Abstract
This paper examines the spatial disparity between the HIV/AIDS service providers and the HIV/AIDS patients. The empirical focus is on Miami-Dade, a large metropolitan county in the United States with a Latino population majority and a high AIDS incidence rate. This exploratory study contributes to the existing literature on geographical access to health providers. Geographic Information System (GIS) is used to examine the spatial disparity between the service providers and the patients. The study reveals that aggregate-level analysis masks the reality of the spatial disparity. Miami Dade County’s Health Department focuses on aggregate zones for prioritizing its resources. At this level, there is little spatial disparity. However, evidence of spatial disparity emerges at the ZIP-code–level analysis. The major lesson from the study is that health policies need to be based on a finer-grained analysis to address spatial disparity.
Keywords: accessibility, geographic analysis, Miami, service providers, spatial disparity
INTRODUCTION
This paper presents exploratory research examining the spatial relationship between where HIV/AIDS service providers are geographically located and where HIV/AIDS patients reside. Previous research has documented that the location of health and social service providers is an important determinant for patients’ utilization of services, particularly among African Americans and Latinos (Logan, 1996; Mays, Cochran, & Sullivan, 2000). Geographical inaccessibility to patient services could increase health care disparities among the minority and other underserved populations (Heckman et al., 1998; Hendryx, Ahern, Lovrich, & McCurly, 2002; Hyndman & Holman, 2001). This geographic inaccessibility to health and social services may be further exacerbated by the lack of accessible transportation due to low car ownership rates (Raphael & Stoll, 2000) and inequitable access to public transit. Examining if spatial disparity exists between the location of HIV/AIDS patients and HIV/AIDS health care and social service providers is important to understanding the geographical accessibility of these providers. Few studies have focused on such spatial disparity; our study is a step toward filling this gap.
The issue of spatial disparity is examined in this paper using Miami-Dade County as the empirical case. The county provides a useful empirical base for examining the issue of spatial disparity because it is located in one of the largest urban metropolitan areas of the country afflicted with high HIV/AIDS incidence. It is among the top 10 largest counties in the United States with a population majority of Hispanic or Latino descent (henceforth referred to as Latinos for convenience). It had the highest reported AIDS annual rates among metropolitan areas in the United States (48.5 per 100,000 population) in 2006 according to the latest HIV/AIDS Surveillance Report (Centers for Disease Control and Prevention [CDC], 2008, p. 32). A majority of those who live with HIV/AIDS are African American (i.e., black) or Latino.
Geographic Information Systems (GIS) tools are used to analyze if there is spatial disparity between HIV service providers and patients in Miami-Dade County. Presently, Miami Dade County’s Health Department focuses on aggregate zones for prioritizing its resources. GIS analysis at the aggregate level reveals little disparity. However, evidence of spatial disparity emerges at the disaggregated ZIP-code level. Thus, policies for locating HIV/AIDS service providers based on aggregate-level zones masks the reality of the spatial disparity. This study points to the need for health policies to be based on more fine-grained analysis to address spatial disparity.
LITERATURE REVIEW
Although our literature review is mainly concerned with spatial disparity with respect to HIV/AIDS service providers and patients, it is set within the broader context of spatial disparity of health services in general. The location of service providers is an important element in patients’ accessibility and usage of health and social services. Research on the geography of health and social services has focused on the diffusion of physicians and other health care resources across different locations (Goodman, 2004; Guagliardo, 2004; Joseph & Phillips, 1984), intra- and inter-urban differences in service provision (Heckman et al., 1998; Hendryx et al., 2002), and the implications of the geographic disparity on health expenditures (Hirth, Tedisch, & Wheeler, 2001). Spatial disparity in terms of geographical inaccessibility is an additional barrier for equitable access to health care services faced by patients of minority groups like African Americans and Latinos, who already face disproportionate problems such as limited or no insurance coverage, cultural and linguistic obstacles, and the feeling that they are not being treated with respect by health care providers (Collins et al., 2002; Higgs, 2004; Hogue, Hargraves, & Collins, 2000; Smedley, Stith, & Nelson, 2003; Waters, 2000). According to Higgs, (2004), three broad factors affect spatial accessibility to health care services. They include (a) the spatial configuration and characteristics of the health delivery system, (b) the role of the transport system (private and public) in getting individuals to these destinations, and (c) the characteristics of individuals utilizing the health services.
Specifically with respect to HIV/AIDS, the spatial disparity in prevention, testing, social services, medical interventions, and end-of-life services could render such patients to have fewer choices when obtaining care (Hanchette, Gibbs, Fogarty, & Bruhn, 2002; Kaukinen & Fulcher, 2006). Although spatial disparity is an additional barrier for the HIV/AIDS patients to access health and social services, the research on such disparity is limited in the HIV/AIDS literature. One exception is the study by Fulcher and Kaukinen (2005), who analyzed the geographical distribution of five categories of HIV-related services in Toronto. They found some types of HIV-related services (e.g., emergency and preventive services) are geographically clustered, whereas other services (e.g., medical and end-of-life services) are more evenly distributed across the city. Indeed, their study is a useful guide for locating HIV/AIDS services to better serve the underserved populations in metropolitan areas. However, Fulcher and Kaukinen’s study concentrated only on the spatial distribution of the service providers; due to data unavailability, it did not take into account the geographical distribution of HIV/AIDS patients, who are in most need of these services. Simultaneous consideration needs to be paid both to the location of HIV/AIDS service providers and where HIV/AIDS patients reside to provide a more adequate guide for determining whether the location of such service providers is effectively catering to their target population needs.
This paper is a step toward filling the above gap in the literature by considering the location of service providers and HIV/AIDS patients simultaneously. The central question for our paper is: Is there a spatial disparity between where HIV/AIDS patients reside and where HIV/AIDS health care and social service providers are located? That is, we examine if the service providers are geographically accessible to the HIV/AIDS patients. The examination of geographical accessibility is important in that it allows service providers to be effectively utilized by patients (Gulliford & Morgan, 2003; Ricketts, 1997).
METHODS
We use GIS tools to examine the above question. Fundamentally, GIS is “a system of hardware, software, data, people, organizations, and institutional arrangements for collecting, storing, analyzing, and disseminating information about areas of the earth” (Dueker & Kjerne, 1989, pp. 7–8). It helps manipulate, analyze, and visually present information that is tied to a spatial location. At its core, GIS comprises two data components: spatial and attribute data. Spatial data represent locations and shapes (i.e., polygons, lines, and points) of geographic features (e.g., boundaries of census tracts, ZIP-codes, counties, states, etc.). Attribute data (qualitative or quantitative) provide the spatial characteristics that describe a geographical feature (e.g., population of a jurisdiction). GIS combines the data to provide a graphical representation of geographical features. Several attribute layers are combined to give a composite depiction of the feature. Program managers at the Centers for Disease Control and Prevention (CDC) have increasingly recognized the potential of GIS to organize and analyze information about HIV prevention services (Hanchette, Gibbs, Fogarty, & Bruhn, 2005). GIS has been adopted in the health care field to show the results of complex analyses (Richards, Croner, Rushton, Brown, & Fowler, 1999) and to assist in evidence based practices by community health organizations (Boulos, 2004). GIS provides useful tools to assess geographical access to health care services, a comprehensive review of which is covered by Graves (2008) and Higgs (2004).
