Abstract
Objective:
Rural areas in Ontario have fewer psychiatrists, making access to specialist mental health care challenging. Our objective was to characterise psychiatrists delivering and patients receiving telepsychiatry in Ontario and to determine the number of patients who accessed a psychiatrist via telepsychiatry following discharge from psychiatric hospitalisation.
Method:
We conducted a serial panel study to evaluate the characteristics of psychiatrists providing telepsychiatry from April 2007 to March 2013. In addition, we conducted a cross-sectional study for fiscal year 2012-2013 to examine telepsychiatry patient characteristics and create an in-need patient cohort of individuals with a recent psychiatric hospitalisation that assessed if they had follow-up with a psychiatrist in person or through telepsychiatry within 1 year of discharge.
Results:
In fiscal year 2012-2013, a total of 3801 people had 5635 telepsychiatry visits, and 7% (n = 138) of Ontario psychiatrists provided telepsychiatry. Of the 48,381 people identified as in need of psychiatric care, 60% saw a local psychiatrist, 39% saw no psychiatrist, and less than 1% saw a psychiatrist through telepsychiatry only or telepsychiatry in addition to local psychiatry within a year. Three northern regions had more than 50% of in-need patients fail to access psychiatry within 1 year.
Conclusions:
Currently, relatively few patients and psychiatrists use telepsychiatry. In addition, patients scarcely access telepsychiatry for posthospitalisation follow-up. This study, which serves as a preliminary baseline for telepsychiatry in Ontario, demonstrates that telepsychiatry has not evolved systematically to address need and highlights the importance of system-level planning when implementing telepsychiatry to optimise access to care.
Keywords: telepsychiatry, telemental health, telemedicine, access, telehealth, e-health, psychiatry
Abstract
Objectif:
Les régions rurales de l’Ontario comptent moins de psychiatres, ce qui complique l’accès aux soins de santé mentale d’un spécialiste. Notre objectif était de caractériser les psychiatres qui fournissent la télépsychiatrie et les patients qui la reçoivent en Ontario, et de déterminer le nombre de patients qui ont eu accès à un psychiatre par la télépsychiatrie par suite d’un congé d’une hospitalisation psychiatrique.
Méthode:
Nous avons mené une étude par panel en série afin d’évaluer les caractéristiques des psychiatres qui ont fourni la télépsychiatrie entre avril 2007 et mars 2013. En outre, nous avons mené une étude transversale pour l’exercice financier 2012-2013 afin d’examiner les caractéristiques des patients de la télépsychiatrie et de créer une cohorte de patients en besoin qui ont eu une hospitalisation psychiatrique récente ayant évalué si leur suivi serait avec un psychiatre en personne ou par télépsychiatrie dans l’année suivant le congé.
Résultats:
Dans l’exercice financier 2012-2013, 3 801 personnes ont eu un total de 5 635 visites en télépsychiatrie, et 7% (n = 138) des psychiatres ontariens ont fourni la télépsychiatrie. Sur les 48 381 personnes identifiées comme ayant des besoins de soins psychiatriques, 60% voyaient un psychiatre local, 39% ne voyaient pas de psychiatre, et moins de 1% voyaient un psychiatre par télépsychiatrie seulement ou par télépsychiatrie en plus d’un psychiatre local, en une année. Trois régions nordiques avaient plus de 50% de patients en besoin qui n’ont pas eu accès à la psychiatrie en un an.
Conclusions:
À l’heure actuelle, relativement peu de patients et de psychiatres ont recours à la télépsychiatrie. En outre, les patients ont rarement accès à la télépsychiatrie pour un suivi post-hospitalisation. Cette étude, qui sert de base préliminaire à la télépsychiatrie en Ontario, démontre que la télépsychiatrie n’a pas évolué systématiquement pour répondre aux besoins et met en évidence l’importance de la planification au niveau du système pour la mise en œuvre de la télépsychiatrie, afin d’optimiser l’accès aux soins.
Telepsychiatry, a real-time consultation by a psychiatrist to a patient via videoconferencing, is an effective and reliable mode of health services delivery with high levels of patient satisfaction.1–8 Telepsychiatry can bridge geographical disparities and, therefore, improve access to psychiatric care in rural areas, which is particularly important given that rural populations typically have poorer mental health outcomes and higher rates of suicide in comparison to urban populations.2,5,9–12 Although telepsychiatry has been implemented globally, few studies have evaluated its implementation and utilisation, including whether telepsychiatry resources are systematically applied based upon areas of greatest need, such as local resources relative to local need.2,9,13–16 In Ontario, there is limited evidence to guide the strategic implementation of telepsychiatry to effectively distribute and integrate care from areas with high supply of psychiatry health human resources to areas of low supply.
In light of the inequitable access to psychiatrists and mental health services within rural areas, it is pivotal that telepsychiatry is well planned and implemented, especially for those with high need. As a first step towards understanding the present state of telepsychiatry, we aimed to describe the current distribution and utilisation of telepsychiatry using administrative data. To do this, we 1) characterised psychiatrists delivering telepsychiatry (examining demographic, geographic, and practice pattern information) from April 1, 2007, to March 31, 2013, and patients receiving telepsychiatry services in Ontario (examining demographic and geographic information) between April 1, 2012, and March 31, 2013, and 2) using psychiatric hospitalisation (from April 1, 2012 to March 31, 2013) as a proxy of need, determined how many people saw a psychiatrist, telepsychiatrist, or both within 1 year postdischarge from a psychiatric hospitalisation. The first objective describes the status of telepsychiatry; the second objective measures the extent to which telepsychiatry is meeting the needs of individuals with high need for psychiatrist services.
