Abstract
Background:
Much controversy exists regarding the optimal surgical intervention for lateral epicondylitis because of a multitude of options available and the lack of comparative studies. Knowledge of the current practice trends would help guide the design of comparative studies needed to determine which surgical technique results in the best outcome.
Purpose:
To review the latest practice trends for the surgical treatment of lateral epicondylitis among newly trained surgeons in the United States utilizing the American Board of Orthopaedic Surgery (ABOS) database.
Study Design:
Cross-sectional study; Level of evidence, 3.
Methods:
The ABOS database was utilized to identify surgical cases for lateral epicondylitis submitted by Part II board certification examination candidates from 2004 through 2013. Inclusion criteria were predetermined using a combination of International Classification of Diseases, Ninth Revision (ICD-9) and Current Procedural Terminology (CPT) codes. Cases were organized by open and arthroscopic treatment groups and by fellowship training and were analyzed to determine differences in surgical techniques, complication rates, and concomitant procedures.
Results:
In total, 1150 surgeons submitted 2106 surgical cases for the treatment of lateral epicondylitis. The number of surgical cases for lateral epicondylitis performed per 10,000 submitted cases significantly decreased from 26.7 in 2004 to 21.1 in 2013 (P = .002). Among all cases, 92.2% were open and 7.8% were arthroscopic, with no change in the incidence of arthroscopic surgeries over the study period. Shoulder and elbow (18.1%) and sports medicine (11.4%) surgeons were more likely to perform surgery arthroscopically compared with hand surgeons (6.1%) (P < .001). There was no difference in overall self-reported complication rates between open (4.4%) and arthroscopic (5.5%) procedures (P = .666). Percutaneous tenotomy, debridement only, and debridement with tendon repair comprised 6.4%, 46.3%, and 47.3% of open treatment, respectively. Sports medicine, hand, and shoulder and elbow surgeons were more likely to repair the tendon after debridement compared with other surgeons, who were more likely to perform debridement alone (P < .001). Hand surgeons were most likely to perform concomitant procedures, of which the majority were neuroplasties.
Conclusion:
Although comparative studies are ultimately necessary for determining the optimal surgical technique, researchers should be mindful of the differences in practices according to training and the extent to which concomitant procedures are being performed, as both these factors may confound any future results.
Keywords: lateral epicondylitis, tennis elbow, ECRB, enthesopathy, arthroscopic surgery
Lateral epicondylitis, often referred to as “tennis elbow,” is a common condition thought to be related to overuse injuries to the extensor carpi radialis brevis (ECRB). The natural history of lateral epicondylitis typically involves the resolution of symptoms in 6 to 24 months, with most patients experiencing an improvement in symptoms within 1 year.3,11 Despite this phenomenon, it is estimated that 4% to 11% of patients fail nonoperative treatment and still undergo surgery.8 This may be related to the wide spectrum of tendinopathies in which mild forms (ie, loosening of the array of collagen fibers) may benefit from nonoperative measures, while more severe forms (ie, macroscopic tearing of the tendon-to-bone enthesis) may be more likely to fail nonoperative treatment.2
Much controversy exists regarding the optimal surgical intervention because of the many options available and the lack of comparative studies. Nirschl and Pettrone17 first described success with surgical excision of the diseased ECRB with good long-term results.6 Over the past decade, alternative surgical techniques have been posited to further improve upon clinical outcomes. Studies on arthroscopic and percutaneous techniques have reported a quicker recovery and return-to-work time,5,10,18,21,22 which are notable given that lateral epicondylitis is highly prevalent among manual laborers. Additionally, many have proposed that a main advantage of arthroscopic treatment is the ability to address other intra-articular abnormalities. Improved grip and pinch strength has been described with anatomic suture anchor repair of the tendon back to the lateral epicondyle.13,23
The extent to which these newer techniques have been adopted by surgeons, particularly newly practicing surgeons, is unknown. Given the multitude of options and the lack of consensus on the optimal surgical technique for lateral epicondylitis, knowledge of the current practice trends (and their contributing factors) would help guide the design of comparative studies needed to determine which procedure results in the best outcome. Therefore, the purpose of this study was to review the latest practice trends for the surgical treatment of lateral epicondylitis among newly trained surgeons in the United States utilizing the American Board of Orthopaedic Surgery (ABOS) database. We hypothesized that arthroscopic treatment would be increasingly performed by newly trained surgeons, given the recent evidence suggesting that it leads to good outcomes and an earlier return to work for patients. Additionally, in this population of newly practicing surgeons, we sought to determine any differences in practice according to fellowship training as well as any difference in complication rates between open and arthroscopic techniques.
