Abstract
Our aim was to systematically review how social functioning is measured, conceptualised, impacted, and associated with mental disorders in populations affected by humanitarian crises. Quantitative studies conducted with civilian populations affected by humanitarian crises in low- and middle-income countries with outcomes of social functioning were examined up to 2014. Data sources included Medline, Embase, PsycInfo, and Global Health, and 8 grey literature sources, yielding 14,350 records, of which 20 studies met inclusion criteria. A descriptive synthesis analysis was used, and the final selected studies assessed for quality using a modified Newcastle-Ottawa Scale. In the 20 studies, social functioning was conceptualised in six categories: family functioning, friendship quality, functional impairment, overall social functioning, social adaptation, and social relations. Seventeen studies were cross-sectional, two were cohort, and one a controlled trial. The quality of the studies was generally moderate. The limited evidence suggests that social functioning is relevant variable. Greater crisis exposure is associated with more severe depression and lower social functioning. The protective role of familial and social resources for social functioning is highlighted in different crisis settings. However, greater research on social functioning and mental health is required.
Keywords: humanitarian crisis, mental health, functioning, disability, war
Background
More than two-thirds of the world’s population live in countries affected by humanitarian crises from armed conflicts and natural disasters, and the vast majority of these are low- and middle-income countries (LMICs) where the need for assistance is greatest (UNOCHA, 2013). These crises can precipitate and exacerbate mental disorders (Jones, Asare, Elmasri, & Mohanraj, 2007). The most frequently reported mental health outcomes in humanitarian settings are post-traumatic stress disorder (PTSD) (Neria, Nandi, & Galea, 2008), depression, anxiety, and ‘general mental health’ (Blanchet, Roberts, Sistenich, Ramesh, Frison, Warren, Hossain, Knight, Lewis, & Smith, 2013). Elevated rates of mental disorders have been observed in crisis settings due to exposure to violence and other potentially traumatic events; and also social stressors such as loss of livelihoods and homes, increasing poverty, and reduced social support (Steel, Chey, Silove, Marnane, Bryant, & van Ommeren, 2009) (Porter & Haslam, 2005; Roberts & Browne, 2011). Underpinning these factors is limited infrastructure for mental health (Tol, Barbui, Galappatti, Silove, Betancourt, Souza, Golaz, & van Ommeren, 2011) (WHO, 2013).
Social functioning can be defined as “an individual’s ability to perform and fulfil normal social roles” (Hirschfeld, Montgomery, Keller, Kasper, Schatzberg, Moller, Healy, Baldwin, Humble, Versiani, Montenegro, & Bourgeois, 2000). Conceptually, social functioning can be thought of as one aspect of disability, in addition to physical functioning and satisfaction, which are all sub-domains of quality of life (Murray & Lopez, 1996). Measures of social Functioning commonly includes assessment of ability to make and maintain friends, quality of interpersonal relationships, participation in work and community activities, or quality of familial interactions. Historically, the Global Assessment of Functioning (GAF) scale to assess general functioning was first included in the Diagnostic and Statistical Manual of Mental Disorders (DSM) III-R which providde an overall rating of “psychological, social, and occupational functioning” (Cooper and Michels, 1988). This was further expanded in DSM IV-TR with the development of the Social and Occupational Functional Assessment Scale (SOFAS) which assessed social and occupational functioning independent of psychiatric symptoms (Burns & Patrick, 2007). With the publication of the DSM 5, the GAF and SOFAS scales were dropped and an optional measure of disability was included – the World Health Organization’s Disability Assessment Scale 2.0 (WHODAS 2.0). The WHODAS 2.0 assesses functioning in six domains, and is grounded in the theory of the International Classification of Functioning, Disability and Health (ICF) which considers functioning and disability as multi-dimensional concepts relating to an individual’s body and structures, the activities and areas of life in which they participate, and how the environment shapes their experiences (WHO, 2001b).
Evidence from stable settings shows that social functioning is impaired by a number of mental disorders, particularly depression and schizophrenia, and contributes strongly to the stigma around these illnesses (De Silva, Cooper, Li, Lund, & Patel, 2013). The impairment in individuals with mental disorders can be higher than for those with chronic physical conditions such as heart disease and diabetes (Hays, Wells, Sherbourne, Rogers, & Spritzer, 1995; Moussavi, Chatterji, Verdes, Tandon, Patel, & Ustun, 2007). Social functioning is also an area that is improved by psychosocial interventions (Burns & Patrick, 2007). Improving social functioning is increasingly seen as an important factor in reducing the burden of mental disorders (Lopez, Mathers, Ezzati, Jamison, & Murray, 2006; Patel, Araya, Chatterjee, Chisholm, Cohen, De Silva, Hosman, McGuire, Rojas, & van Ommeren, 2007b). However, social functioning is not well understood, primarily due to the fact that there is no consensus on how to measure it – with multiple measures used (some without proven validity and reliability) and the interchangeable use of terms such as “social functioning,” “social adaptation,” “patient functioning,” and “functional impairment” (Goldman, Skodol, & Lave, 1992) (Burns & Patrick, 2007).
Exposure to humanitarian crises and the associated increase in mental disorders is linked with different domains of psychosocial functioning (Steel, Silove, Phan, & Bauman, 2002). The potential importance of the concept of social functioning in humanitarian crises has been highlighted, along with the need for more research on it (Blanchet, Roberts, Sistenich, Ramesh, Frison, Warren, Hossain, Knight, Lewis, & Smith, 2013). The aim of this study was to systematically examine how social functioning is measured, conceptualised, impacted, and associated with mental disorders in civilian populations affected by humanitarian crises in LMICs.
Methods
A systematic review methodology was used, following the guidance in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement for reporting systematic reviews and meta-analyses (Liberati, Altman, Tetzlaff, Mulrow, Gøtzsche, Ioannidis, Clarke, Devereaux, Kleijnen, & Moher, 2009).
The exposure of interest was humanitarian crisis, defined as “a serious disruption of the functioning of a community or a society causing widespread human, material, economic or environmental losses which exceeds the ability of the affected community or society to cope using its own resources, necessitating a request to national or international level for external assistance” (Blanchet, Roberts, Sistenich, Ramesh, Frison, Warren, Hossain, Knight, Lewis, & Smith, 2013). This includes armed conflict (within or between nations), and natural disasters such as earthquakes, tsunamis, hurricanes. All humanitarian crises phases were included (e.g. acute, chronic, early recovery, and post conflict).
The population of interest was civilians (all ages) in LMICs exposed to humanitarian crises. LMICs were selected as the vast majority of people affected by LMICs live in humanitarian crises and the resources available to support them are very different to those in high-income countries. The population of interest includes those remaining in humanitarian settings, those forcibly displaced within the country as internally displaced persons (IDPs) and forcibly displaced across national borders as refugees. Studies were included if the country setting was a LMIC at the time the study was conducted as determined by World Bank classification (World Bank, 2014). Refugees from LMICs resident in high-income countries were excluded.
