Summary
Background
Psoriasis is an inflammatory long‐term condition involving comorbidities, unhealthy lifestyle and significant life impact. Patients’ understanding of psoriasis is limited and support lacking. The Common‐Sense Model of Self‐Regulation of Health and Illness emphasizes the role of illness and treatment beliefs on coping and self‐management. New ‘Pso Well®’ patient materials informed by the model, addressed psoriasis as a long‐term condition, medication management and lifestyle behaviours.
Objectives
To investigate whether Pso Well® materials (i) broaden understanding of psoriasis without increasing anxiety; (ii) are acceptable; and (iii) comprise features that appear to effect change.
Methods
The Revised Illness Perceptions Questionnaire (IPQ‐R modified) and the Hospital Anxiety and Depression Scale (HADS) were administered in patients before and after intervention. Numerical rating scales assessed perceptions of change in understanding and anxiety resulting from engagement with the materials. Qualitative interviews explored acceptability and perceived ‘active ingredients’.
Results
Fifty‐five patients completed pre‐ and postintervention questionnaires (56% female; median age 59 years). Postintervention, a large effect size was indicated in two IPQ‐R domains – illness coherence [t(55) = −3·48, P = 0·001 (two‐tailed), η2 = 0·19] and personal control [t(55) = −2·98, P = 0·004 (two‐tailed), η2 = 0·14] – and a medium effect in one, treatment control [t(55) = −2·08, P = 0·042 (two‐tailed), η2 = 0·08]. HADS scores did not change. For numerical rating scales, 80% of participants reported increased understanding of psoriasis and none reported increased anxiety. Interviews with 19 patients indicated the materials were acceptable and usable. Factors reported to broaden understanding and promote engagement with self‐management included linking of related disease aspects, personally relevant content and high‐quality design.
Conclusions
High‐quality, theory‐based psoriasis materials are acceptable to patients and can improve understanding and sense of control without increasing anxiety.
Short abstract
What's already known about this topic?
Psoriasis is associated with comorbidities, unhealthy lifestyle and significant life impact.
Patients’ understanding of psoriasis is limited, self‐management support is lacking and disengagement from healthcare services is common.
What does this study add?
The new, theory‐informed Pso Well® patient materials address psoriasis as a long‐term condition; medications management and lifestyle behaviour.
The Pso Well® patient materials can increase understanding of psoriasis, promote feelings of self‐worth and encourage a desire to engage in self‐management and behaviour change, without increasing anxiety or depression.
What are the clinical implications of this work?
The Pso Well® patient materials could support clinical consultations by helping patients recognize the remitting–relapsing nature of psoriasis.
This will help to improve understanding of the disease, as well as providing a clearer rationale for treatment adherence and lifestyle behaviour change.
Linked Comment: Prinsen. Br J Dermatol 2017; 177:616–617
Psoriasis is a complex, long‐term inflammatory skin condition affecting at least 2% of the U.K. population.1 It is associated with high levels of physical and psychological disability,2, 3, 4, 5 comorbidities6, 7, 8, 9, 10 and significant life impact.11, 12 While individuals with psoriasis have additional risk factors for13 and higher mortality from14 cardiovascular disease, recent evidence suggests that psoriasis in the absence of inflammatory arthritis is not an independent risk factor.13
Unhealthy lifestyle behaviours15, 16, 17, 18, 19, 20 and obesity21 are more common in individuals with psoriasis, complicating understanding of comorbidities13, 18 and contributing to risks of psoriasis onset and/or exacerbation,16, 22, 23, 24, 25, 26, 27 although patients and nonspecialist clinicians may be unaware of these associations. Improving lifestyles may improve outcomes;27, 28, 29, 30, 31 however, complex interactions between physiological and behavioural processes can be compounded by high levels of associated psychological distress. Distress can increase risk behaviour (e.g. smoking) and reduce motivation and capacity to engage in healthy behaviours.32
Dissatisfaction with psoriasis management,33, 34 problematic medication adherence35 and disengagement from health services are common among patients.34, 36 Clinicians express low confidence in managing psoriasis comorbidities, including supporting healthy lifestyle.37, 38, 39, 40 Patients’ understanding of psoriasis is limited,41 and patient information rarely addresses comorbidity risk or rationale for lifestyle modification. There is little evidence to support the effectiveness of generic education‐based interventions in psoriasis for patient self‐management.42, 43 While tailored, disease‐specific programmes appear to be more promising,44, 45 these interventions may be labour intensive and relatively costly, and do not explicitly recognize the central importance of patient understanding in self‐management. Informing patients of additional possible health risks could further increase anxiety. Lack of ‘illness coherence’, or the mismatch between understanding underlying disease mechanisms and corresponding self‐care activities, is a barrier to action, reducing perceived personal control of psoriasis with consequent suboptimal outcomes.34
The Common‐Sense Model of Self‐Regulation of Health and Illness (CS‐SRM)46 provides an explanation as to how an individual's beliefs about their condition and its treatment influence their emotional and behavioural responses,47 including self‐care behaviours. The five key beliefs highlighted in the model relate to symptoms attributed to the condition, its cause, chronicity, levels of perceived controllability or curability, and its perceived consequences.48 In 2002, the concept of ‘illness coherence’ was added to the CS‐SRM to describe an individual's ability to hold a congruent working model of their symptoms.49 Patients’ beliefs have been shown to predict health outcomes and are amenable to change in a range of long‐term conditions including psoriasis.50 Thus, changing patients’ understanding of psoriasis and the relevance of health behaviours may help increase motivation to engage in appropriate self‐management. However, exposing patients to a revised picture of psoriasis as an incurable condition associated with comorbidities risks creating or compounding distress.
Guided by the Medical Research Council framework for complex healthcare interventions51, 52 and evidence from the Identification and Management of Psoriasis‐Associated Co‐morbidiTy (IMPACT) programme,53 we developed and tested new ‘Pso Well®’ patient‐focused materials to: (i) improve illness coherence (i.e. broaden patient understanding of psoriasis as a systemic long‐term condition without increasing anxiety); (ii) improve understanding of treatments by linking disease mechanisms with effective self‐care options, including behavioural change; and (iii) identify aspects of the intervention that patients perceive as motivating them to change (i.e. mechanisms of action).
Materials and methods
Study design
This was a within‐group, before‐and‐after feasibility and acceptability study to develop, test and evaluate new patient materials for psoriasis, described using TIDieR guidance.54
Materials development, design and content
Guiding principles informed the materials’ presentation and communication style (Table 1).55, 56, 57, 58 Materials were designed iteratively, by mapping key concepts against the CS‐SRM domains (to increase understanding by relating information to patients’ own personal experience of psoriasis rather than simply increasing knowledge about the disease), and refining content and style in consultation with the IMPACT Patient User Group, specialist clinicians and graphic designers (Table S1; see Supporting Information).
Table 1.