Methods
Study Design
We conducted a serial panel study for psychiatrists, in which we evaluated the change in psychiatrist demographic data for each fiscal year from April 2007 to March 2013 and examined the characteristics of psychiatrists providing telepsychiatry. Next, to examine patient characteristics, we conducted a yearly cross-sectional study that captured all telepsychiatry visits that occurred between April 1, 2012, and March 31, 2013. In addition, we used the information described above about psychiatrists delivering telepsychiatry and patients receiving telepsychiatry from April 1, 2012, to March 31, 2013, to map the data to examine the service distribution of telepsychiatry.
Finally, we developed a cohort of all Ontario patients who were discharged from a psychiatric hospital between April 1, 2012, and March 31, 2013. A psychiatric hospitalisation discharge was our proxy of need for access to an outpatient psychiatric consultation. As with preexisting performance indicators (Organisation for Economic Co-operation and Development [OECD], Canadian Institute for Health Information [CIHI], Health Quality Ontario [HQO]), we evaluated physician follow-up (psychiatrist or family physician) following psychiatric hospitalisation discharge.17–19 To be more inclusive, we measured follow-up appointments within 1 year after hospital discharge rather than the more standard 7- or 30-day window. In addition, of the psychiatrist follow-up appointments, we investigated whether the visit was in person (local) versus telepsychiatry. Patients with dementia/delirium (International Classification of Diseases, Tenth Revision codes F00-F09) were excluded because a substantial number of patients with delirium are discharged to nursing homes rather than into community-based settings where outpatient telepsychiatry is typically provided. Patients who did not have a valid health card number and missing age or sex were also excluded.
Data Sources
The administrative health data sets were linked using unique encoded identifiers and analysed at the Institute for Clinical Evaluative Sciences (ICES). We used the Ontario Health Insurance Plan (OHIP) claims database, including codes that identify whether a psychiatric consultation was delivered via telepsychiatry, to create a cohort of telepsychiatry visits (by psychiatrist site and patient site). To assess psychiatrist characteristics within this cohort, we used the ICES Physician Database to measure annual demographics, specialisation, and workload of psychiatrists. For patients, we used the Registered Persons Database (RPDB) to attain demographic characteristics of patients within this cohort. With these data, we were able to determine the Local Health Integration Network (LHIN) of providers delivering and patients receiving telepsychiatry consultations and generate an image mapping the distribution of telepsychiatry. Statistics Canada Census 2006 data were used to derive neighbourhood-level income.
To identify in-need patients, psychiatric hospital discharges were identified using the CIHI–Discharge Abstract Database (DAD) and Ontario Mental Health Reporting System (OMHRS). The RPDB was used to then investigate the demographics of in-need patients, and the OHIP claims database was used to measure primary care and psychiatry follow-up visits (both local and telepsychiatry visits). Sunnybrook Health Sciences Centre Research Ethics Board approved this study.
Measures
Psychiatrists in Ontario are required to use the Ontario Telemedicine Network (OTN) technology platform to deliver telepsychiatry and subsequently can bill 2 OHIP codes: one for the consultation and a second telemedicine billing code. We focused our analyses on completed telepsychiatry visits, which were defined using the telemedicine codes B100A and B200A (delivery of a first telepsychiatry patient encounter or subsequent patient encounter, respectively). Using these codes, we measured how many psychiatrists provided telepsychiatry by year and measured the following demographic characteristics of these providers: sex, age, region of practice (LHIN), and number of years in practice.
For patients receiving telepsychiatry, we measured sex, age, region of residence (LHIN), and income quintile. Neighbourhood-level income was categorised as income quintiles. The income quintile from the neighbourhood in which the subjects resided was assigned to the subject. To examine patient need for access to psychiatry, we developed an in-need cohort by taking the first discharge per patient within each given year, and we determined if individuals received follow-up care within 1 year of a hospital discharge by physician type (family physician or psychiatrist) and whether psychiatric follow-up was provided through telepsychiatry or in person. We included all family physician follow-up visits.
Data Analyses
Descriptive statistics are provided for the demographic variables for each cohort (psychiatrists and patients) to examine telepsychiatry visits and characteristics of psychiatrists delivering telepsychiatry and patients receiving telepsychiatry. We created an image that maps the use of telepsychiatry by LHIN between providers and patients and analysed distribution of care. For all in-need patients hospitalised for psychiatric reason(s), we looked for follow-up within a year by
- Physician (primary care provider and/or psychiatrist)
- Primary care provider and psychiatrist
- Only a psychiatrist
- Neither a primary care provider or a psychiatrist (psychiatry includes telepsychiatry and local psychiatry)
- Psychiatrist appointment type
- Local and telepsychiatry
- Local psychiatry only
- Telepsychiatry only
- No psychiatry
Data that had cell sizes smaller than 6 were excluded from the table and not reported as a means to preserve confidentiality and anonymity.
Results
Psychiatrists Delivering Telepsychiatry
In 2012, psychiatrists performing telepsychiatry were an average age of 50 years (mean = 49.7, SD = 11.3), with an average of 24 years in practice (mean = 23.9, SD = 11.9). In 2012, of 1911 total practicing psychiatrists, only 7% were delivering care through telepsychiatry (n = 138) (Table 1). In 2012, 41% (n = 57) of psychiatrists who conducted telepsychiatry were in the Toronto Central LHIN, 11.6% (n = 16) were in the Hamilton Niagara Haldimand Brant LHIN, 8.7% (n = 12) were in the Champlain LHIN, 5.8% (n = 8) were in the North Simcoe Muskoka LHIN, and 5% (n = 7) were in the South West LHIN. All other LHINs each had less than 5% (n < 6) of total psychiatrists who delivered telepsychiatry in 2012.