The outcome of interest was social functioning. A review of social functioning measures found that despite variability in domains assessed, all measures shared three domains in common: work, social, and family (Hirschfeld, Montgomery, Keller, Kasper, Schatzberg, Moller, Healy, Baldwin, Humble, Versiani, Montenegro, & Bourgeois, 2000). Thus, only measures of social functioning that involved an interpersonal component in either the social, work, and/or family domain were included. No restriction was placed on whether these components were assessed individually, or as part of a composite scale assessing more than one of them. Thus, if a study assessed a single component (e.g. occupational functioning) it would be included, as would studies which assessed multiple components of social functioning. No restriction was placed on whether social functioning was assessed as a primary or secondary outcome. Studies were excluded if they employed a composite measure involving, but not specific to, social functioning (for example, quality of life, Global Assessment of Functioning, and the short 12 item version of the WHODAS 2.0 measures). However, studies were included if they reported specific subscales on social functioning within these larger measures. Single-item measures of social functioning, such as a single question assessing functioning status, were excluded as they were considered insufficient measures of social functioning.
The types of studies included were primary quantitative studies from both published and grey literature. Mixed-methods studies were included for their quantitative component. Only English language studies were included. The search was not restricted by date.
Search strategy
A combination of free text and subject headings were used for each database. Free text was determined by compiling a list of relevant and recurring terms related to humanitarian crises, functioning, and mental health. Functioning was searched broadly rather than focusing on “social functioning” due to the lack of consensus on the construct’s description in the literature. Search terms were organized into three categories: humanitarian crisis terms (e.g. armed conflict, natural disaster), functioning terms (e.g. social functioning, psychosocial functioning), and mental health terms (e.g. depression, PTSD). Subject headings and MeSH terms were identified for each database, and then combined with free text using Boolean operators “OR” and “AND.” The bibliographic databases searched were: Medline, PsycInfo, Embase, and Global Health. The full search terms for each bibliographic database varied as a result of their different subject headings. The full search terms with results for each database are provided in Appendix 1. The following grey literature databases were searched: MSF Field Research, PsycExtra, the Mental Health and Psychosocial Support Network, WHO, UNICEF IRC, UNHCR, Healthnet TPO, and the Global Initiative on Psychiatry. Most grey literature sources did not have provisions for conducting advanced searches and so a broad search terms of ‘functioning’, ‘mental health’ and ‘humanitarian crisis’ were used.
Searches were conducted in June 2014 (with no publication time limits placed). All records were downloaded into Endnote X6, and screened in the following process: stage 1 – duplicates deleted; stage 2 – title/abstract screened; stage 3 – title/abstract double screened; stage 4 – full-text review and screening of identified articles; stage 5 – full-text review of final selected studies. Bibliographies of the final selected studies were also checked for additional references.
Data extraction and analysis
Data from all included studies were extracted into a spreadsheet. The following variables were extracted: study author(s), year, study design, study country, population, humanitarian crisis type, crisis stage, social functioning type, assessment instrument used, descriptive data on social functioning, data on association between social functioning and mental health, and data on other variable associations with social functioning. Descriptive analysis was conducted on the extracted data as a meta-analysis was not possible due to the heterogeneity in measures of crisis exposure, social functioning, and mental health. The domains used to categorize social functioning in the studies were: overall social functioning, family functioning, functional impairment, friendship quality, social adaptation, and social relations.
Quality appraisal was conducted using a modified Newcastle-Ottawa Scale (NOS), which has proven validity and reliability (Deeks, Dinnes, D'Amico, Sowden, Sakarovitch, Song, Petticrew, Altman, International Stroke Trial Collaborative, & European Carotid Surgery Trial Collaborative, 2003; Higgins & Green, 2008; Wells G.A., 2014), by two independent reviewers whom achieved consensus on separate category areas after resolving discrepancies. The NOS assigns stars for methodological rigour based on three categories: study selection, comparability of study groups, and outcome assessment. The NOS version by Herzog, Alvarez-Pasquin, Diaz, Del Barrio, Estrada, and Gil (2013) for cross-sectional studies was used, with an additional category created in which a star was awarded for use of a validated social functioning measure. For simplicity, three categories were created to assign a quality rating for each study: ‘weak’ (1-4 stars), ‘moderate’ (5-7 stars), and ‘strong’ (8-11 stars).’ The adapted NOS scale is presented in Appendix 2. No studies were excluded based on quality criteria.
Results
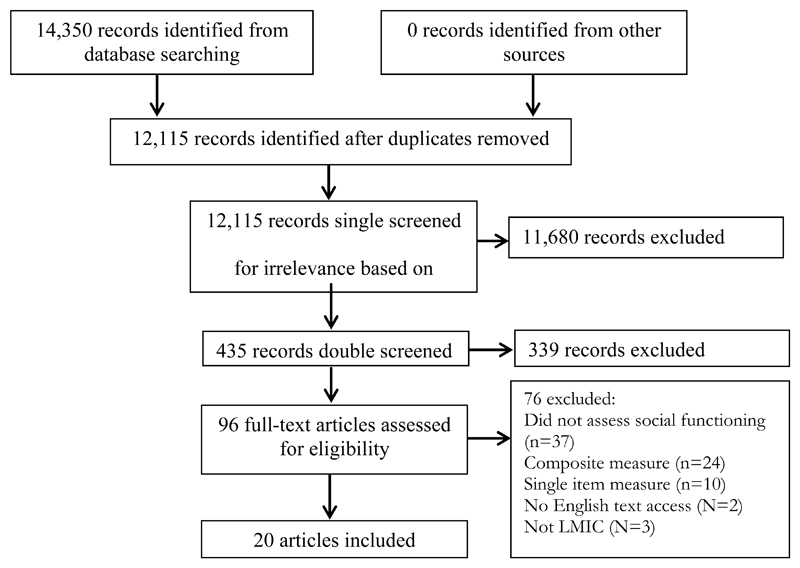
The results of the study selection process are shown in Figure 1. Upon completion of searching, duplicates were removed which yielded 12,115 unique records. After screening titles and abstracts for relevance, 435 records were identified, which were then double screened to yield 96 records. After full-text review of these studies, the final sample meeting eligibility criteria was 20 (referred to by number as studies 1–20). The excluded papers were those that were not in LMICs, did not assess social functioning, used single item measures or were part of a larger composite health measure, and not in English (two potentially eligible studies were excluded based on language). No included studies came from grey literature sources. Nineteen studies were observational in design (16 cross-sectional, 2 cohort, 1 case-control), with a single intervention study using a controlled trial design.
Figure 1. results of search process.
The sample of studies covered 12 LMICs affected by humanitarian crises. The general study characteristics are provided in Table 1. The majority of study settings were affected by armed conflict (n=13), followed by earthquake (n=3), tsunami (n=3), and flood (n=1). The studies conducted in the aftermath of natural disasters (n=7) ranged from 6-24 months post-disaster. Six of the studies were conducted post-conflict with non-displaced populations (6, 7, 8, 10, 16, 18). Three studies were with IDPs, refugees, or both (4, 9, 15). Four studies were conducted during conflict with non-displaced populations (1, 11, 13, 14). The studies focused mainly on adult populations, with 16 studies assessing individuals 15 years and above (1, 2, 3, 4, 6, 7, 8, 9, 10, 12, 13, 15, 16, 17, 19, 20), while 3 studies assessed children 10-14 years old (5, 14, 18), and 1 study assessing children around 5 years old (11).
