Abstract.
Ocular gnathostomiasis is rather a rare food-borne zoonosis caused by infection with the larvae of several species of genus Gnathostoma and is a representative ocular larva migrans syndrome. In our previous literature survey, we found 73 cases of ocular gnathostomiasis reported up to and including 2009, though additional sporadic cases have been reported in Asia and the Americas since that report. Here, we review 10 additional cases reported since 2010, and also update current findings regarding epidemiological and clinical features in affected patients.
INTRODUCTION
Some zoonotic helminth parasites, especially the larval stage of zoonotic nematodes, can cause eye infections in humans.1 Gnathostomiasis is a food-borne zoonotic nematodiasis caused by the larval stage, or sometimes by immature/mature adults of Gnathostoma spp. Humans become infected by ingesting raw or undercooked meat from fish, amphibians, reptiles, birds, or mammals, which can carry advanced third stage larvae (AL3) of Gnathostoma spp., and serve as second-intermediate and/or paratenic hosts.2 Among 13 valid species reported (six in Asia, seven in the Americas), five (four in Asia, one in Latin America) have been identified as pathogenic for humans. When ingested, Gnathostoma AL3 larvae preferentially migrate to the skin, causing cutaneous lesions such as migratory panniculitis, or serpiginous eruptions (cutaneous larva migrans syndrome). The larvae also occasionally migrate to unexpected sites such as visceral organs (visceral larva migrans syndrome), the eyes (ocular larva migrans syndrome), and/or the central nervous system (neuro-gnathostomiasis), leading to serious clinical manifestations and possible death.2 Since several helminth parasites can cause larva migrans syndrome of any types, identification of causative pathogens is critically necessary for accurate diagnosis and treatment.1
In our previous comprehensive literature survey, we examined 73 ocular gnathostomiasis cases.3 Recently, we performed another thorough and extensive literature survey, and found 10 additional cases of ocular gnathostomiasis reported since 2010. Including findings presented in our previous review, the epidemiological and clinical features of ocular gnathostomiasis are summarized herein.
METHODS
Published reports that underwent our review were identified by a search of PubMed through December 2016 using the following search strings: “gnathostoma” and “ocular” or “eye,” “gnathostomiasis” and “ocular” or “eye,” and “gnathostomosis” and “ocular” or “eye.” Only studies that included ophthalmological manifestations of gnathostomiasis were selected, which were reviewed for relevance by the present authors. References listed in those papers were checked for cases not cited. Additional searches of Japanese and Chinese language literature were performed using Japana Centra Revuo Medicina (Ichushi), Google Scholar, and cnki.net. In addition, some case reports that appeared in local journals were obtained from the Library of Nara Medical University, Kashiwara, Japan.
RESULTS
Since our initial survey performed of cases reported up to and including 2009, we found an additional nine case reports of ocular gnathostomiasis and two of our own unpublished cases (one each from Thailand and Venezuela), which were listed in Table 1.4–12 Following careful investigation of each report, two cases reported from India 5,6 were determined to be the same case. Therefore, during the survey period the actual number of unique cases from India is four and the total number is 10 including two unpublished cases. Apart from four cases from India, three were from Latin America (one each from Brazil, Ecuador, and Venezuela) and three from Asia (one each from Cambodia, Korea, and Thailand) (Table 1).
Table 1.
Ocular gnathostomiasis cases reported since 2010
| No.* | Year | Sex | Age (years) | Affected side | Country | Worm recovery | Reference |
|---|---|---|---|---|---|---|---|
| 74 | 2011 | F | 62 | L | India | Yes | 4 |
| 75† | 2011 | M | 44 | R | India | Yes | 5 |
| 75† | 2012 | M | 41 | R | India | Yes | 6 |
| 76 | 2012 | M | 15 | R | Korea (VNM) | No | 7 |
| 77 | 2013 | M | 55 | L | India | Yes | 8 |
| 78 | 2015 | M | 37 | L | Cambodia | Yes | 9 |
| 79 | 2015 | M | 37 | L | Ecuador | Yes | 10 |
| 80 | 2016 | M | 30 | L | Brazil | Yes | 11 |
| 81 | 2016 | M | 29 | R | India | Yes | 12 |
| 82‡ | 2017 | M | 69 | L | Venezuela | Yes | Benavides and others |
| 83‡ | 2017 | M | 22 | L | Thailand | Yes | Sawanyawisuth and others |
Nine of the affected patients in the present 10 cases were male and only one was female. Their ages ranged from 15 to 62 years (mean 39 and median 37 years). The affected side of the eye was; left eye = 7 and right eye = 3. Nine cases were diagnosed by morphological findings of worms surgically extirpated from the eye, whereas one case from Korea was suspected of having ocular gnathostomiasis based on subretinal tracks in the right eye, after which the diagnosis was confirmed by results of immuno-serological testing using western blotting. As for clinical aspects, all of these patients complained of visual disturbance, which became normalized after surgical extirpation of the worm, except for the case from Korea in which no worm was found in the eye.