Table 1.
Characteristics of Ontario Psychiatrists Providing Telepsychiatry, 2007-2012.
| 2008-2009 | 2009-2010 | 2010-2011 | 2011-2012 | 2012-2013 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Characteristic | n | Column % | n | Column % | n | Column % | n | Column % | n | Column % |
| Number of providers | 46 | 100 | 57 | 100 | 74 | 100 | 115 | 100 | 138 | 100 |
| Sex | ||||||||||
| Female | 11 | 23.9 | 16 | 28.1 | 23 | 31.1 | 43 | 37.4 | 51 | 37 |
| Male | 35 | 76.1 | 41 | 71.9 | 51 | 68.9 | 72 | 62.6 | 87 | 63 |
| Age category, y | ||||||||||
| 31 to 40 | 7 | 15.2 | 13 | 22.8 | 14 | 18.9 | 32 | 27.8 | 37 | 26.8 |
| 41 to 50 | 13 | 28.3 | 13 | 22.8 | 14 | 18.9 | 25 | 21.7 | 35 | 25.4 |
| 51 to 60 | 15 | 32.6 | 19 | 33.3 | 25 | 33.8 | 38 | 33 | 38 | 27.5 |
| >60 | 11 | 23.9 | 12 | 21.1 | 21 | 28.4 | 20 | 17.4 | 27 | 19.6 |
| Local Health Integration Networka | ||||||||||
| Champlain | 6 | 13 | 9 | 15.8 | 9 | 12.2 | 13 | 11.3 | 12 | 8.7 |
| Hamilton Niagara Haldimand Brant | <6 | <13 | <6 | <11 | <6 | <8 | 9 | 7.8 | 16 | 11.6 |
| Toronto Central | 23 | 50 | 29 | 50.9 | 38 | 51.4 | 54 | 47 | 57 | 41.3 |
The 2007-2008 fiscal year is not reported because it had too few psychiatrists (<6) in certain categories such that particular psychiatrists could potentially be identifiable.
aLargest providers of telepsychiatry.
The total number of psychiatrists delivering telepsychiatry increased 3-fold from 2008 to 2012. We did not include the data from 2007-2008 in our analysis, because all cells reported too few psychiatrists (n < 6) such that particular psychiatrists could potentially be identifiable. The proportion of psychiatrists providing telepsychiatry who were female steadily increased from 24% in 2008 to 37% in 2012. By 2012, the proportion of female psychiatrists providing telepsychiatry (37%; n = 51/138) was much closer to the overall proportion of female psychiatrists in Ontario (40%; n = 759/1911).
Patients Receiving Telepsychiatry
In 2012, 17% of telepsychiatry patients were 15 years and younger, 19% were aged 16 to 25 years, 34% were 26 to 45 years, 23% were 46 to 65 years, and only 7% were older than 65 years (Table 2). Of all patients seen through telepsychiatry in 2012, about 55% of visits occurred within 3 LHINs: 22.7% in the North East LHIN, 16.9% in the Central East LHIN, and 15.5% in the North Simcoe Muskoka LHIN. The remaining 11 LHINs made up approximately 45% of all patient telepsychiatry visits. Patients in lower neighbourhood income quintiles had higher rates of telepsychiatry consultations: quintile 1 (lowest) had 29%, quintile 2 had 22%, quintile 3 had 18%, quintile 4 had 17%, and quintile 5 (highest) had 13%.
Table 2.
Characteristics of Ontario Patients Receiving Telepsychiatry, 2012.
| Characteristic | n | Column % |
|---|---|---|
| Number of patients | 3801 | 100 |
| Sex | ||
| Female | 1925 | 50.6 |
| Male | 1876 | 49.4 |
| Age category, y | ||
| 15 and younger | 641 | 16.9 |
| 16 to 25 | 730 | 19.2 |
| 26 to 45 | 1289 | 33.9 |
| 46 to 65 | 881 | 23.2 |
| 65 and older | 260 | 6.8 |
| Local Health Integration Network | ||
| Central | 76 | 2 |
| Central East | 642 | 16.9 |
| Central West | 58 | 1.5 |
| Champlain | 133 | 3.5 |
| Erie St. Clair | 284 | 7.5 |
| Hamilton Niagara Haldimand Brant | 346 | 9.1 |
| Mississauga Halton | 56 | 1.5 |