Table 1. General characteristics of the studies.
| Ref | Author(s), (Year) | Design | Country | Population | Crisis Type | Group Classification |
|---|---|---|---|---|---|---|
| 1 | Babic-Banaszak et al., 2002 | Cross-sectional | Croatia* | 1,297 adults from war and non-war affected areas. Mean age = 50.8 years. | War | During conflict; non-displaced |
| 2 | Cao et al., 2013a | Cross-sectional | China | 264 bereaved individuals. Mean age = 45.9 years. | Earthquake | 18 months after disaster; displaced |
| 3 | Cao et al., 2013b | Cross-sectional | China | 190 adults who lost a child. Mean age = 40.5 years. | Earthquake | 18 months after disaster; displaced |
| 4 | Ferren, 1999 | Cross-sectional | Croatia*/Bosnia-Herzegovina | 104 refugee and displaced adolescents. Mean age = 15.8 years. | War | Post-conflict; IDPs and refugees |
| 5 | Kilic et al., 2003 | Cross-sectional | Turkey | 49 children in survivor camps. Mean age = 10.3 years. 65 parents in same camp. Mean age = 35.7 years. | Earthquake | 6 months after disaster; displaced |
| 6 | Lopes Cardozo et al., 2005 | Cross-sectional | Afghanistan | 699 Afghani adults. No mean age given. Most between 15-34 years. | War | During conflict; non-displaced |
| 7 | Lopes Cardozo et al., 2004a | Cross-sectional | Afghanistan | 699 Afghani adults and 100 disabled Afghani adults. No mean age given. Most between 15-34 years. | War | During conflict; non-displaced |
| 8 | Lopes Cardozo et al., 2003 | Cross-sectional | Kosovo | 1399 Kosovar Albanians. No mean age given. Most between 15-34 years. | War | Post-conflict; IDPs |
| 9 | Lopes Cardozo et al., 2004b | Cross-sectional | Thailand | 495 Karen refugees. No mean age given. Most between 15-34 years. | War | Post-conflict; refugees |
| 10 | Lopes Cardozo et al., 2000 | Cross-sectional | Kosovo | 1358 Kosovar Albanians. No mean age given. Most between 15-34 years. | War | Post-conflict; IDPs and refugees |
| 11 | Massad et al., 2011 | Cross-sectional | Palestine | 350 preschool children in Gaza Strip. Mean age = 4.9 years. | War | During conflict; non-displaced |
| 12 | Norris et al., 2005 | Cohort | Mexico | 658 adults from flood-affected areas. Mean age = 37.0 years. | Flood | 6,12,18,24 months after disaster; non-displaced |
| 13 | Pat-Horenczyk et al., 2009 | Cross-sectional | Palestine/Israel | 1,235 Palestinian school children in the West Bank. Mean age = 15.9 years. | War | During conflict; non-displaced |
| 14 | Peltonen et al., 2012 | Controlled trial | Palestine | 225 Palestinian school children in Gaza Strip. Mean age = 11.4 years. | War | During conflict; non-displaced |
| 15 | Radanovic-Grguric et al., 2009 | Case-control | Croatia* | 47 women with at least one episode of major depressive disorder. No mean age given. All between 35-55 years. | War | Post-conflict; IDPs |
| 16 | Talbot et al., 2013 | Cohort | Rwanda | 120 orphan full-time students. Median age = 18.0 years. | Genocide | Post-conflict; non-displaced |
| 17 | Tuicomepee et al., 2013 | Cross-sectional; semi-structured interviews | Thailand | 400 adolescents attend 4 tsunami-affected public schools. Mean age = 15.3 years. | Tsunami | 1 year after disaster; non-displaced |
| 18 | Usta et al., 2010 | Cross-sectional | Lebanon | 1028 children presenting at primary health centres. Mean age = 11.9 years. | War | Post-conflict; non-displaced |
| 19 | van Griensven, et al., 2006 | Cross-sectional | Thailand | 256 displaced and 400 non-displaced individuals from tsunami affected provinces. Mean ages = 39.5 and 42.0 for displaced and non-displaced respectively. | Tsunami | 1 year after disaster; displaced and non-displaced |
| 20 | Wickrama et al., 2011 | Cross-sectional | Sri Lanka | 325 tsunami affected mothers and adolescents. Mean age for mothers = 42.0 years. No mean age given for adolescents. Most (90%) above 10 years. | Tsunami | 1 year after disaster; displaced and non-displaced |
Study conducted in Croatia before it was classified as a high-income country by the World Bank.
Quality Assessment
The NOS ‘Selection’ category assesses representativeness of the sample, sample size, response rate, and method for measuring the exposure. Ten studies received at least 4 stars out of a possible 5 in this category, indicating that half of the included studies are likely to possess biases in their sampling strategies. Seven studies did not employ random sampling, and consequently did not receive a star (3, 4, 13, 15, 17, 18, 20). Additionally, only one study provided data on non-respondents (14). Eight studies did not use a validated tool to measure exposure to violent and traumatic events.
The ‘Comparability’ category assesses controlling for confounding factors based on study design or analysis. All studies received a maximum 2 stars in controlling for confounding factors.
The ‘Outcome’ category concerns whether the outcome was assessed using independent blind assessment, linkage to existing records, or self-report. A star is also awarded for conducting the appropriate statistical test, and reporting confidence intervals and probability level (p value). All but one study (20) received a star for measuring social functioning with a validated instrument. Twelve studies received a full rating for statistical completeness as they presented measurement of association data, probability levels, and/or confidence intervals. The overall quality of included studies was judged to be ‘moderate’ as the average quality was 7.5 stars out of a possible 11 stars. Further details are provided in Appendix 3.
Social functioning classification and association with mental health
Social functioning was conceived in six different ways in the included studies: family functioning (n=6), friendship quality (n=1), functional impairment (n=1), overall social functioning (n=10), social adaptation (n=1), and social relations (n=1). It was measured using 16 different scales. Of the included studies, only 3 used scales that were validated against the country context (studies 1, 5, and 19), and 9 reported reliability of scales in the study population (studies 4–7, 9, 11, 14, 17, and 19). The measurement instruments utilized in more than one study were the Short-Form 36 subscale (n=5), the Medical Outcomes Study 20 (n=2), and the Family APGAR Index (n=2). The types of social functioning addressed in the studies and their corresponding measures are provided in Table 2.
