Abstract
In recent years, the search for a less invasive and thus, less painful approach has driven technical innovation in modern thoracic surgery. In this context, subxiphoid uniportal approach has emerged as an alternative to avoid intercostal space manipulation and decrease postoperative pain and intercostal nerve chronic impairment. Subxiphoid uniportal major lung resections have been safe and effective procedures when performed by experienced surgeons even in complex cases or unexpected intraoperative situations. We present six of these surgical scenarios such as big tumors, incomplete or absent fissures, hilar calcified lymph nodes, active bleeding and massive adhesions to show the feasibility of subxiphoid approach to manage even these conditions.
Keywords: Subxiphoid VATS, uniportal video-assisted thoracic surgery (uniportal VATS), minimally invasive thoracic surgery (MITS)
Introduction
Adoption of video-assisted thoracic surgery (VATS) as the standard approach for major lung resections has been the quantum leap of modern thoracic surgery. Minimally invasive procedures offer today unprecedented outcomes in morbidity and patient comfort (1).
Conversely, this technique has been continuously evolving as surgeons push the boundaries to cause no postoperative pain at all by reducing the number of intercostal spaces involved (2). Uniportal VATS lobectomy is considered a safe and effective approach for major and even complex lung resections, but some degree of chronic pain and chest wall numbness is still present.
In 2014 Liu et al. performed the first uniportal subxiphoid VATS left upper lobectomy (3) with the aim to avoid pain related to the aggression of intercostal nerves. Recent observational studies showed that subxiphoid approach is a safe and feasible procedure for early-stage lung cancer (4), significantly relieves postoperative incision pain and is also useful for the treatment of bilateral pathology (5).
In this paper we report some of our experience with complex surgical situations managed by uniportal subxiphoid approach such as big tumors, incomplete or absent fissures, hilar calcified lymph nodes, control of active bleeding and massive adhesions.
Patients and workup
All six procedures were done in high volume institutions by the same experienced surgeon. The lesions were confirmed or highly suspected malignant lung tumors. Four complex uniportal subxiphoid VATS major resections (fissureless left upper lobectomy, middle lobectomy, left lower lobectomy with uncomplete fissure, and right upper lobectomy for big size tumor with tracheal bronchus) were included beside two difficult intraoperative situations that can be resolved with this approach (massive adhesions in left upper lobectomy and bleeding control).
Procedure
Under general anesthesia and double-lumen endotracheal tube the patients were positioned in a lateral position inclined at 60–70° to allow better access and view of the anterior mediastinum. A single 3–4 cm incision was made over the subxiphoid area to allow access to the thoracic cavity by a subcostal tunnel. The xiphoid process was cut and the pericardial fatty tissue was removed to avoid interference with instruments. Energy devices were used alongside special double-hinged, longer than regular, angulated instruments to perform dissection. Longer Endoscopic staplers were used for vascular lobar branches and bronchial stapling. Smaller vessels were ligated with polymer clips by using a 45° uniportal specific applier. The specimen was routinely extracted with a retrieval bag.
In the first case, left upper lobectomy was performed trough a left subcostal incision to minimize the chance of the heart to move the instruments. Fissure was incomplete so we decided to perform a fissureless resection (Figure 1). After transecting left upper pulmonary vein, carina between upper and lower lobe bronchi is defined (Figure 2). Pulmonary artery is identified over the bronchial plane and fissure can be divided anteriorly with the anvil of the stapler pointing over the artery. This step allows us to dissect the bronchus, which is transected protecting the lingular branch with the sucker (suction device trick) (Figure 3). Lingular artery is exposed after cutting the bronchus and is transected. The fissure is then completed posteriorly with staplers.
Figure 1.
Uniportal subxiphoid VATS fissureless left upper lobectomy (6). VATS, video-assisted thoracic surgery. Available online: http://www.asvide.com/articles/1598
Figure 2.
Pulmonary artery can be identified behind the carina between upper and lower bronchi.
