The hamstring muscles and tendons are the most commonly injured muscle group in athletes.11,15,20,28 The hamstring tendons are particularly vulnerable to injuries, as they cross 2 joints and have a high proportion of type 2 muscle fibers.17 They act mainly as decelerators of the leg, and as they work eccentrically, they are prone to excessive force in the muscle-tendon unit.17,18 Most hamstring injuries are strains occurring at the myotendinous junction.1,14,22 Injuries may involve proximal bone-tendon ruptures and, more rarely, distal bone-tendon avulsions.24 Distal avulsion injuries most frequently involve the biceps femoris and semitendinosus, with semimembranosus tendon injuries being very uncommon.14,24
Injuries at the myotendinous junction have been shown to have good outcomes with nonoperative treatment.1,10,21,25,34 The rate of hamstring reinjuries after conservative treatment, however, can be relatively high.9,28 Proximal tendon avulsion injuries have better outcomes with surgical interventions.6 The literature regarding distal tendon injuries is limited, but poor outcomes have been reported with conservative management and delayed surgery.27 The few reports on the surgical treatment of distal tears of the hamstring muscle consist mainly of biceps femoris tears.12,16,26,27,29,32 Reports of injuries to the distal semimembranosus tendon are even more scarce.3
The purpose of this study was to report the results of the successful acute surgical repair of a distal semimembranosus tendon avulsion in a professional rugby player with 18 months’ clinical follow-up. Institutional review board approval was obtained for this study.
Case Presentation
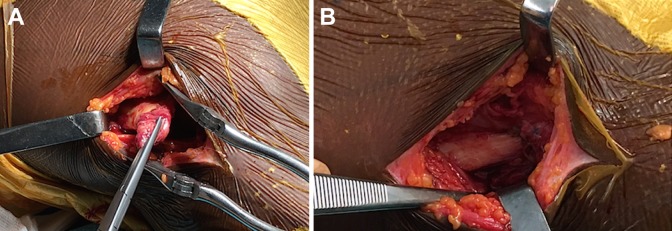
A 22-year-old male professional rugby player, with no history of injuries, was standing in a ruck with his hips flexed and knees extended. He was pushed backwards, causing knee hyperextension, and felt a sudden crack on the medial side of his thigh with immediate pain. The following day, the patient presented with posteromedial knee pain. On clinical examination of his knee, he had full range of motion and negative test findings for instability. Magnetic resonance imaging (MRI) showed an isolated complete rupture of the distal tendon of the semimembranosus muscle (Figure 1). After a discussion of the treatment options, the patient elected to undergo early surgical repair.
Figure 1.
A distal semimembranosus tendon rupture (red circle) on magnetic resonance imaging.
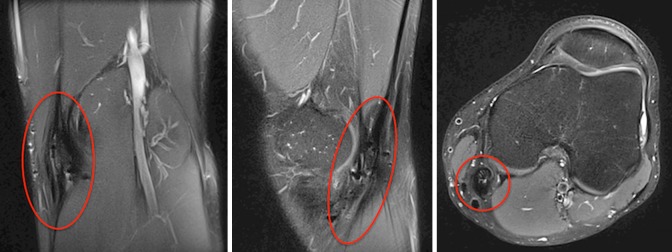
Surgery was performed 1 week after the injury. The position of the semimembranosus tendon was identified with ultrasound preoperatively and marked. The patient received general anesthesia and was positioned supine with a pillow under the knee. A longitudinal skin incision 5 cm in length was made at the level of the rupture in the posteromedial aspect of the knee, superior to the saphenous nerve and vein. After careful dissection, the distal tendon of the semimembranosus muscle was identified medial to the semitendinosus tendon (Figure 2A). A mark on the skin was made at the location of the lesion by the radiologist. Exploration confirmed a complete tendon rupture, with retraction of 1 to 2 cm. The bony bed was freshened to bleeding bone. The tendon was repaired to the bone with suture anchors (with nonresorbable No. 1 sutures). The sutures were passed through the hamstring tendons using a Krackow locking technique on one end and a sliding suture on the other end (Figure 2B).
Figure 2.
(A) The identification of a semimembranosus tendon rupture and (B) surgical repair to bone with suture anchors.
Postoperatively, the limb was immobilized with 20° of knee flexion for 4 days. A hinged knee brace was then applied to allow passive motion from 20° to 110°. This was increased to full range of motion at 6 weeks. Weightbearing was kept to 50% for the first 4 weeks and then was advanced to full weightbearing. Active movement without resistance was started at 4 weeks. At 2 months, resisted exercises were started with light jogging. The patient returned to full training at 4 months. At 4 months after surgery, isokinetic testing of the operated leg showed satisfactory concentric and eccentric function compared to the other leg (Table 1). The patient returned to competitive rugby at 5 months after surgery. At 18 months after surgery, the patient remained pain free without any noticeable strength deficit. He played 12 professional matches without any problems. MRI performed 18 months after surgery demonstrated satisfactory healing of the distal semimembranosus tendon (Figure 3).
