Abstract
Purpose
To re-evaluate the population-based incidence of idiopathic intracranial hypertension (IIH) and determine if it mirrors the rise in obesity.
Design
Retrospective, population-based cohort.
Participants
All residents of Olmsted County, Minnesota, USA, diagnosed with idiopathic intracranial hypertension between January 1, 1990, and December 31, 2014.
Methods
All cases of IIH were identified using the Rochester Epidemiology Project, which is a record-linkage system of medical records for all patient-physician encounters among Olmsted County, Minnesota residents. All medical records were reviewed to confirm a diagnosis of idiopathic intracranial hypertension. The incidence rates of IIH were compared against the incidence of obesity in Minnesota over the same time period.
Main Outcome Measures
Incidence of IIH, lumbar puncture opening pressures, body mass index.
Results
There were 63 new cases of IIH, yielding an overall age- and sex-adjusted annual incidence of 1.8/100,000 (95% CI: 1.3–2.2) between 1990 and 2014. It increased from 1.0/100,000 (1990–2001) to 2.4/100,000 (2002–2014) (p=0.007). The incidence of IIH was 3.3/100,000 in women and 0.3/100,000 in men (p=<0.001). In obese women aged 15 to 44 years, the incidence was 22.0/100,000 compared to 6.8/100,000 among all female patients in the same age group. A strong correlation was observed between IIH incidence rates and obesity rates in Minnesota (R2=0.70, p=0.008).
Conclusion
The incidence of IIH has increased since 1990, which is highly correlated with the rise in obesity during the same time period.
Keywords: idiopathic intracranial hypertension, pseudotumor cerebri, obesity, incidence
Idiopathic intracranial hypertension (IIH) is a condition of increased intracranial pressure of unknown etiology, often producing papilledema and visual loss.1–3 IIH typically occurs in obese women in the childbearing years. The incidence of obesity has been rapidly increasing since the 1970s.4 Because obesity is a large risk factor for IIH, the incidence of IIH conceivably could rise in parallel with the current epidemic of obesity, but there have been no studies to evaluate this possibility. Much of the knowledge on the incidence of IIH came from a prior epidemiology study from the Rochester Epidemiology Project (REP), which demonstrated an incidence of 1.0 per 100,000 from 1976 through 1990.5 The goal of this study was to re-evaluate the population-based incidence of IIH using the REP and to determine if the incidence of IIH mirrors the large rise in obesity over the past 20 years.
Methods
The medical records of all patients diagnosed in Olmsted County with idiopathic intracranial hypertension, intracranial hypertension, pseudotumor cerebri, or papilledema, from January 1, 1990, through December 31, 2014, were reviewed. Potential subjects were identified using the Rochester Epidemiology Project, a multicenter medical records database designed to capture data on all patient-physician encounters in Olmsted County, Minnesota.6, 7 This study was approved by the Institutional Review Board of the Mayo Clinic and the Olmsted Medical Center, Minnesota. It conforms to the requirements of the United States Health Insurance Portability and Accountability Act (HIPAA) and adheres to the tenets of the Declaration of Helsinki.
A total of 427 patients were diagnosed with at least one of the above conditions during the 24-year study period. Patients were classified as having IIH if they met the Modified Dandy criteria, which included signs and symptoms of increased intracranial pressure, no localizing neurologic finding except cranial nerve VI palsies, normal neuroimaging, lumbar puncture opening pressure >250 mm H2O with normal cerebrospinal fluid constituents, and no other apparent cause. Patients presenting with papilledema and borderline opening pressures (200–250 mm H2O) were also included in the study.3, 8 Patients without papilledema were excluded from this study.
Data on the patients’ sex, ethnicity, age at diagnosis, body mass index (BMI), ocular and medical histories, risk factors, presenting signs and symptoms, and treatments were obtained from the medical records. Obesity was defined by a BMI ≥30. Continuous data were presented as a mean and standard deviation, and categorical data were presented as counts and percentages. Incidence rates and confidence intervals were calculated using population figures in Olmsted County. Age- and sex-adjusted rates were based on the total U.S. white population in 2000. Yearly gender- and age-specific incidence rates were determined by dividing the number of IIH cases within each group by the estimated total Olmsted County resident population. The exact number of obese individuals in Olmsted County was unknown; an estimate of 20% was used based on available statewide rates during the study period. Population figures for 1990, 2000, and 2010 came from the U.S. census data and population; figures for inter-census years were estimated using linear interpolation. Poisson regression models were used to test for trends over time, across age groups, and between genders. Correlation between age- and sex-adjusted IIH incidence and Minnesota obesity rates in two-year categories were estimated using Pearson’s correlation coefficient.
