Abstract
Purpose
The role of radiotherapy for unresectable pancreatic cancer is controversial. A benefit of additional radiotherapy is supported by some observations. A dose-effect relationship was recently found by dose escalation employing image guided and intensity modulated radiotherapy.
Methods
We retrospectively evaluated 28 consecutive patients, all with history of extensive prior therapies for unresectable locally advanced/ recurrent pancreatic cancer (LAPC/LRPC). Treatment was delivered by helical tomotherapy after daily position verification with computed tomography. Dose to the planned target volume (PTV) was 51 Gy, while the dose to the macroscopic tumor was escalated by a simultaneous integrated boost to a median cumulative dose of 66 Gy (60–66 Gy). Concomitant chemotherapy consisted mainly of capecitabine (n = 23).
Results
10 of 28 patients presented acute toxicities > grade 2, one patient succumbed to gastrointestinal bleeding after treatment. No correlations of toxicities and dose volume histograms (DVH) of retrospectively delineated small bowel loops were observed, although average small bowel volume receiving ≥ 20 Gy was 374 ml. DVH analyses revealed a correlation of splenic parameters and acute toxicity: Vomiting, anorexia, dehydration, hematologic toxicity, fatigue, combined gastro-intestinal toxicity wit R-values between 0.392 and 0.561 (all p-values > 0.05). Only one patient developed late toxicities > grade 2. With an average follow-up time in surviving patients of 14 months median overall survival time was 19 months and median time to local recurrence 13 months. In 8 patients with available imaging of local recurrence: 5 in field recurrences, 2 marginal recurrences and one lymph node recurrence outside the high dose radiation field were observed. In univariate analysis only ΔCA-19-9 during radiotherapy was associated with local control (p = 0.029) and overall survival (p = 0.049).
Conclusion
Dose escalated normo-fractionated radiotherapy for LAPC/LRPC seems feasible and suitable to prolong local control and in consequence long-term survival. However, in-field local progression is still frequently observed and possibilities to increase the local effectiveness should be evaluated. Exposure of the spleen was predictive for acute toxicity and should be further investigated.
Introduction
Pancreatic cancer is an aggressive disease with unfavourable prognosis. Even for localized stages, the 5 year overall survival rate after curative resection and adjuvant chemotherapy is only around 20% [1,2]. For locally advanced stages (LAPC) unable to undergo surgery, the patients´ outcome is dismal and the goal of the treatment is survival prolongation and symptom control with a median overall survival (OS) between 5 to 11 months [3]. The prognosis for isolated locally recurrent pancreatic carcinomas is similar to initial LAPC with reported median overall survival around 6 months [4] if patients are not eligible for re-surgery [5,6].
The role of radiotherapy (RT) for LAPC (or LRPC) is controversial due to the high prevalence of distant metastases (long-term up to 70%) and the radiosensitivity of surrounding organs at risk (OAR) in the upper abdomen. As a consequence, the design of any study to evaluate the impact of radiotherapy is critical. First patient selection is crucial, because only in about 30% of patients outcome potentially could be improved by intensifying local treatment. Second the intolerances in the upper abdomen can mislead to prescribe ineffective radiotherapy schedules in order to avoid high toxicity.
In a couple of renowned studies radiochemotherapy (RCT) was evaluated, which combines sensitizing chemotherapy schemes with a more or less effective radiotherapy scheme. The sensitizing chemotherapy schedules were based on 5-FU or capecitabine and have only a limited systemic effect. The radiotherapy has been prescribed either as split-course schemes of 20 x 2 Gy until 40 Gy of low effectivity [1,7] or as standard schemes of 30 x 1.8 Gy until 54 Gy [8] or 30 x 2 Gy until 60 Gy [9]. These less effective RCT approaches are not able to improve a systemic chemotherapy [1,7] and are inferior, if they are applied front-line and replace or delay an effective systemic chemotherapy [1,9] because a large proportion of patients have already undetected dissemination and do not benefit from an early local treatment. Therefore, induction chemotherapy and re-staging was recommended to select patients for an additional consolidative RCT [10,11]. However even in a second-line approach (after 4 cycles of gemcitabine) RCT (54 Gy plus capecitabine) was not superior to a continuation of the gemcitabine chemotherapy in terms of overall survival [8]. Nevertheless a trend for improved progression-free survival was observed, probably caused by sustained local control.