TABLE 1.
Isokinetic Testing Results at 4 Months After Surgery
| Peak Torque of Healthy Leg, N·m | Peak Torque of Injured Leg, N·m | Ratio of Weak Leg/Strong Leg,a % | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Concentric | Eccentric | Concentric | Eccentric | Concentric | Eccentric | |||||||
| 90 deg/s × 4 | 180 deg/s × 6 | 240 deg/s × 20 | 30 deg/s × 5 | 90 deg/s × 4 | 180 deg/s × 6 | 240 deg/s × 20 | 30 deg/s × 5 | 90 deg/s × 4 | 180 deg/s × 6 | 240 deg/s × 20 | 30 deg/s × 5 | |
| Quadriceps | 241.1 | 202.3 | 172.2 | 279.0 | 250.7 | 196.1 | 170.2 | 322.6 | 4 | –3 | –1 | 16 |
| Hamstring | 177.6 | 150.7 | 145.2 | 174.1 | 141.4 | 127.0 | 126.1 | 202.6 | –20 | –16 | –13 | 16 |
| Ratio of hamstring/quadricepsb | 0.74 | 0.74 | 0.84 | 0.62 | 0.56 | 0.65 | 0.74 | 0.63 | ||||
aThe peak torque of the weaker leg divided by the peak torque of the stronger leg, then multiplied by 100 to give a percentage. A positive value is used when the injured leg is the stronger leg.
bThe peak torque of the hamstring divided by the peak torque of the quadriceps.
Figure 3.
Magnetic resonance imaging at 18 months after surgery demonstrating satisfactory healing of the distal semimembranosus tendon (red circle).
Discussion
This case report demonstrates that acute repair of distal semimembranosus tendon avulsions can lead to an excellent outcome. Distal semimembranosus tendon avulsions are extremely rare. We only identified one other case of surgical repair of an isolated distal semimembranosus tendon rupture in the literature.3 This was in a professional soccer player, who had a satisfactory outcome with a return to competitive sports at 3 months. Varela et al33 reported on 2 patients with a chronic rupture of the distal semimembranosus tendon who presented with a painful palpable mass in the posterior compartment of the knee. MRI demonstrated a complete rupture of the distal tendon, with significant retraction and associated muscle atrophy. Bosnjak et al7 reported a case of delayed sciatic neuropathy due to perineurial scarring after a distal semimembranosus muscle rupture. These articles suggest that if treated nonoperatively, the consequences are not benign.
The literature on the surgical treatment of distal tears of the hamstring muscle is very scarce and comprises mostly biceps femoris tears.12,16,26,27,29,32 Lempainen et al27 reported on a series of 18 patients with distal hamstring tendon tears. Of these, 5 had semimembranosus tears, all of which were at the musculotendinous junction. There were poor results with the 4 patients who underwent delayed surgical repair (at 6-72 months after the injury), with none returning to preinjury levels of sports. The one patient who underwent acute repair (6 weeks after the injury) had an excellent outcome, with a return to sporting activity at 6 months after surgery. Studies on proximal hamstring injuries have also reported worse results with delayed repair compared to acute repair.6,19 Our group reported satisfactory outcomes after surgery for chronic distal semitendinosus injuries, with resection of the tendon using an open stripper for tendon harvesting.30 This technique, however, is not possible with the semimembranosus because of the large size of its distal attachment.
The distal semimembranosus tendon is a very complex structure. It is divided into up to 6 tendinous branches at the level of the joint line.4,13 These tendinous arms are intimately related to the posterior oblique ligament and the arcuate ligament, which contribute to the posteromedial corner of the knee.4 It therefore plays an important role in posteromedial stability of the knee. At surgery, it is important to carefully evaluate if its distal insertions are damaged. In the present case, the rupture was 1 cm proximal to the joint line, and the posteromedial corner structures were intact. Distal semimembranosus tendon avulsions can also be associated with other knee injuries. Aldebeyan et al2 reported a case of a semimembranosus tendon avulsion associated with a biceps femoris avulsion and posterolateral corner injury in a professional American football player. Khoshnoodi et al23 reported a semimembranosus avulsion fracture associated with a posterior cruciate ligament tear, medial meniscal tear, and capsular rupture in a 26-year-old football player. It is therefore important to assess for any associated injuries on MRI and at the time of surgery.