Guiding principles for Pso Well® patient materials development
| Principles | Techniques | Aim |
|---|---|---|
| Broadening understanding (beliefs) about psoriasis and treatment options |
Clearly written, accurate information directly addressing key beliefs in CS‐SRM Use of analogies and metaphors to communicate complex disease and treatment mechanisms Directly addressing common emotional responses to psoriasis |
Improve illness coherence Improve understanding of relapsing–remitting nature of psoriasis Improve understanding of links between treatment options and underlying disease processes |
| Recommendations for writing effective health communication |
Textual and graphical coherence Attention to readability and usability Chunking information into ‘bite‐size’ sections Pilot testing with target audience |
Promote optimum information processing |
| Content of personal relevance to people with psoriasis |
Inclusion of issues and experiences grounded in in‐depth qualitative research with patients and clinicians managing psoriasis Advice and suggestions from current best evidence‐based self‐management approaches |
Promote understanding of comorbidities Provide rationale for personally relevant lifestyle behaviour change and medication adherence |
| Positive messages |
Use of self‐affirmation to build confidence and motivation Hopeful tone Modelling functional coping |
Counteract possible increase in anxiety resulting from new understanding of psoriasis as a lifelong, incurable inflammatory condition |
CS‐SRM, Common‐Sense Model of Self‐Regulation of Health and Illness.
The collaborative design and refinement process resulted in 15 paper‐based leaflets (see Figure 1 for design and Table 2 for content).
Figure 1.

Pso Well® patient materials design.
Table 2.
Content of Pso Well® patient materials
| Leaflet set | Leaflet title | Content |
|---|---|---|
| Introductory (two leaflets) | Psoriasis: new for you | Signposting for patients with a new diagnosis of psoriasis |
| Knowing your psoriasis | Signposting for patients with a long‐standing diagnosis of psoriasis | |
| Understanding psoriasis as a complex long‐term condition (three leaflets) | Changing phases | What is psoriasis? |
| Linking mind and body | Associated comorbidities | |
| Your journey with psoriasis | Cardiovascular risk and mood factors | |
| Medications management (six leaflets) | Treatment overview | Explanation of first‐, second‐ and third‐line treatments for psoriasis and relevance for stages of disease |
| Topical treatments | ||
| Emollients | ||
| Steroid‐based topicals | ||
| Light therapy | ||
| Systemics and biologics | Practical tips for treatment use. Reflective activities to enhance adherence | |
| Lifestyle management (four leaflets) | Why does my weight matter? | Weight/nutrition |
| Keeping active feeling good | Physical activity | |
| Smokeless | Smoking | |
| Is your glass half full? | Alcohol |
Materials testing
Sampling and recruitment
A community‐based sample of primary‐care patients from a previous study59 was invited to participate (University of Manchester ethics reference 14269).
Study procedure and outcome measures
Informed written consent was obtained by post. Data collected at baseline via postal questionnaire prior to intervention included the following. Firstly, three domains of the Revised Illness Perceptions Questionnaire (IPQ‐R).49 Both the revised and earlier versions of this instrument have been widely used in the psoriasis population50, 60, 61, 62, 63, 64, 65, 66, 67 and have good evidence for reliability and validity.49 The illness coherence domain score was the primary outcome. Secondary outcome measures were the personal control and the treatment control domains. Illness coherence scores and treatment control scores are each calculated by summing the scores of five items, each with a possible score of 1–5 (range 5–25). The personal control score is similarly calculated; however, this domain contains six items (range 6–30).
Secondly, two further items, which were administered to assess other aspects of illness coherence specific to psoriasis. Data from these items were analysed separately from the original IPQ‐R illness coherence domain. They were: (i) ‘I have a clear picture or understanding of other conditions that are associated with psoriasis (sometimes called comorbidities)’ and (ii) ‘Having a healthy lifestyle can improve my psoriasis or psoriasis flares’.
Thirdly, the Hospital Anxiety and Depression Scale (HADS), which was used to assess anxiety and depression.68 This is a widely used tool that has been used extensively in patients with psoriasis and shown to have good reliability and validity in these populations.69, 70, 71 It comprises seven items assessing anxiety symptoms and seven assessing depression symptoms. Anxiety and depression scores are produced by summing the scores from a four‐point Likert scale (0–3) with a maximum possible value of 21 for each; scores under seven indicate no or normal levels of anxiety or depression.
Fourthly, the Simplified Psoriasis Index, administered to assess current psoriasis severity, historical course of the condition and perceived psychological and social impact.72 Baseline Simplified Psoriasis Index scores were used to characterize the sample of participants.
Participants were given 2 weeks to read and reflect upon the materials and were invited to identify information that was new or made them think differently about psoriasis or its management. Views were recorded on a ‘relevance’ chart according to two categories: ‘highly relevant now’ and ‘relevant in the past’. Once completed and returned, postintervention assessments were collected by post. These included the three domains of the IPQ‐R as above; the two additional illness coherence questions; HADS; and two simple numerical rating scales (NRS) to enable participants to indicate changes (positive, negative or none) in (i) understanding and (ii) anxiety, which the participants attributed as resulting directly from interacting with the materials. Figure 2 shows the study process flowchart.
Figure 2.
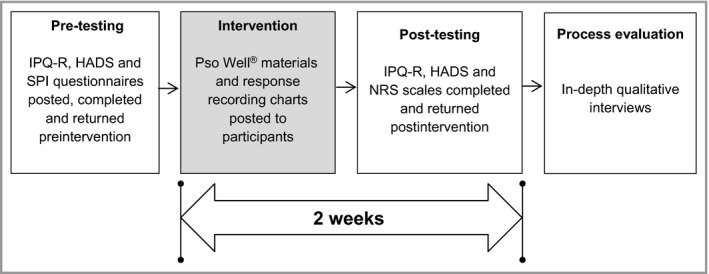
Pso Well® patient materials study process flowchart. IPQ‐R, Revised Illness Perceptions Questionnaire; HADS, Hospital Anxiety and Depression Scale; SPI, Simplified Psoriasis Index; NRS, numerical rating scale.
Process evaluation
A subset of participants purposively sampled for age, sex, psoriasis severity and responses to the outcome measures was invited to participate in follow‐up interviews based on a flexible topic guide (Table S2; see Supporting Information). This was to evaluate the usability and acceptability of the materials and to identify any perceived influences on understanding psoriasis (i.e. ‘active ingredients’).
Data analyses
Paired‐sample t‐tests assessed change in illness perceptions and anxiety and depression scores before and after intervention. All quantitative analyses used SPSS version 22 (IBM, Armonk, NY, U.S.A.).
Qualitative data collection and analysis were carried out concurrently.73 Data were managed in NVivo 10 (QSR International, Doncaster, Australia) and explored iteratively for similarities and differences within and across interviews using principles of framework analysis.74 Data were labelled in a series of coding steps. The first author (P.A.N.) led and coordinated the coding process to generate a draft conceptual framework (key themes). A series of analysis meetings between authors P.A.N., K.K. and L.C. took place regularly during coding. Data were considered from the perspectives of dermatology, health psychology and health service research, to identify whether and how exposure to the materials had prompted any change in participants’ understanding or coherence in relation to psoriasis. The second author (K.K.) applied the draft conceptual framework to a subset of data, and the final list of key themes was agreed. Data collection was concluded when key themes were fully developed.73
Results
Participants
Of the 127 invited, 58 participants completed the ‘relevance’ chart and 55 completed the pre‐ and postintervention questionnaires. Of the 24 invited for interview, 19 accepted. The sampling frame for the interviews was the total number of participants (n = 55) who completed the postintervention assessments. Individuals were selected based on maximizing heterogeneity on the following four attributes: age, sex, psoriasis severity and responses to the item, ‘Since reading the leaflets, my understanding of psoriasis has changed’.
