What really ails the US health care system? My answer is documented in the compelling 2017 book by Elizabeth Rosenthal called An American Sickness: How Healthcare Became Big Business and How You Can Take It Back,1 which was reviewed in AJPH by Fox and Grogan.2 Here is her thesis:
In the past quarter century, the American medical system has stopped focusing on health or even science. Instead it attends more or less single-mindedly to its own profits.1
In short, her answer is a five-letter word, g-r-e-e-d.
Rosenthal, a medical doctor and now editor of the Kaiser Health News, pulls no punches and lets no one off the hook, including health insurers, hospitals, physicians, drug and medical device makers, ancillary service providers, home health companies, contractors, researchers, philanthropists, and more:
These days our treatment follows not scientific guidelines, but the logic of commerce in an imperfect and poorly regulated market, whose big players spend more on lobbying than defense contractors. Financial incentives to order more and do more—to default to the most expensive treatment for whatever ails you— drive much of our healthcare.1
When and how did we get to this place, and is there any way out?
US MEDICAL CARE AS A BUSINESS
From its humble beginnings, US medical care has always been a business, initially owned by solo and small entrepreneurs. The emergence of private health insurance in the 1930s and 1940s for the first time put medical care on a financially sustainable—and inflationary—footing. The 1966 launch of Medicare and Medicaid, with the former’s inflationary and provider-set reimbursement formula, put payment on jet skis and established health care as a profit center.
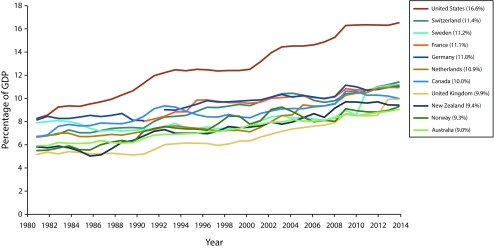
These developments set the stage for the transformations of the 1970s and 1980s. Figure 1 shows health care spending as a percentage of gross domestic product in 10 advanced nations over 33 years. In 1980, US health spending was among the highest, and part of the pack. In the early 1980s, for the first time, US health spending jumped ahead of the pack, and the gap has ballooned ever since, leveling off in the 1990s and the early 2010s. What happened in the 1980s?
FIGURE 1—
Health Care Spending as Percentage of Gross Domestic Product
Source. Adapted from Schneider et al.3
Arnold Relman, late editor of the New England Journal of Medicine, described what happened in a 1980 article, “The New Medical Industrial Complex,” documenting “a vast array of investor-owned businesses supplying health services for profit—services heretofore provided by nonprofit institutions or individual practitioners” including hospitals, nursing homes, home care, laboratory and other services, hemodialysis, and more.4 In 1979 alone, net earnings of health companies with public stock shares rose by 30% to 35%, with more banner years ahead, Relman reported.
In Paul Starr’s 1982 Pulitzer Prize–winning book, The Social Transformation of American Medicine, he presciently titled his final chapter “The Coming of the Corporation,” predicting that “the last decades of the 20th century are likely to be a time of . . . the rise of corporate enterprise in health services, which is already having a profound impact on the ethos and politics of medical care as well as its institutions.”5(p420–421)
Relman and Starr foresaw that the investor-owned health sector would grow. Between 1989 and 2017, while the overall Standard and Poor’s (S&P) 500 Index grew 696%, from 348 to 2419, the S&P 500 Health Index of stocks increased by 1389%, from 66 to 921, twice the rate of the overall index (data obtained from Compustat; Health Index is unavailable before 1989). The transformation can be seen within health industry sectors. Between the mid-1980s and the late 2000s, for-profit ownership of dialysis centers rose from 42% to 78%, rehab hospitals from 15% to 61%, in-home health from 36% to 68%, and hospices from 13% to 53%. Not all sectors saw such growth—for example, for-profit ownership of nursing homes dropped from 75% to 68%—though the growth in homes claimed by investor-owned corporations since the 1970s has been explosive.6
Although for-profit ownership growth of acute care hospitals was not as dramatic, most for-profit hospitals are now part of investor-owned national chains. As Gray and Schlesinger note in The State of Nonprofit America,
The stock price of publicly traded companies is a function of both the company’s earnings and investors’ expectations of future earnings. Since a company’s access to capital and the wealth of its executives are a function of stock price, investor-owned corporations have strong incentives to grow. The most rapid path is via acquisitions, and many of the publicly traded health care companies have gone through periods of omnivorous growth, fed by high stock prices, which in turn were fed by the expectations and fact of further growth.6
Gray and Schlesinger observe that the for-profit sector’s impact extends beyond its walls:
Even where nonprofits have maintained their role in health care, they have often responded to the challenges confronting them by becoming institutionally more like commercial enterprises. . . . Today’s nonprofit health care providers engage in advertising, marketing, and other business practices that have long typified for-profit companies. . . .6
These include nonprofit boards resembling their for-profit peers, for-profit subsidiaries for new service areas, joint ventures with proprietary physician groups or specialized for-profit companies, and more.