A central dimension of spatial accessibility is the geographical distance, which gives the potential geographical accessibility of the patients to service providers (Guagliardo, 2004). In this, accessibility is conceptualized as the HIV/AIDS services available to the HIV/AIDS patients within their vicinity. Spatial disparity between the service providers and the patients would exist if the services are not within the vicinity of the patients. Previous studies have used 5 miles as an indicator for spatial accessibility since use of health services falls significantly beyond this level (Shannon, Bashshur, & Spurlock, 1978) and because it is considered to be physically close, within a medium-range driving distance (Cervero & Duncan, 2003; Gimpel & Schuknecht, 2003). Guagliardo (2004, p. 7) reported a shorter range of 3miles to define the cone of distance beyond which provider attractiveness becomes negligible. For our purposes, we have used the 5-mile distance as a rough measure of being “within the vicinity” of service providers. Adopting any threshold distance is bound to be problematic, since accessibility has several other dimensions (Rushton, 1999). Yet, the 5-mile distance measure gives a first-level estimate of the geographical accessibility of service providers.
We obtained data for the study from the Miami-Dade HIV/AIDS Partnership for service providers and the Miami-Dade County Health Department’s surveillance reports for HIV/AIDS patients. Since such information is in the public domain, the Institutional Review Board gave the study the “exempt” approval status for secondary data analysis. Addresses of the HIV/AIDS service providers were geocoded using ArcGIS 9.3 software. The software was also used to produce choropleth maps indicating the geographical distribution of the HIV/AIDS incidence. Multiple GIS methods (e.g., average nearest neighbor, hotspot analysis) were then used to analyze the spatial relationships between the service providers and the HIV/AIDS patients.
Background: HIV/AIDS in Miami-Dade County
The prevalence of HIV/AIDS incidence in Miami-Dade County, especially among minority groups, provides the background context for studying spatial disparity between HIV/AIDS service providers and patients. Until December 31, 2007, the cumulative number of reported adult AIDS cases since 1980 in the county was 30,532, and the cumulative number of reported adult HIV cases since July 1997 was 11,473 (Miami Dade County Health Department, 2008a, pp. 3, 9). Figure 1 summarizes the number of AIDS cases reported by the Ryan White CARE Act in Miami-Dade County and Florida from July 1995 to June 2005. As the figure shows, AIDS cases increased from 2002 onward in Florida as well as Miami-Dade County, with the county accounting for nearly a quarter of the reported cases.
FIGURE 1.
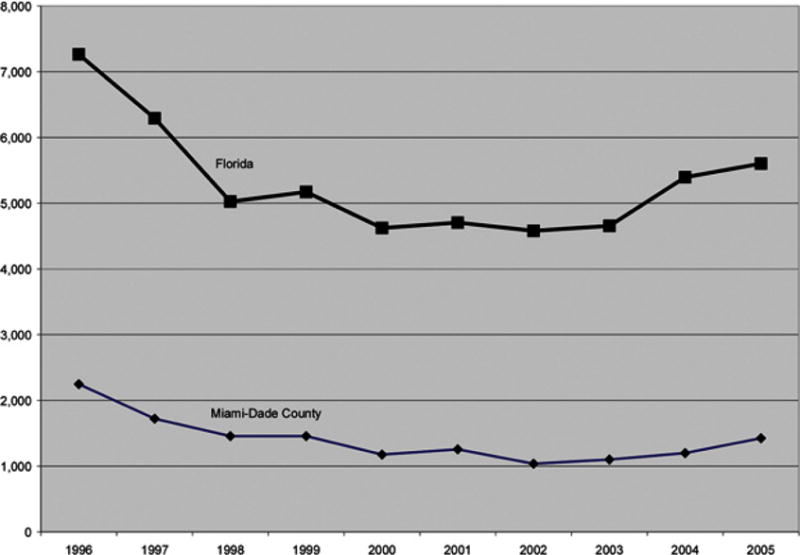
Reported AIDS cases by Ryan White CARE Act in Miami-Dade County and Florida, July 1995 through June 2005. Source: Centers for Disease Control and Prevention (CDC), 2006.
Demographically, Miami-Dade County is the only county in the United States with foreign-born population majority (which was 50.4% in 2007; U.S. Census Bureau, 2007a). In 2007, the county’s population was over 2.38 million, of which nearly 62% were Latinos. Immigrants of Cuban descent are the largest single population group, accounting for 51% of all Latino immigrants. Cubans are followed by Colombians, Nicaraguans, Hondurans, and Dominicans, who together make up approximately 70% of Latino immigrants (including Cubans) in Miami-Dade County. Partly due to its demographic characteristics, Miami-Dade has a high percentage of residents who have difficulty speaking English. Indeed, the county had the highest percentage of people 5 years of age or older who speak English less than “very well” (35.8%) in the United States (U.S. Census Bureau, 2007a).
The minority groups of African Americans and Latinos form the large share of Miami-Dade County’s HIV and AIDS cases. Table 1 shows the number of HIV and AIDS cases by race and ethnicity in the county between 2005 and 2007. African Americans constituted nearly half of HIV cases and over half of the AIDS cases since 2005; Latinos accounted for nearly two-fifths and one-third of the HIV and AIDS cases, respectively. Overall, the share of HIV cases fell by 1% for African Americans; among Latinos, it increased by 2% between 2005 and 2007. The share of AIDS cases increased among both African Americans and Latinos by 2% and 1%, respectively.
TABLE 1.
HIV and AIDS Cases by Ethnicity and Race in Miami-Dade County, 2005–2007
| Male
|
Female
|
Total
|
|||||||
|---|---|---|---|---|---|---|---|---|---|
| 2005 | 2006 | 2007 | 2005 | 2006 | 2007 | 2005 | 2006 | 2007 | |
| HIV (regardless of AIDS status) cases | |||||||||
| African American | 362 | 283 | 393 | 273 | 245 | 270 | 635 | 528 | 663 |
| Latino | 411 | 406 | 512 | 111 | 78 | 81 | 522 | 484 | 593 |
| White | 150 | 134 | 150 | 32 | 21 | 32 | 182 | 155 | 182 |
| Total | 933 | 832 | 1060 | 421 | 347 | 387 | 1354 | 1179 | 1447 |
| AIDS cases | |||||||||
| African American | 394 | 355 | 257 | 303 | 283 | 210 | 697 | 638 | 467 |
| Latino | 321 | 321 | 213 | 79 | 82 | 52 | 400 | 403 | 265 |
| White | 103 | 101 | 54 | 16 | 25 | 8 | 119 | 126 | 62 |
| Total | 832 | 788 | 534 | 402 | 394 | 277 | 1234 | 1182 | 811 |
Note: The “total” figure is not a sum of the African-American, Latino, and White since these are not exhaustive categories.