Methods
Data Collection
A research proposal was submitted and approved by the ABOS to query the database for lateral epicondylitis procedures submitted for review by ABOS Part II examination candidates from 2004 to 2013. This database includes all case information from candidates’ case collection period, which consists of all operative cases performed over a 6-month period in preparation for Part II of their orthopaedic board certification. This case collection period typically occurs during an orthopaedic surgeon’s first 2 years in clinical practice. Data from the ABOS database were devoid of patient- or surgeon-identifying information. The provided data included the year of the procedure, International Classification of Diseases, Ninth Revision (ICD-9) codes, Current Procedural Terminology (CPT) codes, total number of cases submitted by the candidate, total number of cases submitted by all candidates, fellowship training (if applicable), region of practice, patient age, patient sex, and any associated surgeon-related complications.
From 2004 to 2013, 6854 board-eligible orthopaedic surgeons submitted a total of 858,146 cases for the ABOS Part II examination, resulting in a mean number of 125.2 cases per surgeon. For this study, cases coded as ICD-9 726.32 (lateral epicondylitis) and at least one of the open or arthroscopic CPT codes listed in the Appendix were collected. Before 2008, CPT codes for open epicondylitis procedures consisted of 24350, 24351, 24352, 24354, and 24356. Since 2008, these were replaced by more specific CPT codes: 24357 (percutaneous), 24358 (debridement only), and 24359 (debridement with tendon repair). Among the queried cases, those with secondary CPT codes were examined to determine the rates of concomitant procedures.
Statistical Analysis
Bivariate comparisons of means and proportions were performed using the Student t test and chi-square test, respectively. Comparisons of means and proportions among fellowship training were performed using 1-way analysis of variance and the chi-square test, respectively, with post hoc Bonferroni correction for multiple comparisons. To determine the significance of trends over time, a line of best fit was generated for the graphed data to illustrate the change over the years. The slope of this best-fit line was compared with a line with a slope of zero (no change over time) using chi-square linear-by-linear association analysis. Statistical significance was set at P < .05.
Results
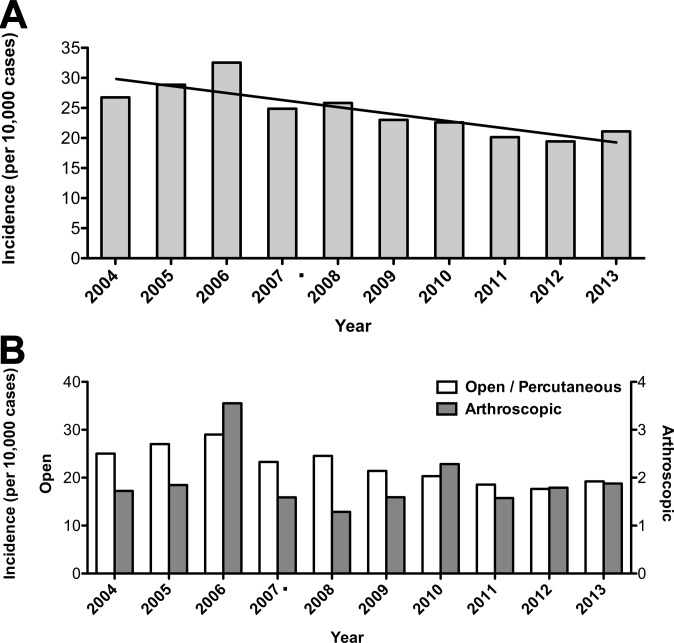
After querying the database for surgical procedure codes for lateral epicondylitis, we determined that 2106 cases submitted by 1150 surgeons met the inclusion criteria. Overall, the mean patient age was 45.7 ± 8.5 years, and 921 patients (43.7%) were male. The majority of cases were performed by surgeons with hand (44.3%), sports (27.4%), and no additional (15.7%) fellowship training. On average, surgeons with hand fellowship training performed more surgical cases (2.4) per 6-month collection period compared with those having sports medicine (1.5), adult reconstruction (1.4), and no additional (1.5) fellowship training (P < .001) (Table 1). The annual incidence, defined as the number of surgical cases for lateral epicondylitis performed per 10,000 submitted cases, significantly decreased from 26.7 in 2004 to 21.1 in 2013 (P = .002) (Figure 1A).
