Abstract.
Despite the availability of proven measures to prevent the disease, rabies now kills more people in Myanmar than malaria. Although there are challenges in controlling rabies in such a large and culturally diverse country, Myanmar’s successful National Malaria Control Program demonstrates what can be achieved with sufficient political, financial, and scientific commitment. Presently, however, Myanmar lacks a comparable program to coordinate the multifaceted approach that is necessary to control rabies. The national government has invested heavily in improving access to postexposure prophylaxis, but there should also be an emphasis on other, more cost-effective strategies, particularly mass canine vaccination, which has been an essential component of successful rabies elimination programs in other countries. Continued health system strengthening is also required to improve primary health care, while decentralization of laboratory diagnostic services is needed to facilitate more timely, rational, and cost-effective use of postexposure prophylaxis.
Although an effective vaccine has been available for 130 years, people continue to die of rabies.1 Although the burden of disease has decreased in many parts of the world,2–4 in other regions there has been frustratingly little progress despite the existence of proven strategies to prevent the disease.5
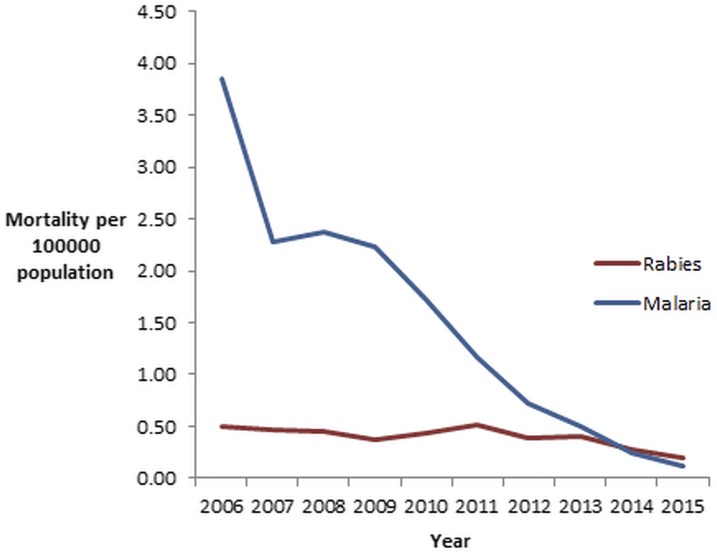
Southeast Asia continues to bear a disproportionate rabies burden and Myanmar, a country emerging from five decades of military rule, has a disease incidence that is among the highest in the world.6 Myanmar’s newly elected government and under-resourced health system face enormous challenges in improving the health of its people.7 Although the country has made impressive progress against many infectious diseases,8,9 rabies mortality remains stubbornly elevated and the disease is now responsible for more deaths in Myanmar than malaria (Figures 1 and 2, Table 1).
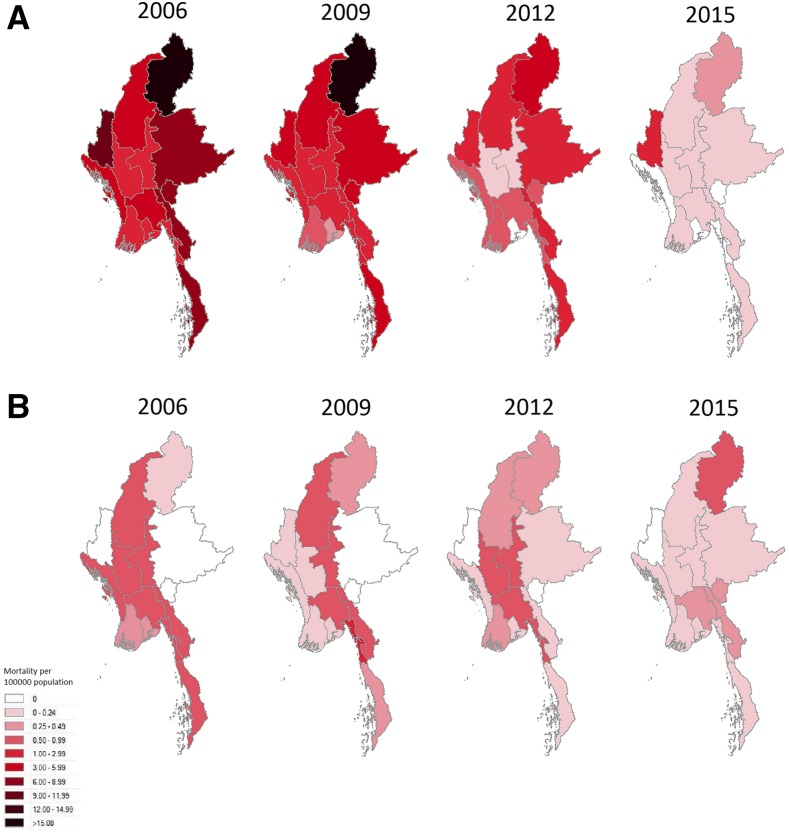
Figure 1.