Source: Compiled from Miamic Dade County Health Department (2008c).
In terms of HIV/AIDS risk factors, Table 2 shows that men who have sex with men (MSM) represents the primary mode of exposure in HIV and AIDS cases. This is followed by heterosexual transmission and injection drug use (IDU). Although most of these risk factors indicate a downward trend between 2005 and 2007, unidentified risk factors have been on the rise. Based on their study of sex workers in Miami, Inciardi, Surratt, and Kurtz (2006) highlight not only unsafe sex but also the problems of drug abuse, homelessness, and other lifestyle factors that contribute to risky behaviors. Miami became the vanguard of circuit parties and related club drug use (e.g., ecstasy, ketamine, crystal methamphetamine) during the 1990s (Fernández et al., 2005; Kurtz, 2005). Miami-Dade County administers health education and risk reduction programs through health related communications, group- and community-level interventions, and a special initiative targeted toward Latinos to reduce the prevalence of risk factors. Location of the service providers is important for the effective utilization of their services.
TABLE 2.
HIV/AIDS Cases by Mode of Exposure, 2005–2007
| Male
|
Female
|
Total
|
|||||||
|---|---|---|---|---|---|---|---|---|---|
| 2005 | 2006 | 2007 | 2005 | 2006 | 2007 | 2005 | 2006 | 2007 | |
| HIV cases | |||||||||
| MSM | 576 | 497 | 560 | – | – | – | 576 | 497 | 560 |
| IDU | 45 | 31 | 38 | 37 | 23 | 21 | 82 | 54 | 59 |
| MSM/IDU | 35 | 34 | 25 | – | – | – | 35 | 34 | 25 |
| Heterosexual | 163 | 147 | 157 | 321 | 250 | 223 | 484 | 397 | 380 |
| Unidentified | 114 | 120 | 256 | 58 | 67 | 117 | 172 | 187 | 373 |
| Total | 933 | 829 | 1036 | 416 | 340 | 361 | 1349 | 1169 | 1397 |
| AIDS cases | |||||||||
| MSM | 440 | 445 | 245 | – | – | – | 440 | 445 | 245 |
| IDU | 73 | 43 | 38 | 49 | 49 | 23 | 122 | 92 | 61 |
| MSM/IDU | 51 | 48 | 26 | – | – | – | 51 | 48 | 26 |
| Hemophilia | 2 | 1 | 0 | 0 | 0 | 0 | 2 | 1 | 0 |
| Heterosexual | 181 | 173 | 122 | 315 | 295 | 200 | 496 | 468 | 322 |
| Other | 2 | 2 | 3 | 5 | 4 | 7 | 7 | 6 | 10 |
| Unidentified | 83 | 72 | 99 | 33 | 42 | 46 | 116 | 114 | 145 |
| Total | 832 | 784 | 533 | 402 | 390 | 276 | 1234 | 1174 | 809 |
Note: MSM = men who have sex with men; IDU = injection drug use.
Source: Compiled from Miamic Dade County Health Department (2008c).
The socioeconomic characteristics of Miami-Dade County exacerbate the HIV/AIDS epidemic. The county faces high levels of poverty, with a poverty rate of 15.3%, compared to the national rate of 13.0% (U.S. Census Bureau, 2007a, 2007b). The city of Miami has a significantly higher poverty rate of 25.5% and ranks among the top 10 poorest large cities in the United States (Bishaw & Simega, 2008, p. 25). The county’s residents (especially immigrants) have less ability to provide for basic services for their families, including health care services (Brookings Institution, 2004). Compared to other large counties, Miami-Dade County also had the highest rent burden among the 100 largest counties in the United States (Brookings Institution, 2004).
Last, minorities constitute a majority of the medically underserved population in the county and they face significant health disparities (Health Council of South Florida, 2008). They also face significant economic, cultural, and linguistic barriers to obtaining medical care. The cost of health care in Miami is the highest in country, nearly 21% more than the national average (Milliman Inc., 2009). Although Miami ranks high on the number of physicians per capita (Goodman, 2004), nearly 63% of Miami-Dade’s population live in areas designated as Medically Underserved Areas/Population by the U.S. Health Resources and Services Administration (Dalton, 2007; Graziosi, 2005). There is also a scarcity of community-based primary care centers/ programs in areas that accommodate large populations of new immigrants and lower-income groups. In the above context of social and cultural barriers, relative lack of medical services, and high incidence of HIV/AIDS, spatial disparity could enhance the already existing disparities among the minority groups.
FINDINGS
Spatial Distribution of Service Providers in Miami-Dade County
In our study, we consider the service providers as the “Ryan White & General Service Providers” administered by the Miami-Dade HIV/AIDS Partnership. The Ryan White program is the federal government program that supports HIV/AIDS-related health services. It is administered by the U.S. Department of Health and Human Services. It was first authorized in 1990, and is currently funded at $2.1 billion. The program works in conjunction with cities, states, and local community-based organizations to provide funds under different categories to service providers for the delivery of care to eligible patients. By and large, the program is for those who do not have sufficient health care coverage or the financial resources to cope with HIV. The majority of the program funds are used to support primary medical care and essential support services. A smaller portion is used to fund technical assistance, clinical training, and research on innovative models of care. The spatial distribution of these service providers with respect to patients is an important determinant for geographical accessibility of health services.
The county designated 33 “Ryan White & General Service Providers” to provide HIV/AIDS services. Many of these service providers offer more than one service. On average, each service provider offers nearly four services. Figure 2 gives the spatial distribution of the service providers in Miami Dade County, graded according to number of services. As the figure shows, most of the service providers, especially those with higher numbers of services, are located in the northeastern edge of the county. Indeed, most are located in the cities of Miami and Miami Beach. A fewer number of the service providers are located toward the south, in Homestead. Analysis of the “average nearest neighbor” in ArcGIS, which is used to interpret spatial clustering of point features, indicates that the “nearest neighbor ratio” is 0.64 (p < 0.001), indicating a very high degree of clustering of the service providers (a value of less than 1 of “nearest neighbor ratio” indicates clustering). The spatial clustering implies that HIV/AIDS patients will need to commute to this area to obtain health services.
FIGURE 2.