Table 2. Social functioning types and associations with mental disorders and other variables.
| Ref | Author(s), (year) | Type | Measure | Associations with Mental Disorders | Associations with Other Variables |
|---|---|---|---|---|---|
| 2 | Cao et al., 2013a | Family functioning | Family APGAR Index; Family Adaptability and Cohesion Evaluation Scale a (FACESa). | - | Family functioning negatively associated with Emotional and social loneliness;*** positively associated with having another baby* and less financial loss** (controlling for demographic and disaster-affected variables) |
| 3 | Cao et al., 2013b | Family functioning | Family APGAR Index | Positive family functioning associated with less severe depression*** (controlling for demographic and disaster-affected variables) | |
| 5 | Kilic et al., 2003 | Family functioning | McMaster Family Assessment Device | - | Family dysfunction positively associated with state-trait anxiety in children** (controlling for age, gender, parents’ GHQ and BDI scores, PTSD status of parents, and FAD general score) |
| 17 | Tuicomepee et al., 2013 | Family functioning | The General Functioning Scale | - | Family functioning negatively associated with adolescent behavioural problems** (controlling for demographic variables, religious beliefs, school connectedness, mental health services, and tsunami-related variables) |
| 18 | Usta et al., 2010 | Family functioning | Family Functioning in Adolescence Questionnaire | - | Family functioning negatively associated with childhood sexual abuse* (controlling for age, family size, and father’s education) |
| 20 | Wickrama et al., 2011 | Family functioning | 14 items adapted from questionnaire in Portes, Rumbaut | Positive family functioning associated with less severe depression* (controlling for negative life events, family poverty, and perceived community participation) | Family functioning negatively associated with family poverty and negative life events* |
| 14 | Peltonen et al., 2012 | Friendship quality | Friendship Quality Scale | - | Intervention associated with higher friendship quality in girls exposed to trauma*** (controlling for time, group, gender, and trauma variables) |
| 13 | Pat-Horenczyk et al., 2009 | Functional impairment | Relevant items from the Diagnostic Predictive Scales (DPS) | Increased post-traumatic stress associated with greater functional impairment*** (bivariate analysis) | Functional impairment positively associated with increased exposure to conflict*** (controlling for gender) |
| 1 | Babic-Banaszak et al., 2002 | Overall social functioning | SF-36 subscale | - | Social functioning negatively associated with living in a war-affected area* (bivariate analysis) |
| 4 | Ferren, 1999 | Overall social functioning | Children’s Multidimensional Scales of Perceived Self-Efficacy (CMSPSE) | Perceived self-efficacy positively associated with PTSD trauma* (controlling for age) | - |
| 9 | Lopes Cardozo et al., 2005 | Overall social functioning | SF-36 subscale | - | Social functioning negatively associated with female gender** (controlling for demographic variables) |
| 7 | Lopes Cardozo et al., 2004a | Overall social functioning | SF-36 subscale | - | Social functioning negatively associated with female gender* and disability* (controlling for demographic variables) |
| 8 | Lopes Cardozo et al., 2003 | Overall social functioning | MOS-20 subscale | - | - (controlling for demographic, chronic illness, and exposure variables) (controlling for demographic variables) |
| 9 | Lopes Cardozo et al., 2004b | Overall social functioning | SF-36 subscale | - | Social functioning negatively associated with lack of sufficient food*** and older age* |
| 10 | Lopes Cardozo et al., 2000 | Overall social functioning | MOS-20 subscale | - | Social functioning negatively associated with living in a rural environment***, unemployment*, and having a chronic health condition** (controlling for stratification and clustered design effects, in addition to demographic and chronic illness variables) |
| 11 | Massad et al., 2011 | Overall social functioning | PedsQL subscale | - | Social functioning negatively associated with older age*, greater exposure to traumatic events***, and living in direct military confrontation*** (controlling for child and household variables) |
| 16 | Talbot et al., 2013 | Overall social functioning | Acceptance and Action Questionnaire 2nd Edition (AAQ2). Children Global Assessment Scale (CGAS). | - - | Social functioning negatively associated with higher trauma symptoms* (controlling for HIV risk-taking behaviours, trauma symptoms, and HIV knowledge) |
| 19 | van Griensven, et al., 2006 | Overall social functioning | SF-36 subscale | - | Social functioning negatively associated with displacement*** (bivariate analysis) |
| 15 | Radanovic-Grguric et al., 2009 | Social adaptation | Social Adaptation Self-evaluation Scale | Depression after two years associated with poorer social adjustment* (controlling for time spent in displacement, accommodation during displacement, and family circumstances during displacement) | - |
| 12 | Norris et al., 2005 | Social relations | Provisions of Social Relations Scale | - | Education positively associated with help received from family and friends*** Female gender negatively associated with social support* and social embeddedness*** (controlling for demographic variables) |
p<.05.
p<.01.
p<.001
Family Functioning
Emotional and social loneliness was significantly negatively associated with family functioning among earthquake-affected parents in China, meaning that the stronger one perceived family functioning, cohesion, and adaptability, the less loneliness they felt (r ranged from –0.31 to –0.53, p<0.001) (2). In the same sample, having another baby in the wake of bereavement significantly positively predicted better family functioning and family cohesion scores (β = 0.13, p <0.04; β = 0.15, p <0.01) (2). Additionally, the more bereaved parents positively perceived family functioning, the less severe depression they felt (r = −.46, p<.001) (3). The study among earthquake survivors in Turkey observed a positive association between family dysfunction and anxiety (r=.48, p<.01 and r=.43, p<.01 respectively for state and trait anxiety) (5).
Family functioning was also positively correlated with less financial loss after an earthquake in China (β = –0.20, p<0.01) (2), and with greater perceived community participation after a tsunami in Sri Lanka leading to a reduction in depression symptoms (β = –0.50, p < 0.05) (20). It was negatively correlated with adolescent behavioural problems (r= -0.19, p<.01) in post-tsunami Thailand (17), childhood sexual abuse (r = -0.068, p<.05) in war-affected Lebanon (18), and family poverty (t= -3.39, p<.05) and stressful family events (t= -2.61, p<.05) in post-tsunami Sri Lanka (20).
Friendship Quality
Among girls in the Gaza Strip exposed to high levels of trauma, participation in a school mediated intervention was associated with a higher level of friendship quality (F(2, 149) = 10.25, p <.001) (14). No other significant differences were found on other dimensions of social functioning.
Functional Impairment
One study among adolescents in the Israeli Palestinian Conflict recorded that greater exposure to conflict resulted in greater functional impairment (F(1, 1218) = 52.65, p< .001) (13). Additionally, increased post-traumatic stress symptoms were significantly associated with greater functional impairment (r= .39, p< .001) in this sample (13).
Overall Social Functioning
In a study of Palestinian children in the Gaza strip, better social functioning was negatively associated with greater exposure to traumatic events (mean scores for witnessing more than 10 events compared with less than 10 events=52.0 and 65.5 respectively, p<.01), and living in areas of direct military confrontation (mean scores for living compared with not living in military area=56.0 and 66.0 respectively, p<.001) (11). Similarly, in a study of Rwandan orphans, higher trauma symptoms were associated with poorer social functioning (r=-.20, p<.05) (16). Living in a war-affected area of Croatia was negatively associated with social functioning as well (t=2.111, p<.05) (1). Living in displacement was also associated with poorer social functioning among tsunami survivors in Thailand (mean scores for displaced compared with non-displaced individuals=65.7 and 74.9 respectively, p<.001) (19). However, in a study among adolescent Bosnian And Croatian refugees adults, enlisting social resources and family support surprisingly had a significant positive correlation with PTSD symptoms (mean self-efficacy scores=5.52 and 4.40 for PTSD positive and non-traumatized groups respectively, p<.05) (4).