| North East | 864 | 22.7 |
| North Simcoe Muskoka | 588 | 15.5 |
| North West | 276 | 7.3 |
| South East | 116 | 3.1 |
| South West | 179 | 4.7 |
| Toronto Central | 32 | 0.8 |
| Waterloo Wellington | 151 | 4 |
| Neighbourhood income quintile | ||
| Missing | 29 | 0.8 |
| 1 | 1113 | 29.3 |
| 2 | 825 | 21.7 |
| 3 | 698 | 18.4 |
| 4 | 661 | 17.4 |
| 5 | 475 | 12.5 |
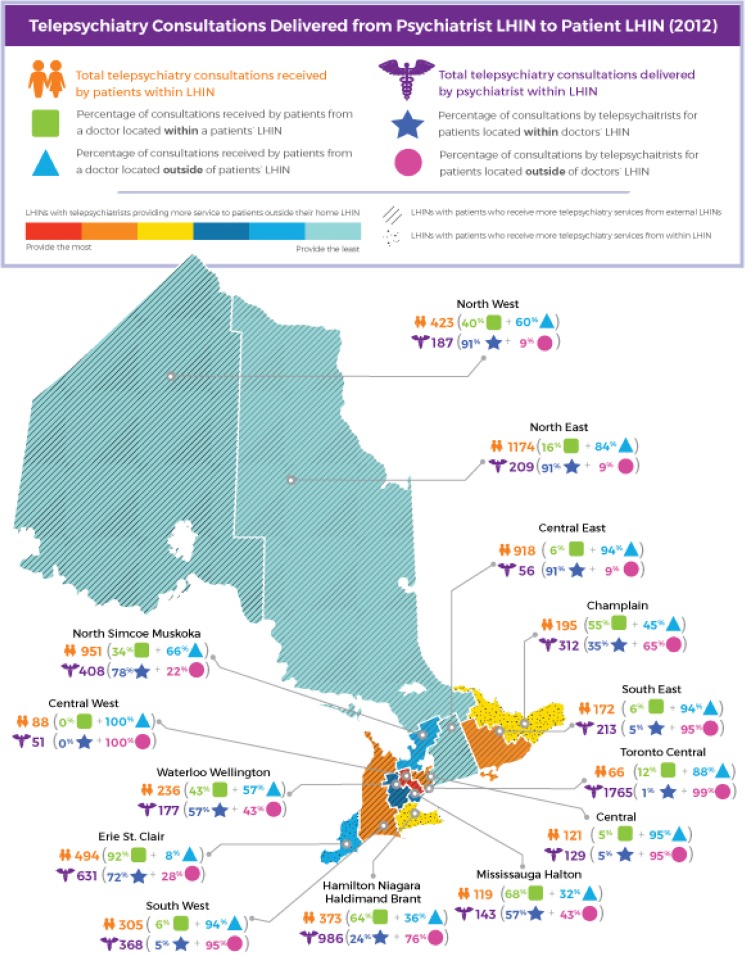
Distribution of Telepsychiatry
A map visualising the 2012 distribution of telepsychiatry providers and patients is included in Figure 1. The map shows data reflecting the locations from which telepsychiatry is delivered by psychiatrists and received by patients. To summarise, there were 6283 billed telepsychiatry-related visits, but after applying exclusions for people with missing data (i.e., sex, age), missed/cancelled telepsychiatry consultations, and those not eligible for OHIP, there were 5635 telepsychiatry visits delivered to 3801 patients throughout Ontario. Of those visits, the 3 largest providers of telepsychiatry (total appointments delivered by local psychiatrists) were from Toronto Central (31%; n = 1765), Hamilton Niagara Haldimand Brant (17.5%; n = 986), and Erie St. Clair (11%; n = 631) LHINs. Central West (n = 51) and Central East (n = 56) both had less than 1% of total telepsychiatry delivered from their local psychiatrists. Of total visits, the 3 largest recipients of telepsychiatry (patients) were from the North East (21%; n = 1174), North Simcoe Muskoka (17%; n = 951), and Central East (16%, n = 918) LHINs, and the Toronto Central LHIN (n = 66) had only about 1% of total telepsychiatry received by patients within their LHIN. While most LHINs either predominantly provide or receive substantial quantities of telepsychiatry, a few LHINs both provide and receive substantial quantities of telepsychiatry.
Figure 1.
Telepsychiatry consultations delivered from psychiatrist Local Health Integration Network (LHIN) to patient LHIN.
Patients in Need of Psychiatric Consultation after Hospital Discharge
Among the 48,381 patients who had a psychiatric hospitalisation discharge in fiscal year 2012, 50.8% (n = 24,562) saw a psychiatrist and primary care provider, 10.4% (n = 5047) saw only a psychiatrist, 29% (n = 14,040) saw only a primary care provider, and 9.8% (n = 4732) saw neither a psychiatrist nor a primary care provider within a year of discharge. We further examined only psychiatrist visits and found that patients accessed care through local and telepsychiatry (n = 445; <1%), telepsychiatry (n = 25; <1%), or local psychiatry (n = 29,139; 60.2%) or had no psychiatry follow-up (n = 18,772; 38.8%) (Table 3). Fifty percent of adults 65 years or older did not receive any psychiatric follow-up within 1 year of discharge from a hospital, 49% sought care through a local psychiatrist, and less than 1% received care via telepsychiatry. All other age groups had between approximately 36% and 40% of in-need patients who did not see a psychiatrist in person or through telepsychiatry, and 59% to 63% saw a local psychiatrist. Telepsychiatry alone was not reported in Table 3 due to the very low number of telepsychiatry visits (n = 25), which led to small cell sizes after stratification.
Table 3.
Psychiatrist Follow-up after Hospitalisation, 2012.