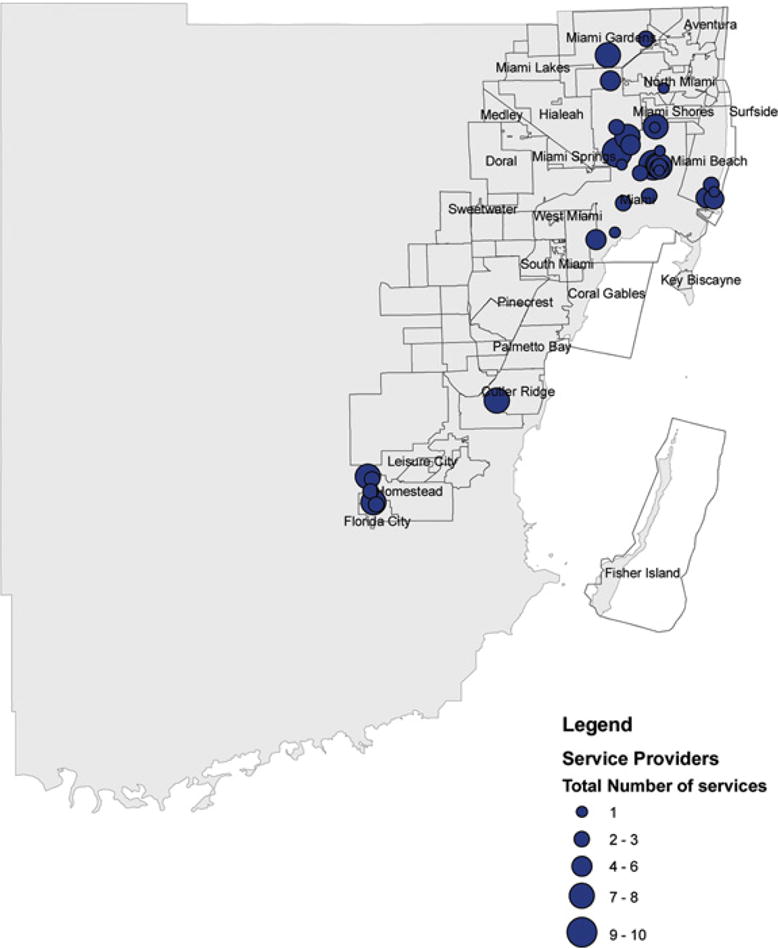
Geographical distribution of Ryan White Care Service Providers.
Florida’s Statewide Coordinated Statement of Need (SCSN) identified 13 services as the core services for HIV/AIDS patients funded by the Ryan White program (Florida Department of Health, 2008). However, additional services are funded according to the specific needs of each community. In Miami-Dade County, the range of services provided by the Ryan White and General Service Providers is summarized in Table 3. As the table shows, nearly 70% of the service providers are involved in case management. Most of the service providers have case management services because they are considered to be among the core services. The Ryan White CARE Act defines case management services as “a range of client-centered services that link clients with health care, psychosocial, and other services to insure timely, coordinated access to medically appropriate levels of health and support services, continuity of care, ongoing assessment of the clients’ and other family members’ needs and personal support systems, and inpatient case management services that prevent unnecessary hospitalization or that expedite discharge, as medically appropriate, from inpatient facilities” (Florida Department of Health, 2001). The case management tasks are undertaken by case management support staff, Ryan White Title II lead agency staff, the County Health Department personnel, and case managers.
TABLE 3.
Type of Services Provided by Ryan White and General Service Providers in Miami-Dade County
| Service | No. of service centers providing service | Percent of service centers providing service |
|---|---|---|
| Case management | 23 | 70% |
| Medical services | ||
| Outpatient medical care | 16 | 48% |
| The AIDS Drug Assistance Program | 15 | 45% |
| Prescription drugs | 11 | 33% |
| Dental care | 9 | 27% |
| Psychological counseling | 9 | 27% |
| Obstetrics and gynecology | 2 | 6% |
| Health insurance | 1 | 3% |
| Home health care | 1 | 3% |
| Psychiatry | 1 | 3% |
| Substance abuse | ||
| Outpatient Substance Abuse Center | 5 | 15% |
| Residential Substance Abuse Program | 3 | 9% |
| Family support services | ||
| Transport vouchers | 15 | 45% |
| Transportation services | 4 | 12% |
| Standard day care | 2 | 6% |
| Foster care | 1 | 3% |
| Intensive day care | 1 | 3% |
| Pastoral care | 1 | 3% |
| Other services | ||
| Outreach | 13 | 39% |
| Legal assistance | 2 | 6% |
| Food bank | 2 | 6% |
| Home delivery of meals | 2 | 6% |
| Shelter beds | 1 | 3% |
Among other core services, medical services such as outpatient medical care, AIDS Drug Assistance Program (ADAP), and prescription drugs are respectively provided by 48%, 45%, and 33% of the service providers. The outpatient medical care covers regular physician and specialist visits or nursing care in the physician’s office. The ADAP provides free medications for the treatment of HIV/AIDS and opportunistic infections; the program is aimed at increasing the longevity of those with HIV/AIDS and treating the symptoms of HIV infection. Other major core medical services include dental care and psychological counseling, which are provided by 27% of the service providers. Substance abuse treatment through Outpatient Substance Abuse Centers is carried out by only 15% of the service providers.
Family oriented support services are mainly related to providing transportation assistance, mostly in the form of vouchers (e.g., bus passes) (given by 45% of the service providers) and less so in the form of actual transportation services (given by 12% of the service providers). Very few family support services in the form of day care centers for children are available in Miami-Dade County. Some of the service providers give substance abuse treatment or counseling services. Although many service centers provide outreach services (39%), other services such as legal, food, and shelter services are fewer in number.
Spatial Distribution of HIV/AIDS Patients
The Miami-Dade County Health Department divides the county into 10 zones for HIV/AIDS surveillance. The HIV and AIDS cumulative incidence for the 10 zones (until December 2007) is summarized in Table 4. As the table shows, the most number (and greatest share) of cases are reported in Zone IV, which accounts for nearly 20% of the cases of AIDS and 17% of the HIV cases. Indeed, this zone, which comprises of the inner city areas of Liberty city and vicinity, has been one of the areas with high incidence of HIV/AIDS historically. Zone IV is followed by the adjacent Zones II, III, V, and VI. Zone II is the North Dade area and has the fourth highest number of cumulative adult AIDS and HIV cases. The coastal Zone III has had the second highest number of cumulative HIV cases and the fifth highest number of cumulative AIDS cases. The area includes South Beach, which is a popular tourist Mecca and has increasingly attracted the gay population since the 1990s (Holcomb and Luongo, 1996); MSM has been a major risk factor for HIV/AIDS in South Beach (Webster et al., 2005). Zone V is in North Central Dade, which has the second highest concentration of AIDS cases and the third highest concentration of HIV cases. Zone VI is closer to the downtown Miami and includes Little Havana, which has a high concentration of population with Cuban descent; this area has had the third highest number of AIDS cases and the fifth highest number of HIV cases. The HIV/AIDS incidence is comparatively lower in other zones, namely Zones I, VII, VIII, IX, and X. Zone I is similar to Zone II in terms of the share of HIV and AIDS cases. Zones VIII and IX are next in terms of the share of HIV and AIDS cases. Zones VII and X have the fewest HIV/AIDS cases.
TABLE 4.