In order to obtain meaningful feedback on the materials from the interviews we purposively sampled people who reported their understanding of psoriasis to have changed a lot after reading the leaflets (e.g. participant 3, female, aged 42 years and participant 5, male, aged 69 years) and those who reported no change in understanding (e.g. participant 6, male, aged 44 years and participant 12, female, aged 67 years). The ranges of scores recorded for individuals in the interview sample on other variables reflected those of the larger sample used in the quantitative analysis. The qualitative subsample also included those with both positive views (e.g. participant 1, female, aged 65 years and participant 2, male, aged 62 years) and negative views (e.g. participant 9, female, aged 59 years and participant 11, female, aged 59 years) about the relevance of the content of the patient support materials.
Figure 3 shows the final study sample (with dropouts at each stage) and Table 3 presents the sample demographics for the quantitative (outcome measures) and qualitative (process evaluation) data.
Figure 3.
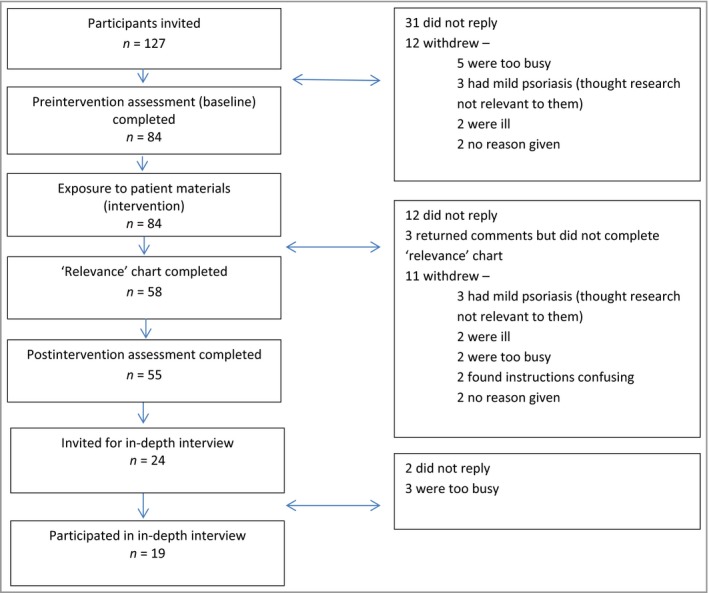
Final study sample with dropouts.
Table 3.
Sample characteristics
| Characteristics | Participants: quantitative outcomes study | Participants: qualitative process evaluation study |
|---|---|---|
| Female, n (%) | 55 (56) | 19 (63) |
| Current age (years), median (range) | 59 (31–79) | 59 (31–69) |
| Age at diagnosis (years), median (range) | 29 (7–65) | 40 (7–62) |
| Years with psoriasis, median (range) | 28 (2–67) | 19 (3–49) |
| Psoriasis severity (SPI severity subscale) | 48 mild, 5 moderate, 2 severe | 16 mild, 1 moderate, 2 severe |
SPI, Simplified Psoriasis Index.
Quantitative study (outcome measures)
Revised Illness Perceptions Questionnaire
Postintervention, a statistically significant difference between the means was found in the primary outcome ‘illness coherence’ [from 16·0 to 17·5; t(55) = −3·48, P = 0·001 (two‐tailed)], indicating a large effect size (η2 = 0·19). Notably, both the personal control and treatment control domains also improved postintervention, with a large [t(55) = −2·98, P = 0·004 (two‐tailed), η2 = 0·14] and moderate [t(55) = −2·08, P = 0·042 (two‐tailed), η2 = 0·08] effect size, respectively (Table 4). Data for all domains are reported in Table S3 (see Supporting Information).
Table 4.
Revised Illness Perceptions Questionnaire (IPQ‐R) domain and Hospital Anxiety and Depression Scale (HADS) changes pre‐ and postintervention
| IPQ‐R domain | Cronbach α | Mean changea | η2 | Effect size | P‐value |
|---|---|---|---|---|---|
| Illness coherence (primary target) | 0·91 | −1·49 | 0·19 | Large | ≤ 0·001 |
| Personal control | 0·91 | −1·42 | 0·14 | Large | ≤ 0·01 |
| Treatment control | 0·72 | −0·79 | 0·08 | Medium | ≤ 0·05 |
| HADS | Cronbach α | Mean changea | SD | t | P‐value |
|---|---|---|---|---|---|
| Anxiety | 0·88 | −0·25 | 2·34 | −0·76 | 0·45 |
| Depression | 0·84 | −0·26 | 2·63 | 0·73 | 0·47 |
Pre‐ vs. postintervention.
The materials resulted in changes in understanding of specific aspects of psoriasis: 31 of 54 (57%) participants reported not having a clear understanding of comorbidities preintervention, reducing to 19 (35%) postintervention; and 31 of 53 (58%) of the sample did not know about the relevance of lifestyle behaviours preintervention, reducing to 19 (36%) postintervention (the similarity in reported frequencies is coincidental).
Hospital Anxiety and Depression Scale
There were no clinically or statistically significant increases in HADS anxiety or depression scores after exposure to the materials, implying that improvements in understanding of the nature of psoriasis occurred without a corresponding increase in either anxiety or depression (Table 4). Cronbach's α scores for the IPQ‐R and the HADS domains range from 0·91 to 0·72, indicating high levels of internal reliability for these scores (Table 4).
Numerical rating scale scores
Overall 80% of participants reported that their understanding of psoriasis increased postintervention; none reported that their anxiety increased after reading the leaflets and 16% reported reduced anxiety (Table 5).
Table 5.
Self‐reported changes in understanding and anxiety after reading Pso Well® materials
| Increased, n (%) | Neutral, n (%) | Decreased, n (%) | |
|---|---|---|---|
| Understanding | 44 (80) | 11 (20) | 0 |
| Anxiety | 0 | 46 (84) | 9 (16) |
Leaflet relevance
The majority of participants indicated that the content of the leaflets was highly relevant. Notably, many indicated that it would have had relevance earlier in the course of their disease (Table 6).
Table 6.
Number and percentage of participants reporting on leaflet ‘relevance’ (n = 58)
| Leaflet | Highly relevant now | Relevant in the past |
|---|---|---|
| Changing phases | 29 (50) | 29 (50) |
| Linking mind and body | 26 (45) | 35 (60) |
| Your journey with psoriasis | 38 (67) | 42 (72) |
| Treatment overview | 26 (45) | 32 (55) |
| Topical treatments | 32 (55) | 29 (50) |
| Emollients | 33 (57) | 30 (52) |
| Steroid‐based topicals | 24 (41) | 33 (57) |
| Light therapy | 12 (21) | 21 (36) |
| Systemics and biologics | 14 (24) | 29 (50) |
| Why does my weight matter? | 31 (53) | 37 (64) |
| Keeping active feeling good | 34 (58) | 32 (55) |
| Smokeless | 7 (12) | 25 (43) |
| Is your glass half full? | 19 (33) | 27 (47) |
Process evaluation (qualitative study)
Analysis generated three themes explaining participants’ perspectives on the Pso Well® materials and what influenced their understanding of psoriasis: (i) ‘Seeing the bigger picture: psoriasis as more than a skin condition’; (ii) ‘Personalizing psoriasis: developing illness coherence’ and (iii) ‘Managing psoriasis differently: making changes’. All themes and subthemes are presented alongside illustrative data extracts (Table 7).
