Abstract
Objectives. To examine the association between Colorado’s legalization of recreational cannabis use and opioid-related deaths.
Methods. We used an interrupted time-series design (2000–2015) to compare changes in level and slope of monthly opioid-related deaths before and after Colorado stores began selling recreational cannabis. We also describe the percent change in opioid-related deaths by comparing the unadjusted model-smoothed number of deaths at the end of follow-up with the number of deaths just prior to legalization.
Results. Colorado’s legalization of recreational cannabis sales and use resulted in a 0.7 deaths per month (b = −0.68; 95% confidence interval = −1.34, −0.03) reduction in opioid-related deaths. This reduction represents a reversal of the upward trend in opioid-related deaths in Colorado.
Conclusions. Legalization of cannabis in Colorado was associated with short-term reductions in opioid-related deaths. As additional data become available, research should replicate these analyses in other states with legal recreational cannabis.
As more states loosen regulations on medical and recreational cannabis use, cannabis remains illegal under US federal law. Research into the health effects of recent state cannabis policies has found mixed results. Anderson et al.1 noted a reduction in fatal automobile crashes in states that legalized medical cannabis, whereas Hall and Lynskey2 found an increase in the proportion of fatal crashes involving cannabis. Recreational legalization in Colorado has led to increases in cannabis-related emergency department visits for both adults and children.3 States and the US federal government continue to consider modifying cannabis policies, and more research is warranted to assess health effects of these policies across a diverse set of outcomes.
One topic of current research is whether cannabis is substituted for opioids in pain management.4 With this substitution, an immediate reduction in opioid-related poisonings would be expected. Bachhuber et al.5 assessed the effect of medical marijuana laws on reducing opioid-related deaths, reporting a 25% decrease in opioid overdose mortality in states with medical marijuana laws compared with states without such laws.
Death rates from opioid poisoning continue a disturbing upward trend in the United States and now constitute the leading cause of injury-related death. In 2014, 61% of all drug poisoning deaths involved an opioid, representing nearly 30 000 deaths.6 Experts have proposed the need for a multifaceted approach, including collaborative efforts by public health and law enforcement, and a diverse set of regulatory policies to address this epidemic.
Researchers continue studying the public health implications of medical marijuana laws, but less is known about the effects of recreational cannabis legalization, particularly whether it reduces or exacerbates the current opioid epidemic. We investigated changes in opioid-related deaths in a state that substantially increased cannabis availability by legalizing sales of cannabis for recreational use.
METHODS
We used an interrupted time-series design to evaluate the effect of Colorado’s recreational cannabis legalization on opioid-related deaths. We analyzed monthly counts of opioid deaths from January 2000 through December 2015, covering 168 baseline months and the first 24 months after legalization. Most confounders change slowly over time and are accounted for by having a long baseline time series. To further strengthen the design, we included opioid-related deaths in 2 regionally similar states as covariates. We selected Nevada to allow for comparison with a state that permits the sale of only medical cannabis, helping to isolate the effect of Colorado’s recreational legalization from medical legalization. Nevada is a particularly suitable comparison because its legalization of medical cannabis occurred within months of medical legalization in Colorado. A second comparison state, Utah, was incorporated into the design for comparison between Colorado and a state where cannabis use remains illegal in state law.
An important threat to interrupted time-series designs are confounders that change at the same time as the policy under study. In our case, an important concern was that Colorado changed their prescription drug monitoring program in May 2014, 5 months after recreational cannabis legalization. Although the prescription drug monitoring program was established in 2007, the 2014 change required that all opioid prescribers and pharmacists register with, but not necessarily use, the prescription drug monitoring program by the end of 2014. Research indicates that prescription drug monitoring programs can abruptly affect opioid-related deaths.7 Thus, changes to Colorado’s prescription drug monitoring program could have confounded associations with recreational cannabis legalization. Because of variation in state prescription drug monitoring programs, no comparable state exists with respect to Colorado’s prescription drug monitoring program change. Therefore, we relied on statistical controls for the potential prescription drug monitoring program effect.
