Philadelphia, PA: 2016. Trecator (Ethionamide tablets, USP) [Google Scholar]
- 40.Jenner PJ, Ellard GA, Gruer PJ, Aber VR. A comparison of the blood levels and urinary excretion of ethionamide and prothionamide in man. J Antimicrob Chemother. 1984;13(3):267–7. doi: 10.1093/jac/13.3.267. [DOI] [PubMed] [Google Scholar]
- 41.Dickinson JM, Mitchison DA. In vitro and in vivo studies to assess the suitability of antituberculous drugs for use in intermittent chemotherapy regimens. Tubercle. 1968;49(Suppl):66–70. doi: 10.1016/s0041-3879(68)80051-0. [DOI] [PubMed] [Google Scholar]
- 42.Dickinson JM, Mitchison DA. Short-term intermittent chemotherapy of experimental tuberculosis in the guinea pig. Tubercle. 1966;47(4):381–393. [Google Scholar]
- 43.Dickinson JM. The suitability of new drugs for intermittent chemotherapy of tuberculosis. An experimental study. Scand J Respir Dis Suppl. 1969;69:91–98. [PubMed] [Google Scholar]
- 44.Mitchison DA, Dickinson JM. Laboratory aspects of intermittent drug therapy. Postgrad Med J. 1971;47(553):737–41. doi: 10.1136/pgmj.47.553.737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Palmer AL, Leykam VL, Larkin A, Krueger SK, Phillips IR, Shephard EA, Williams DE. Metabolism and pharmacokinetics of the anti-tuberculosis drug ethionamide in a flavin-containing monooxygenase null mouse. Pharmaceuticals (Basel) 2012;5(11):1147–59. doi: 10.3390/ph5111147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ishizuka H, Konno K, Shiina T, Naganuma H, Nishimura K, Ito K, Suzuki H, Sugiyama Y. Species differences in the transport activity for organic anions across the bile canalicular membrane. J Pharmacol Exp Ther. 1999;290(3):1324–30. [PubMed] [Google Scholar]
- 47.Garcia-Contreras L. In vivo animal models for controlled-release pulmonary drug delivery. In: Hugh DC, Smyth AJH, editors. Controlled pulmonary drug delivery. Springer Science+Business Media, LLC.; NY: 2011. pp. 443–475. [Google Scholar]