Results
From 1990 through 2014, 63 patients were diagnosed in Olmsted County with IIH, 92.1% of who were female (Table 1). Thirty-eight (60.3%) were obese, more than half of whom were morbidly obese (52.6%). BMI was unknown for 17 patients.
Table 1.
Historical and clinical characteristics of the 63 patients with IIH
| N (%) | |
|---|---|
| Sex | |
| Females | 58 (92.1) |
| Ethnicity | |
| Caucasian | 56 (88.9) |
| African American | 1 (1.6) |
| Native American | 0 (0.0) |
| Asian | 0 (0.0) |
| Other | 4 (6.3) |
| Unknown | 2 (3.2) |
| Body Mass Index | |
| <30 | 8 (12.7) |
| 30–40 | 18 (28.6) |
| ≥40 | 20 (31.7) |
| Unknown | 17 |
The incidence rates of IIH in the Olmsted population are summarized in Table 2. The overall age- and sex-adjusted incidence rate was 1.8/100,000 persons. The IIH incidence increased significantly over the study period from 1.0/100,000 persons between 1990 and 2001 to 2.4/100,000 persons between 2002 and 2014. The incidence of IIH was significantly higher in females than in males, with an overall age-adjusted incidence rate of 3.3/100,000 in females in contrast to 0.3/100,000 in males (p-value<0.001). From 2002 until 2014, the incidence rate had risen to 4.2/100,000 in females and 0.5/100,000 in males.
Table 2.
Idiopathic intracranial hypertension incidence rates and BMI by year, sex, and age in Olmsted County from 1990 through 2014
| Group | Total N | Incidence Rate (95% CI) Per 100,000 Persons |
|---|---|---|
| Years | Age- and Sex- Adjusted Incidence Rate | |
| 1990–2014 | 63 | 1.759 (1.324, 2.194) |
| 1990–2001 | 17 | 1.046 (0.559, 1.575) |
| 2002–2014 | 46 | 2.359 (1.676, 3.042) |
| p-value: 0.007 | ||
| Gender 1990–2014 | Age-Adjusted Incidence Rate | |
| Males | 5 | 0.290 (0.035, 0.544) |
| Females | 58 | 3.277 (2.432, 4.121) |
| p-value: <0.001 | ||
| Gender 1990–2001 | Age-Adjusted Incidence Rate | |
| Males | 0 | 0.000 (0.000, 0.000) |
| Females | 17 | 2.129 (1.115, 3.143) |
| p-value: <0.001 | ||
| Gender 2002–2014 | Age-Adjusted Incidence Rate | |
| Males | 5 | 0.530 (0.064, 0.997) |
| Females | 41 | 4.247 (2.945, 5.549) |
| p-value: <0.001 |
Adjusted to the total U.S. white population in 2000. The calculated p-values compare the crude incidence rates. The age-, sex-, and year-adjusted rates are presented to generalize IIH incidence to the U.S. white population.
Table 3 shows the age- and sex-specific incidence rates of IIH in Olmsted County over the study period. The incidence rate peaked at 11.7/100,000 persons for females between the ages of 25 and 34 years, while the rate peaked for males between the ages of 0 and 14 years at 0.8/100,000 persons. Based on Centers for Disease Control (CDC) data for obesity in Minnesota among 15- to 44-year-olds in 2000, the incidence among obese 15- to 44-year-olds was 11.1/100,000 compared to 3.5/100,000 among all patients in the same age group. The incidence rate among obese female patients in this age group was 22.0/100,000 persons compared to 6.8/100,000 persons among all the female study patients in the same age group. Comparing IIH incidence rates to obesity rates in Minnesota from 1990 through 2014 (Figure 1), there was a strong correlation observed between obesity and the age-, sex-, and year-adjusted IIH incidence rates (R2=0.70, p=0.008).