Data
We examined monthly opioid-related deaths from 2000 to 2015 with the Multiple Cause of Death files available through the Centers for Disease Control and Prevention WONDER (Wide-Ranging Online Data for Epidemiologic Research) system. Opioid-related deaths were defined as any deaths with an International Classification of Diseases, 10th Revision, code indicating opioid poisoning (both pharmaceutical and nonpharmaceutical).8
We calculated policy variables based on the date retail stores began selling recreational cannabis directly to consumers (January 1, 2014).
Statistical Analysis
To estimate the effect of recreational cannabis legalization on monthly opioid-related deaths in Colorado, we analyzed 3 separate segmented regressions:
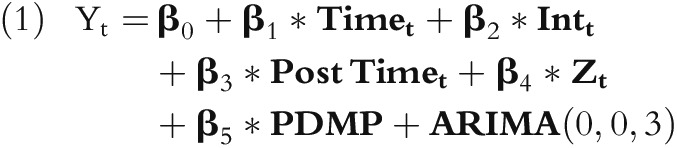 |
where Yt is the number of opioid-related deaths, β0 is the intercept, β1 is the prelegalization trend, β2 is an abrupt change in level postlegalization, Intt is the dummy variable estimating an immediate level change postlegalization, β3 is the change in trend starting at the time of legalization, β4 is the association between Colorado’s opioid-related deaths and those of the comparison state in each model, Zt is the number of opioid-related deaths in the comparison state each month, β5 is the change in level resulting from the May 2014 change in Colorado’s prescription drug monitoring program (PDMP), and ARIMA is autoregressive integrated moving average.9 This model assumes an immediate effect of legalization allowing for an immediate change in either the mean or the slope postlegalization. Following inspection of the autocorrelation and partial autocorrelation functions, we included an MA(3) parameter to achieve white-noise residuals.10
We describe the total effect of cannabis legalization as the percent change at the end of the follow-up period (December 2015). To be conservative, we estimated the percent change by comparing the model-smoothed number of deaths at the end of follow-up relative to the number of deaths just prior to legalization.
RESULTS
Analyses showed a statistically significant reduction in trend in opioid-related deaths following recreational cannabis legalization in Colorado. When we controlled for comparison state trends and Colorado’s PDMP, opioid-related deaths decreased by approximately 0.7 deaths per month relative to the baseline period (b = −0.68; 95% confidence interval = −1.34, −0.03) (Table A, available as a supplement to the online version of this article at http://www.ajph.org). Comparing the model-smoothed opioid-related deaths per month just prior to legalization with the modeled number at the end of follow-up resulted in an estimated 6.5% reduction in opioid-related deaths.
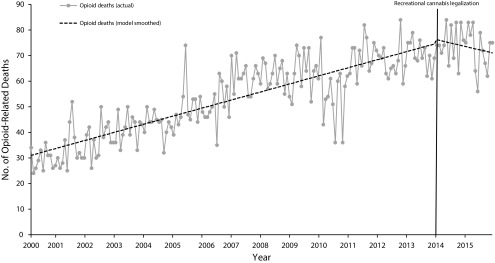
These results were robust to controlling for trends in opioid-related deaths in the 2 comparison states and Colorado’s strengthening of their PDMP by implementing mandatory registration (Figure 1). Results also did not change in any substantive way with Poisson rather than ARIMA models.
FIGURE 1—
Changes in Monthly Opioid-Related Deaths Following Recreational Cannabis Legalization in Colorado, 2000–2015
Note. Change in opioid-related deaths per month following legalization = −0.68 (95% confidence interval = −1.34, −0.03; P = .043). Change in model-estimated opioid-related deaths was robust to covariate control of opioid-related deaths in all comparison states. Change in model-estimated opioid-related deaths was robust to whether the prescription drug monitoring program (PDMP) covariate was modeled at the beginning of implementation or at full implementation of the 2014 PDMP change.
DISCUSSION
After Colorado’s legalization of recreational cannabis sale and use, opioid-related deaths decreased more than 6% in the following 2 years. These findings extend Bachhuber et al.’s5 results on the potential protective effect of medical cannabis legalization on opioid-related deaths. Available data provide only an assessment of the short-term effects of Colorado’s recreational cannabis legalization. However, these initial results clearly show that continuing research is warranted as data become available, involving longer follow-ups and additional states that have legalized recreational cannabis.