TABLE 1.
Cases Submitted per 6-Month Collection Period by Fellowship Training
| Fellowship Training | Mean No. of Cases |
|---|---|
| Adult reconstruction | 1.4a |
| Foot and ankle | 1.5 |
| Hand | 2.4 |
| Oncology | 1.5 |
| Pediatrics | 1.6 |
| Shoulder and elbow | 1.9 |
| Spine | 1.6 |
| Sports medicine | 1.5a |
| Trauma | 1.7 |
| None | 1.5a |
aP < .001 versus hand and upper extremity cases.
Figure 1.
Annual incidence of (A) total and (B) open/percutaneous versus arthroscopic treatment of lateral epicondylitis. The black line represents the linear trend for the presented data.
Since 2008 (after the implementation of more specific CPT codes), percutaneous tenotomy, debridement only, and debridement with tendon repair comprised 6.4%, 46.3%, and 47.3% of nonarthroscopic cases, respectively. Surgeons with sports medicine, hand, and shoulder and elbow fellowship training were more likely to perform debridement with tendon repair compared with other surgeons, who were more likely to perform debridement alone (P < .001) (Figure 2). More than half of open cases (55.8%) performed by sports medicine surgeons consisted of tendon repair, whereas this only consisted of a third (33.9%) of open cases performed by non–upper extremity surgeons. The rate of complications did not differ between the 3 treatment types (P = .412).
Figure 2.
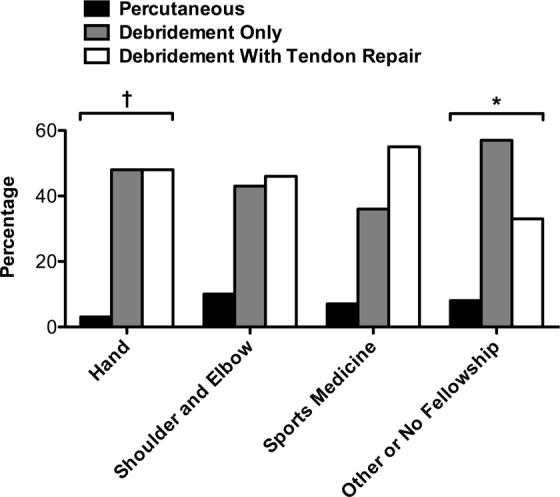
Percentage of percutaneous tenotomy, debridement only, and debridement with tendon repair cases by fellowship training. Cases presented are from 2008 to 2013 after the implementation of the latest Current Procedural Terminology (CPT) codes. *P < .001 compared with hand, shoulder and elbow, and sports medicine. † P < .001 compared with sports medicine and P = .023 compared with shoulder and elbow.
There were 1942 (92.2%) open/percutaneous cases and 164 (7.8%) arthroscopic cases for the treatment of lateral epicondylitis (Table 2). The mean age and sex distribution did not differ between the 2 groups. Overall, 18.1% of cases performed by shoulder and elbow surgeons and 11.4% of cases performed by sports medicine surgeons were arthroscopic. In contrast, only 6.1% of cases performed by hand surgeons and 4.9% of cases performed by surgeons without fellowship training were arthroscopic. There were no significant differences in the annual incidence of open/percutaneous and arthroscopic cases over time (P = .320) (Figure 1B).
TABLE 2.