| Characteristic | Psychiatrist Follow-up after Hospitalisation | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| All | Local and Telepsychiatry | Local Psychiatry Only | No Psychiatry | |||||||||
| n | Column % | Row % | n | Column % | Row % | n | Column % | Row % | n | Column % | Row % | |
| Number of patients | 48,381 | 100 | 100 | 445 | 100 | 0.9 | 29,139 | 100 | 60.2 | 18,772 | 100 | 38.8 |
| Sex | ||||||||||||
| Female | 24,316 | 50.3 | 100 | 223 | 50.1 | 0.9 | 15,430 | 53 | 63.5 | 8650 | 46.1 | 35.6 |
| Male | 24,065 | 49.7 | 100 | 222 | 49.9 | 0.9 | 13,709 | 47 | 57 | 10,122 | 53.9 | 42.1 |
| Age category, y | ||||||||||||
| 15 and younger | 3916 | 8.1 | 100 | 50 | 11.2 | 1.3 | 2400 | 8.2 | 61.3 | 1459 | 7.8 | 37.3 |
| 16 to 25 | 10,437 | 21.6 | 100 | 103 | 23.1 | 1 | 6513 | 22.4 | 62.4 | 3816 | 20.3 | 36.6 |
| 26 to 45 | 15,283 | 31.6 | 100 | 171 | 38.4 | 1.1 | 9675 | 33.2 | 63.3 | 5427 | 28.9 | 35.5 |
| 46 to 65 | 13,502 | 27.9 | 100 | 96 | 21.6 | 0.7 | 7951 | 27.3 | 58.9 | 5452 | 29 | 40.4 |
| 65 and older | 5243 | 10.8 | 100 | 25 | 5.6 | 0.5 | 2600 | 8.9 | 49.6 | 2618 | 13.9 | 49.9 |
| Local Health Integration Network | ||||||||||||
| Central | 4760 | 9.8 | 100 | 21 | 4.7 | 0.4 | 3288 | 11.3 | 69.1 | 1451 | 7.7 | 30.5 |
| Central East | 4935 | 10.2 | 100 | 47 | 10.6 | 1 | 3132 | 10.7 | 63.5 | 1753 | 9.3 | 35.5 |
| Central West | 2487 | 5.1 | 100 | 16 | 3.6 | 0.6 | 1565 | 5.4 | 62.9 | 905 | 4.8 | 36.4 |
| Champlain | 4317 | 8.9 | 100 | 16 | 3.6 | 0.4 | 2957 | 10.1 | 68.5 | 1344 | 7.2 | 31.1 |
| Erie St. Clair | 2432 | 5 | 100 | 24 | 5.4 | 1 | 1668 | 5.7 | 68.6 | 740 | 3.9 | 30.4 |
| Hamilton Niagara Haldimand Brant | 5296 | 10.9 | 100 | 46 | 10.3 | 0.9 | 3274 | 11.2 | 61.8 | 1974 | 10.5 | 37.3 |
| Mississauga Halton | 2796 | 5.8 | 100 | 13 | 2.9 | 0.5 | 1952 | 6.7 | 69.8 | 831 | 4.4 | 29.7 |
| North East | 3640 | 7.5 | 100 | 112 | 25.2 | 3.1 | 1456 | 5 | 40 | 2062 | 11 | 56.6 |
| North Simcoe Muskoka | 2298 | 4.7 | 100 | 65 | 14.6 | 2.8 | 1051 | 3.6 | 45.7 | 1180 | 6.3 | 51.3 |
| North West | 1484 | 3.1 | 100 | 32 | 7.2 | 2.2 | 255 | 0.9 | 17.2 | 1194 | 6.4 | 80.5 |
| South East | 1935 | 4 | 100 | <15 | <3.4 | 0.6 | 1075 | 3.7 | 55.6 | 848 | 4.5 | 43.8 |
| South West | 4092 | 8.5 | 100 | 23 | 5.2 | 0.6 | 2108 | 7.2 | 51.5 | 1958 | 10.4 | 47.8 |
| Toronto Central | 4921 | 10.2 | 100 | <6 | <1.5 | 0.1 | 3658 | 12.6 | 74.3 | 1257 | 6.7 | 25.5 |
| Waterloo Wellington | 2988 | 6.2 | 100 | 13 | 2.9 | 0.4 | 1700 | 5.8 | 56.9 | 1275 | 6.8 | 42.7 |
| Neighbourhood income quintile | ||||||||||||
| Missing | 344 | 0.7 | 100 | 10 | 2.2 | 2.9 | 161 | 0.6 | 46.8 | 173 | 0.9 | 50.3 |
| 1 | 13,595 | 28.1 | 100 | 134 | 30.1 | 1 | 8025 | 27.5 | 59 | 5429 | 28.9 | 39.9 |
| 2 | 10,144 | 21 | 100 | 98 | 22 | 1 | 6101 | 20.9 | 60.1 | 3937 | 21 | 38.8 |
| 3 | 8659 | 17.9 | 100 | 90 | 20.2 | 1 | 5132 | 17.6 | 59.3 | 3433 | 18.3 | 39.6 |
| 4 | 8331 | 17.2 | 100 | 58 | 13 | 0.7 | 5120 | 17.6 | 61.5 | 3149 | 16.8 | 37.8 |
| 5 | 7308 | 15.1 | 100 | 55 | 12.4 | 0.8 | 4600 | 15.8 | 62.9 | 2651 | 14.1 | 36.3 |
The numbers for “telepsychiatry only” are not reported because it had too few patients (<6) in certain categories such that findings could be identifiable.
In addition, there were regional variations in psychiatry follow-up. Typically, in-person follow-up was lower in rural LHINs (North East, North West, North Simcoe Muskoka) and higher in predominantly urban LHINs, and very few in-need patients were seen in follow-up using local care and telepsychiatry or telepsychiatry within a year.
Local psychiatry follow-up visits
The percentage of in-need patients accessing local in-person psychiatric follow-up care ranged significantly by LHIN: 17% in North West, 40% in North East, 46% in North Simcoe Muskoka, 52% in South West, 56% in South East, 57% in Wellington Waterloo, 62% in Hamilton Niagara Haldimand Brant, 63% in Central West, 64% in Central East, 69% in Erie St. Clair/Central/Champlain, 70% in Mississauga Halton, and 74% in Toronto Central LHINs had in-need patients follow up in person with a local psychiatrist within a year.