Table 7.
Themes and subthemes
| Theme 1: Seeing the bigger picture: psoriasis as more than a skin condition | |
|---|---|
| Sub‐theme | Data extract |
|
Newly discovered aspects of psoriasis
Learning about co‐morbidities |
It was something I didn't know…I thought that perhaps [psoriatic arthritis] applied to me…I didn't realise that psoriasis and arthritis could be combined (P1 female 65) |
| Learning about lifestyle behaviour links | A lot of the information was new to me…[leaflets] gave me a lot to think about…I didn't realise smoking and alcohol could affect [psoriasis] (P3 female 42) |
| Learning about treatments | I didn't even know there were things for psoriasis other than the ointment I'm using – I thought everybody used that! I wasn't aware there were other types of treatment…light therapy and that (P5 male 69) |
| Learning about disease/treatment mechanisms | Nobody had ever explained why you get…plaques…it's your skin cells speeded up and you've got a build‐up of what you can physically see (P17 female 32) |
| Enablers of learning | |
| Plain language style | The [materials] were at the right level without patronising people – it was just at the right level for me and just going in (P4 female 57) |
| Ease of navigation | [Leaflets] were uniform, so they'd all look nice and you'd choose your colour…and could go straight to it (P9 female 59) |
| Chunking of information | It's little bits at a time, little bits of information…bite‐sized, that's it (P7 female 45) |
| Positive/hopeful tone | It just puts the two things together [psoriasis and heart health]. The way it's written isn't threatening at all, it just makes it plain that there could be a link (P2 male 62) |
| Unintended consequences | |
| Disappointment in health services | It was a bit disappointing really that my doctor had never said there are new things (P5 male 69) |
| Self‐blaming | Having the leaflets, it made me angry with myself for not looking things up…I was a bit angry with myself and annoyed (P8 female 31) |
| Regret that information not made available earlier | When I saw all of [materials] I thought – all right, so this is the kind of information you can get access to! If we had this back then it would've been brilliant…I wouldn't have felt so alone with [psoriasis] (P6 male 44) |
| Theme 2: Personalising psoriasis: developing illness coherence | |
|---|---|
| Sub‐theme | Data extract |
| Making personal sense of psoriasis Finding a ‘reference point’ | I had no reference points or anything to know what should be happening or how bad [psoriasis] could get, so by having the leaflets – they said – if this doesn't work you can try this (P8 female 31) |
| Linking disease aspects to self | I recognised the sort of things that were me…a greater knowledge from reading all the different things and relating certain aspects to myself…I do understand [psoriasis] more now than I did (P4 female 57) |
| New awareness of bi‐directional links | I hadn't put the links together in my mind. I realised being withdrawn had made my psoriasis worse but hadn't…linked that one relates to the other. By having the leaflets I was able to understand all the little things that can affect it, things I hadn't thought about (P8 female 31) |
| Enablers of engagement with materials | |
| Personally relevant/resonant content (acknowledging emotional impact) | I thought…yes that's how it is…there it is on the page…it's not just a skin condition, it's the whole range of emotions that come with it as well (P6 male 44) |
| Perceived trustworthiness of the materials | The source of the information is the thing. You get all sorts of stuff on the internet, put up by all sorts of people, bloggers of every description…if you can go to a trusted source…the NHS is very much in that category (P18 male 61) |
| Perceived ‘high quality’ of materials content and design | [Leaflets] were quite professional…and…attractive, like you want to read them – they're not just your boring leaflets in waiting rooms in the NHS…you want to pick them up (P17 female 32) |
| Changing emotions and cognitions (feelings and thoughts) Reduced feelings of self‐blame/increased confidence | It's not my fault is one of the biggest things. By knowing all these things affect [psoriasis], it's not something I've done…that's made this happen…by having the leaflets… I felt more confident to go and sit and have breakfast in a coffee shop (P8 female 31) |
| Increased feelings of self‐esteem (being valued) | To be given something like [materials]…made me as a psoriasis sufferer feel valued, because so often dermatology – psoriasis – is the bottom of the pile…so this…the way it was presented…actually made me feel for once, somebody was trying to make me feel valued about it (P19 female 67) |
| Bringing previously ‘unconscious’ thoughts to the fore | I kind of made a personal link and I thought – hey – when I get stressed there are times when my psoriasis starts getting worse. So maybe I'd better watch that. Maybe I can do something about it (P17 female 32) |
| Self‐questioning about managing psoriasis differently | When I saw the leaflets…it did make me question things more, especially the use of lotions and things, that made me re‐think my journey with my doctor over the years, how I've let things lapse and not ask for further consultations. Those leaflets made me think, well actually, I should be more proactive (P3 female 42) |
| Theme 3: Managing psoriasis differently: making changes? | |
|---|---|
| Sub‐theme | Data extract |
| Materials as ‘stand‐alone’ tool Consulting in a different way Using medications differently | That leaflet was good in that it made me go back and think about [medication] and I got on a different topical lotion – changed it for the first time in as long as I can remember (P3 female 42) I make sure I look after [skin] properly and put the creams on the right way…I take more care…it's reading [materials] and trying to do things differently than I was before…sometimes I used to just ignore [psoriasis] (P1 female 65) |
| Taking action to address lifestyle behaviour | It [re‐joining Weight Watchers] was after that [reading leaflets]…because I felt better. Somebody understood me, understood my condition, understood how I feel (P7 female 45) |
| Perceived change mechanisms Tracking psoriasis with body diagram | Looking at [body diagram] from 5 months ago I'd have said [psoriasis] didn't do that [fluctuate]. I'm shocked looking now… when I completed the leaflets I felt I was in a good place, but my psoriasis is much better months along the line than it was (P3 female 42) |
| Identifying concerns and priorities with activities/charts | Seeing it written down made me realise that there were phases [to psoriasis] because – yes it's controlled…but…something would trigger it off again. It…made me realise what was bothering me (P4 female 57) |
| Identifying goals and strategies with activities/charts | You need a strategy…you need a plan…and I started to…write down what I need to do and then – right…the next stage is this (P1 female 65) |
| Increasing intention/motivation to make changes through engagement with activities | The activities was something I was able to use to help me…being able to put that tick…gave you a boost – like – yeah, you're doing what you need to do, you're going to get there (P8 female 31) |
| Materials as a ‘shared’ management tool Materials as a useful to ‘share’ with doctor | It would open up a conversation, if [GP] was to say – we've got these leaflets – where are you? It might make you feel…there's somebody caring and trying to improve the situation (P5 male 69) |
| ‘Shared’ tool as an incentive to change | The doctor could actually use [leaflet] and say – look – what we're going to do is I need you to keep a diary, to keep noting and…I want you to fill this in. Then the person is going to use the leaflet rather than…stick it in my drawer when I get home (P17 female 32) |
| Materials as a support for clinicians’ practice | I imagine [materials] would help GPs massively because I wonder how much GPs actually update their information about [skin] conditions…invaluable information here that you could use with the doctor (P3 female 42) |
| Resistance to using the materials | |
| Psoriasis experienced as mild/not bothersome | I don't think I was so keen on the [activities]…because it's saying how much is [psoriasis] affecting you at the moment and it wasn't affecting me…my psoriasis isn't normally that bad (P9 female 59) |
| Feeling ‘bombarded’ with lifestyle behaviour change messages in general |
I'm not sure anything in the [weight] leaflet would help…it's on the telly all the time, there's stop smoking things all over…all these years I've been trying to lose weight by doing what the doctors and everyone have said…and I think I was probably feeling like strangling them. (P9 female 59) |
| Perceiving messages as rigid/rule‐based |
For me personally it smacks a bit of work…you went on various courses and it would be ‘let's have a target here’ and… ‘we need to write an action plan!’…oh crikey here we go again (P13 female 64) |
Theme 1: seeing the bigger picture: psoriasis as more than a skin condition
Newly discovered aspects of psoriasis
Discovering hitherto unknown or unexplained aspects of psoriasis through exposure to the materials was a commonly reported experience. The leaflets enabled participants to build up a wider picture of psoriasis as a complex long‐term condition affecting more than the skin. Many were unaware of comorbidities, links with lifestyle behaviours, treatments available and the need for treatment review. Some learned about the mechanisms involved in psoriasis for the first time, for example the relapsing–remitting nature, its systemic basis, the plaque formation process and inflammatory links.