Hamstring injuries are the most common injuries in athletes.28 They are the single largest cause of lost playing time in Australian football20 and American football.11 They are also the predominant injury responsible for a prolonged absence (>28 days) from playing soccer.15 The incidence of hamstring injuries in rugby players is nearly twice that reported for soccer players.8 A study found a substantial burden placed on rugby union clubs from hamstring muscle injuries, with a mean of 7 injuries and 123 days lost per club per season.8 The mechanism of the rupture in the present case was forced hip flexion and knee hyperextension against an opposing force during a ruck. Hamstring injuries result from forceful eccentric muscle contraction or excessive passive lengthening. This normally occurs after abrupt hyperflexion of the hip with an extended knee.5,31 This is a classic mechanism of injury in a rugby player. In a ruck, the player is not allowed to go to ground and must stay standing with the hips flexed and upper body over the ball. This position puts the player at risk if the force of the opposition pack pushes the ruck backwards.
It is important to identify at which level the hamstring tendon has been injured to guide treatment. This study adds to the scarce literature on distal semimembranosus tendon avulsion injuries. It demonstrates that acute surgical repair leads to satisfactory results with a return to high-level sporting activity.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: B.S.-C. is a paid consultant for, receives research support from, has made presentations for, and receives royalties from Arthrex. M.T. is a paid consultant for, receives research support from, and has made presentations for Arthrex.
Ethical approval for this report was obtained from the Centre Orthopédique Santy.
References
- 1. Agre JC. Hamstring injuries: proposed aetiological factors, prevention, and treatment. Sports Med Auckl NZ. 1985;2(1):21–33. [DOI] [PubMed] [Google Scholar]
- 2. Aldebeyan S, Boily M, Martineau PA. Complete tear of the distal hamstring tendons in a professional football player: a case report and review of the literature. Skeletal Radiol. 2016;45(3):427–430. [DOI] [PubMed] [Google Scholar]
- 3. Alioto RJ, Browne JE, Barnthouse CD, Scott AR. Complete rupture of the distal semimembranosus complex in a professional athlete. Clin Orthop Relat Res. 1997;(336):162–165. [DOI] [PubMed] [Google Scholar]
- 4. Beltran J, Matityahu A, Hwang K, et al. The distal semimembranosus complex: normal MR anatomy, variants, biomechanics and pathology. Skeletal Radiol. 2003;32(8):435–445. [DOI] [PubMed] [Google Scholar]
- 5. Bencardino JT, Mellado JM. Hamstring injuries of the hip. Magn Reson Imaging Clin N Am. 2005;13(4):677–690, vi. [DOI] [PubMed] [Google Scholar]
- 6. Blakeney WG, Zilko SR, Edmonston SJ, Schupp NE, Annear PT. A prospective evaluation of proximal hamstring tendon avulsions: improved functional outcomes following surgical repair. Knee Surg Sports Traumatol Arthrosc. 2017;25(6):1943–1950. [DOI] [PubMed] [Google Scholar]
- 7. Bosnjak R, Mofardin S, Derham C. Delayed sciatic neuropathy after distal semimembranosus muscle rupture associated with tethering of the sciatic nerve by a rare distal muscular branch. Injury. 2009;40(2):226–229. [DOI] [PubMed] [Google Scholar]
- 8. Brooks JHM, Fuller CW, Kemp SPT, Reddin DB. Incidence, risk, and prevention of hamstring muscle injuries in professional rugby union. Am J Sports Med. 2006;34(8):1297–1306. [DOI] [PubMed] [Google Scholar]
- 9. Brukner P. Hamstring injuries: prevention and treatment. An update. Br J Sports Med. 2015;49(19):1241–1244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Clanton TO, Coupe KJ. Hamstring strains in athletes: diagnosis and treatment. J Am Acad Orthop Surg. 1998;6(4):237–248. [DOI] [PubMed] [Google Scholar]
- 11. Cohen SB, Towers JD, Zoga A, et al. Hamstring injuries in professional football players: magnetic resonance imaging correlation with return to play. Sports Health. 2011;3(5):423–430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. David A, Buchholz J, Muhr G. Tear of the biceps femoris tendon. Arch Orthop Trauma Surg. 1994;113(6):351–352. [DOI] [PubMed] [Google Scholar]