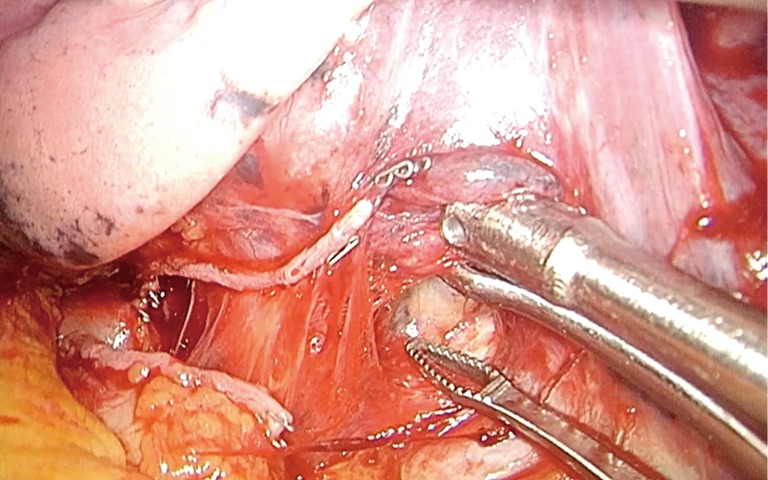
Figure 3.
Suction device can be used for both protecting the lingular branch and opening the pathway for the stapler.
In the second case, a subxiphoid middle lobectomy was performed (Figure 4). Bronchus and artery for the middle lobe were surrounded by calcified lymph nodes. After careful and difficult dissection, bronchus was dissected and divided. Middle lobe artery was very risky to separate from the calcified lymph nodes (Figure 5), so we retracted the lymph nodes to use a stapler to complete the fissure including the artery (Figure 6).
Figure 4.
Uniportal subxiphoid VATS middle lobectomy (7). VATS, video-assisted thoracic surgery. Available online: http://www.asvide.com/articles/1599
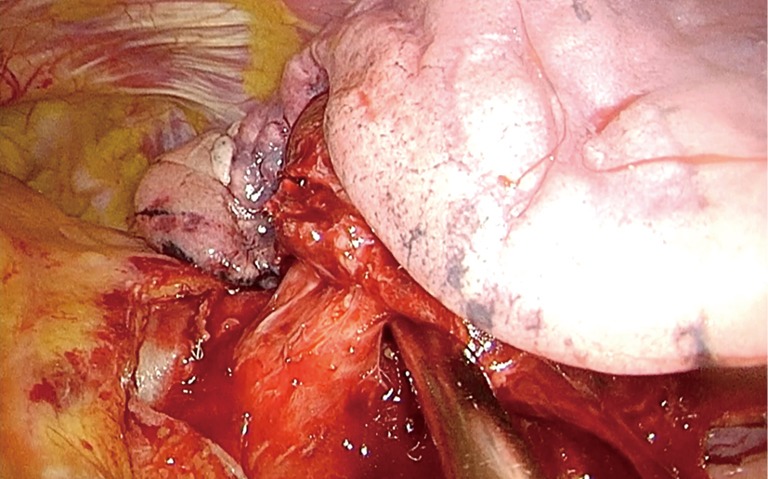
Figure 5.
Calcified lymph nodes were blocking the plane between the bronchial stump and the middle lobe artery.
Figure 6.
A stapler was used to divide the fissure and the middle lobe artery after lifting the lymph nodes as much as possible.