Enablers of learning
Features enabling participants to assimilate information, link aspects of psoriasis together and gain a sense of reassurance rather than distress included plain‐language style, colour coding to aid navigation, ‘chunking’ of information and the positive tone of language used.
Unintended consequences of exposure to Pso Well® materials
There were some unintended consequences of exposure to the new materials, highlighting that acquiring new information about psoriasis was not always a positive or even neutral process.
Some participants expressed disappointment in health services for failing to provide similar information; others blamed themselves for not actively seeking information. Participants expressed regret about not having access to the materials earlier in life, believing that this could have improved how they managed psoriasis.
Almost every participant interviewed learned something new from the materials, enabling them to link disease aspects together in a new way. Learning that psoriasis was a complex long‐term condition appeared to be offset by the positive, hopeful tone of the materials, but some disappointment was expressed that information had not been made available earlier.
Theme 2: personalizing psoriasis – developing illness coherence
Making personal sense of psoriasis
Participants reported that the materials helped ‘make sense’ of psoriasis. Sense making involved finding a ‘reference point’, linking disease aspects to self, understanding how psoriasis affects individuals personally and ways to manage it. A new awareness of the bidirectional links between psoriasis, mood and lifestyle behaviours and where these were personally relevant became apparent for some.
Enablers of engagement with the materials
Several factors enabled participants to engage with the materials. These included personally relevant or resonant content that confirmed or validated previously unarticulated feelings and thoughts (particularly having the emotional impact of psoriasis acknowledged), the perceived trustworthiness of the materials, and their high‐quality content and design.
Changes to emotions and cognitions (feelings and thoughts)
Participants reported that engagement with the materials promoted an improved personalized understanding of psoriasis (illness coherence). This encouraged an increased sense of personal control and/or prompted new ways of thinking about self‐management. Participants stated they: (i) felt less inclined to self‐blame for having psoriasis; (ii) experienced increased self‐confidence and self‐esteem (as a result of ‘warranting’ high‐quality, attractive health‐focused materials); (iii) became aware of new concepts (e.g. psoriasis and links with mood; the concept of ‘goal‐setting’); and (iv) began to self‐question about how to manage psoriasis differently (e.g. medication use, consulting behaviour and lifestyle behaviours).
Participants identified factors that promoted engagement with the materials: the trusted source and high quality, conveying a message that people with psoriasis were valued.
Theme 3: managing psoriasis differently: making changes?
Differing reasons were given for the materials’ potential to influence behavioural change. Some participants used them immediately as a ‘stand‐alone’ self‐management tool; some viewed them as a ‘shared’ management tool for use in conjunction with a health professional; and, more rarely, some participants were resistant to using the materials at all.
Pso Well® materials as a ‘stand‐alone’ self‐management tool
Some participants (who generally perceived their psoriasis as bothersome) used the materials as a ‘stand‐alone’ tool to change psoriasis management. Behavioural changes reported were: consulting differently, seeking referral to secondary care, using medications as recommended, taking steps to address low mood, and acting to make lifestyle behavioural changes. Thus, some participants were able to use the materials of their own volition without support from a third party.
Perceived mechanisms promoting intention or motivation for change
Participants who had been able to use the materials to make changes identified the ‘activity’ sections as useful facilitators of change. The activities (charts and exercises) enabled participants to track flares and identify concerns, priorities and goals, and to find strategies to achieve goals and increase intention to make changes.
Pso Well® materials as a ‘shared’ management tool
Some also viewed the materials as a beneficial self‐management tool, for use in partnership with health professionals such as general practitioners or specialist clinicians. This was particularly, but not exclusively, where individuals valued further explanation of the rationale for change (e.g. the mechanisms and evidence to support lifestyle behaviour links) or individualized support to identify goals and plans. The materials were viewed as useful for prompting meaningful discussions between patients and professionals, facilitating ‘shared’ monitoring and increasing the incentive for medication adherence and lifestyle changes. Participants believed that using the materials together with a clinician could enhance their credibility further, encouraging sustained patient engagement. The materials were also viewed as useful support for professionals in clinical practice.
Resistance to using the materials as a self‐management tool
There were some reports of resistance to using the materials, from participants who saw no need to change their self‐care routine if psoriasis was well controlled or mild. However, particularly in relation to lifestyle behaviour change, others appeared to react to an initial perception of the ‘top‐line’ messages, which could be experienced as threatening (similarly to commonly heard ‘fear‐based’ or rule‐bound health messages). If participants were already feeling negative about lifestyle changes, initial reading appeared to compound this response, acting as a barrier to further reading or deeper engagement with the materials.
In summary, the Pso Well® materials were used independently by some participants as tools for self‐management, while others saw benefit in sharing them to monitor and manage psoriasis in partnership with a clinician. Others had difficulty conceiving of their use, particularly in relation to lifestyle behaviour change, and appeared ‘defensive’ and unwilling to receive such health messages in general.
Discussion
The findings from the Pso Well® patient materials study indicate that carefully designed, high‐quality, theory‐based resources are acceptable to patients with psoriasis and can improve their understanding, coherence and sense of control, without a corresponding increase in anxiety. Furthermore, the materials appeared to have effects on beliefs about psoriasis, as well as emotional responses, of some participants, increasing their motivation or intention to change self‐management behaviour.
This study is the first to develop, test and evaluate an intervention for psoriasis that targets patients’ understanding of disease and treatment. This was a gap identified from a previous IMPACT programme of work,34, 37, 38, 39 and represents a new way of thinking about health communication in the psoriasis field. The authors recognized the possibility that a new or deeper understanding of the lifelong, relapsing–remitting nature of the condition might increase distress and that learning of the risks of comorbidities may be potentially anxiety provoking. In fact, understanding, motivation and intention all increased with no corresponding change in anxiety or depression. Several features of the Pso Well® materials appeared to facilitate this.