Comparison of Open Versus Arthroscopic Surgical Treatment of Lateral Epicondylitisa
| Open | Arthroscopic | P | |
|---|---|---|---|
| Overall | 1942 (92.2) | 164 (7.8) | |
| Mean age, y | 45.7 | 45.7 | .960 |
| Sex | .536 | ||
| Male | 845 (43.5) | 76 (46.3) | |
| Female | 1097 (56.5) | 88 (53.7) | |
| Surgeon fellowship training | <.001 | ||
| Adult reconstruction | 65 (89.0) | 8 (11.0) | |
| Foot and ankle | 27 (100.0) | 0 (0.0) | |
| Hand | 915 (93.9) | 59 (6.1) | |
| Oncology | 3 (100.0) | 0 (0.0) | |
| Pediatric | 10 (90.9) | 1 (9.1) | |
| Shoulder and elbow | 86 (81.9) | 19 (18.1) | <.001b |
| Spine | 18 (100.0) | 0 (0.0) | |
| Sports medicine | 534 (88.6) | 69 (11.4) | <.001b |
| Trauma | 37 (94.9) | 2 (5.1) | |
| No fellowship | 329 (95.1) | 17 (4.9) |
aData are presented as n (%) unless otherwise indicated.
bCompared with hand.
A total of 95 self-reported complications were documented among all cases, resulting in an overall complication rate of 4.5% (Table 3). There was no significant difference in the rate of complications between open (4.4%) and arthroscopic (5.5%) procedures (P = .666). Similarly, there was no significant difference in the rate of complications when comparing surgeon fellowship training (P = .519).
TABLE 3.
Self-Reported Complication Rates Associated With Surgical Treatment of Lateral Epicondylitis
| Complication | Open, % | Arthroscopic, % |
|---|---|---|
| Infection | 0.93 | — |
| Surgical, unspecified | 0.88 | 3.05 |
| Nerve palsy or injury | 0.51 | 0.61 |
| Wound healing delay or dehiscence | 0.51 | — |
| Medical, unspecified | 0.46 | 0.61 |
| Skin ulcer or blister | 0.41 | — |
| Hemorrhage | 0.21 | — |
| Anesthetic complication | 0.15 | 0.61 |
| Stiffness or arthrofibrosis | 0.15 | — |
| Hematoma or seroma | 0.10 | — |
| Surgical procedure intervention | 0.10 | — |
| Deep venous thrombosis | 0.05 | — |
| Dermatological complaint | 0.05 | — |
| Failure of tendon or ligament repair | 0.05 | — |
| Fall | 0.05 | — |
| Pain, uncontrolled | 0.05 | 0.61 |
| Tendon or ligament injury | 0.05 | — |
| Total | 4.43 | 5.49 |
Concomitant procedures were seldom performed for both open and arthroscopic treatments of lateral epicondylitis (Table 4). Among open cases, cubital tunnel release (3.3%), neuroplasty (excluding ulnar) of the arm (3.2%), and carpal tunnel release were the most common concomitant procedures, and the majority of these were performed by surgeons with hand fellowship training. Specifically, 86.5% of concomitant radial tunnel releases were performed by surgeons with hand fellowship training. Arthroscopic synovectomy (13.4%) and removal of loose bodies (4.3%) were the most common concomitant procedures among arthroscopic cases.
TABLE 4.
Concomitant Procedures With Surgical Treatment of Lateral Epicondylitisa
| Concomitant Procedure | Open, n (%) | Arthroscopic, n (%) | Performed by Fellowship Training, % | |
|---|---|---|---|---|
| Hand | Sports Medicine | |||
| Neuroplasty (excluding ulnar), arm | 62 (3.2) | 1 (0.6) | 80.1 | 17.5 |
| Radial tunnel releaseb | 36 (1.9) | 1 (0.6) | 86.5 | 2.7 |
| Cubital tunnel release | 64 (3.3) | 6 (3.7) | 70.0 | 14.3 |
| Carpal tunnel release | 63 (3.2) | 3 (1.8) | 75.8 | 15.2 |
| LCL repair or reconstruction | 13 (0.7) | 1 (0.6) | 64.3 | 15.4 |
| Arthrotomy, elbow, with synovectomy | 13 (0.7) | 1 (0.6) | 85.7 | 0.0 |
| Arthroscopic synovectomy | NA | 22 (13.4) | 31.8 | 45.5 |
| Arthroscopic removal of loose bodies | NA | 7 (4.3) | 42.9c | 85.7c |
aLCL, lateral collateral ligament; NA, not applicable.
bCases of neuroplasty (excluding ulnar), arm coded with International Classification of Diseases, Ninth Revision (ICD-9) code 354.3 (radial nerve syndrome).
cSum of percentages is >100 because of 1 surgeon with both hand and sports medicine fellowship training.