Overall social functioning was significantly negatively associated with the female gender in two studies from Afghanistan, with mean scores on the SF-36 social functioning subscale for women and men were 51.89 and 65.63 respectively, p<.002 (6); and 51.89 and 65.63, p<.02 respectively (7). When adjusting for all other demographic variables, older age (p<.016), lack of sufficient food (p<.001), living in a rural environment (p<.001), current employment (p<.046), having a chronic health condition (p<.01), and greater exposure to traumatic events (p<.02) were significantly associated with social functioning in two studies from Kosovo and the Thai-Burmese border (9, 10). Social functioning was significantly negatively associated with physical disability in a study from Afghanistan, with mean scores (95% CI) for nondisabled and disabled respondents of 57.2 (53.5-61.0) and 46.4 (38.0-54.8), (p<.04), respectively (7).
Social Adaptation
One study examined social adaptation among internally displaced women in the Croatian war for independence (15). Women with a history of depressive disorders who were depressed for 2 years post-conflict showed difficulties in social adjustment compared with women who were depressed for less than 2 years: (mean Social Adaptation Self-Evaluation Scale scores: 25.30±11.20 for depressed refugees and 39.75±4.56 for non-depressed refugees, t=2.42, p<.05) (15).
Social Relations
In a study of flood-affected populations in Mexico, education was significantly positively related to receiving help from family (β=.21, p<.001), friends (β=.19, p<.001), but not help from outsiders (β=.07, not significant) (12). Women felt less social support (β= -.09, p<.05) and social embeddedness/the feeling of having a role in a social structure (β= -.24, p<.001) than men after a disaster (12).
Discussion
The findings from this systematic review suggest that the amount of knowledge on social functioning in humanitarian crises is still limited. Most of the included studies were cross-sectional in design, with only one study of an intervention, indicating the evidence on effectiveness mental health psychosocial support interventions promoting social functioning remains negligible. Furthermore, only five studies included mental disorder outcomes (3, 4, 13, 15, 20). These commonly observed an association between lower social functioning and worse mental disorder symptoms
The quality of the studies was generally moderate with an average of 7.5 stars out of a possible 11 stars. Key deficiencies in quality included incomplete statistical reporting regarding confidence intervals, lack of non-respondent data, and use of non-randomised sampling. These issues suggest that many included studies are likely to possess biased results.
The use of locally validated measures for social functioning appears limited. Though some studies used feedback from locals to guide the development of a general questionnaire, only 3 studies used measures validated for their study population (1, 5, 19). This reflects the findings of a similar systematic review of social functioning in non-humanitarian LMIC contexts, in which very few of the included studies used social functioning measures validated for the respective settings (De Silva, Cooper, Li, Lund, & Patel, 2013). Given the challenges of developing and validating new measures, a pragmatic approach would be the greater use of measures that have been used and validated in multiple cultural contexts such as the WHODAS 2.0 (Ustun TB, Kostanjsek N, Chatterji S, & Rehm J, 2010). A related recommendation is that studies should consider reporting the specific results of the social functioning domain from broader validated functioning measures, such as the specific “getting along” interpersonal domain in the WHODAS 2.0.
Social functioning was conceptualised into 6 domains in this review – family functioning, friendship quality, functional impairment, overall social functioning, social adaptation and social relations – each incorporating an interpersonal element regarding daily life activities and the individual’s ability to perform them. Even when the construct measured was not explicitly termed ‘social functioning’ or ‘family functioning,’ they all emphasised the ability of individuals to interact with others in their environment. The study by Ferren (4) of adolescent Bosnian and Croatian refugees was unique in that it conceptualised social functioning specifically as perceived self-efficacy in a number of interpersonal domains such as enlisting social resources, social self-efficacy, and enlisting familial support. Similarly, the study by Norris et al (12) of a flood-affected population in Mexico was unique as it conceptualised social functioning on multiple levels involving couples, families, social networks, and communities. In line with previous work on the temporal processes of social functioning (Rajkumar, Premkumar, & Tharyan, 2008), this review highlights the need to capture how social functioning changes over time, on multiple levels, and within a changing humanitarian context.
In line with the finding that the ability to enjoy supportive relationships and accept help from others relates to resilience during hardship (Armstrong, Birnie-Lefcovitch, & Ungar, 2005), these elements were explored through measuring elements such as “functional impairment,” “social relations,” “social adaptation,” and “friendship quality”. The study by Ferren (4) of adolescent Bosnian and Croatian refugees was unique in that it conceptualised social functioning specifically as perceived self-efficacy in a number of interpersonal domains such as enlisting social resources, social self-efficacy, and enlisting familial support. This was the only study that attempted to assess specific indicators of social functioning, and equated it with an individual’s belief in their own social abilities (4).
Interestingly, the study by Van Griensven et al (19) in post-tsunami Thailand found that increased perceived community participation in recovery processes was positively associated with recovery at the family and individual level. Perceived community participation was significantly negatively associated with depression and PTSD symptoms. Community participation post-disaster may be protective against PTSD and depression severity as it fosters a certain degree of routine daily activity, and returns individuals to a certain level of functioning (Andermann, 2002). Shared ethno-cultural understandings among disaster victims in the wake of a disaster can result in a rearrangement of the social hierarchy, leading to less inhibited and mutually supportive interaction between different social groups, with the development of a “post-disaster culture” strengthening social functioning through collective resiliency (Rajkumar, Premkumar, & Tharyan, 2008).
The relevance of family in preserving social functioning after a disaster has been demonstrated in this review as well. In the study by Cao et al (2) in China, positive family functioning perceived by bereaved parents was associated with reduced depression symptoms. The impact of loss on parents was especially pronounced in the context of the one child Policy in China. The finding that bereaved parents who were having another baby reported higher family functioning indicates the role of familial resources as coping mechanism for grief and trauma. The other study by Cao et al (3) showed positive family functioning was related to less social and emotional loneliness.
Despite the six different conceptualisations of social functioning observed in this review, all share the common thread of relating to interpersonal interaction in daily life. While elements of interpersonal interaction are present in seemingly disparate thematic areas such as social adaption, family functioning, and functional impairment, they have yet to be unified under an umbrella term in the literature. The ICF represents a universally-endorsed conceptualization of functioning more broadly. Greater use of the specific ‘getting along’ domain within the validated WHODAS 2.0 could be used and developed in future studies on social functioning to introduce methodological consistency in the field.
There may also be a cyclical nature of poor mental health and functioning outcomes in contexts of crises. In the study by Radanovic-Grguric et al (15), depressed female refugees in Croatia with social adaptation difficulties resulting from war trauma became caught in a vicious cycle wherein their depression led to worse social adjustment, which exacerbated their depression. This is in contrast to female refugees who improved in their depression symptoms over two years, and enjoyed better social adjustment (15).
The overall evidence on associations between mental health and social functioning was extremely limited, with only 5 studies identified. Therefore, future studies investigating associations between social functioning and mental health are urgently required, particularly longitudinal studies examining temporal relationships and experimental and quasi-experimental studies investigating effectiveness of interventions addressing both mental health and social functioning outcomes.
The review findings also indicate a possible pathway in which a crisis interferes with a person’s daily routine and consequently their related functional processes. The study by Pat-Horenczyk et al (13) on schoolchildren in the West Bank suggests that the greater disruption faced by Palestinian students in their daily routines due to road blocks and school closures led to higher functional impairment than the Israeli students who faced less disruption. This is in line with previous findings that maintaining daily routine is protective for functional impairment (Pat-Horenczyk, Schiff, & Doppelt, 2006). Displacement appears especially disruptive. In the study by Van Griensven et al (19) of tsunami-affected individuals in Thailand, mean social functioning scores were lower for displaced compared with non-displaced participants. Additionally, Radanovic-Grguric (15) observed that greater time in displacement was associated with communication difficulties, lower social interest, and lower social compliance among Croatian refugees.