Regional Distribution of Cumulative Reported AIDS and HIV Cases in Miami-Dade County through December 2007
| AIDS cases | HIV cases | Share of AIDS cases | Share of HIV cases | |
|---|---|---|---|---|
| Zone I (North West Dade) | 2383 | 1021 | 8% | 9% |
| Zone II (North Dade) | 3204 | 1267 | 10% | 11% |
| Zone III (Miami Beach and Vicinity) | 3097 | 1686 | 10% | 15% |
| Zone IV (Liberty City and Vicinity) | 6251 | 1983 | 20% | 17% |
| Zone V (North Central Dade) | 4314 | 1360 | 14% | 12% |
| Zone VI (Little Havana and Vicinity) | 3935 | 1229 | 13% | 11% |
| Zone VII (West Dade) | 1373 | 512 | 4% | 4% |
| Zone VIII (South Miami) | 2377 | 620 | 8% | 5% |
| Zone IX (South Dade) | 1821 | 655 | 6% | 6% |
| Zone X (South Dade) | 1220 | 449 | 4% | 4% |
| Uncategorized | 577 | 691 | 2% | 6% |
| 30,532 | 11,473 |
Note: Uncategorized include the homeless, those in the department of corrections, and the cases of wrong or no ZIP-codes.
Analysis at the zonal level indicates that there is little or no spatial disparity between the service providers and the HIV/AIDS cases. A GIS-based hotspot analysis (i.e., where HIV/AIDS incidences are concentrated) at the zonal level indicates that most cases are centered on Zone IV toward the north of the county (Fig. 3). GIS analysis shows that the adjacent Zones II, III, IV, V, and VI, which account for nearly 67% of the AIDS cases (and 66% of HIV cases), are also home to 81% of the service providers in the county. These zones are almost fully encompassed within the 5-mile buffer of the service providers. At the aggregate zonal level of analysis, thus, the service providers are overrepresented. The location of the service providers is not a surprise, given that HIV/AIDS incidence historically began in Zones IV and VI.
FIGURE 3.
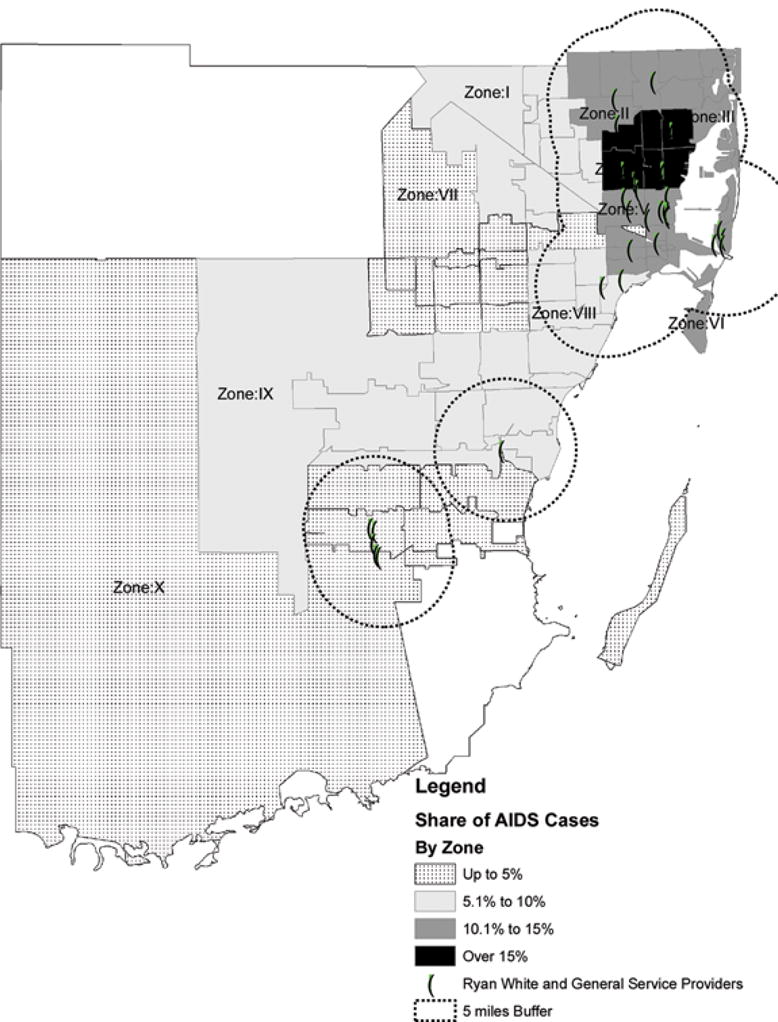
Geographic distribution of AIDS cases (until December 2007) by zone. Source: Based on Miamib Dade County Health Department (2008b).
Analysis at the zonal level, however, aggregates the HIV/AIDS cases and masks the fine-grained distribution of the cases in the county. Due to confidentiality issues, the data cannot be analyzed at the census tract level (for which data are not available). However, subzonal analysis at the ZIP-code level provides a better insight into the fine-grained pattern. Analysis at the sub-zonal level indicates that the geographic distribution at the zonal level is at variance from the ZIP-code level. Figure 4 shows the geographic distribution of the AIDS cases in the county based on ZIP-codes. The figure generally confirms the high incidence of HIV/AIDS in Zone IV and the northern segment of the county. The figure also confirms that there is some spread of HIV/AIDS cases toward the south of the county. However, unlike the zonal-level analysis, the ZIP-code–level data indicate that there is also a spread of HIV/AIDS incidences toward the west of the county. This is especially so in ZIP-code 33178, which consists of parts of Doral, Miami, and Medley. In the zonal-level analysis, the western part (Zones I and VII) does not indicate a high level of HIV/AIDS incidence; the ZIP-code–level analysis shows a different picture. Moreover, in the ZIP-code–level analysis, the spatial disparity is quite pronounced since these areas are outside of the 5-mile buffer zone from the service providers.
FIGURE 4.