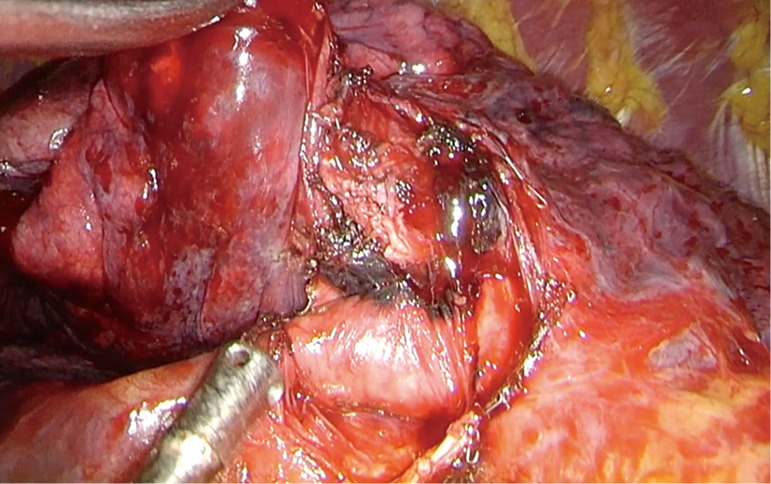
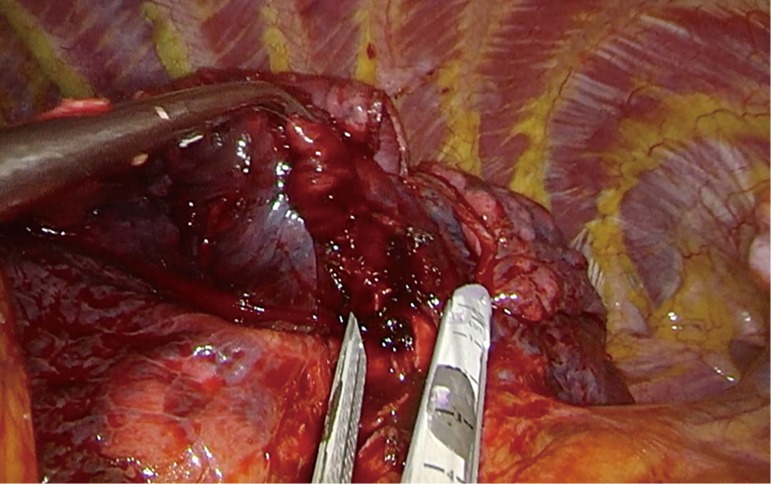
In the third case, uncomplete fissure was found while performing a left lower lobectomy (Figure 7). It is important to notice that in this lobectomy, space is more limited because of the proximity of the heart. Left inferior vein is divided after cutting the pulmonary ligament. In this point, bronchus can also be transected, but we preferred to expose the pulmonary artery first. Dissecting over the carina between upper and lower lobe bronchus, artery is identified (Figure 8) and fissure is divided anteriorly aiming the anvil of the stapler over the vessel (Figure 9). This maneuver is repeated if needed. Once the artery is fully exposed, lower lobectomy is completed with the usual operative steps.
Figure 7.
Uniportal subxiphoid VATS left lower lobectomy with uncomplete fissure (8). VATS, video-assisted thoracic surgery. Available online: http://www.asvide.com/articles/1600
Figure 8.
Once the artery is identified, a tunnel over it can be made to safely place the stapler.
Figure 9.
The anvil of the stapler is placed in the plane over the artery and below the parenchyma.
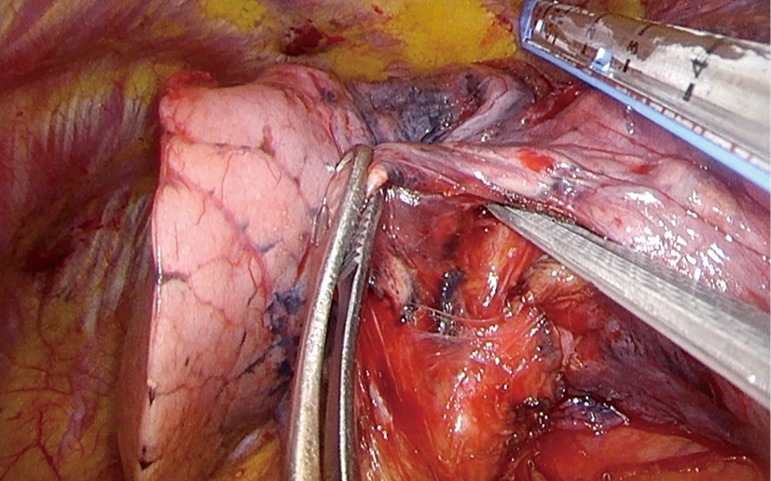
In the fourth case, right upper lobectomy was performed for a big mass with strong adhesions and abnormal anatomy (Figure 10). A tracheal bronchus for the apical segment was diagnosed preoperatively in both the CT scan and bronchoscopy (Figure 11). A combination of blunt and sharp dissection was needed to liberate the right upper lobe from the chest wall (Figure 12). Mediastinal pleura was opened beside a phrenic nerve lymph node and artery, vein and tracheal bronchus were exposed and divided. Station eleven lymph nodes were lifted to gain access to the origin of the remaining right upper bronchus and lobectomy was completed with the usual operative steps. The apical and posterior-anterior trunk of bronchus were divided individually.