These changes did not occur in a vacuum. The 1980s was our first deregulation decade, characterized by President Ronald Reagan in his first inaugural address: “In the present crisis, government is not the solution to our problem, government is the problem.” Equally memorable were the words “greed is good” from Gordon Gekko in the 1987 movie, Wall Street.
Today, health stocks are the second-highest category of both revenue and profits on the S&P 500 index. Within the health category, pharmaceuticals, biotechnology, and health care equipment made up 29.5% of revenue and 75.2% of profits in 2016.
HELPFUL SUGGESTIONS
What can be done? Rosenthal’s book offers a cornucopia of helpful suggestions for consumers and policymakers from modest caveat emptor warnings to consumers all the way to a single-payer takeover and much in between. She addresses dealing with physician, hospital, and ancillary service bills, as well as insurers and drug or device makers. Earlier this year, Gaynor et al. at Brookings offered a set of smart recommendations to address growing concentration and lack of competition across health care markets.7
Still, sometimes it feels as though the horse has been out the barn so long that getting it back is a fool’s errand. The first step is to diagnose correctly what ails our system. I think we know what that is. At its core, our health care system and its soul have been bought and sold so many times over, it is hard to know what is left. Only the people can reclaim it.
REFERENCES
- 1.Rosenthal E. An American Sickness: How Healthcare Became Big Business and How You Can Take It Back. New York, NY: Penguin Press; 2017. [Google Scholar]
- 2.Fox DM, Grogan CM. A platform to launch a collective discussion about reforming US health politics and policy. Am J Public Health. 2017;107(8):1200–1202. doi: 10.2105/AJPH.2017.303909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schneider EC, Sarnak DO, Squires D, Shah A, Doty MM. Mirror, mirror: how the US health care system compares internationally at a time of radical change. The Commonwealth Fund. Available at: http://www.commonwealthfund.org/~/media/files/publications/fund-report/2017/jul/schneider_mirror_mirror_2017.pdf. Accessed September 19, 2017.
- 4.Relman AS. The new medical industrial complex. N Engl J Med. 1980;303(17):963–970. doi: 10.1056/NEJM198010233031703. [DOI] [PubMed] [Google Scholar]
- 5.Starr P. The Social Transformation of American Medicine. 2nd ed. New York, NY: Basic Books; 2017. [Google Scholar]
- 6.Gray B, Schlesinger M Health care. In: The State of Nonprofit America. 2nd ed. Salaman L, editor. Washington, DC: Brookings Institution Press; 2012. [Google Scholar]
- 7.Gaynor M, Mostashari F, Ginsburg PB. Making health care markets work: competition policy for health care. Brookings Institute. 2017. Available at: https://www.brookings.edu/research/making-health-care-markets-work-competition-policy-for-health-care. Accessed September 13, 2017. [DOI] [PubMed]