Table 3.
Age- and sex-specific average annual incidence rates of IIH in Olmsted County from 1990 through 2014.
| Female | Male | Total | ||||
|---|---|---|---|---|---|---|
| Group | N | Incidence | N | Incidence | N | Incidence |
| Age (years) | ||||||
| 0–14 | 4 | 1.151 | 3 | 0.823 | 7 | 0.983 |
| 15–24 | 19 | 9.372 | 0 | 0.000 | 19 | 4.718 |
| 25–34 | 30 | 11.673 | 1 | 0.396 | 31 | 6.084 |
| 35–44 | 4 | 1.643 | 0 | 0.000 | 4 | 0.823 |
| 45+ | 1 | 0.169 | 1 | 0.195 | 2 | 0.181 |
| All age groups | 58 | 3.534 | 5 | 0.318 | 63 | 1.961 |
| Age-adjusteda | – | 3.325 | – | 0.287 | – | 1.816 |
| 95% CI | 2.465 – 4.185 | 0.033 – 0.542 | 1.366 – 2.267 | |||
| Crude Annual Incidence Rate | ||||||
| Total | 58 | 3.534 | 5 | 0.318 | 63 | 1.961 |
| Aged 15–44 | 48 | 6.826 | 1 | 0.144 | 49 | 3.508 |
| Obese, aged 15–44b | 31 | 22.041 | 0 | 0.000 | 31 | 11.097 |
Adjusted to the total U.S. white population in 2000.
Accurate data are unavailable on the prevalence of obesity for Olmsted County. These figures assume an obesity rate of 20%, approximated based on CDC data for obesity in Minnesota in 2000. Obesity was defined as body mass index of ≥30.
Figure 1.
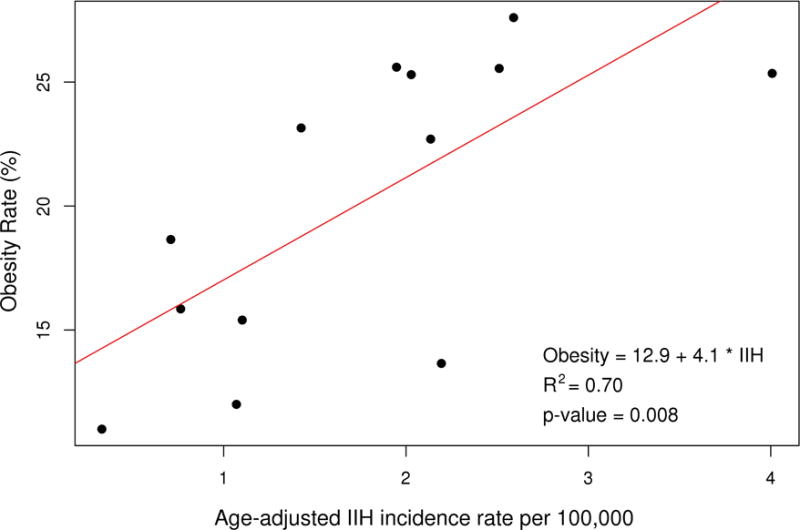
Correlation between age-adjusted IIH incidence and obesity rates in Minnesota.
Discussion
A prior study utilizing the REP to evaluate the epidemiology of IIH before 1990 found a crude annual incidence of 1.0/100,000 persons and 3.3/100,000 in females 15 to 44 years of age in Olmsted Country, Minnesota.5 This study has been used to quote the incidence of IIH since it was published in 1993.9 Looking at the same patient population, the current study found that the crude annual incidence rate has doubled in Olmsted County, Minnesota, to 2.0/100,000 persons between 1990 and 2014 (p=0.038). In addition, within the time period of the current study, there was a significant rise in the incidence of IIH from the first half of the study at 1.0/100,000 persons to 2.4/100,000 persons in the second half of the study.