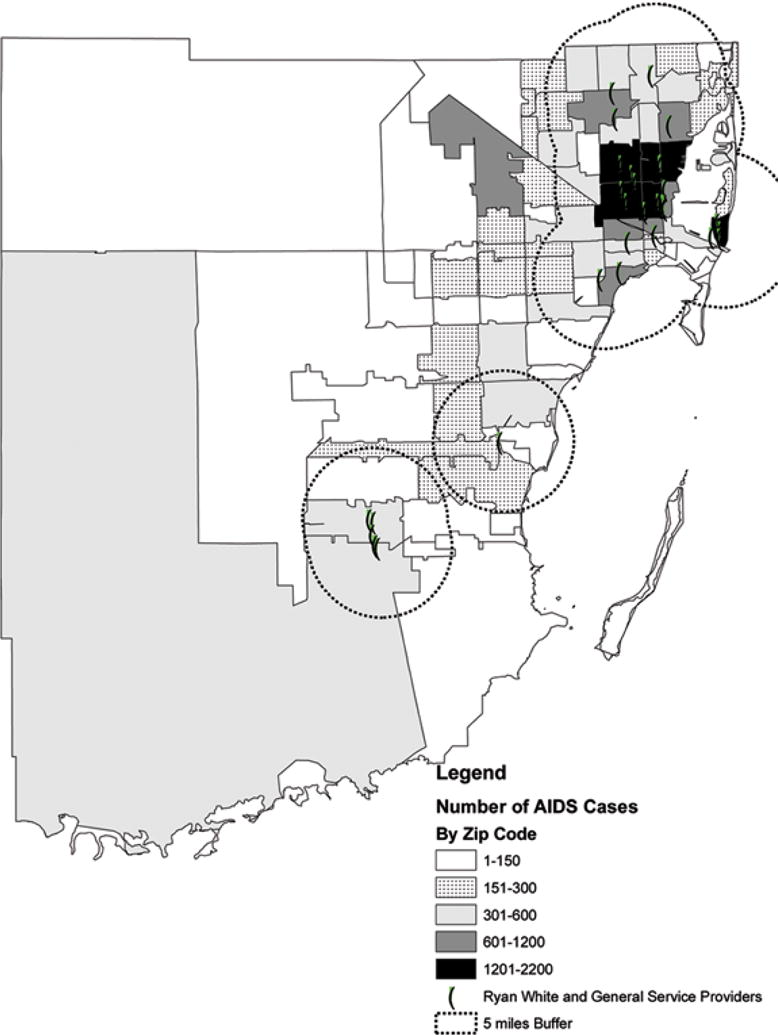
Geographic distribution of AIDS cases (until December 2007) by ZIP code. Source: Based on Miami-Dade County Health Department (2008b).
The geographical focus on zones in Miami-Dade County thus masks the deeper fine-grained distribution of HIV/AIDS in the county. The Miami-Dade County Health Department’s Prevention plan follows the zones, and gives priority to the zones with the highest concentration of HIV and AIDS cases (Miami-Dade County Health Department, 2008a). Following this priority, the Health Department has rightly prioritized the service providers’ resources in the northern segment of the county, centering on Zone IV. Although southern Miami-Dade County (Zones IX and X) does not have a high concentration of cases, a few service providers are located there since it has HIV/AIDS prone risk characteristics due to the migrant rural community. Yet, as our analysis shows, the broader zonal-level emphasis does not reflect the spread of HIV/AIDS. The ZIP-code–level analysis indicates a westward spread of the disease, but there are no service providers in that area of the county.
From a socioeconomic viewpoint, the Zone IV (Liberty City and vicinity) is a disadvantaged area in the county with a predominantly low-income and minority (mostly Blacks) population (Fig. 5) (Dunn & Stepick, 1992; Gainsborough, 2008). This zone encompasses the inner-city ghettoes, with high levels of drug trafficking, substance abuse, and prostitution (Martinez, Rosenfeld, & Mares, 2008; Nielsen, Martinez, & Lee, 2005). Hence, the concentration of most HIV/AIDS service providers in the vicinity of Zone IV is justified to a large extent. However, the concentration overlooks the spread of HIV/AIDS toward the west, where there is a critical need for the service providers. Demographically, the western part consists mainly of the Latino immigrants from Colombia, Venezuela, and other countries (Fig. 5).
FIGURE 5.

Service providers and distribution of African American and Latino population (2000). Source: Based on U.S. Census, 2000.
CONCLUSION
In this article, we have examined the issue of spatial disparity between the service providers and HIV/AIDS patients in Miami-Dade County. Spatial disparity is an important consideration for the accessibility of services to patients. Our article reveals that aggregate-level analysis could mask the reality of the spatial disparity found in a more fine-grained geographical analysis. In the case of Miami-Dade County, the zonal-level analysis does not reflect spatial disparity between the service providers and the HIV/AIDS patients in the county. However, such disparity becomes evident at the ZIP-code level. Since the county’s health policies are focused on zones, the policies do not account for the finer grained health needs that have emerged within pockets of the zones due to higher incidence of the HIV/AIDS.
The study has broader implications for the geographical accessibility of service providers. State and metropolitan agencies typically fund HIV/AIDS service providers based on larger administrative jurisdictions. Such funding allocation may indeed be administratively justified for prioritizing HIV/AIDS resources. However, such broad administrative division could mask the reality of geographical accessibility at the local level. Policies for locating HIV/AIDS service providers thus need to be more sensitive to the local level accessibility at a more fine-grained level. That is, the service providers need to be located in the vicinity of those areas that have high demand for such services for better geographical accessibility. In this, Public Participation GIS (PPGIS), which has emerged as a powerful tool to empower local communities, could be a useful tool to locate HIV/AIDS service providers (Vanmeulebrouk, Ulrike, Ricketts, & Loudon, 2008).
Although our paper presents some interesting findings, the study is principally an exploratory one. The GIS methods were also exploratory in nature. The study presents several possibilities for future research directions. First, further study incorporating spatial statistical methods is required to quantify the nature of the spatial disparity between the service providers and the HIV/ AIDS patients. We have not incorporated such statistical methods due to data limitations on HIV/AIDS patients. Second, although we did make an advancement over Fulcher and Kaukinen (2005) in considering the service providers simultaneously with the patients (rather than the accessibility to general population), our analysis implicitly assumes that patients will access nearby service providers. We have not accounted for the actual catchment areas of the service providers (e.g., ZIP-codes from which the patients come to a particular provider) and the travel patterns of the patients. Such a consideration is required to find out the patient pool for each provider. For example, we have assumed a 5-mile buffer for geographical accessibility. Although this may be a generous assumption, service providers at a greater distance with better public transportation routes could be more accessible than assumed in this study. Surveys of service providers and HIV/AIDS patients are required to account for the catchment areas and the travel behavior. Third, our study focuses only on Miami-Dade County; it would be interesting to see if the findings apply to other counties. A comprehensive study covering major metropolitan regions with high HIV/AIDS prevalence is required for more informed policy measures.
Results from this study need to be considered in light of other limitations. First, distance is one among the many other considerations for accessibility. Although GIS analysis may better inform policymakers about geographical accessibility, GIS may not be the only basis for allocating resources. Other epidemiological, social, and economic concerns also shape such resource allocation. Second, our study is limited to ZIP-code–level analysis, since data are only available up to this level. However, a more fine-grained analysis should be based on census tract information. We have not used census tract level analysis due to data unavailability. Although such analysis could be more informative, privacy concerns regarding HIV/AIDS patients also need to be taken into account. Balancing the need for information and privacy is a larger policy debate that is beyond the scope of this paper but needs to be considered in future studies.
Acknowledgments
The authors would like to thank the Center for Research on U.S. Latinos HIV/AIDS and Drug Abuse (CRUSADA) at the Florida International University for its generous funding of this research.
Contributor Information
SUKUMAR GANAPATI, Department of Public Administration, Florida International University, Miami, Florida, USA.
N. EMEL GANAPATI, Department of Public Administration, Florida International University, Miami, Florida, USA.
MARIO De La ROSA, School of Social Work, Florida International University, Miami, Florida, USA.