Deaths from malaria (panel A) compared with deaths from rabies (panel B) in Myanmar 2006–2015 (Data from the Health Management Information System, Department of Public Health, Union of the Republic of Myanmar). This figure appears in color at www.ajtmh.org.
Figure 2.
Deaths from rabies and malaria (per 100,000 population) in Myanmar 2006–2015 (Data from the Health Management Information System, Department of Public Health, Union of the Republic of Myanmar). This figure appears in color at www.ajtmh.org.
Table 1.
Deaths from rabies and malaria (per 100,000 population) in Myanmar 2006–2015
| 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | |
|---|---|---|---|---|---|---|---|---|---|---|
| Rabies deaths | 0.50 | 0.47 | 0.45 | 0.37 | 0.43 | 0.51 | 0.39 | 0.40 | 0.28 | 0.20 |
| Malaria deaths | 3.86 | 2.27 | 2.37 | 2.24 | 1.73 | 1.17 | 0.73 | 0.50 | 0.25 | 0.12 |
Data from the Health Management Information System, Department of Public Health, Union of the Republic of Myanmar.
Indeed, these data, collected by the Health Management Information System (HMIS) section of Myanmar’s Department of Public Health, are likely to be a significant underestimate of the country’s true rabies burden.10 Only the country’s largest city, Yangon, has laboratories that are equipped to diagnose rabies and autopsies are performed very rarely; accordingly, most reported cases lack pathological confirmation and are based instead on clinical findings. Although encephalitic (“furious”) rabies has a relatively specific clinical presentation (fluctuating consciousness, hydrophobia inspiratory spasms, and signs of autonomic dysfunction), up to 20% of rabies victims present with an ascending paralysis (paralytic or “dumb” rabies). This less florid presentation can be easily misdiagnosed as Guillain–Barré syndrome, a condition that is extremely common in Myanmar.4
There are several additional reasons that these data are likely to underestimate the true incidence of rabies in the country. The disease disproportionally affects disadvantaged, rural populations; precisely the locations with the poorest diagnostic and reporting systems.4,10 Chin State, in the remote, mountainous northwest of the country is the poorest state in Myanmar with more than 80% of its population living in rural settings.11 The fact that there were no documented rabies deaths in Chin State in 7 of the 10 years of the HMIS data is more likely to reflect incomplete reporting of cases than a genuine absence of the disease. It is also important to note that these HMIS figures only include the patients presenting for medical care; in a country with a population that recognizes that there is no successful medical treatment of clinical rabies, a significant proportion of rabies victims in Myanmar dies at home rather than being admitted to a hospital.6 Finally, the fact that rabies is not a notifiable disease in Myanmar, almost certainly results in the disease being underreported.