Limitations
Only one person screened and extracted the data which increases the likelihood of selection and appraisal bias. To avoid searching errors, the search strategy was developed and conducted in consultation with a systematic review librarian and systematic review researchers. Two reviewers did independently conduct the quality review. The study also only used descriptive analysis, as the limited number of studies and heterogeneous outcomes precluded conducting a meta-analysis. English language restrictions were used which resulted in 2 Chinese language studies being excluded at the full-text review stage. One related to an earthquake in Sichuan, China (Hu, Li, Jiang, Li, & Dou, 2012) which was also covered by the two studies from China in this review (2,3). The other (Cui, 2013) made no mention of social functioning as defined in this review.
The exclusion of studies explicitly assessing social support in humanitarian crisis settings could be seen as a limitation as it overlaps with social functioning. The construct of social support is not well understood, and while certain of its dimensions have been linked to social functioning, others have been linked with different health outcomes leading to much uncertainty as to how to measure the construct (Bloom & Spiegel, 1984). However, the literature suggests that social support and social functioning are distinct constructs, with social support having the potential to impact developmental processes which influence social functioning (Uchino, 2006).
Another limitation of this study concerns the cross-sectional nature of the majority of included studies. As causal pathways cannot be established through cross-sectional designs, the associations between social functioning and mental health outcomes can only be deemed correlational. Future quantitative studies employing generic measures of social functioning such as the relevant subscales of the full WHODAS 2.0 would enable more systematic comparisons, including greater use of meta-analyses.
The exclusion of studies employing single item measures of social functioning could be viewed as a limitation. However, they were excluded as it is unclear how successfully they can be applied for assessing multiple social, physical and psychological dimensions such as social functioning (Kaplan & Baron-Epel, 2003; Mavaddat, Kinmonth, Sanderson, Surtees, Bingham, & Khaw, 2011).
Although a broad search strategy was employed and leading grey literature sources were used, local grey literature may have been missed as access for research in LMICs to publication channels can be limited due to barriers such as lack of research training, difficulty writing in a foreign language, and lack of access to lack of access to journals and databases (WHO, 2004).
Conclusions
Social functioning is an important component of well-being. Reduced social functioning appears associated with increased depression symptoms and greater exposure to crisis, while better social functioning may be fostered through familial and social resources and “post-disaster culture”. Interventions to promote social functioning may have far-reaching benefits, but the evidence-base is weak and no causal inferences can be made without longitudinal and experimental intervention studies.
Greater engagement with the construct of social functioning is also required, particularly to ensure culturally appropriate and validated constructs and measures are used. While conceptualisations of social functioning vary, all seem to relate to interpersonal interaction in daily life. A pragmatic approach could be to use the WHODAS 2.0 which has been widely used and validated in multiple countries and contexts. In summary, better recognising, measuring and addressing social functioning could help maximise the benefits of investing in mental health and psychosocial support for populations affected by humanitarian crises.
Supplementary Material
Role of the Funding Source
No funding was used for this research.
Footnotes
Disclaimer: The authors alone are responsible for the content and writing of the article. The views expressed are those of the authors and do not necessarily represent the views, policies, or decisions of their employers.
Conflicts of interest: the authors declare no conflicts of interest.
Final Selected Studies for systematic review
- 1).Babic-Banaszak A, Kovacic L, Kovacevic L, Vuletic G, Mujkic A, Ebling Z. Impact Of War On Health Related Quality Of Life In Croatia: Population Study. Croatian Medical Journal. 2002;43:396–402. [PubMed] [Google Scholar]
- 2).Cao X, Jiang X, Li X, Lo M, Li R. Family Functioning And Its Predictors Among Disaster Bereaved Individuals In China: Eighteen Months After The Wenchuan Earthquake. Plos One. 2013a;8 doi: 10.1371/journal.pone.0060738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3).Cao X, Jiang X, Li X, Lo MCJH, Li R, Dou X. Perceived Family Functioning And Depression In Bereaved Parents In China After The 2008 Sichuan Earthquake. Archives Of Psychiatric Nursing. 2013b;27:204–209. doi: 10.1016/j.apnu.2013.04.001. [DOI] [PubMed] [Google Scholar]
- 4).Ferren PM. Comparing Perceived Self-Efficacy Among Adolescent Bosnian And Croatian Refugees With And Without Posttraumatic Stress Disorder. Journal Of Traumatic Stress. 1999;12:405–420. doi: 10.1023/A:1024749118463. [DOI] [PubMed] [Google Scholar]
- 5).Kilic EZ, Ozguven HD, Sayil I. The Psychological Effects Of Parental Mental Health On Children Experiencing Disaster: The Experience Of Bolu Earthquake In Turkey. Family Process. 2003;42:485–495. doi: 10.1111/j.1545-5300.2003.00485.x. [DOI] [PubMed] [Google Scholar]
- 6).Lopes Cardozo B, Bilukha OO, Gotway CA, Wolfe MI, Gerber ML, Anderson M. Mental Health Of Women In Postwar Afghanistan. Journal Of Women's Health. 2005;14:285–293. doi: 10.1089/jwh.2005.14.285. [DOI] [PubMed] [Google Scholar]
- 7).Lopes Cardozo B, Bilukha OO, Gotway Crawford CA, Shaikh I, Wolfe MI, Gerber ML, Anderson M. Mental Health, Social Functioning, And Disability In Postwar Afghanistan. Journal Of The American Medical Association. 2004a;292:575–584. doi: 10.1001/jama.292.5.575. [DOI] [PubMed] [Google Scholar]
- 8).Lopes Cardozo B, Kaiser R, Gotway CA, Agani F. Mental Health, Social Functioning, And Feelings Of Hatred And Revenge Of Kosovar Albanians One Year After The War In Kosovo. Journal Of Traumatic Stress. 2003;16:351–360. doi: 10.1023/A:1024413918346. [DOI] [PubMed] [Google Scholar]
- 9).Lopes Cardozo B, Talley L, Burton A, Crawford C. Karenni Refugees Living In Thai-Burmese Border Camps: Traumatic Experiences, Mental Health Outcomes, And Social Functioning. Social Science & Medicine. 2004b;58:2637–44. doi: 10.1016/j.socscimed.2003.09.024. [DOI] [PubMed] [Google Scholar]