Figure 10.
Uniportal subxiphoid VATS right upper lobectomy for big size tumor with tracheal bronchus (9). VATS, video-assisted thoracic surgery. Available online: http://www.asvide.com/articles/1601
Figure 11.
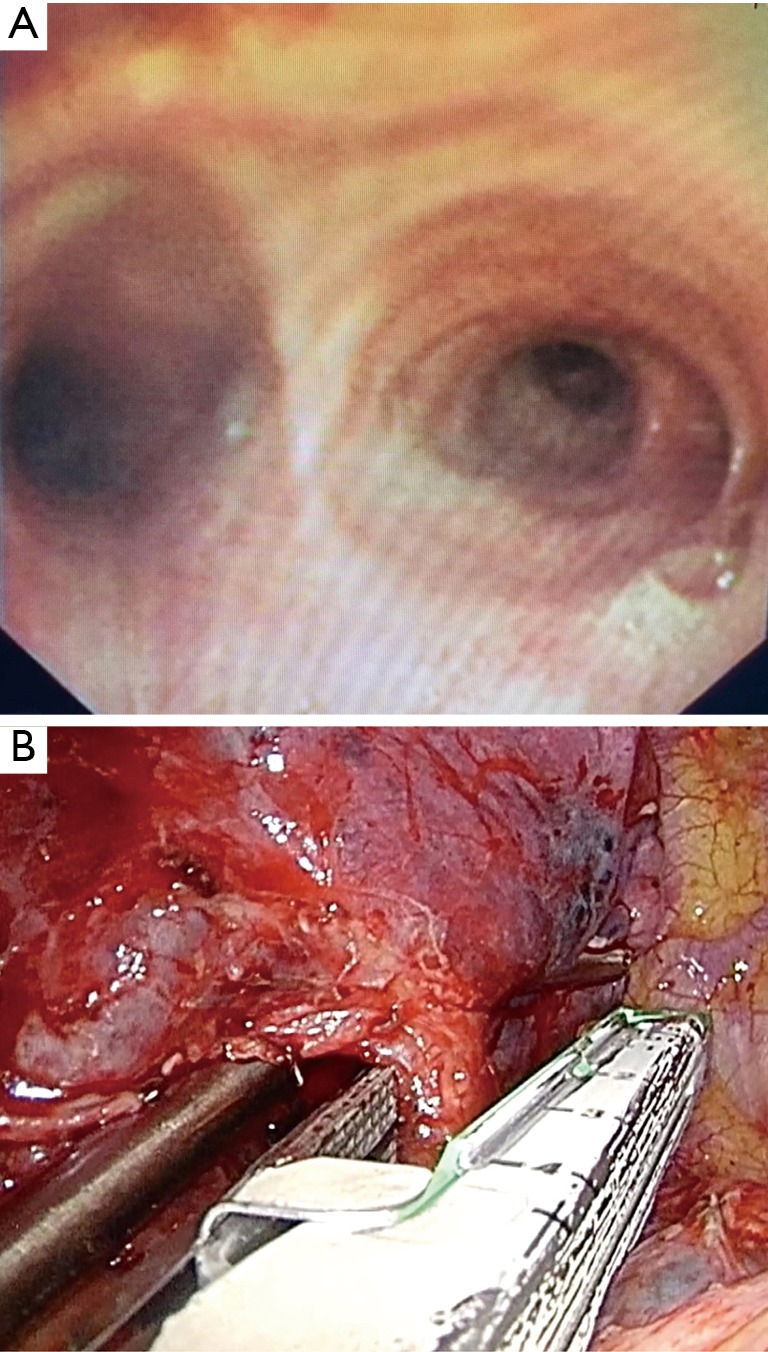
Bronchoscopic (A) and intraoperative view (B) of the tracheal bronchus.
Figure 12.