Discussion
The results of this study demonstrate a declining incidence of surgical procedures for lateral epicondylitis in recent years, with no change in the incidence of arthroscopic procedures being performed by newly trained surgeons. No significant difference in the overall complication rate was found between open and arthroscopic techniques. Substantial differences in practices were found among newly trained surgeons depending on fellowship training. Surgeons with hand fellowship training performed a higher number of surgical cases per collection period than those trained in other subspecialties and were most likely to perform concomitant procedures, of which the majority were to address compression neuropathies at the elbow and wrist. Most surgical cases were performed in an open fashion, although shoulder and elbow as well as sports medicine surgeons were most likely to perform arthroscopic surgery. Finally, sports medicine, hand, and shoulder and elbow surgeons were more likely to repair the tendon after debridement compared with other surgeons, who were more likely to perform debridement alone.
The optimal management of lateral epicondylitis remains ambiguous, in part, because of the uncertainty regarding its pathological basis. Nevertheless, the natural history of lateral epicondylitis seems to indicate that it is a self-limiting condition, with 80% to 90% of patients reporting the resolution of symptoms within 1 year.3,11 It stands to reason that symptoms persisting for longer than 1 year can still resolve without any particular treatment. In our study, the annual incidence of surgery declined over the observed decade, with an overall mean of 1.8 cases per surgeon per 6-month collection period, indicating that newly practicing surgeons are being more cautious in their approach. Additionally, this decline may be partially attributed to the popularization of platelet-rich plasma injections for the treatment of lateral epicondylitis7,19 as well as the addition of eccentric exercises to improve physical therapy protocols.25 Many patients, however, may be unwilling to pursue conservative modalities after a prolonged period of pain and dysfunction, and without a standardized treatment protocol for lateral epicondylitis, surgeons are not remiss in offering operative treatment with proven long-term success and a minimal risk to those who may have more severe grades of tendinopathy.2,4,6,9 It is estimated that between 4% and 11% of patients eventually undergo surgery,8 and our results demonstrate that newly practicing hand surgeons performed a higher rate of these surgeries than other fellowship-trained surgeons. Although it may be easy to attribute this observation to differences in the treatment culture between the hand community and others, additional factors, such as a higher clinic volume and patient demographics, may also contribute. Nevertheless, a more detailed comparison of the management strategies between newly trained hand and sports medicine surgeons, who performed the majority of surgical cases in this study, is warranted, as our results suggest vastly different philosophies between the 2 groups.
The implementation of more specific CPT codes in 2008 allowed us to differentiate between 3 surgical techniques: percutaneous tenotomy, debridement only, and debridement with tendon repair. Interestingly, sports medicine, hand, and shoulder and elbow surgeons were more likely to repair the tendon compared with other surgeons, who were more likely to perform debridement alone. Although the early studies by Nirschl et al6,14,17 described the excision of diseased tissue alone without reattachment to the lateral epicondyle, several recent studies have reported superior grip and pinch strength after suture anchor repair of the ECRB tendon to the lateral epicondyle after open debridement.13,20,23 Surgeons specialized in hand, shoulder and elbow, and sports medicine may be more familiar with these recently published results, and thus, they may be more inclined to include suture anchor repair as part of their open treatment. Although several studies have advocated for percutaneous release,5,10 the incidence of percutaneous treatment remained low throughout the observation period in our study. Our study suggests that percutaneous and arthroscopic techniques are not being increasingly adopted by newly trained surgeons, even as minimally invasive procedures are becoming more popular to patients in medicine overall.
Arthroscopic treatment consisted of a small percentage of the total surgical cases for lateral epicondylitis, and there was high variation in the use of arthroscopic surgery among surgeons with different fellowship training. It is not surprising that shoulder and elbow as well as sports medicine surgeons were more likely to perform arthroscopic treatment, given the emphasis on arthroscopic surgery during their fellowship training. In contrast, hand surgeons typically receive less training in arthroscopic surgery during their fellowship and may be more resistant to performing arthroscopic treatment. In the past decade, there have been several studies comparing open versus arthroscopic techniques for lateral epicondylitis, with arthroscopic release demonstrating at least equivalent outcomes to open release and a more rapid return to work.5,18,21,22 However, contrary to our hypothesis, the incidence of arthroscopic treatment did not change over the study period. Although arthroscopic treatment potentially offers the advantages of a faster return to work and less postoperative physical therapy, the disadvantages of increased operative time and technical challenges may continue to discourage surgeons from adopting this approach.