It is illustrative to compare the changing epidemiology of malaria and rabies in Myanmar as southeast Asia has a schedule for elimination of both diseases.6,12 Myanmar’s National Malaria Control Program has been very successful and demonstrates what can be achieved in resource-limited settings with sustained political, financial, and scientific commitment.8 Even in the face of rising artemisinin-resistance in the region,13 a coordinated and collaborative approach from the national government, international donors, nongovernment organizations, and partners has resulted in a dramatic reduction in estimated malaria deaths in the country in recent years.14 Myanmar’s success in countering malaria has been facilitated by a significant and sustained increase in the funding of effective control programs.14 There has been a focus on prevention: insecticide-treated bed nets are distributed free of charge and the coverage of high-risk populations now approaches 100%.14 There have been efforts to improve early, accurate diagnosis with an increase in trained community health workers and free rapid diagnostic testing.8 Finally, there has been an emphasis on improved access to safe, affordable, and effective treatment with artemisinin-based combination therapy available free of charge to all those in the public sector.14
However, there has been less success in countering rabies in Myanmar over the same period, despite the fact that rabies is, arguably, an easier disease to control than malaria.5,13 There are several explanations for this. At a community level, there is poor understanding of how to manage dog bites, inadequate access to primary health services, and a lack of education and awareness about the use of postexposure prophylaxis.5,6,15 Within the health system, it is only relatively recently that Myanmar has been able to phase out the inferior nerve tissue vaccines and adopt intradermal rabies vaccination.6,10 Although postexposure prophylaxis is now available free of charge to all Myanmar citizens, preexposure prophylaxis is only available to select, high-risk populations and cold-chain issues limit access to rabies immunoglobulin in many locations. At a national level, there is poor access to laboratories with the capacity to diagnose human and canine rabies promptly, which makes decision-making for rational and cost-effective postexposure prophylaxis more challenging. Finally, and perhaps most crucially, there is no national program to coordinate the multisectoral, collaborative approach that is necessary to control the disease, particularly in the canine population.1
Access to the safer and more effective cell-culture vaccines is welcome, but these vaccines are expensive: in the 2016–2017 financial year $US 36 million of the country’s rabies budget has been committed to postexposure prophylaxis.16 Meanwhile, there is no specific funding for the control of canine rabies, despite the fact that it is cost-effective and that it has been shown to be feasible in even the poorest parts of the world.17,18 Although there will always be competing public health priorities, dogs are responsible for more than 99% of human rabies cases and it has been shown that control of canine rabies can be achieved with sustained vaccination coverage of 70%.4 The success of this strategy is illustrated by the successful rabies prevention and control programs in Latin America in which mass canine vaccination was one of the central components.3
There are significant challenges associated with the introduction of mass canine vaccination in Myanmar. It is a mountainous country of 678,500 km2 divided by three river systems with a dispersed, predominantly rural population consisting of more than 100 ethnicities that speak a variety of languages. However, establishing a national rabies program that encourages better communication and greater collaboration between departments responsible for human and animal health would be an important first step. Mass canine vaccination would be expensive but could be justified on a health economic basis through future savings from reduced human postexposure prophylaxis and hospital care.4 If rabies control programs can be integrated with existing effective public health programs this may also defray costs.8,19
It should be noted that Myanmar’s situation is not unique and in almost all the countries where rabies remains prevalent, the issues are similar.1,4 In nearby Cambodia, there is also no national rabies program or coordinated canine vaccination campaign. Human and canine disease surveillance is suboptimal there is similarly poor access to postexposure prophylaxis and laboratory diagnostics services.20 Just as in Myanmar, in Cambodia rabies is estimated to cause more deaths than malaria, despite the appropriate concern about evolving artemisinin resistance in Plasmodium falciparum.13,20
We have all the necessary tools to control rabies.1,5 Myanmar has its unique social, political, and economic challenges to overcome, but the success of the country’s malaria program shows what can be achieved with appropriate funding and integration of effective disease prevention strategies. Many of the concepts that underpin malaria and rabies control are similar and include an emphasis on prevention, improved access to primary health care, and the facilitation of early, accurate diagnosis which permits prompt, effective therapy. Although there are additional challenges in coordinating public health programs that target animal and human health concurrently, the success of Myanmar’s National Malaria Control shows and the elimination of rabies in other resource-poor countries show what can be achieved with sustained political, financial, and scientific commitment. There should be no reason that these principles cannot also be applied successfully to eliminate rabies in Myanmar.