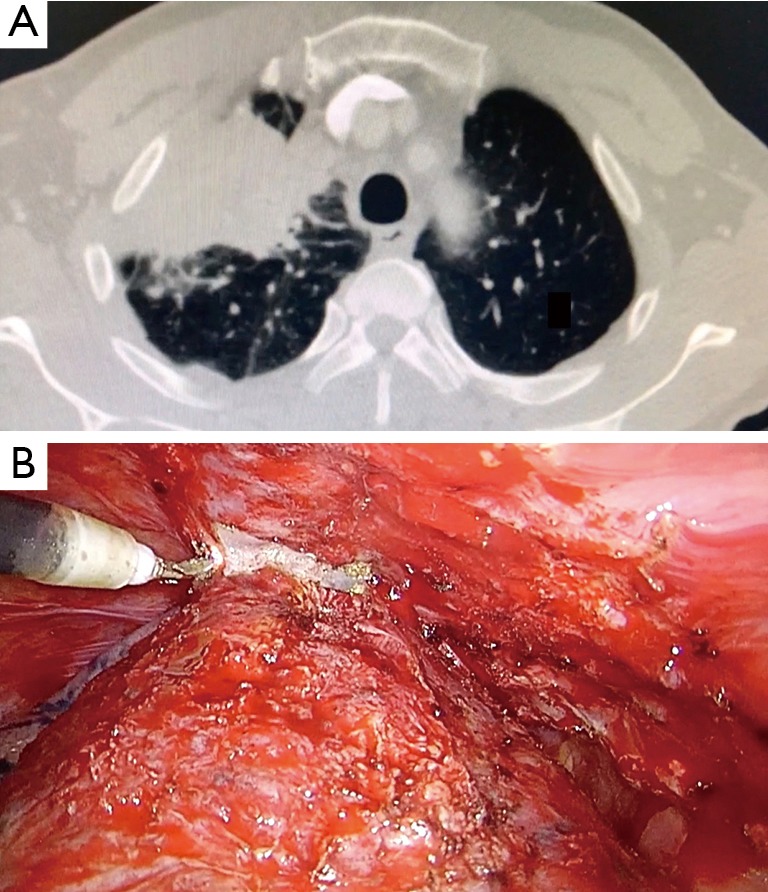
CT scan of the mass (A) and intraoperative view (B) of adhesions that require the use of the electrocautery to be liberated.
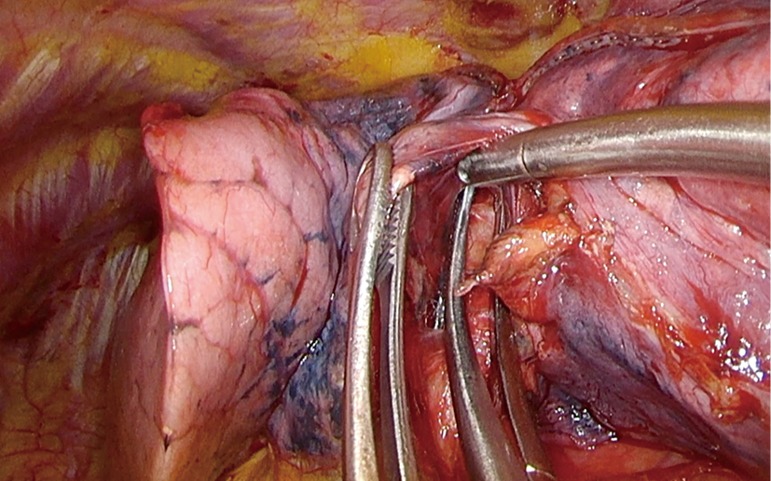
In the fifth case, uniportal left upper lobectomy was performed despite extensive adhesions (Figure 13). Lung could be completely liberated combining blunt and sharp dissection using only two instruments at a time (Figure 14). Sucker was used for dissection, aspiration and traction. Long curved electrocautery was used to dissect and cut in the vicinity of the chest wall and an energy device was used when near the mediastinum and hilar structures.
Figure 13.

Uniportal subxiphoid VATS approach for massive adhesions in left upper lobectomy (10). VATS, video-assisted thoracic surgery. Available online: http://www.asvide.com/articles/1602
Figure 14.
Sucker is used for traction, dissection and aspiration allowing us to have only two instruments trough the incision.