- 10).Lopes Cardozo B, Vergara A, Agani F, Gotway CA. Mental Health, Social Functioning, And Attitudes Of Kosovar Albanians Following The War In Kosovo. Journal Of The American Medical Association. 2000;284:569–577. doi: 10.1001/jama.284.5.569. [DOI] [PubMed] [Google Scholar]
- 11).Massad SG, Nieto FJ, Palta M, Smith M, Clark R, Thabet AAM. Health-Related Quality Of Life Of Palestinian Preschoolers In The Gaza Strip: A Cross-Sectional Study. Bmc Public Health. 2011;11 doi: 10.1186/1471-2458-11-253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12).Norris FH, Baker CK, Murphy AD, Kaniasty K. Social Support Mobilization And Deterioration After Mexico's 1999 Flood: Effects Of Context, Gender, And Time. American Journal Of Community Psychology. 2005;36:15–28. doi: 10.1007/s10464-005-6230-9. [DOI] [PubMed] [Google Scholar]
- 13).Pat-Horenczyk R, Qasrawi R, Lesack R, Haj-Yahia M, Peled O, Shaheen M, Berger R, Brom D, Garber R, Abdeen Z. Posttraumatic Symptoms, Functional Impairment, And Coping Among Adolescents On Both Sides Of The Israeli Palestinian Conflict: A Cross-Cultural Approach. Applied Psychology: An International Review. 2009;58:688–708. [Google Scholar]
- 14).Peltonen K, Qouta S, El Sarraj E, Punamäki R-L. Effectiveness Of School-Based Intervention In Enhancing Mental Health And Social Functioning Among War-Affected Children. Traumatology. 2012;18:37–46. [Google Scholar]
- 15).Radanovic-Grguric L, Barkic J, Filakovic P, Koic O, Laufer D, Petek A, Mandic N. The Impact Of Displacement On The Expression Of Depressive Disorder And Social Functioning Among The War Refugees. Psychiatria Danubina. 2009;21:474–482. [PubMed] [Google Scholar]
- 16).Talbot A, Uwihoreye C, Kamen C, Grant P, Mcglynn L, Mugabe I, Nshimyumukiza M, Dongier P, Slamowitz D, Padilla C, Uvamahoro J, et al. Treating Psychological Trauma Among Rwandan Orphans Is Associated With A Reduction In Hiv Risk-Taking Behaviors: A Pilot Study. Aids Education & Prevention. 2013;25:468–79. doi: 10.1521/aeap.2013.25.6.468. [DOI] [PubMed] [Google Scholar]
- 17).Tuicomepee A, Romano JL. Thai Adolescent Survivors 1 Year After The 2004 Tsunami: A Mixed Methods Study. Journal Of Counseling Psychology. 2008;55:308–320. [Google Scholar]
- 18).Usta J, Farver J. Child Sexual Abuse In Lebanon During War And Peace. Child: Care, Health And Development. 2010;36:361–368. doi: 10.1111/j.1365-2214.2010.01082.x. [DOI] [PubMed] [Google Scholar]
- 19).Van Griensven F, Chakkraband M, Thienkrua W, Pengjuntr W, Cardozo BL, Tantipiwatanaskul P, Mock PA, Ekassawin S, Varangrat A, Gotway C, Sabin M, et al. Mental Health Problems Among Adults In Tsunami-Affected Areas In Southern Thailand. Jama: Journal Of The American Medical Association. 2006;296:537–548. doi: 10.1001/jama.296.5.537. [DOI] [PubMed] [Google Scholar]
- 20).Wickrama K, Wickrama T. Perceived Community Participation In Tsunami Recovery Efforts And The Mental Health Of Tsunami-Affected Mothers: Findings From A Study In Rural Sri Lanka. International Journal Of Social Psychiatry. 2011;57:518–527. doi: 10.1177/0020764010374426. [DOI] [PubMed] [Google Scholar]
Cited References
- Andermann LF. Cultural aspects of trauma. Canadian Psychiatric Association Bulletin. 2002;34(4) [Google Scholar]
- Armstrong M, Birnie-Lefcovitch S, Ungar M. Pathways Between Social Support, Family Well Being, Quality of Parenting, and Child Resilience: What We Know. Journal of Child and Family Studies. 2005;14(2):269–281. doi: 10.1007/s10826-005-5054-4. [DOI] [Google Scholar]
- Blanchet K, Roberts B, Sistenich V, Ramesh A, Frison S, Warren E, Hossain M, Knight A, Lewis C, Smith J. An evidence review of research on health interventions in humanitarian crises. London: London School of Hygiene and Tropical Medicine/Harvard School of Public Health. 2013 [Google Scholar]
- Bloom JR, Spiegel D. The relationship of two dimensions of social support to the psychological well-being and social functioning of women with advanced breast cancer. Social Science & Medicine. 1984;19(8):831–837. doi: 10.1016/0277-9536(84)90400-3. [DOI] [PubMed] [Google Scholar]
- Burns T, Patrick D. Social functioning as an outcome measure in schizophrenia studies. Acta Psychiatr Scand. 2007;116(6):403–418. doi: 10.1111/j.1600-0447.2007.01108.x. [DOI] [PubMed] [Google Scholar]
- Cooper A, Michels R. Diagnostic and Statistical Manual of Mental Disorders, revised (DSM-III-R) American Journal of Psychiatry. 1988;145(10):1300–1301. [Google Scholar]
- Cui YH. [Psychological trauma and crisis intervention in children after earthquake] Zhongguo Dang Dai Er Ke Za Zhi. 2013;15(6):423–426. [PubMed] [Google Scholar]
- de Jong JTVM, Komproe IH, Van Ommeren M. Common mental disorders in postconflict settings. The Lancet. 2003;361(9375):2128–2130. doi: 10.1016/S0140-6736(03)13692-6. [DOI] [PubMed] [Google Scholar]
- De Silva MJ, Cooper S, Li HL, Lund C, Patel V. Effect of psychosocial interventions on social functioning in depression and schizophrenia: meta-analysis. Br J Psychiatry. 2013;202(4):253–260. doi: 10.1192/bjp.bp.112.118018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deeks JJ, Dinnes J, D'Amico R, Sowden AJ, Sakarovitch C, Song F, Petticrew M, Altman DG, International Stroke Trial Collaborative G, European Carotid Surgery Trial Collaborative G Evaluating non-randomised intervention studies. Health Technol Assess. 2013;7(27):iii–x. doi: 10.3310/hta7270. 1–173. [DOI] [PubMed] [Google Scholar]
- Goldman HH, Skodol AE, Lave TR. Revising axis V for DSM-IV: a review of measures of social functioning. Am J Psychiatry. 1992;149(9):1148–1156. doi: 10.1176/ajp.149.9.1148. [DOI] [PubMed] [Google Scholar]
- Hays RD, Wells KB, Sherbourne C, Rogers W, Spritzer K. FUnctioning and well-being outcomes of patients with depression compared with chronic general medical illnesses. Archives of General Psychiatry. 1995;52(1):11–19. doi: 10.1001/archpsyc.1995.03950130011002. [DOI] [PubMed] [Google Scholar]
- Herzog R, Alvarez-Pasquin MJ, Diaz C, Del Barrio JL, Estrada JM, Gil A. Are healthcare workers' intentions to vaccinate related to their knowledge, beliefs and attitudes? A systematic review. BMC Public Health. 2013;13:154. doi: 10.1186/1471-2458-13-154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins JP, Green S. Cochrane handbook for systematic reviews of interventions. Vol. 5. Wiley Online Library; 2008. [Google Scholar]
- Hirschfeld RM, Montgomery SA, Keller MB, Kasper S, Schatzberg AF, Moller HJ, Healy D, Baldwin D, Humble M, Versiani M, Montenegro R, et al. Social functioning in depression: a review. J Clin Psychiatry. 2000;61(4):268–275. doi: 10.4088/jcp.v61n0405. [DOI] [PubMed] [Google Scholar]