A proposed advantage of arthroscopic treatment is the ability to address concomitant intra-articular abnormalities. Previous studies have reported addressing concomitant abnormalities in 18% to 58% of patients undergoing arthroscopic treatment for lateral epicondylitis, of which the vast majority of these conditions were synovitis.1,9,12,22 This is consistent with the results of our study, in which arthroscopic synovectomy was coded in 13% of all arthroscopic cases. However, it is unclear what criteria are used to establish this diagnosis and, more importantly, to what degree the synovectomy portion of the procedure truly affects the outcome. Loose intra-articular bodies can be addressed arthroscopically, and doing so can have a significant impact on relieving mechanical symptoms. Szabo et al22 reported a 5% incidence of loose bodies in their series, and Lattermann et al12 reported a 3% incidence of loose bodies. Similarly, among newly trained surgeons, we found that removal of loose bodies was coded in 4% of arthroscopic cases. This indicates that concomitant abnormalities may be uncommon in the setting of lateral epicondylitis and that the proposed benefit of arthroscopic surgery for assessing and simultaneously addressing these conditions may be overstated.
Interestingly, the most common concomitant procedure was neuroplasty, and a significant majority of these were performed by hand surgeons. Prior studies have shown that in patients with lateral epicondylitis, 5% have coexisting radial tunnel syndrome, while 50% of patients with radial tunnel syndrome may have concomitant lateral epicondylitis.24 In contrast, the coexistence of cubital tunnel syndrome and carpal tunnel syndrome with lateral epicondylitis is less defined. Szabo et al22 reported 7 posterior interosseous nerve releases and 3 carpal tunnel releases in their series of 109 patients. Dunn et al6 reported 24 ulnar nerve releases and 1 carpal tunnel release in their series of 139 procedures. There is a subset of patients with compromised tendon durability, multiple tendinosis symptoms (rotator cuff, medial and lateral tennis elbow), and compression neuropathies (carpal tunnel syndrome, cubital tunnel syndrome) whose clinical presentations Nirschl et al15,16 termed as mesenchymal syndrome. According to the results of the present study, hand surgeons seemed to be more cognizant of these compression neuropathies and were more inclined to treat them. Whether the ultimate outcomes are affected by these concomitant neuroplasties is unknown.
There are several limitations to this study. As with any retrospective review of a national database, the results may be subject to errors in coding and data logging and are limited by the nonspecific description of certain codes. For instance, among the CPT codes for neuroplasties at the elbow, only one is specific to a single nerve (64718, neuroplasty and/or transposition of the ulnar nerve). Additionally, arthroscopic procedure codes specific to the treatment of lateral epicondylitis do not exist. This likely resulted in the underestimation of arthroscopic cases. Because the database is used for administrative and board certification purposes, detailed clinical patient information was not available, making it difficult to ascertain the homogeneity of the populations or the indications for concomitant procedures. The complications provided were often nonspecific and rare, preventing a more meaningful interpretation or conclusions. Furthermore, the follow-up for patients may have ranged from as short as 9 to 15 months because of the structure of the case collection period for the Part II examination. This may have substantially underreported the number of complications.
In conclusion, the incidence of surgical procedures for lateral epicondylitis has declined in recent years, with no change in the incidence of arthroscopic procedures being performed among newly trained orthopaedic surgeons. Although comparative studies are ultimately necessary for determining the optimal surgical technique, researchers should be mindful of the differences in practices according to training and the extent to which concomitant procedures are being performed, as both these factors may confound any future results.