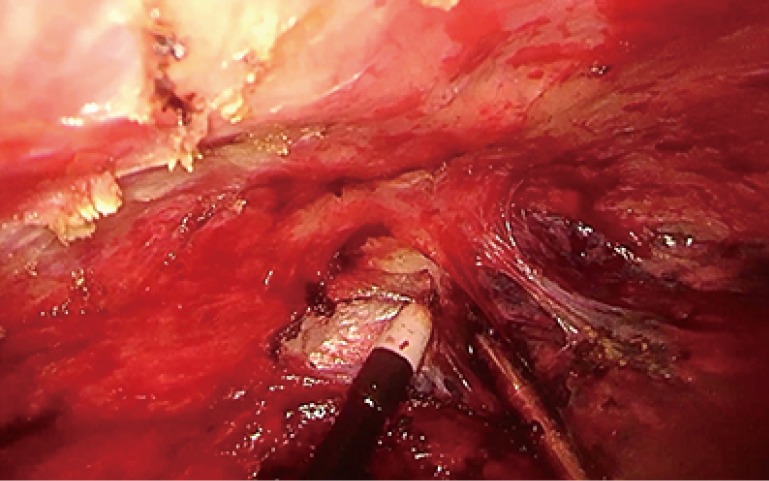
In the sixth case, bleeding occurred during right upper lobectomy and was safely controlled maintaining subxiphoid approach (Figure 15). A 3/0 non-absorbable monofilament suture was used to give a u-shaped stitch around the vascular tear (Figure 16).
Figure 15.
Uniportal subxiphoid VATS bleeding control (11). VATS, video-assisted thoracic surgery. Available online: http://www.asvide.com/articles/1603
Figure 16.
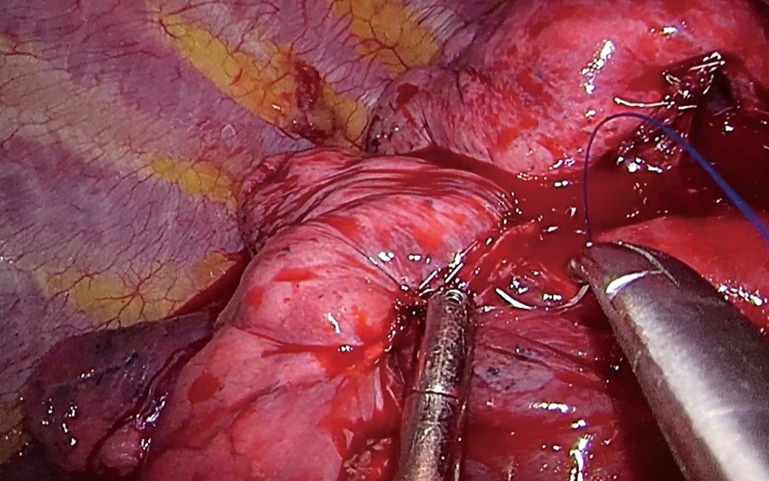
3/0 non-absorbable monofilament suture is used while providing exposure with the sucker.
Discussion
The uniportal subxiphoid approach is a novel technique initially described in 2014 with the aim to reduce the risk of intercostal nerve injury and paraesthesia, avoiding the intercostal space (3).
Due to the vision is more limited than transthoracic approach, the assistant has to be very focused in using the proper angulation of the camera to show clearly the structures the surgeon is dissecting. The assistant can also provide aid with retraction of the lung with another instrument, so that the surgeon can use bimanual instrumentation in the dissection process.
The previous experience in Uniportal VATS major pulmonary resections and a skilled assistant are mandatory requirements to performed subxiphoid resections especially when dealing with difficult cases (12). As it happens with the transthoracic uniportal approach, bimanual instrumentation is crucial to achieve a good anatomic hilar dissection through a single subxiphoid incision. The view is caudal-cranial and anterior to posterior, so the access for the view of the posterior mediastinum is difficult, resulting in the need for the lung requiring more traction to assess the lesions in this area. The complete dissection of the subcarinal lymph nodes is more difficult to accomplish than transthoracic approach, especially on the left side (13). When a bleeding is difficult to control by this approach, an extension of the subxiphoid incision is unlikely to be useful so an additional thoracic port must be performed (3–4 cm utility incision).
On the left side, the instrumentation over a beating heart is more challenging, so extra care must be taken to avoid arrhythmias or other kind of cardiac complications.