Firstly, the high‐quality, accurate content directly targeted illness beliefs, for example linking disease mechanisms with treatment options including the relevance of behaviour change for self‐management and helping patients recognize the remitting–relapsing nature of psoriasis. Notably, materials to improve understanding of disease also appeared to provide patients with a clearer rationale for treatments and vice versa.
Secondly, design values such as attention to readability and usability appeared to aid information processing. Writing for a basic reading ability while avoiding oversimplification, which may deter those with greater literacy levels, is recommended in health communication but challenging to accomplish.75 The Pso Well® leaflets appeared to achieve this balance. Additionally, their high‐quality ‘look and feel’ conveyed that psoriasis (a condition that often involves appearance‐related concerns) warrants attractive, engaging materials and that their target audience is valued. This contrasts markedly with the lack of design values in many health communication resources identified in our previous work.76
Thirdly, personally resonant and relevant information addressed emotional effects directly, acknowledging emotional impact and the rationale for self‐management using advice based on best evidence and improving understanding rather than simply increasing knowledge as many educational interventions do.
Finally, the positive, hopeful tone (emphasizing that people could take steps to help control their psoriasis and minimize the impact the condition had on their lives, even if comorbidities did arise in the future) appeared to reassure and encourage participants to engage with the materials, offsetting potentially threatening health messages about psoriasis as a more complex disease. The associated unintended consequences of exposure to the materials identified by the process evaluation highlight that information‐giving is not a neutral process and that attention to tone, language and message framing are crucial components in health communication.
This apparently simple intervention took the form of high‐quality paper leaflets; however, the content had undergone extensive development and testing. Participants’ accounts suggest that our use of written communication, including phrasing, use of metaphor and context, was important for clarifying or reinforcing messages that may have been superficially familiar but not previously understood in ways that could be of use in planning self‐care. Additionally, the study suggests that changing understanding may be a precursor to behaviour change. A trial of a face‐to‐face intervention to modify patients’ illness and treatment beliefs based on the same theoretical model as this study resulted in behavioural changes (increases in walking) that were maintained for at least 2 years.77 It is promising that a lower‐cost intervention may have at least some of the same outcomes.
The positive results must be interpreted with some caution due to the lack of a separate control group; however, restricting participants’ exposure to the intervention to a 2‐week period makes it unlikely that any confounding factor promoted the change in understanding within the time frame. Precise measures of responsiveness for the IPQ‐R domains and HADS are not readily available for this population, and this is a potential limitation of using these measures to assess the effects of exposure to these materials. We also recognize that this self‐selected sample may not be representative of the wider psoriasis population in that they may be more ‘engaged’ with health messages. However, the strong study design, which, following the Medical Research Council guidelines,52 measured the effects of the intervention and evaluated the intervention process to identify perceived mechanisms of action, can usefully inform future research. Patients in this study perceived that the materials could be a useful tool for ‘shared’ management of psoriasis in partnership with clinicians. A parallel skills‐based Pso Well® intervention demonstrated positive effects on clinicians’ knowledge and skills in managing psoriasis.78 It is possible that there would be additional synergistic effects of these materials if used by patients in collaboration with healthcare professionals who have undertaken the training.
In conclusion, the new Pso Well® materials are acceptable to patients and can improve understanding, coherence and sense of control in relation to psoriasis, without a corresponding increase in anxiety.
Supporting information
Table S1. Consultation process for Pso Well® patient materials development and refinement.
Table S2. Interview topic guide.
Table S3. Domain scores of the Revised Illness Perceptions Questionnaire from individuals who completed the pre‐ and postintervention measures.
Acknowledgments
We are grateful to the study participants for testing the Pso Well® materials and to members of the IMPACT Research User Group and clinicians who helped refine them. Thanks are due to Spoken Image (www.spoken-image.com) for design expertise. Access to the intervention materials can be arranged through the study principal investigator Dr Lis Cordingley (e‐mail: lis.cordingley@manchester.ac.uk).
Funding sources This article presents independent research funded by the National Institute for Health Research (NIHR) under its Programme Grants for Applied Research scheme (RP‐PG‐0608‐10163). The views expressed are those of the authors and not necessarily those of the National Health Service, the NIHR or the Department of Health.
Conflicts of interest None declared.
References
- 1. Parisi R, Symmons DPM, Griffiths CEM, Ashcroft DM. Global epidemiology of psoriasis: a systematic review of incidence and prevalence. J Invest Dermatol 2013; 133:377–85. [DOI] [PubMed] [Google Scholar]
- 2. de Korte J, Sprangers MAG, Mombers FMC, Bos JD. Quality of life in patients with psoriasis: a systematic literature review. J Invest Dermatol Symp Proc 2004; 9:140–7. [DOI] [PubMed] [Google Scholar]
- 3. Kurd SK, Troxel AB, Crits‐Christoph P, Gelfand JM. The risk of depression, anxiety, and suicidality in patients with psoriasis. A population‐based cohort study. Arch Dermatol 2010; 146:891–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Lebwohl M. Psoriasis. Lancet 2003; 361:1197–204. [DOI] [PubMed] [Google Scholar]
- 5. Russo PA, Ilchef R, Cooper AJ. Psychiatric morbidity in psoriasis: a review. Australas J Dermatol 2004; 45:155–61. [DOI] [PubMed] [Google Scholar]
- 6. Christophers E, Barker JN, Griffiths CE et al The risk of psoriatic arthritis remains constant following initial diagnosis of psoriasis among patients seen in European dermatology clinics. J Eur Acad Dermatol Venereol 2010; 24:548–54. [DOI] [PubMed] [Google Scholar]
- 7. Cohen AD, Dreiher J, Shapiro Y et al Psoriasis and diabetes: a population‐based cross‐sectional study. J Eur Acad Dermatol Venereol 2008; 22:585–9. [DOI] [PubMed] [Google Scholar]
- 8. Gisondi P, Targher G, Zoppini G, Girolomoni G. Non‐alcoholic fatty liver disease in patients with chronic plaque psoriasis. J Hepatol 2009; 51:758–64. [DOI] [PubMed] [Google Scholar]