In the U.S., the incidence of obesity has been rising from the 1970s until 2014. The prevalence of adulthood obesity, as defined by a BMI of ≥30, was 12.7% from 1976 until 1980, 20.5% from 1988 until 1994, 32.2% from 2003 until 2004, and 34.9% from 2011 until 2012.4 Among children, 16.9% were obese as defined by a BMI at or above the 95th percentile.4 Obesity in Minnesota in 1990 was <10%, which increased from 15% to 19% in 2000, 20% to 24% in 2010, and 27.6% in 2014 (CDC data).10 Olmsted County mirrors this trend and now has an adulthood obesity of 27% (CDC data).11 Overall, a strong correlation was found between obesity rates in Minnesota over the study period and the corresponding IIH incidence rates (Figure 1. R2=0.70, p=0.008).
Obesity is known to be a large risk factor for IIH. Durcan et al. found that, in Iowa and Louisiana, the incidence of IIH was 19/100,000 among obese women aged 20 to 44 years who were ≥20% over ideal weight.9 Numerous studies have confirmed that the vast majority of patients with IIH are obese women of childbearing age.5, 12, 13 In addition, a recent multicenter case control study demonstrated a “dose-response effect” where higher BMI was associated with a progressively greater risk of IIH.14 Some studies suggest that environmental factors, such as obesity rates, are responsible for different incidences of IIH in their populations. In Japan, where obesity is less common, the incidence of IIH was found to be only 0.03/100,000,15 whereas the incidence was reported to be 2.2/100,000 in Libya.16 Our study confirmed the association between obesity and IIH incidence, where the rate was 22.0/100,000 in obese females aged 15 to 44 years compared to 6.8/100,000 among all female patients in the same age group.
The limitations of the study include the retrospective design, the racial homogeneity of the study population, and incomplete data on obesity rates in the county and state. Given the retrospective nature of this investigation, some patients unavoidably had poor follow-up or incomplete medical records. Secondly, with 90% of the study population identifying themselves as Caucasian, it may be difficult to extrapolate these results to other non-Caucasian populations. Lastly, the exact data on obesity rates in Minnesota could not be found for some of the years within the study period. Olmsted county-specific obesity rates were unavailable during the study years; thus, Minnesota obesity rates were used under the assumption that the obesity rates in Olmsted County were very similar. Despite these limitations, this study yields invaluable results, because it provides a population-based incidence, which directly compares with a prior incidence study also using the Rochester Epidemiology project.5 This comparison clearly demonstrates an increase in the incidence of IIH that mirrors the rise in obesity.
In conclusion, this study shows that the incidence rates of IIH and obesity have risen in parallel since 1990. With no sign of obesity rates declining in the U.S., recognizing and treating patients with IIH promptly are, therefore, of increasing importance. Although these patients may only have headaches initially, they can develop severe visual impairment.17, 18 Additionally, determining the current incidence of IIH is important, as the annual cost of IIH in the U.S. alone has been estimated to exceed 444 million dollars.19
Acknowledgments
This work was supported in part by an unrestricted grant to the Department of Ophthalmology by Research to Prevent Blindness, Inc., New York, NY. This study was made possible using the resources of the Rochester Epidemiology Project, which is supported by the National Institute on Aging of the National Institutes of Health under R01AG034676. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Financial Support: Research to Prevent Blindness, Inc., New York, NY. Rochester Epidemiology Project, National Institute on Aging of the National Institutes of Health, R01AG034676. The sponsor or funding organization had no role in the design or conduct of this research.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Meeting Presentation: (Re-evaluating the Incidence of Idiopathic Intracranial Hypertension in an Era of Increasing Obesity, Chicago, IL, October 15–18, 2016).
Conflict of Interest: No conflicting relationship exists for any author.