- 13. De Maeseneer M, Shahabpour M, Lenchik L, et al. Distal insertions of the semimembranosus tendon: MR imaging with anatomic correlation. Skeletal Radiol. 2014;43(6):781–791. [DOI] [PubMed] [Google Scholar]
- 14. De Smet AA, Best TM. MR imaging of the distribution and location of acute hamstring injuries in athletes. AJR Am J Roentgenol. 2000;174(2):393–399. [DOI] [PubMed] [Google Scholar]
- 15. Ekstrand J, Hägglund M, Waldén M. Epidemiology of muscle injuries in professional football (soccer). Am J Sports Med. 2011;39(6):1226–1232. [DOI] [PubMed] [Google Scholar]
- 16. Fortems Y, Victor J, Dauwe D, Fabry G. Isolated complete rupture of biceps femoris tendon. Injury. 1995;26(4):275–276. [DOI] [PubMed] [Google Scholar]
- 17. Garrett WE. Injuries to the muscle-tendon unit. Instr Course Lect. 1988;37:275–282. [PubMed] [Google Scholar]
- 18. Gidwani S, Bircher MD. Avulsion injuries of the hamstring origin: a series of 12 patients and management algorithm. Ann R Coll Surg Engl. 2007;89(4):394–399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Harris JD, Griesser MJ, Best TM, Ellis TJ. Treatment of proximal hamstring ruptures: a systematic review. Int J Sports Med. 2011;32(7):490–495. [DOI] [PubMed] [Google Scholar]
- 20. Hickey J, Shield AJ, Williams MD, Opar DA. The financial cost of hamstring strain injuries in the Australian Football League. Br J Sports Med. 2014;48(8):729–730. [DOI] [PubMed] [Google Scholar]
- 21. Ishikawa K, Kai K, Mizuta H. Avulsion of the hamstring muscles from the ischial tuberosity: a report of two cases. Clin Orthop Relat Res. 1988;(232):153–155. [PubMed] [Google Scholar]
- 22. Järvinen TAH, Järvinen TLN, Kääriäinen M, Kalimo H, Järvinen M. Muscle injuries: biology and treatment. Am J Sports Med. 2005;33(5):745–764. [DOI] [PubMed] [Google Scholar]
- 23. Khoshnoodi P, Tehranzadeh AD, Dunn JM, Tehranzadeh J. Semimembranosus tendon avulsion fracture of the posteromedial tibial plateau associated with posterior cruciate ligament tear and capsular rupture. Skeletal Radiol. 2014;43(2):239–242. [DOI] [PubMed] [Google Scholar]
- 24. Koulouris G, Connell D. Evaluation of the hamstring muscle complex following acute injury. Skeletal Radiol. 2003;32(10):582–589. [DOI] [PubMed] [Google Scholar]
- 25. Kujala UM, Orava S, Järvinen M. Hamstring injuries: current trends in treatment and prevention. Sports Med Auckl NZ. 1997;23(6):397–404. [DOI] [PubMed] [Google Scholar]
- 26. Kusma M, Seil R, Kohn D. Isolated avulsion of the biceps femoris insertion-injury patterns and treatment options: a case report and literature review. Arch Orthop Trauma Surg. 2007;127(9):777–780. [DOI] [PubMed] [Google Scholar]
- 27. Lempainen L, Sarimo J, Mattila K, Heikkilä J, Orava S. Distal tears of the hamstring muscles: review of the literature and our results of surgical treatment. Br J Sports Med. 2007;41(2):80–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Opar DA, Williams MD, Shield AJ. Hamstring strain injuries: factors that lead to injury and re-injury. Sports Med Auckl NZ. 2012;42(3):209–226. [DOI] [PubMed] [Google Scholar]
- 29. Sebastianelli WJ, Hanks GA, Kalenak A. Isolated avulsion of the biceps femoris insertion: a case report. Clin Orthop Relat Res. 1990;(259):200–203. [PubMed] [Google Scholar]
- 30. Sonnery-Cottet B, Daggett M, Gardon R, Pupim B, Clechet J, Thaunat M. Surgical management of recurrent musculotendinous hamstring injury in professional athletes. Orthop J Sports Med. 2015;3(10):2325967115606393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Stevens MA, El-Khoury GY, Kathol MH, Brandser EA, Chow S. Imaging features of avulsion injuries. RadioGraphics. 1999;19(3):655–672. [DOI] [PubMed] [Google Scholar]
- 32. Valente M, Mancuso F, Alecci V. Isolated rupture of biceps femoris tendon. Musculoskelet Surg. 2013;97(3):263–266. [DOI] [PubMed] [Google Scholar]
- 33. Varela JR, Rodríguez E, Soler R, González J, Pombo S. Complete rupture of the distal semimembranosus tendon with secondary hamstring muscles atrophy: MR findings in two cases. Skeletal Radiol. 2000;29(6):362–364. [DOI] [PubMed] [Google Scholar]
- 34. Worrell TW. Factors associated with hamstring injuries: an approach to treatment and preventative measures. Sports Med Auckl NZ. 1994;17(5):338–345. [DOI] [PubMed] [Google Scholar]