- 9. Gisondi P, Tessari G, Conti A et al Prevalence of metabolic syndrome in patients with psoriasis: a hospital‐based case–control study. Br J Dermatol 2007; 157:68–73. [DOI] [PubMed] [Google Scholar]
- 10. Griffiths CE, Barker JN. Psoriasis 1 – Pathogenesis and clinical features of psoriasis. Lancet 2007; 370:263–71. [DOI] [PubMed] [Google Scholar]
- 11. Baker CS, Foley PA, Braue A. Psoriasis uncovered – measuring burden of disease impact in a survey of Australians with psoriasis. Australas J Dermatol 2013; 54(Suppl. 1):1–6. [DOI] [PubMed] [Google Scholar]
- 12. Kimball AB, Gieler U, Linder D et al Psoriasis: is the impairment to a patient's life cumulative? J Eur Acad Dermatol Venereol 2010; 24:989–1004. [DOI] [PubMed] [Google Scholar]
- 13. Parisi R, Rutter MK, Lunt M et al Psoriasis and the risk of major cardiovascular events: cohort study using the Clinical Practice Research Datalink. J Invest Dermatol 2015; 135:2189–97. [DOI] [PubMed] [Google Scholar]
- 14. Mehta NN, Azfar RS, Shin DB et al Patients with severe psoriasis are at increased risk of cardiovascular mortality: cohort study using the General Practice Research Database. Eur Heart J 2010; 31:1000–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Favato G. High incidence of smoking habit in psoriatic patients. Am J Med 2008; 121:e17. [DOI] [PubMed] [Google Scholar]
- 16. Fortes C, Mastroeni S, Leffondre K et al Relationship between smoking and the clinical severity of psoriasis. Arch Dermatol 2005; 141:1580–4. [DOI] [PubMed] [Google Scholar]
- 17. Kirby B, Richards HL, Mason DL et al Alcohol consumption and psychological distress in patients with psoriasis. Br J Dermatol 2008; 158:138–40. [DOI] [PubMed] [Google Scholar]
- 18. Landriscina AL, Friedman AJ. Integrating lifestyle approaches into psoriasis care: improving patient outcomes? Psoriasis Targets Ther 2016; 6:1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Samarasekera EJ, Neilson JM, Warren RB et al Incidence of cardiovascular disease in individuals with psoriasis: a systematic review and meta‐analysis. J Invest Dermatol 2013; 133:2340–6. [DOI] [PubMed] [Google Scholar]
- 20. Sommer DM, Jenisch S, Suchan M et al Increased prevalence of the metabolic syndrome in patients with moderate to severe psoriasis. Arch Dermatol Res 2006; 298:321–8. [DOI] [PubMed] [Google Scholar]
- 21. Naldi L, Chatenoud L, Linder D et al Cigarette smoking, body mass index, and stressful life events as risk factors for psoriasis: results from an Italian case–control study. J Invest Dermatol 2005; 125:61–7. [DOI] [PubMed] [Google Scholar]
- 22. Finucane MM, Stevens GA, Cowan MJ et al National, regional, and global trends in body‐mass index since 1980: systematic analysis of health examination surveys and epidemiological studies with 960 country‐years and 9.1 million participants. Lancet 2011; 377:557–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Gerdes S, Zahl VA, Weichenthal M, Mrowietz U. Smoking and alcohol intake in severely affected patients with psoriasis in Germany. Dermatol 2010; 220:38–43. [DOI] [PubMed] [Google Scholar]
- 24. Poikolainen K, Karvonen J, Pukkala E. Excess mortality related to alcohol and smoking among hospital‐treated patients with psoriasis. Arch Dermatol 1999; 135:1490–3. [DOI] [PubMed] [Google Scholar]
- 25. Setty AR, Curhan G, Choi HK. Smoking and the risk of psoriasis in women: Nurses’ Health Study II. Am J Med 2007; 120:953–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Smith KE, Fenske NA. Cutaneous manifestations of alcohol abuse. J Am Acad Dermatol 2000; 43:1–16. [DOI] [PubMed] [Google Scholar]
- 27. Wolk K, Mallbris L, Larsson P et al Excessive body weight and smoking associates with a high risk of onset of plaque psoriasis. Acta Derm Venereol 2009; 89:492–7. [DOI] [PubMed] [Google Scholar]
- 28. Frankel HC, Han J, Li T, Qureshi AA. The association between physical activity and the risk of incident psoriasis. Arch Dermatol 2012; 148:918–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Hamminga EA, van der Lely AJ, Neumann HA, Thio HB. Chronic inflammation in psoriasis and obesity: implications for therapy. Med Hypotheses 2006; 67:768–73. [DOI] [PubMed] [Google Scholar]
- 30. Jensen P, Zachariae C, Christensen R et al Effect of weight loss on the severity of psoriasis: a randomized clinical study. JAMA Dermatol 2013; 149:795–801. [DOI] [PubMed] [Google Scholar]
- 31. Naldi L, Conti A, Cazzaniga S et al Diet and physical exercise in psoriasis: a randomized controlled trial. Br J Dermatol 2014; 170:634–42. [DOI] [PubMed] [Google Scholar]
- 32. Appelhans BM, Whited MC, Schneider KL et al Depression severity, diet quality, and physical activity in women with obesity and depression. J Acad Nutr Diet 2012; 112:693–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Krueger G, Koo J, Lebwohl M et al The impact of psoriasis on quality of life – results of a 1998 National Psoriasis Foundation patient‐membership survey. Arch Dermatol 2001; 137:280–4. [PubMed] [Google Scholar]
- 34. Nelson PA, Chew‐Graham CA, Griffiths CEM, Cordingley L. Recognition of need in health care consultations: a qualitative study of people with psoriasis. Br J Dermatol 2013; 168:354–61. [DOI] [PubMed] [Google Scholar]
- 35. Thorneloe RJ, Bundy C, Griffiths CEM et al Adherence to medication in patients with psoriasis: a systematic literature review. Br J Dermatol 2013; 168:20–31. [DOI] [PubMed] [Google Scholar]
- 36. Edwards G, Gilbert AK, McAteer H. The patient experience: a survey of members of the Psoriasis Association. Br J Dermatol 2010; 163(Suppl. 1):40. [Google Scholar]
- 37. Nelson PA, Barker Z, Griffiths CEM et al ‘On the surface’: a qualitative study of GPs’ and patients’ perspectives on psoriasis. BMC Fam Pract 2013; 14:158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Nelson PA, Kane K, Chisholm A et al ‘I should have taken that further’ – missed opportunities during cardiovascular risk assessment in patients with psoriasis in U.K. primary care settings: a mixed‐methods study. Health Expect 2016; 19:1121–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Nelson PA, Keyworth C, Chisholm A et al ‘In someone's clinic but not in mine’ – practitioners’ views of supporting lifestyle behaviour change with patients with psoriasis: a qualitative study. Br J Dermatol 2014; 171:1116–22. [DOI] [PubMed] [Google Scholar]
- 40. Richards HL, Fortune DG, Weidmann A et al Detection of psychological distress in patients with psoriasis: low consensus between dermatologist and patient. Br J Dermatol 2004; 151:1227–33. [DOI] [PubMed] [Google Scholar]
- 41. Cordingley L, Nelson PA, Griffiths CEM, Chew‐Graham CA. Beyond skin: the need for a new approach to the management of psoriasis in primary care. Br J Gen Pract 2012; 62:568–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Larsen MH, Hagen KB, Krogstad A‐L et al Limited evidence of the effects of patient education and self‐management interventions in psoriasis patients: a systematic review. Patient Educ Couns 2014; 94:158–69. [DOI] [PubMed] [Google Scholar]