DISCUSSION
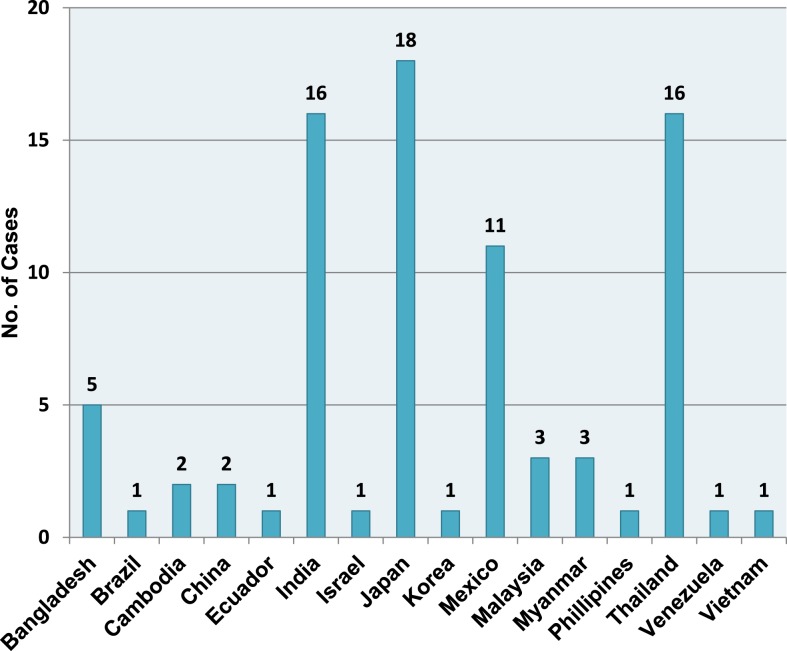
The combination of our previous3 and present literature survey, as well as our own experience revealed a total of 83 cases of ocular gnathostomiasis. In terms of geographical distribution, three countries, Brazil, Korea, and Venezuela, were added to the 12 countries listed in our previous review. From Venezuela, gnathostomiasis of any clinical manifestations have never been reported and this ocular case is the first one in the country, although the patient seemed to be infected in United States while he has been to leisure fishing holidays. Among all 15 countries, only four, India, Japan, Mexico, and Thailand, have more than 10 cases reported, while there were fewer than five in each of the other 11 countries (Figure 1). Ocular gnathostomiasis is highly endemic in Japan, Mexico, and Thailand, where thousands of cutaneous gnathostomiasis cases have been recorded.2 Thus, the relatively high incidence of ocular cases in these countries is not surprising. On other hand, in India, where 16 cumulative ocular cases are known thus far, very few cutaneous gnathostomiasis cases have been reported,13,14 even when the very old report of 11 cases by Maplestone15 is included. Because of the high incidence of ocular cases in India, we speculate that many more hidden cases of cutaneous and/or visceral gnathostomiasis have actually occurred there.
Figure 1.
Geographic distribution of ocular gnathostomiasis cases. Country names are listed in alphabetical order. This figure appears in color at www.ajtmh.org.
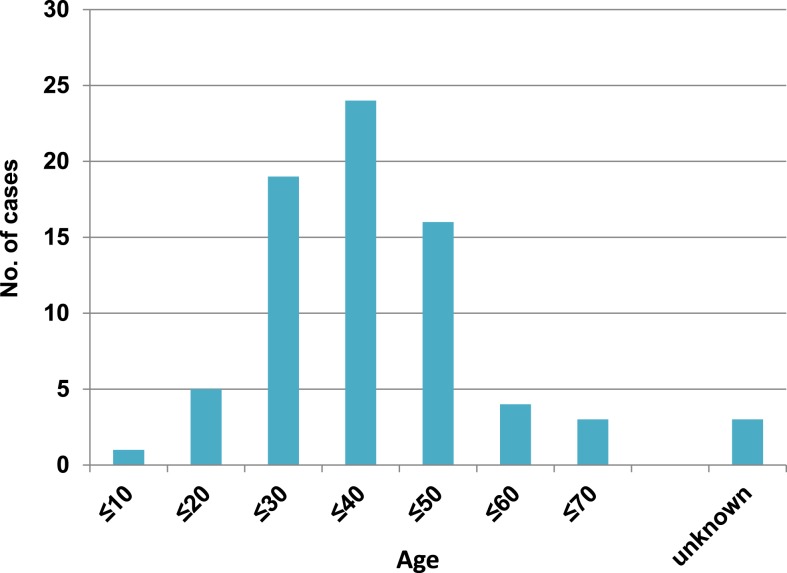
In our previous review, the ratio of males to females was approximately 6 to 4. In contrast, the ratio was 9 to 1 in the most recent 10 cases found in the present review. Thus, when the previous and present findings are combined, the ratio of males to females for ocular gnathostomiasis is approximately 5 to 3 (46 males, 31 females, and 6 unknown). Male dominance in gnathostomiasis cases is generally well known and has been attributed to the higher frequency of males who consume raw fish.16 In this review as well as our previous review,3 the majority of patients were middle-aged over 30 years old as shown in Figure 2. This again is assumed to be related to the raw fish consumption with alcoholic drinks.2,16
Figure 2.