Local psychiatry and telepsychiatry follow-up visits
Although the North East, North West, and North Simcoe Muskoka LHINs each had 2% to 3% of in-need patients access both local psychiatry and telepsychiatry, all other LHINs received less than 1% of postdischarge care through both local psychiatry and telepsychiatry.
No psychiatric follow-up
Three LHINs—North West (81%), North East (57%), and North Simcoe Muskoka (51%)—had over half of their total in-need patients fail to access any psychiatry within 1 year after hospitalisation. All other LHINs had between 26% and 48% of total in-need patients within their LHIN failing to access a psychiatrist within 1 year of hospitalisation.
Discussion
Three key findings emerged from our analysis: 1) relatively few practicing psychiatrists deliver care through telepsychiatry (although this percentage is growing), and only a small number of patients are receiving care through telepsychiatry; 2) there is no clearly defined, systematic rationale for the organisation of telepsychiatry delivery; and 3) patients with high need for psychiatrists are not accessing care through telepsychiatry. These findings are further discussed and contextualised below.
Overview of Psychiatrists Providing Telepsychiatry
On average, psychiatrists delivering telepsychiatry have been in practice for approximately 25 years and are predominantly male, and the highest proportion (60%) typically provide care from LHINs with major urban or academic centres, such as Toronto Central, Hamilton Niagara Haldimand Brant, and Champlain. The total number of psychiatrists providing telepsychiatry has increased 3-fold during our study period, and there was an increase in female psychiatrists and psychiatrists in the 31- to 40-year age bracket delivering telepsychiatry. Toronto Central LHIN was the largest contributor of telepsychiatry over the 5 years examined; however, the number of Toronto Central LHIN psychiatrists providing telepsychiatry was relatively stable from April 2008 to March 2013, such that Toronto Central LHIN psychiatrists accounted for a progressively lower proportion of all Ontario psychiatrists providing telepsychiatry. There remains significant opportunity for increased utilisation of telepsychiatry, given that approximately 7% of psychiatrists delivered care through telepsychiatry in 2012.
Overview of Patients Receiving Telepsychiatry
The largest percentage of patients receiving telepsychiatry care were between 26 and 45 years old, followed by those between 46 and 65 years old. Almost half (45%) of all patients receiving telepsychiatry services reside in 1 of the 3 northern rural regions (North East/North West/North Simcoe Muskoka). The North East LHIN had the largest percentage of patients receiving telepsychiatry, followed by the Central East and North Simcoe Muskoka LHINs. Although there are numerous reasons why these LHINs have high telepsychiatry utilisation, it is likely because these LHINs have among the lowest supply of psychiatrists relative to population and therefore the greatest need for access to psychiatrists through telepsychiatry.
Regional Distribution of Telepsychiatry in 2012
While telepsychiatry is commonly used to deploy psychiatry from LHINs with greater supply of psychiatrists to those that are underserved, several other themes emerged that revealed a lack of systematic coordination and possible redundancy in the provision of service. The 4 distribution themes we identified are included in Table 4.
Table 4.
Telepsychiatry Distribution Themes.
| Type of Distribution | Explanation and Examples |
|---|---|
| Large recipient of external and internal telepsychiatry, minor provider of external telepsychiatry | There are a number of LHINs where local psychiatrists provide the majority of telepsychiatry to patients within their own LHIN, and local patients also receive numerous telepsychiatry appointments from psychiatrists in external LHINs. Typically, these LHINs do not deliver much telepsychiatry in general. |
| Minor recipient of telepsychiatry, large provider of external telepsychiatry | One LHIN with a large local psychiatrist supply, the Toronto Central LHIN, provides a vast amount of telepsychiatry to other LHINs, but a very small proportion of telepsychiatry delivered by Toronto Central LHIN psychiatrists is received within their LHIN. |
| Majority of telepsychiatry provided within LHIN, minimal external telepsychiatry received | There are LHINs such as Erie St. Clair, where psychiatrists provide the majority of telepsychiatry to patients within their own LHIN, and minimal telepsychiatry is received from external LHIN psychiatrists. |
| Telepsychiatry provided to numerous LHINs, telepsychiatry received from numerous LHINs | Some LHINs (e.g., South East, South West, Central, and Hamilton Niagara Haldimand Brant) have psychiatrists who both deliver a significant amount of telepsychiatry to other LHINs and patients who receive a large amount of telepsychiatry from external LHIN psychiatrists. Given that these LHINs are robust providers to other LHINs, it is unclear why they receive such large amounts of telepsychiatry from external LHINs. |
LHIN, Local Health Integration Network.
Use of Telepsychiatry to Support In-Need Patients
While telepsychiatry was delivered to 3801 patients across the province, only 1% of those who met our criteria of high need received care by telepsychiatry. Approximately 10% of in-need patients throughout the province do not access any follow-up care from either a psychiatrist or primary care provider, and nearly 40% do not see a psychiatrist. However, there is a large regional disparity for in-need patients who access local psychiatric follow-up care, ranging from 17% to 74% across LHINs. These findings indicate that although telepsychiatry is delivering care to a number of patients provincially, it is not being used to support those in high need of mental health support.
Contextualising Findings
In Ontario, there is a high degree of regional variability in psychiatrists per capita, with low-supply LHINs having only 7.2 psychiatrists per 100,000 residents and the highest supply LHIN, the Toronto Central LHIN, having 62.7 psychiatrists per 100,000 residents.20 Our findings suggest that telepsychiatry effectively increases the supply of psychiatrists in low-supply regions—psychiatrists in high-supply urban centres provide the majority of telepsychiatry to patients in LHINs that are largely rural, with low psychiatrist supply. This trend is evident in our results, as over 60% of all psychiatrists providing telepsychiatry are from Toronto Central, Hamilton Niagara Haldimand Brant, and Champlain LHINs, and patients in the North East, North West, and North Simcoe Muskoka LHINs receive almost half of all telepsychiatry consultations. It is interesting to note that while Champlain had more total psychiatrists providing telepsychiatry, it was not one of the 3 top providers of telepsychiatry appointments, which suggests that while they have more unique psychiatrists delivering telepsychiatry, they may not do so as frequently as psychiatrists in other LHINs may.