PATRIA ROJAS, School of Social Work, Florida International University, Miami, Florida, USA.
References
- Bishaw A, Simega J. Income, earnings, and poverty data from the 2007 American Community Survey. Washington, DC: U.S. Census Bureau; 2008. (American Community Survey Reports, ACS-09). Retrieved June 302009 , from http://www.census.gov/prod/2008pubs/acs-09.pdf. [Google Scholar]
- Boulos M. Towards evidence-based, GIS-driven national spatial health information infrastructure and surveillance services in the United Kingdom. International Journal of Health Geographics. 2004;3(1):1–50. doi: 10.1186/1476-072X-3-1. Retrieved September 30, 2008, from http://www.ij-healthgeographics.com/content/pdf/1476-072X-3-1.pdf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brookings Institution (Center on Urban, and Metropolitan Policy) Growing the middle class: Connecting all Miami-Dade residents to economic opportunity. Washington, DC: Brookings Institution; 2004. [Google Scholar]
- Centers for Disease Control and Prevention. AIDS cases by state and metropolitan area, provided for the Ryan White CARE Act, June 2005. HIV=AIDS Surveillance Supplemental Report 2005. 1. Vol. 11. Atlanta: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; 2006. Retrieved September 30, 2008, from: http://www.cdc.gov/hiv/topics/surveillance/resources/reports/2005supp_vol11no1/default.htm. [Google Scholar]
- Centers for Disease Control and Prevention. Cases of HIV infection and AIDS in the United States and Dependent Areas, 2006. HIV/AIDS Surveillance Report. 18. Atlanta: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; 2008. 2006. Retrieved September 30 2008, from http://www.cdc.gov/hiv/topics/surveillance/resources/reports/ [Google Scholar]
- Cervero R, Duncan M. Walking, bicycling, and urban landscapes: Evidence from the San Francisco bay area. American Journal of Public Health. 2003;93(9):1478–1483. doi: 10.2105/ajph.93.9.1478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins KS, Hughes DL, Doty MM, Ives BL, Edwards JN, Tenney K. Diverse communities, common concerns: Assessing health care quality for minority Americans. Washington, DC: The Commonwealth Fund; 2002. [Google Scholar]
- Dalton R. US higher education: Medicinal properties. Nature. 2007;446(7139):971–972. doi: 10.1038/446971a. [DOI] [PubMed] [Google Scholar]
- Dueker K, Kjerne D. Multipurpose cadastre: Terms and definitions. Falls Church, VA: American Society for Photogrammetry and Remote Sensing and American Congress on Surveying and Mapping (ASPRS-ACSM); 1989. [Google Scholar]
- Dunn M, Stepick A. Blacks in Miami. In: Grenier GJ, Stepick A, editors. Miami now: Immigration, ethnicity, and social change. Gainesville, FL: University Press of Florida; 1992. [Google Scholar]
- Fernández MI, Bowen GS, Varga LM, Collazo JB, Hernandez N, Perrino T. High rates of club drug use and risky sexual practices among Hispanic men who have sex with men in Miami, Florida. Substance Use & Misuse. 2005;40(9–10):1347–1362. doi: 10.1081/JA-200066904. [DOI] [PubMed] [Google Scholar]
- Florida Department of Health. HIV/AIDS case management standards and guidelines. 2001 Retrieved September 30 2008, from http://www.doh.state.fl.us/Disease_ctrl/aids/care/cmstands.pdf.
- Florida Department of Health. HIV/AIDS patient care comprehensive plan & statewide coordinated statement of need 2009–2012. 2008 Retrieved June 30 2009, from http://www.doh.state.fl.us/Disease_ctrl/aids/PCCP_final.pdf.
- Fulcher C, Kaukinen C. Mapping and visualizing the location HIV service providers: An exploratory spatial analysis of Toronto neighborhoods. AIDS Care. 2005;17(3):386–396. doi: 10.1080/09540120512331314312. [DOI] [PubMed] [Google Scholar]
- Gainsborough JF. A tale of two cities: Civic culture and public policy in Miami. Journal of Urban Affairs. 2008;30(4):419–435. [Google Scholar]
- Gimpel JG, Schuknecht JE. Political participation and the accessibility of the ballot box. Political Geography. 2003;2(5):471–488. [Google Scholar]
- Goodman DC. Twenty-year trends in regional variations in the U.S. physician workforce. Health Affairs Web Exclusive, 90–97. 2004 doi: 10.1377/hlthaff.var.90. Retrieved September 30 2008, from http://content.healthaffairs.org/cgi/reprint/hlthaff.var.90v1.pdf. [DOI] [PubMed]
- Graves BA. Integrative literature review: A review of literature related to geographical information systems, health care access, and health outcomes. Perspectives in Health Information Management. 2008;5(11):1–13. [PMC free article] [PubMed] [Google Scholar]
- Graziosi GH. Distribution of medically underserved areas and populations-MUA/P-in Florida (Appendix 1) Florida International University: Proposal for a program in allopathic medicine. 2005 Submitted to Florida Board of Governors. [Google Scholar]
- Guagliardo MF. Spatial accessibility of primary care: Concepts, methods and challenges. International Journal of Health Geographics. 2004;3(3):1–13. doi: 10.1186/1476-072X-3-3. Retrieved September 30 2009, from http://www.pubmedcentral.nih.gov/picrender.fcgi?artid=394340&blobtype=pdf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gulliford M, Morgan M, editors. Access to health care. London/New York: Routledge; 2003. [Google Scholar]
- Hanchette CL, Gibbs D, Mobley L, Bruhn M, Rickman E. Geoanalysis of HIV prevention services provided by CDC Funded Community-Based Organizations (CBOs) (Final Report) Atlanta: Centers for Disease Control and Prevention (Division of HIV/AIDS Prevention); 2002. Retrieved September 30 2008, from http://aspe.hhs.gov/pic/pdf/7840.pdf. [Google Scholar]
- Hanchette C, Gibbs DA, Fogarty KJ, Bruhn M. A national, geographic database of CDC-funded HIV prevention services: Development challenges and potential applications. International Journal of Health Geographics. 2005;4(28):1–12. doi: 10.1186/1476-072X-4-28. Accessed September 30, 2008, from http://www.ij-healthgeographics.com/content/4/1/28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Health Council of South Florida. Racial and ethnic health disparities in Miami-Dade County. Prepared for the Miami-Dade County Health Department; 2008. Retrieved June 30 2009, from http://www.healthcouncil.org/publications/Racial_and_Ethnic_Health_Disparities_in_Miami_Dade.pdf. [Google Scholar]
- Heckman T, Somlai A, Peters J, Walker J, Otto L, Galdabini C, Kelly J. Barriers to care among persons living with HIV/AIDS in urban and rural areas. AIDS Care. 1998;10(3):365–375. doi: 10.1080/713612410. [DOI] [PubMed] [Google Scholar]