Appendix
ICD-9 and CPT Codes Useda
| Diagnosis/Procedure | ICD-9/CPT Code |
|---|---|
| Diagnosis | |
| Lateral epicondylitis | 726.32 |
| Radial nerve syndrome | 354.3 |
| Open Treatment - Before 2008 | |
| Fasciotomy, lateral or medial (eg, tennis elbow or epicondylitis) | 24350 |
| Fasciotomy, lateral or medial (eg, tennis elbow or epicondylitis); with extensor origin detachment | 24351 |
| Fasciotomy, lateral or medial (eg, tennis elbow or epicondylitis); with annular ligament resection | 24352 |
| Fasciotomy, lateral or medial (eg, tennis elbow or epicondylitis); with stripping | 24354 |
| Fasciotomy, lateral or medial (eg, tennis elbow or epicondylitis); with partial ostectomy | 24356 |
| Open Treatment - 2008 and After | |
| Tenotomy, elbow, lateral or medial (eg, epicondylitis, tennis elbow, golfer’s elbow); percuteanous | 24357 |
| Tenotomy, elbow, lateral or medial (eg, epicondylitis, tennis elbow, golfer’s elbow); debridement, soft tissue and/or bone, open | 24358 |
| Tenotomy, elbow, lateral or medial (eg, epicondylitis, tennis elbow, golfer’s elbow); debridement, soft tissue and/or bone, open with tendon repair or reattachment | 24359 |
| Arthroscopic Treatment | |
| Arthroscopy, elbow, surgical; with removal of loose body or foreign body | 29834 |
| Arthroscopy, elbow, surgical; synovectomy, partial | 29835 |
| Arthroscopy, elbow, surgical; synovectomy, complete | 29836 |
| Arthroscopy, elbow, surgical; debridement, limited | 29837 |
| Arthroscopy, elbow, surgical; debridement, extensive | 29838 |
| Unlisted procedure, arthroscopy | 29999 |
| Concomitant Procedures | |
| Neuroplasty (excluding ulnar), arm | 64708, 64722 |
| Radial tunnel release | 64708, 64722, and 354.3 |
| Cubital tunnel release | 64718 |
| Carpal tunnel release | 64721, 29848 |
| Lateral collateral ligament repair or reconstruction | 24343, 24344 |
| Arthrotomy, elbow, with synovectomy | 24102 |
| Arthroscopic synovectomy | 29835, 29836 |
| Arthroscopic removal of loose body | 29834 |
aICD-9, International Classification of Diseases, Ninth Revision; CPT, Current Procedural Terminology.
Footnotes
The authors declared that they have no conflicts of interest in the authorship and publication of this contribution.
Ethical approval for this study was obtained from the American Board of Orthopaedic Surgery.
References
- 1. Baker CL, Jr, Baker CL., 3rd Long-term follow-up of arthroscopic treatment of lateral epicondylitis. Am J Sports Med. 2008;36(2):254–260. [DOI] [PubMed] [Google Scholar]
- 2. Bhabra G, Wang A, Ebert JR, Edwards P, Zheng M, Zheng MH. Lateral elbow tendinopathy: development of a pathophysiology-based treatment algorithm. Orthop J Sports Med. 2016;4(11):2325967116670635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Binder AI, Hazleman BL. Lateral humeral epicondylitis: a study of natural history and the effect of conservative therapy. Br J Rheumatol. 1983;22(2):73–76. [DOI] [PubMed] [Google Scholar]
- 4. Calfee RP, Patel A, DaSilva MF, Akelman E. Management of lateral epicondylitis: current concepts. J Am Acad Orthop Surg. 2008;16(1):19–29. [DOI] [PubMed] [Google Scholar]
- 5. Dunkow PD, Jatti M, Muddu BN. A comparison of open and percutaneous techniques in the surgical treatment of tennis elbow. J Bone Joint Surg Br. 2004;86(5):701–704. [DOI] [PubMed] [Google Scholar]
- 6. Dunn JH, Kim JJ, Davis L, Nirschl RP. Ten- to 14-year follow-up of the Nirschl surgical technique for lateral epicondylitis. Am J Sports Med. 2008;36(2):261–266. [DOI] [PubMed] [Google Scholar]
- 7. Gosens T, Peerbooms JC, van Laar W, den Oudsten BL. Ongoing positive effect of platelet-rich plasma versus corticosteroid injection in lateral epicondylitis: a double-blind randomized controlled trial with 2-year follow-up. Am J Sports Med. 2011;39(6):1200–1208. [DOI] [PubMed] [Google Scholar]