REFERENCES
- 1.Fooks AR, Banyard AC, Horton DL, Johnson N, McElhinney LM, Jackson AC, 2014. Current status of rabies and prospects for elimination. Lancet 384: 1389–1399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Murray CJ. et al. , 2012. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 380: 2197–2223. [DOI] [PubMed] [Google Scholar]
- 3.Belotto A, Leanes LF, Schneider MC, Tamayo H, Correa E, 2005. Overview of rabies in the Americas. Virus Res 111: 5–12. [DOI] [PubMed] [Google Scholar]
- 4.World Health Organization, 2013. WHO Expert Consultation on Rabies: Second Report. Geneva, Switzerland: World Health Organization. [PubMed] [Google Scholar]
- 5.Zinsstag J, 2013. Towards a science of rabies elimination. Infect Dis Poverty 2: 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.World Health Organization; Regional Office for Southeast Asia,2012. Strategic Framework for Elimination of Human Rabies Transmitted by Dogs in the South-East Asia Region. New Delhi, India: World Health Organization, Regional Office for Southeast Asia. [Google Scholar]
- 7.Saw YM, Win KL, Shiao LW, Thandar MM, Amiya RM, Shibanuma A, Tun S, Jimba M, 2013. Taking stock of Myanmar’s progress toward the health-related millennium development goals: current roadblocks, paths ahead. Int J Equity Health 12: 78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mu TT, Sein AA, Kyi TT, Min M, Aung NM, Anstey NM, Kyaw MP, Soe C, Kyi MM, Hanson J, 2016. Malaria incidence in Myanmar 2005–2014: steady but fragile progress towards elimination. Malar J 15: 503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.World Health Organization, 2015. Myanmar: WHO Statistical Profile Available at: http://www.who.int/gho/countries/mmr.pdf. Accessed February 22, 2017.
- 10.Kyi TT, 2014. Rabies control, elimination and vaccination. Myanmar Medical Journal 56: 44–49. [Google Scholar]
- 11.UNICEF, 2015. Chin State Profile Available at: http://www.unicef.org/myanmar/Chin_State_Profile_30-07-15.pdf. Accessed 1 July, 2016.
- 12.World Health Organization, 2015. Strategy for Malaria Elimination in the Greater Mekong Subregion (2015–2030). Manila, Philippines: World Health Organization Regional Office for the Western Pacific. [Google Scholar]
- 13.Imwong M, et al. , 2017. The spread of artemisinin-resistant Plasmodium falciparum in the Greater Mekong Subregion: a molecular epidemiology observational study. Lancet Infect Dis 17: 491–497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.World Health Organization,2016. World Malaria Report. Geneva, Switzerland: WHO. [Google Scholar]
- 15.Gongal G, Wright AE, 2011. Human rabies in the WHO southeast Asia Region: forward steps for elimination. Adv Prev Med 2011: 383870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.2017. Department of Public Health, Ministry of Health and Sport, Republic of the Union of Myanmar.
- 17.Fitzpatrick MC, Hampson K, Cleaveland S, Mzimbiri I, Lankester F, Lembo T, Meyers LA, Paltiel AD, Galvani AP, 2014. Cost-effectiveness of canine vaccination to prevent human rabies in rural Tanzania. Ann Intern Med 160: 91–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lembo T, Hampson K, Kaare MT, Ernest E, Knobel D, Kazwala RR, Haydon DT, Cleaveland S, 2010. The feasibility of canine rabies elimination in Africa: dispelling doubts with data. PLoS Negl Trop Dis 4: e626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tulenko K, Mogedal S, Afzal MM, Frymus D, Oshin A, Pate M, Quain E, Pinel A, Wynd S, Zodpey S, 2013. Community health workers for universal health-care coverage: from fragmentation to synergy. Bull World Health Organ 91: 847–852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ly S, Buchy P, Heng NY, Ong S, Chhor N, Bourhy H, Vong S, 2009. Rabies situation in Cambodia. PLoS Negl Trop Dis 3: e511. [DOI] [PMC free article] [PubMed] [Google Scholar]