- Hendryx M, Ahern M, Lovrich N, McCurdy A. Access to health care and community social capital. Health Services Research. 2002;37(1):87–103. [PubMed] [Google Scholar]
- Higgs G. A literature review of the use of GIS-based measures of access to health care services. Health Services & Outcomes Research Methodology. 2004;5(2):119–139. [Google Scholar]
- Hirth RA, Tedischi PJ, Wheeler JR. Extent and sources of geographic variation in medicare and end-stage renal disease expenditures. American Journal of Kidney Diseases. 2001;38(4):824–831. doi: 10.1053/ajkd.2001.27702. [DOI] [PubMed] [Google Scholar]
- Hogue C, Hargraves M, Collins KS, editors. Minority health in America: Findings and policy implications from the Commonwealth Fund Minority Health Survey. Baltimore, MD: The Johns Hopkins University Press; 2000. [Google Scholar]
- Holcomb B, Luongo M. Gay tourism in the United States. Annals of Tourism Research. 1996;23(3):711–713. [Google Scholar]
- Hyndman J, Holman J. Accessibility and spatial distribution of general practice services in an Australian city by level of social disadvantage. Social Science & Medicine. 2001;53(12):1599–1609. doi: 10.1016/s0277-9536(00)00444-5. [DOI] [PubMed] [Google Scholar]
- Inciardi JA, Surratt HL, Kurtz SP. HIV, HBV, and HCV infections among drug-involved, inner-city, street sexworkers in Miami, Florida. AIDS and Behavior. 2006;10(2):139–147. doi: 10.1007/s10461-005-9049-3. [DOI] [PubMed] [Google Scholar]
- Joseph AE, Phillips DR. Accessibility and utilization: Geographical perspectives on health care. New York: Harper & Row; 1984. [Google Scholar]
- Kaukinen C, Fulcher C. Mapping the social demography and location of HIV services across Toronto neighbourhoods. Health & Social Care in the Community. 2006;14(1):37–48. doi: 10.1111/j.1365-2524.2005.00595.x. [DOI] [PubMed] [Google Scholar]
- Kurtz SP. Post-circuit blues: Motivations and consequences of crystal meth use among gay men in Miami. AIDS and Behavior. 2005;9(1):63–73. doi: 10.1007/s10461-005-1682-3. [DOI] [PubMed] [Google Scholar]
- Logan S. The black family: Strengths, self-help, and positive change. Boulder, CO: Westview Press; 1996. [Google Scholar]
- Martinez R, Rosenfeld R, Mares D. Social disorganization, drug market activity, and neighborhood violent crime. Urban Affairs Review. 2008;43(6):846–874. doi: 10.1177/1078087408314774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mays V, Cochran S, Sullivan J. Health care for African American and Hispanic women: Report on perceived health status, access to care, and utilization patterns. In: Hogue C, Hargraves M, Collins KS, editors. Minority health in America: Findings and policy implications from the Commonwealth Fund Minority Health Survey. Baltimore: The Johns Hopkins University Press; 2000. [Google Scholar]
- Miami-Dade County Health Department. HIV/AIDS surveillance: Monthly surveillance report, December 2007. 2008a Accessed September 30 2008, from http://www.dadehealth.org/downloads/Dec-2007.pdf.
- Miami-Dade County Health Department. Miami-Dade County neighborhood profiles. 2008b Retrieved September 30 2003, from http://www.dadehealth.org/hiv/HIVprofiles.asp.
- Miami-Dade County Health Department. Number of reported AIDS and HIV cases in 2005 2006 and 2007. 2008c Retrieved September 30, 2008, from http://www.dadehealth.org/hiv/HIVsurveillance.asp.
- Miami-Dade HIV/AIDS Partnership. Ryan White program service providers & services. 2008 Retrieved September 30 2008, from http://www.aidsnet.org/main/mainpages/providers.html.
- Milliman, Inc. Milliman medical index, 2009. 2009 Retrieved June 30 2009, from http://www.milliman.com/expertise/healthcare/products-tools/mmi/pdfs/milliman-medical-index-2009.pdf.
- Nielsen AL, Martinez R, Lee MT. Alcohol, ethnicity, and violence: the role of alcohol availability for Latino and Black aggravated assaults and robberies. The Sociological Quarterly. 2005;46(3):479–502. [Google Scholar]
- Raphael S, Stoll MA. (Berkeley Program on Housing and Urban Policy Working Paper #W00-002).Can boosting minority car-ownership rates narrow inter-racial employment gaps? 2000 [Google Scholar]
- Richards TB, Croner CM, Rushton G, Brown CK, Fowler L. Geographic information systems and public health: Mapping the future. Public Health Reports. 1999;114:359–373. doi: 10.1093/phr/114.4.359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ricketts TC. Using geographic methods to understand health issues. Rockville, Md: Agency for Health Care Policy and Research Dept. of Health and Human Services, U.S. Public Health Service; 1997. (AHCPR Publication No. 97-NO13). [Google Scholar]
- Rushton G. Methods to evaluate geographic access to health services. Journal of Public Health Management Practice. 1999;5(2):93–100. [PubMed] [Google Scholar]
- Shannon GW, Bashshur RL, Spurlock CW. The search for medical care: An exploration of urban black behavior. International Journal of Health Service. 1978;8(3):519–530. doi: 10.2190/0F28-23GM-42K0-PQDN. [DOI] [PubMed] [Google Scholar]
- Smedley BD, Stith AY, Nelson AR, editors. Unequal treatment: Confronting racial and ethnic disparities in health care. Washington, DC: The National Academies Press; 2003. Retrieved September 30 2008, from http://www.nap.edu/catalog.php?record_id=10260. [PubMed] [Google Scholar]
- U.S. Census Bureau. 2007 American Community Survey, data profile, Miami-Dade County. Washington, DC: U.S. Census Bureau; 2007a. [Google Scholar]
- U.S. Census Bureau. 2007 American Community Survey, data profile, United States. Washington, DC: U.S. Census Bureau; 2007b. [Google Scholar]
- Vanmeulebrouk B, Ulrike U, Ricketts A, Loudon M. Open source GIS for HIV/AIDS management. International Journal of Health Geographics. 2008;7(53):1–16. doi: 10.1186/1476-072X-7-53. Retrieved June 30, 2009, from http://www.ij-healthgeographics.com/content/pdf/1476-072X-7-53.pdf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waters H. Measuring equity in access to health care. Social Science and Medicine. 2000;51(4):599–612. doi: 10.1016/s0277-9536(00)00003-4. [DOI] [PubMed] [Google Scholar]
- Webster RD, Darrow WW, Paul JP, Roark RA, Taylor RA, Stempel RR. Community planning, HIV prevention, and a needs assessment for men who have sex with men: The South Beach health survey. Sexually Transmitted Diseases. 2005;32(5):321–327. doi: 10.1097/01.olq.0000159211.40719.2b. [DOI] [PubMed] [Google Scholar]