- 8. Gregory BP, Wysocki RW, Cohen MS. Controversies in surgical management of recalcitrant enthesopathy of the extensor carpi radialis brevis. J Hand Surg Am. 2016;41(8):856–859. [DOI] [PubMed] [Google Scholar]
- 9. Grewal R, MacDermid JC, Shah P, King GJ. Functional outcome of arthroscopic extensor carpi radialis brevis tendon release in chronic lateral epicondylitis. J Hand Surg Am. 2009;34(5):849–857. [DOI] [PubMed] [Google Scholar]
- 10. Grundberg AB, Dobson JF. Percutaneous release of the common extensor origin for tennis elbow. Clin Orthop Relat Res. 2000;(376):137–140. [DOI] [PubMed] [Google Scholar]
- 11. Haahr JP, Andersen JH. Prognostic factors in lateral epicondylitis: a randomized trial with one-year follow-up in 266 new cases treated with minimal occupational intervention or the usual approach in general practice. Rheumatology (Oxford). 2003;42(10):1216–1225. [DOI] [PubMed] [Google Scholar]
- 12. Lattermann C, Romeo AA, Anbari A, et al. Arthroscopic debridement of the extensor carpi radialis brevis for recalcitrant lateral epicondylitis. J Shoulder Elbow Surg. 2010;19(5):651–656. [DOI] [PubMed] [Google Scholar]
- 13. Monto RR. Tennis elbow repair with or without suture anchors: a randomized clinical trial. Tech Shoulder Elbow Surg. 2014;15(3):92–97. [Google Scholar]
- 14. Nirschl RP. Lateral extensor release for tennis elbow. J Bone Joint Surg Am. 1994;76(6):951. [DOI] [PubMed] [Google Scholar]
- 15. Nirschl RP. Mesenchymal syndrome. Va Med Mon (1918). 1969;96(11):659–662. [PubMed] [Google Scholar]
- 16. Nirschl RP, Ashman ES. Tennis elbow tendinosis (epicondylitis). Instr Course Lect. 2004;53:587–598. [PubMed] [Google Scholar]
- 17. Nirschl RP, Pettrone FA. Tennis elbow: the surgical treatment of lateral epicondylitis. J Bone Joint Surg Am. 1979;61(6A):832–839. [PubMed] [Google Scholar]
- 18. Peart RE, Strickler SS, Schweitzer KM., Jr Lateral epicondylitis: a comparative study of open and arthroscopic lateral release. Am J Orthop (Belle Mead NJ). 2004;33(11):565–567. [PubMed] [Google Scholar]
- 19. Peerbooms JC, Sluimer J, Bruijn DJ, Gosens T. Positive effect of an autologous platelet concentrate in lateral epicondylitis in a double-blind randomized controlled trial: platelet-rich plasma versus corticosteroid injection with a 1-year follow-up. Am J Sports Med. 2010;38(2):255–262. [DOI] [PubMed] [Google Scholar]
- 20. Pruzansky ME, Gantsoudes GD, Watters N. Late surgical results of reattachment to bone in repair of chronic lateral epicondylitis. Am J Orthop (Belle Mead NJ). 2009;38(6):295–299. [PubMed] [Google Scholar]
- 21. Solheim E, Hegna J, Oyen J. Arthroscopic versus open tennis elbow release: 3- to 6-year results of a case-control series of 305 elbows. Arthroscopy. 2013;29(5):854–859. [DOI] [PubMed] [Google Scholar]
- 22. Szabo SJ, Savoie FH, 3rd, Field LD, Ramsey JR, Hosemann CD. Tendinosis of the extensor carpi radialis brevis: an evaluation of three methods of operative treatment. J Shoulder Elbow Surg. 2006;15(6):721–727. [DOI] [PubMed] [Google Scholar]
- 23. Thornton SJ, Rogers JR, Prickett WD, Dunn WR, Allen AA, Hannafin JA. Treatment of recalcitrant lateral epicondylitis with suture anchor repair. Am J Sports Med. 2005;33(10):1558–1564. [DOI] [PubMed] [Google Scholar]
- 24. Tsai P, Steinberg DR. Median and radial nerve compression about the elbow. Instr Course Lect. 2008;57:177–185. [PubMed] [Google Scholar]
- 25. Tyler TF, Thomas GC, Nicholas SJ, McHugh MP. Addition of isolated wrist extensor eccentric exercise to standard treatment for chronic lateral epicondylosis: a prospective randomized trial. J Shoulder Elbow Surg. 2010;19(6):917–922. [DOI] [PubMed] [Google Scholar]