- 43. Pickett K, Frampton G, Loveman E. Education to improve quality of life of people with chronic inflammatory skin conditions: a systematic review of the evidence. Br J Dermatol 2016; 174:1228–41. [DOI] [PubMed] [Google Scholar]
- 44. Larsen MH, Krogstad AL, Aas E et al A telephone‐based motivational interviewing intervention has positive effects on psoriasis severity and self‐management: a randomized controlled trial. Br J Dermatol 2014; 171:1458–69. [DOI] [PubMed] [Google Scholar]
- 45. Wahl AK, Langeland E, Larsen MH et al Positive changes in self‐management and disease severity following climate therapy in people with psoriasis. Acta Derm Venereol 2015; 95:317–21. [DOI] [PubMed] [Google Scholar]
- 46. Leventhal H, Diefenbach M. Illness cognition: using common sense to understand treatment adherence and affect cognition interactions. Cognit Ther Res 1992; 16:143–63. [Google Scholar]
- 47. Petrie KJ, Jago LA, Devcich DA. The role of illness perceptions in patients with medical conditions. Curr Opin Psychiatry 2007; 20:163–7. [DOI] [PubMed] [Google Scholar]
- 48. Peyrot M, Rubin RR. Behavioral and psychosocial interventions in diabetes – a conceptual review. Diabetes Care 2007; 30:2433–40. [DOI] [PubMed] [Google Scholar]
- 49. Moss‐Morris R, Weinman J, Petrie KJ et al The revised Illness Perception Questionnaire (IPQ‐R). Psychol Health 2002; 17:1–16. [Google Scholar]
- 50. Fortune DG, Richards HL, Griffiths CEM, Main CJ. Targeting cognitive‐behaviour therapy to patients’ implicit model of psoriasis: results from a patient preference controlled trial. Br J Clin Psychol 2004; 43:65–82. [DOI] [PubMed] [Google Scholar]
- 51. Craig P, Dieppe P, Macintyre S et al Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ 2008; 337:a1655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Moore GF, Audrey S, Barker M et al Process evaluation of complex interventions: Medical Research Council guidance. BMJ 2015; 350:h1258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Nelson PA, Ashcroft DM, Bundy C et al The IMPACT programme in psoriasis: phase I – where we are now and future directions. Dermatol Nurs 2015; 14:37–44. [Google Scholar]
- 54. Hoffmann TC, Glasziou PP, Boutron I et al Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ 2014; 348:g1687. [DOI] [PubMed] [Google Scholar]
- 55. Abraham C, Kools M. Writing Health Communication: an Evidence‐Based Guide. Los Angeles: SAGE, 2012. [Google Scholar]
- 56. Moon G, Aitken G, Roderick P et al Towards an understanding of the relationship of functional literacy and numeracy to geographical health inequalities. Soc Sci Med 2015; 143:185–93. [DOI] [PubMed] [Google Scholar]
- 57. Osborne H. Health Literacy From A to Z: Practical Ways to Communicate Your Health Message. Burlington, MA: Jones and Bartlett Learning, 2013. [Google Scholar]
- 58. Szramka‐Pawlak B, Hornowska E, Walkowiak H, Zaba R. Hope as a psychological factor affecting quality of life in patients with psoriasis. Appl Res Qual Life 2014; 9:273–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Rutter MK, Kane K, Lunt M et al Primary care‐based screening for cardiovascular risk factors in patients with psoriasis. Br J Dermatol 2016; 175:348–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Fordham B, Griffiths CEM, Bundy C. A pilot study examining mindfulness‐based cognitive therapy in psoriasis. Psychol Health Med 2015; 20:121–7. [DOI] [PubMed] [Google Scholar]
- 61. Fortune DG, Richards HL, Main C, Griffiths CEM. What patients with psoriasis believe about their condition. JAMA Dermatol 1998; 39:196–201. [DOI] [PubMed] [Google Scholar]
- 62. Fortune DG, Richards HL, Main CJ, Griffiths CEM. Pathological worrying, illness perceptions and disease severity in patients with psoriasis. Br J Health Psychol 2000; 5:71–82. [Google Scholar]
- 63. O'Leary CJ, Creamer D, Higgins E, Weinman J. Perceived stress, stress attributions and psychological distress in psoriasis. J Psychosom Res 2004; 57:465–71. [DOI] [PubMed] [Google Scholar]
- 64. Richards HL, Fortune DG, Chong SLP et al Divergent beliefs about psoriasis are associated with increased psychological distress. J Invest Dermatol 2003; 123:49–56. [DOI] [PubMed] [Google Scholar]
- 65. Richards HL, Fortune DG, Griffiths CEM. Adherence to treatment in patients with psoriasis. J Eur Acad Dermatol Venereol 2006; 20:370–9. [DOI] [PubMed] [Google Scholar]
- 66. Scharloo M, Kaptein AA, Weinman J et al Patients’ illness perceptions and coping as predictors of functional status in psoriasis: a 1‐year follow‐up. Br J Dermatol 2000; 142:899–907. [DOI] [PubMed] [Google Scholar]
- 67. Wahl AK, Robinson HS, Langeland E et al Clinical characteristics associated with illness perception in psoriasis. Acta Derm Venereol 2014; 94:271–5. [DOI] [PubMed] [Google Scholar]
- 68. Zigmond AS, Snaith RP. The Hospital Anxiety and Depression Scale. Acta Psychiatr Scand 1983; 67:361–70. [DOI] [PubMed] [Google Scholar]
- 69. Lewis G, Wessely SC. Comparison of the General Health Questionnaire and the Hospital Anxiety and Depression Scale. Br J Psychiatr 1990; 157:860–4. [DOI] [PubMed] [Google Scholar]
- 70. McDonough E, Ayearst R, Eder L et al Depression and anxiety in psoriatic disease: prevalence and associated factors. J Rheumatol 2014; 41:887–96. [DOI] [PubMed] [Google Scholar]
- 71. Wessely SC, Lewis GH. The classification of psychiatric morbidity in attenders at a dermatology clinic. Br J Psychiatr 1989; 155:686–91. [DOI] [PubMed] [Google Scholar]
- 72. Chularojanamontri L, Griffiths CEM, Chalmers RJG. The Simplified Psoriasis Index (SPI): a practical tool for assessing psoriasis. J Invest Dermatol 2013; 133:1956–62. [DOI] [PubMed] [Google Scholar]
- 73. Corbin J, Strauss A. Basics of Qualitative Research: Techniques and Procedures for Developing Grounded Theory. Thousand Oaks, CA: Sage Publications, 2008. [Google Scholar]
- 74. Ritchie J, Lewis J. Qualitative Research Practice: a Guide for Social Science Students and Researchers. London: Sage Publications, 2003. [Google Scholar]
- 75. Rowlands G, Protheroe J, Winkley J et al A mismatch between population health literacy and the complexity of health information: an observational study. Br J Gen Pract 2015; 65:e379–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Keyworth C, Nelson PA, Griffiths CEM et al Do English healthcare settings use ‘Choice Architecture’ principles in promoting healthy lifestyles for people with psoriasis? An observational study. BMC Health Serv Res 2015; 15:215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Cunningham MA, Swanson V, Holdsworth RJ, O'Carroll RE. Late effects of a brief psychological intervention in patients with intermittent claudication in a randomized clinical trial. Br J Surg 2013; 100:756–60. [DOI] [PubMed] [Google Scholar]
- 78. Chisholm A, Nelson PA, Pearce CJ et al Motivational interviewing‐based training enhances clinicians’ skills and knowledge in psoriasis: findings from the Pso Well® study. Br J Dermatol 2017; 176:677–86. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Consultation process for Pso Well® patient materials development and refinement.
Table S2. Interview topic guide.
Table S3. Domain scores of the Revised Illness Perceptions Questionnaire from individuals who completed the pre‐ and postintervention measures.