References
- 1.Chen J, Wall M. Epidemiology and risk factors for idiopathic intracranial hypertension. Int Ophthalmol Clin. 2014;54:1–11. doi: 10.1097/IIO.0b013e3182aabf11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Friedman DI. Idiopathic intracranial hypertension. Curr Pain Headache Rep. 2007;11:62–68. doi: 10.1007/s11916-007-0024-8. [DOI] [PubMed] [Google Scholar]
- 3.Wall M. Idiopathic intracranial hypertension. Neurol Clin. 2010;28:593–617. doi: 10.1016/j.ncl.2010.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA. 2014;311:806–814. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Radhakrishnan K, Ahlskog JE, Cross SA, et al. Idiopathic intracranial hypertension (pseudotumor cerebri). Descriptive epidemiology in Rochester, Minn, 1976 to 1990. Arch Neurol. 1993;50:78–80. doi: 10.1001/archneur.1993.00540010072020. [DOI] [PubMed] [Google Scholar]
- 6.Kurland LT, Molgaard CA. The patient record in epidemiology. Sci Am. 1981;245:54–63. doi: 10.1038/scientificamerican1081-54. [DOI] [PubMed] [Google Scholar]
- 7.Melton LJ., 3rd History of the Rochester Epidemiology Project. Mayo Clin Proc. 1996;71:266–274. doi: 10.4065/71.3.266. [DOI] [PubMed] [Google Scholar]
- 8.Dandy WE. Intracranial Pressure without Brain Tumor: Diagnosis and Treatment. Ann Surg. 1937;106:492–513. doi: 10.1097/00000658-193710000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Durcan FJ, Corbett JJ, Wall M. The incidence of pseudotumor cerebri. Population studies in Iowa and Louisiana. Arch Neurol. 1988;45:875–877. doi: 10.1001/archneur.1988.00520320065016. [DOI] [PubMed] [Google Scholar]
- 10.CDC. Obesity Trends Among US Adults Between 1985 and 2010. https://www.cdc.gov/obesity/downloads/obesity_trends_2010.pdf. 2010 Accessed 08.11.16.
- 11.CDC. Obesity Prevention - Community Profile: Olmsted County, Minnesota. http://www.cdc.gov/nccdphp/dch/programs/communitiesputtingpreventiontowork/communities/profiles/obesity-mn_olmsted-county.htm. 2016 Accessed 08.11.16.
- 12.Kesler A, Gadoth N. Epidemiology of idiopathic intracranial hypertension in Israel. J Neuroophthalmol. 2001;21:12–14. doi: 10.1097/00041327-200103000-00003. [DOI] [PubMed] [Google Scholar]
- 13.Raoof N, Sharrack B, Pepper IM, Hickman SJ. The incidence and prevalence of idiopathic intracranial hypertension in Sheffield, UK. Eur J Neurol. 2011;18:1266–1268. doi: 10.1111/j.1468-1331.2011.03372.x. [DOI] [PubMed] [Google Scholar]
- 14.Daniels AB, Liu GT, Volpe NJ, et al. Profiles of obesity, weight gain, and quality of life in idiopathic intracranial hypertension (pseudotumor cerebri) Am J Ophthalmol. 2007;143:635–641. doi: 10.1016/j.ajo.2006.12.040. [DOI] [PubMed] [Google Scholar]
- 15.Yabe I, Moriwaka F, Notoya A, et al. Incidence of idiopathic intracranial hypertension in Hokkaido, the northernmost island of Japan. J Neurol. 2000;247:474–475. doi: 10.1007/s004150070182. [DOI] [PubMed] [Google Scholar]
- 16.Radhakrishnan K, Thacker AK, Bohlaga NH, et al. Epidemiology of idiopathic intracranial hypertension: a prospective and case-control study. J Neurol Sci. 1993;116:18–28. doi: 10.1016/0022-510x(93)90084-c. [DOI] [PubMed] [Google Scholar]
- 17.Corbett JJ, Savino PJ, Thompson HS, et al. Visual loss in pseudotumor cerebri. Followup of 57 patients from five to 41 years and a profile of 14 patients with permanent severe visual loss. Arch Neurol. 1982;39:461–474. doi: 10.1001/archneur.1982.00510200003001. [DOI] [PubMed] [Google Scholar]
- 18.Wall M, George D. Idiopathic intracranial hypertension. A prospective study of 50 patients. Brain. 1991;114(Pt 1A):155–180. [PubMed] [Google Scholar]
- 19.Friesner D, Rosenman R, Lobb BM, Tanne E. Idiopathic intracranial hypertension in the USA: the role of obesity in establishing prevalence and healthcare costs. Obes Rev. 2011;12:e372–380. doi: 10.1111/j.1467-789X.2010.00799.x. [DOI] [PubMed] [Google Scholar]