Our analysis also revealed that some LHINs provide substantial volumes of telepsychiatry to other LHINs while simultaneously receiving significant amounts of telepsychiatry services from psychiatrists in other LHINs. The rationale for this distribution model is unclear, but it warrants additional investigation and attention from a health systems planning perspective.
Finally, our findings have revealed opportunities to use telepsychiatry to increase access to outpatient psychiatric care for high-need patients, especially in rural areas after hospital discharge. An editorial by Gratzer and Goldbloom21 found that Canadians typically receive fragmented care and that in Ontario in particular, many patients first encounter the mental health care system in the emergency department. In addition, within Ontario, over two-thirds of people who have had a mental health or addiction-related hospitalisation do not receive postdischarge care within 1 week.19 Studies suggest that the absence of postdischarge follow-up strongly predicts early hospital readmission.22 The North East, North Simcoe Muskoka, and North West LHINs have the highest rates of mental illness and/or addiction hospitalisation (10.1, 7.9, and 7.8 per 100,000 people, respectively) compared to the provincial average of 5.3 per 100,000 people.19 With about 40% of in-need patients throughout the province failing to receive follow-up psychiatric care within a year and less than 1% of in-need patients accessing telepsychiatry in northern LHINs, there is likely great benefit to increasing planned access to outpatient telepsychiatry for high-need patients, especially in rural areas.
Strengths and Limitations
A cross-sectional research design using population-level administrative data provides the ability to analyse large amounts of data in a naturally occurring setting and the capacity to estimate prevalence and generate descriptive findings quickly and cost-effectively. However, administrative data do not provide insight into the reasons for the telepsychiatry service patterns we have observed. Qualitative methods could address some of the reasons for the patterns we have observed. As with most administrative data, our study is limited by the ability to capture consultations based on OHIP data. Psychiatry consultations that were not captured by OHIP, such as physician billing through alternate funding models (e.g., Family Health Team sessionals, which can include indirect consultations between the psychiatrist and clinicians/physicians) or non-OHIP billing (e.g., federally funded First Nations clients or third party), salaried physicians, or physicians who omitted submitting telemedicine billing codes, were not reflected in our analysis. For example, a large child and youth telepsychiatry program uses alternate funding, so it is possible that numbers for children and youth are underestimated. In addition, other nonpsychiatrist health care providers who do not bill OHIP, such as nurse practitioners and social workers, are not included in this study. As such, this analysis predominantly captures adult psychiatric care within Ontario. Finally, our study was challenged with defining need and access in terms that could be assessed with retrospective administrative data. While we realise that using hospitalisation for a psychiatric reason does not capture all individuals with need for mental health care, it provides a reasonable proxy of individuals who have been identified as requiring a psychiatric consultation. To our knowledge and despite these limitations, this study remains the most comprehensive description and evaluation of telepsychiatry service delivery published to date.
Conclusion and Next Steps
While telepsychiatry is a service delivery modality that can improve access to psychiatric care, it is currently underused by both psychiatrists and patients. To address this, future psychiatry training should include exposure to telepsychiatry to increase psychiatrist knowledge of and comfort with telepsychiatry,23 and future research should examine barriers to accessing and delivering telepsychiatry, including attitudes about technology, institutional and financial barriers, and health systems planning issues, among other factors. Certain telepsychiatry distribution patterns do not target a clear need or distribute care to reduce variations in access. While this study is the first evaluation of current trends and service utilisation patterns, a longer observation period to evaluate service trends and evaluate referral relationships between provider and patient sites could provide additional insights to the rationale. Future studies may include investigation of factors associated with the use of telepsychiatry, particularly to understand the rationale for deployment of telepsychiatry between LHINs with similar needs.
While patients in general are not currently using vast amounts of telepsychiatry, an extremely small number of high-need patients are currently using telepsychiatry for follow-up services after a psychiatric hospitalisation. Increased planning to connect high-need patients throughout Ontario with follow-up telepsychiatry care can help reduce the regional variability in access to outpatient care. Further research is needed to determine if telepsychiatry can meet the needs of acutely ill, at-risk populations, such as those with recent discharge from a psychiatric hospitalisation.24 In summary, our findings emphasise that telepsychiatry has the potential to be a helpful mode of service delivery to improve access to psychiatrists in regions with low supply, but the organisation of these services has not been developed in ways to maximise the potential for telepsychiatry to improve access.
Acknowledgements
The opinions, results, and conclusions reported in this paper are those of the authors and are independent from the funding sources. No endorsement by the Institute for Clinical Evaluative Sciences (ICES) or the Ontario Ministry of Health and Long-Term Care is intended or should be inferred. These data sets were linked using unique encoded identifiers and analysed at the ICES. This study was approved by the institutional review board at Sunnybrook Health Sciences Centre, Toronto, Canada.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Dr. Paul Kurdyak received operational grant funding from the Ministry of Health and Long-Term Care (MOHLTC) Health Services Research Fund Capacity Award (grant 06682). Dr. Kurdyak’s work is supported in part by the Medical Psychiatry Alliance, a collaborative health partnership of the University of Toronto, the Centre for Addiction and Mental Health, the Hospital for Sick Children, Trillium Health Partners, the Ontario MOHLTC, and an anonymous donor. This study was supported by the Institute for Clinical Evaluative Sciences, which is funded by an annual grant from the Ontario MOHLTC.