Age distribution of ocular gnathostomiasis cases. This figure appears in color at www.ajtmh.org.
In the present case from Korea, the patient was a 15-year-old male who had a history of travel to Vietnam, where he consumed raw wild boar meat and lobster approximately 8 months before onset of the disease. Since Korea itself is an endemic area for several Gnathostoma species and an autochthonous case has been reported there,17 whether this patient was infected with Gnathostoma during travel in Vietnam or during daily life in Korea remains to be clarified.
Based on the cases reported from highly endemic countries, such as Mexico, Thailand, and Japan, ocular gnathostomiasis may only be the tip of the iceberg, with very large numbers of cutaneous or other gnathostomiasis patients possibly not accurately reported. In this regard, physicians should pay attention for possible gnathostomiasis cases among family and community members associated with affected patients.
REFERENCES
- 1.Otranto D, Eberhard ML, 2011. Zoonotic helminths affecting the human eye. Parasit Vectors 4: 41 http://www.parasitesandvectors.com/content/4/1/41. Accessed January 28, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nawa Y, Maleewong W, Intapan PM, Díaz-Camacho SP, 2015. Chapter 21. Gnathostoma. Lihua Xiao, Una Ryan, Yaoyu Feng , eds Biology of Food-borne Diseases. Boca Raton, London, NY: CRC Press, Taylor & Francis, 405–426. [Google Scholar]
- 3.Nawa Y, Katchanov J, Yoshikawa M, Rojekittikhun B, Dekumyoy P, Kusolusuk T, Wattanakulpanich D, 2010. Ocular gnathostomiasis: a comprehensive review. J Trop Med Parasitol 33: 77–86. [Google Scholar]
- 4.Islam S, Bhattacharjee H, Das D, Medhi J, 2011. Gnathostoma and gnathostomiasis in North East India: II. On the occurrence of an advanced third stage larva of Gnathostoma spinigerum Owen, 1836 in human eye with a description of its light microscopic morphology. J Vet Parasitol 25: 18–20. [Google Scholar]
- 5.Mathews AS, Shafi T, Radhakrishnan N, Pillari GS, 2015. Intraocular gnathostomiasis—A case report. Kerala. J Ophthalmol 23: 306–308. [Google Scholar]
- 6.Pillari GS, Kumar A, Radhakrishnan N, Maniyelil J, Shafi T, Dinesh KR, Karim S, 2012. Case report: intraocular gnathostomosis: report of a case and a literature review. Am J Trop Med Hyg 86: 620–623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yang JH, Kim MS, Kim ES, Na BK, Yu SY, Kwak HW, 2012. Imported intraocular gnathostomiasis with subretinal tracks confirmed by western blot assay. Korean J Parasitol 50: 73–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sujata DN, Renu BS, 2013. Intraocular gnathostomiasis from coastal part of Maharashtra. Trop Parasitol 3: 82–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hem S, Tarantola A, Chheang R, Nop P, Kerléguer A, 2015. First reported case of intraocular Gnathostoma spinigerum in Canbodia. Bull Soc Pathol Exot 108: 312–315. [DOI] [PubMed] [Google Scholar]
- 10.Khanifar AA, Espiritu MJ, Myung JS, Aaker GD, Schuetz AN, D’Amico DJ, Paul Chan RV, 2015. Three-dimensional spectral domain optical coherence tomography and light microscopy of an intravitreal parasite. J Ophthalmic Inflamm Infect 5: 33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chaves CM, Chaves C, Zoroquiain P, Belfort R, Jr, Burnier MN, Jr, 2016. Ocular gnathostomiasis in Brazil: a case report. Ocul Oncol Pathol 2: 194–196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rawat P, Gautam M, Jain NC, Jain R, 2016. Intraocular gnathostomiasis: a rare case report from central India. Indian J Ophthalmol 64: 235–237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mukherjee A, Ahmed NH, Samantaray JC, Mirdha BR, 2012. A rare case of cutaneous larva migrans due to Gnathostoma sp. Indian J Med Microbiol 30: 356–358. [DOI] [PubMed] [Google Scholar]
- 14.Subhedar V, Nandedkar S, Jain M, Bajpai T, 2014. Gnathostomiasis: a rare case of cutaneous creeping eruptions. Indian J Dermatopathol Diag Dermatol 1: 32–34. [Google Scholar]
- 15.Maplestone PA, 1929. A case of human infection with a Gnathostome in India. Ind Med Gaz 64: 610–614. [PMC free article] [PubMed] [Google Scholar]
- 16.Ando K, 2003. Chapter 7. Gnathostomiasis (2) Gnathostoma nipponicum Otsuru M, Kamegai S, Hayashi S, eds. Series monograph, Progress of Medical Parasitology in Japan. Tokyo, Japan: Meguro Parasitological Museum, 507–518. [Google Scholar]
- 17.Kim JH, Lim H, Hwang YS, Kim TY, Han EM, Shin EH, Chai JY, 2013. Gnathostoma spinigerum infection in the upper lip of a Korean woman: an autochthonous case in Korea. Korean J Parasitol 51: 343–347. [DOI] [PMC free article] [PubMed]