Without being able to randomize recreational cannabis legalization to states, an interrupted time-series design offers the strongest quasi-experimental design for assessing effects. To nullify our results, remaining confounders would need to occur near the time of legalization in Colorado and differentially affect Colorado more than the comparison states. A potential confounder was Colorado’s prescription drug monitoring program registration mandate in 2014. We addressed this by modeling the effect of both policies simultaneously. Part of the effect attributed here to a change in cannabis policy could be a result of changes in Colorado’s prescription drug monitoring program. As additional data become available, research should replicate these analyses in other states with legal recreational cannabis.
PUBLIC HEALTH IMPLICATIONS
As of 2016, 8 states and Washington, DC, have legalized recreational cannabis. Given the rapidly changing landscape of cannabis and opioid policy in the United States, the need for evidence of the diverse health effects of these laws is increasing. Although we found an apparent public health benefit in a reduction in opioid-related deaths following recreational cannabis legalization in Colorado, we note that expanded legalized cannabis use is also associated with significant potential harms. For policymakers to balance the potential beneficial and deleterious effects of these laws, researchers must continue to examine the full range of health effects in both clinic- and population-level research.
HUMAN PARTICIPANT PROTECTION
The institutional review board at the University of North Texas Health Science Center approved this study.
REFERENCES
- 1.Anderson DM, Hansen B, Rees DI. Medical marijuana laws, traffic fatalities, and alcohol consumption. J Law Econ. 2013;56(2):333–369. [Google Scholar]
- 2.Hall W, Lynskey M. Evaluating the public health impacts of legalizing recreational cannabis use in the United States. Addiction. 2016;111(10):1764–1773. doi: 10.1111/add.13428. [DOI] [PubMed] [Google Scholar]
- 3.Kim HS, Monte AA. Colorado cannabis legalization and its effect on emergency care. Ann Emerg Med. 2016;68(1):71–75. doi: 10.1016/j.annemergmed.2016.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hayes MJ, Brown MS. Legalization of medical marijuana and incidence of opioid mortality. JAMA Intern Med. 2014;174(10):1673–1674. doi: 10.1001/jamainternmed.2014.2716. [DOI] [PubMed] [Google Scholar]
- 5.Bachhuber MA, Saloner B, Cunningham CO, Barry CL. Medical cannabis laws and opioid analgesic overdose mortality in the United States, 1999-2010. JAMA Intern Med. 2014;174(10):1668–1673. doi: 10.1001/jamainternmed.2014.4005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rudd RA, Seth P, David F, Scholl L. Increases in drug and opioid-involved overdose deaths—United States, 2010–2015. MMWR Morb Mortal Wkly Rep. 2016;65(5051):1445–1452. doi: 10.15585/mmwr.mm655051e1. [DOI] [PubMed] [Google Scholar]
- 7.Delcher C, Wagenaar AC, Goldberger BA, Cook RL, Maldonado-Molina MM. Abrupt decline in oxycodone-caused mortality after implementation of Florida’s Prescription Drug Monitoring Program. Drug Alcohol Depend. 2015;150:63–68. doi: 10.1016/j.drugalcdep.2015.02.010. [DOI] [PubMed] [Google Scholar]
- 8. Prescription Drug Overdose Team, Health Systems and Trauma Systems Branch, Division of Unintentional Injury Prevention, National Center for Injury Prevention and Control, Centers for Disease Control and Prevention. Prescription Drug Overdose Data & Statistics: Guide to ICD-9-CM and ICD-10 Codes Related to Poisoning and Pain, Version 1.3. Revised August 12, 2013. Available at: https://www.cdc.gov/drugoverdose/pdf/pdo_guide_to_icd-9-cm_and_icd-10_codes-a.pdf. Accessed February 24, 2017.
- 9.Wagner AK, Soumerai SB, Zhang F, Ross-Degnan D. Segmented regression analysis of interrupted time series studies in medication use research. J Clin Pharm Ther. 2002;27(4):299–309. doi: 10.1046/j.1365-2710.2002.00430.x. [DOI] [PubMed] [Google Scholar]
- 10.Biglan A, Ary D, Wagenaar AC. The value of interrupted time-series experiments for community intervention research. Prev Sci. 2000;1(1):31–49. doi: 10.1023/a:1010024016308. [DOI] [PMC free article] [PubMed] [Google Scholar]