- Hu XL, Li XL, Jiang XL, Li R, Dou XM. [Family function and depression in relatives of earthquake victims: a survey conducted one year after China's Wenchuan Earthquake] Hu Li Za Zhi. 2012;59(5):57–67. doi: 10.6224/jn.59.5.57. [DOI] [PubMed] [Google Scholar]
- Jones L, Asare J, Elmasri M, Mohanraj A. Mental health in disaster settings. 2007;335 doi: 10.1136/bmj.39329.580891.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaplan G, Baron-Epel O. What lies behind the subjective evaluation of health status? Soc Sci Med. 2003;56(8):1669–1676. doi: 10.1016/s0277-9536(02)00179-x. [DOI] [PubMed] [Google Scholar]
- Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JPA, Clarke M, Devereaux PJ, Kleijnen J, Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. 2009;339 doi: 10.1136/bmj.b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJ. Global and regional burden of disease and risk factors, 2001: systematic analysis of population health data. Lancet. 2006;367(9524):1747–1757. doi: 10.1016/S0140-6736(06)68770-9. [DOI] [PubMed] [Google Scholar]
- Mavaddat N, Kinmonth AL, Sanderson S, Surtees P, Bingham S, Khaw KT. What determines Self-Rated Health (SRH)? A cross-sectional study of SF-36 health domains in the EPIC-Norfolk cohort. J Epidemiol Community Health. 2011;65(9):800–806. doi: 10.1136/jech.2009.090845. [DOI] [PubMed] [Google Scholar]
- Moussavi S, Chatterji S, Verdes E, Tandon A, Patel V, Ustun B. Depression, chronic diseases, and decrements in health: results from the World Health Surveys. Lancet. 2007;370(9590):851–858. doi: 10.1016/S0140-6736(07)61415-9. [DOI] [PubMed] [Google Scholar]
- Murray CJ, Lopez AD. The global burden of disease and injury series, volume 1: a comprehensive assessment of mortality and disability from diseases, injuries, and risk factors in 1990 and projected to 2020. Cambridge. MA: 1996. [Google Scholar]
- Neria Y, Nandi A, Galea S. Post-traumatic stress disorder following disasters: a systematic review. Psychological Medicine. 2008;38(04):467–480. doi: 10.1017/S0033291707001353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pat-Horenczyk R, Schiff M, Doppelt O. Maintaining routine despite ongoing exposure to terrorism: a healthy strategy for adolescents? J Adolesc Health. 2006;39(2):199–205. doi: 10.1016/j.jadohealth.2005.11.021. [DOI] [PubMed] [Google Scholar]
- Patel V, Araya R, Chatterjee S, Chisholm D, Cohen A, De Silva M, Hosman C, McGuire H, Rojas G, van Ommeren M. Treatment and prevention of mental disorders in low-income and middle-income countries. Lancet. 2007a;370(9591):991–1005. doi: 10.1016/S0140-6736(07)61240-9. [DOI] [PubMed] [Google Scholar]
- Patel V, Araya R, Chatterjee S, Chisholm D, Cohen A, De Silva M, Hosman C, McGuire H, Rojas G, van Ommeren M. Treatment and prevention of mental disorders in low-income and middle-income countries. The Lancet. 2007b;370(9591):991–1005. doi: 10.1016/S0140-6736(07)61240-9. [DOI] [PubMed] [Google Scholar]
- Porter M, Haslam N. Predisplacement and postdisplacement factors associated with mental health of refugees and internally displaced persons: A meta-analysis. JAMA. 2005;294(5):602–612. doi: 10.1001/jama.294.5.602. [DOI] [PubMed] [Google Scholar]
- Rajkumar AP, Premkumar TS, Tharyan P. Coping with the Asian tsunami: perspectives from Tamil Nadu, India on the determinants of resilience in the face of adversity. Soc Sci Med. 2008;67(5):844–853. doi: 10.1016/j.socscimed.2008.05.014. [DOI] [PubMed] [Google Scholar]
- Roberts B, Browne J. A systematic review of factors influencing the psychological health of conflict-affected populations in low- and middle-income countries. Glob Public Health. 2011;6(8):814–829. doi: 10.1080/17441692.2010.511625. [DOI] [PubMed] [Google Scholar]
- Ross CE, Mirowsky J. Neighborhood Disadvantage, Disorder, and Health. Journal of Health and Social Behavior. 2001;42(3):258–276. doi: 10.2307/3090214. [DOI] [PubMed] [Google Scholar]
- Steel Z, Chey T, Silove D, Marnane C, Bryant RA, van Ommeren M. Association of torture and other potentially traumatic events with mental health outcomes among populations exposed to mass conflict and displacement: A systematic review and meta-analysis. JAMA. 2009;302(5):537–549. doi: 10.1001/jama.2009.1132. [DOI] [PubMed] [Google Scholar]
- Steel Z, Silove D, Phan T, Bauman A. Long-term effect of psychological trauma on the mental health of Vietnamese refugees resettled in Australia: a population-based study. The Lancet. 2002;360(9339):1056–1062. doi: 10.1016/S0140-6736(02)11142-1. [DOI] [PubMed] [Google Scholar]
- Tol WA, Barbui C, Galappatti A, Silove D, Betancourt TS, Souza R, Golaz A, van Ommeren M. Mental health and psychosocial support in humanitarian settings: linking practice and research. The Lancet. 2011;378(9802):1581–1591. doi: 10.1016/S0140-6736(11)61094-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uchino BN. Social support and health: a review of physiological processes potentially underlying links to disease outcomes. J Behav Med. 2006;29(4):377–387. doi: 10.1007/s10865-006-9056-5. [DOI] [PubMed] [Google Scholar]
- UNOCHA. World Humanitarian Data and Trends 2013. Geneva: United Nations Office for the Coordination of Humanitarian Affairs; 2013. [Google Scholar]
- Ustun TB, Kostanjsek N, Chatterji S, Rehm J, editors. Measuring health and disability. Manual for the WHO Disability Assessment Schedule WHODAS 2.0. Geneva: World Health Organization; 2010. [Google Scholar]
- Wells GA, S B, O'Connell D, Peterson J, Welch V, Losos M, Tugwell P. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. 2014 from http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp.
- WHO. The International Classification of Functioning, Disability and Health. Geneva: World Health Organization; 2001a. [Google Scholar]
- WHO. The International Classification Of Functioning, Disability And Health. Geneva: World Health Organization; 2001b. [Google Scholar]
- WHO. Galvanising mental health research in low and middle-income countries: the role of scientific journals. Acta Psychiatr Scand. 2004;110(1):77–79. doi: 10.1111/j.1600-0447.2004.00318.x. Joint Statement by Editors. [DOI] [PubMed] [Google Scholar]
- WHO. Building Back Better: Sustainable Mental Health Care after Emergencies. Geneva: World Health Organization; 2013. [Google Scholar]
- World Bank. How Does the World Bank Classify Countries? 2014 Retrieved July 1, 2014, from https://datahelpdesk.worldbank.org/knowledgebase/articles/378834-how-does-the-world-bank-classify-countries.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.