References
- 1. Chipps J, Brysiewicz P, Mars M. Effectiveness and feasibility of telepsychiatry in resource constrained environments? A systematic review of the evidence. Afr J Psychiatry (Johannesbg). 2012;15(4):235–243. [DOI] [PubMed] [Google Scholar]
- 2. Fortney JC, Pyne JM, Turner EE, et al. Telepsychiatry integration of mental health services into rural primary care settings. Int Rev Psychiatry. 2015;27(6):525–539. [DOI] [PubMed] [Google Scholar]
- 3. Frueh BC, Deitsch SE, Santos AB, et al. Procedural and methodological issues in telepsychiatry research and program development. Psychiatr Serv. 2000;51(12):1522–1527. [DOI] [PubMed] [Google Scholar]
- 4. Garcia-Lizana F, Munoz-Mayorga I. What about telepsychiatry? A systematic review. Prim Care Companion J Clin Psychiatry. 2010;12(2). pii: PCC.09m00831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Hilty DM, Ferrer DC, Parish MB, et al. The effectiveness of telemental health: a 2013 review. Telemed J E Health. 2013;19(6):444–454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Hilty D, Yellowlees PM, Parrish MB, et al. Telepsychiatry: effective, evidence-based, and at a tipping point in health care delivery? Psychiatr Clin North Am. 2015;38(3):559–592. [DOI] [PubMed] [Google Scholar]
- 7. O’Reilly R, Bishop J, Maddox K, et al. Is telepsychiatry equivalent to face-to-face psychiatry? Results from a randomized controlled equivalence trial. Psychiatr Serv. 2007;58(6):836–843. [DOI] [PubMed] [Google Scholar]
- 8. Rabinowitz T, Murphy KM, Amour JL, et al. Benefits of a telepsychiatry consultation service for rural nursing home residents. Telemed J E Health. 2010;16(1):34–40. [DOI] [PubMed] [Google Scholar]
- 9. Caxaj CS. A review of mental health approaches for rural communities: complexities and opportunities in the Canadian context. Canadian J Commun Mental Health. 2016;34(1):29–45. [Google Scholar]
- 10. Deslich S, Stec B. Telepsychiatry in the 21st century: transforming healthcare with technology. Perspect Health Inf Manag. 2013;10(Summer):1–17. [PMC free article] [PubMed] [Google Scholar]
- 11. O’Gorman LD, Hogenbirk JC, Warry W. Clinical telemedicine utilization in Ontario over the Ontario telemedicine network. Telemed J E Health. 2016;22(6):473–479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Shore JH, Hilty DM, Yellowlees P. Emergency management guidelines for telepsychiatry. Gen Hosp Psychiatry. 2007;29(3):199–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Hailey D, Ohinmaa A, Roine R. Limitations in the routine use of telepsychiatry. J Telemed Telecare. 2009;15(1):28–31. [DOI] [PubMed] [Google Scholar]
- 14. Lambert D, Gale J, Hartley D, et al. Understanding the business case for telemental health in rural communities. J Behav Health Serv Res. 2016;43(3):366–379. [DOI] [PubMed] [Google Scholar]
- 15. Meurk C, Leung J, Hall W, et al. Establishing and governing e-mental health care in Australia: a systematic review of challenges and a call for policy-focused research. J Med Internet Res. 2016;18(1):e10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Saeed SA, Bloch RM, Diamond J. Telepsychiatry: overcoming barriers to implementation. Curr Psychiatry. 2012;11(12):29. [Google Scholar]
- 17. Hermann R, Mattke S. Selecting indicators for the quality of mental health care at the health systems level in OECD countries. Paris: OECD Publishing; 2004. OECD Health Technical Papers, No. 17 http://dx.doi.org/10.1787/388745076135. [Google Scholar]
- 18. Canadian Institute for Health Information. Physician follow-up after hospital discharge: progress in meeting best practices. Ottawa (ON): CIHI; 2015. [Google Scholar]
- 19. Health Quality Ontario. Measuring up 2015: a yearly report on how Ontario’s health system is performing. Toronto (ON: ): Queen’s Printer for Ontario; 2015. [Google Scholar]
- 20. Kurdyak PA, Stukel T, Goldbloom D, et al. Universal coverage without universal access: a study of psychiatrist supply and practice patterns in Ontario. Open Med. 2014;8(3):87–99. [PMC free article] [PubMed] [Google Scholar]
- 21. Gratzer D, Goldbloom D. New government, new opportunity, and an old problem with access to mental health care. Can J Psychiatry. 2017;62(1):8–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Hamilton JE, Rhoades H, Galvez J, et al. Factors differentially associated with early readmission at a university teaching psychiatric hospital. J Eval Clin Pract. 2015;21(4):572–578. [DOI] [PubMed] [Google Scholar]
- 23. Crawford A, Sunderji N, López J, et al. Defining competencies for the practice of telepsychiatry through an assessment of resident learning needs. BMC Med Educ. 2016;16(1):1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Koblauch H, Reinhardt SM, Lissau W, et al. The effect of telepsychiatric modalities on reduction of readmissions in psychiatric settings: a systematic review. J Telemed Telecare [epub ahead of print 22 Sep 2016]. doi: 10.1177/1357633X16670285 [DOI] [PMC free article] [PubMed] [Google Scholar]