We strongly believe this novel approach has potential for widespread use after developing of new technology, wireless cameras, magnetic graspers, more angulated instruments and single port robotic technology adapted through the subxiphoid approach (14).
Further studies are necessary to compare clinical outcomes of the subxiphoid versus other transthoracic approaches, in order to show clear advantages from this technique.
Conclusions
Uniportal subxiphoid VATS approach for major pulmonary resections is a safe and feasible procedure for complex resections, even when technically challenging difficulties arise during the procedure. However, these procedures must only be performed by skilled and experienced surgeons with the technique.
Acknowledgements
None.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.Paul S, Altorki NK, Sheng S, et al. Thoracoscopic lobectomy is associated with lower morbidity than open lobectomy: a propensity-matched analysis from the STS database. J Thorac Cardiovasc Surg 2010;139:366-78. 10.1016/j.jtcvs.2009.08.026 [DOI] [PubMed] [Google Scholar]
- 2.Gonzalez D, Paradela M, Garcia J, et al. Single-port video-assisted thoracoscopic lobectomy. Interact Cardiovasc Thorac Surg 2011;12:514-5. 10.1510/icvts.2010.256222 [DOI] [PubMed] [Google Scholar]
- 3.Liu CC, Wang BY, Shih CS, et al. Subxiphoid single-incision thoracoscopic left upper lobectomy. J Thorac Cardiovasc Surg 2014;148:3250-1. 10.1016/j.jtcvs.2014.08.033 [DOI] [PubMed] [Google Scholar]
- 4.Song N, Zhao DP, Jiang L, et al. Subxiphoid uniportal video-assisted thoracoscopic surgery (VATS) for lobectomy: a report of 105 cases. J Thorac Dis 2016;8:S251-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hernandez-Arenas LA, Lin L, Yang Y, et al. Initial experience in uniportal subxiphoid video-assisted thoracoscopic surgery for major lung resections. Eur J Cardiothorac Surg 2016;50:1060-6. 10.1093/ejcts/ezw189 [DOI] [PubMed] [Google Scholar]
- 6.Gonzalez-Rivas D, Lirio F, Sesma J, et al. Uniportal subxiphoid VATS fissureless left upper lobectomy. Asvide 2017;4:289. Available online: http://www.asvide.com/articles/1598
- 7.Gonzalez-Rivas D, Lirio F, Sesma J, et al. Uniportal subxiphoid VATS middle lobectomy. Asvide 2017;4:290. Available online: http://www.asvide.com/articles/1599
- 8.Gonzalez-Rivas D, Lirio F, Sesma J, et al. Uniportal subxiphoid VATS left lower lobectomy with uncomplete fissure. Asvide 2017;4:291. Available online: http://www.asvide.com/articles/1600
- 9.Gonzalez-Rivas D, Lirio F, Sesma J, et al. Uniportal subxiphoid VATS right upper lobectomy for big size tumor with tracheal bronchus. Asvide 2017;4:292. Available online: http://www.asvide.com/articles/1601
- 10.Gonzalez-Rivas D, Lirio F, Sesma J, et al. Uniportal subxiphoid VATS approach for massive adhesions in left upper lobectomy. Asvide 2017;4:293. Available online: http://www.asvide.com/articles/1602
- 11.Gonzalez-Rivas D, Lirio F, Sesma J, et al. Uniportal subxiphoid VATS bleeding control. Asvide 2017;4:294. Available online: http://www.asvide.com/articles/1603
- 12.Gonzalez-Rivas D, Yang Y, Lei J, et al. Subxiphoid uniportal video-assisted thoracoscopic middle lobectomy and anterior anatomic segmentectomy (S3). J Thorac Dis 2016;8:540-3. 10.21037/jtd.2016.02.63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Guido Guerrero W, Hernandez Arenas LA, Jiang G, et al. Subxiphoid mediastinal lymphadenectomy. J Vis Surg 2016;2:105 10.21037/jovs.2016.05.05 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gonzalez-Rivas D, Yang Y, Calvin NG. Advances in uniportal surgery: pushing the envelope. Thorac Surg Clin 2016;26:187-201. 10.1016/j.thorsurg.2015.12.007 [DOI] [PubMed] [Google Scholar]