In an ECOG-trial [12] initial RCT with gemcitabine (600 mg/sqm weekly plus 28 x 1.8 Gy until 50.4 Gy) was compared with gemcitabine 1000 mg/sqm weekly for six weeks, both arms followed by five cycles of gemcitabine at full dosage. Improved survival was found in the RCT arm. In this example, full systemic chemotherapy was only slightly reduced during radiotherapy and patients undergoing radiotherapy demonstrated improved overall survival.
On summary, the optimal usage of radiotherapy for LAPC is still under debate. Current data suggests that a consolidative approach after completing systemic treatment options and careful restaging might be reasonable. A positive role of post-operative radiotherapy was confirmed by a large retrospective analysis [13] which identified radiotherapy in addition to adjuvant chemotherapy as a favorable prognostic indicator for survival.
In a recent retrospective analysis focal radiation dose escalation seemed beneficial for patients with LAPC. Krishnan and colleagues reported on 47 patients that received dose escalation by a simultaneous integrated boost (SIB) and found improved overall survival when comparing these patients to a group of non-dose-escalated patients [14]. Due to the surrounding normal tissues dose-escalation within the upper abdomen can be challenging and the exact dose-response evaluation of LAPC as well as OAR is a matter of ongoing debate. Further information on dose-volume parameters and recurrence patterns is therefore provided by this study.
Patients and methods
Ethics
The data analysis for this study was approved by the Charité ethical review committee (EA1/236//16). Each participant provided written informed consent for publication of pseudonymized data.
Patient characteristics
28 patients were treated between November 2012 and August 2016 for non-resectable LAPC (n = 15) or local recurrent pancreatic cancer after prior radical resection (n = 13). Radical resection consisted of pancreaticojejunostomy (n = 7), pancreatigogastrotomy (n = 5) or distal pancreatectomy (n = 1). The pancreatojejunostomy was performed in mattress positioning U-stitches (4–0 PDS with a MH1 needle) starting at the jejunal back wall, going from back to front, straight through the pancreatic remnant about 1 cm distal from the cut surface. Then the sutures were placed through the front wall of the jejunal loop. The suture than was brought straight through the pancreatic remnant.
The pancreatogastrotomy was performed also in mattress technique using U-stitches (4–0 PDS with a MH1 needle). After incision of the dorsal and ventral stomach the pancreatic remnant has been positioned into the dorsal stomach. The suture than was brought through the pancreas and the dorsal wall of the stomach. After that the ventral stomach was closed with sutures.
In case of distal pancreatectomy the pancreatic remnant closure after distal pancreatectomy has been performed using hand-sewn suturing of the pancreas without any anastomosis. All patients gave written informed consent and approval to conduct this study was obtained by the local Ethics Committee. Patients described here were heavily pre-treated, all patients received prior chemotherapy, either adjuvant after resection or in palliative intent or both. 7 out of 28 patients presented with distant metastases. These metastases were either regarded oligo-metastatic and underwent high dose radiotherapy (n = 3) or were in complete remission after palliative chemotherapy (n = 4). One additional patient who received high-dose neoadjuvant RCT was included for analysis of dose volume histograms and correlation with acute toxicity.
Treatment, delineation and follow-up
Target and OAR delineation were performed using a contrast enhanced computed tomography (CT) and rigid registration of CT scans with with pancreatic protocol and oral contrast agent for bowel delineation and FDG-PET for tumor delineation whenever available. All patients were treated with helical tomotherapy with daily megavoltage CT (MVCT) position verification. Dose prescription was based on a prior pilot study that showed good treatment tolerability [15] and commonly consisted of 30 fractions of 1.7 Gray (Gy) to a total dose of 51 Gy to the planned treatment volume (PTV), which compromised the extended tumor region and regional lymphatic nodes (defined as clinical target volume = CTV with a safety margin of 5mm). CTV delineation was based on the risk of lymph node involvement proposed by Sun and colleagues [16]. For tumors of the pancreatic head posterior pancreatiocoduodenal, superior mesenteric and paraaortic nodes were included. For tumors of the pancreatic body or tail the lymphatic drainage around the splenic artery was partially included. Dose to the macroscopic tumor volume was escalated by a simultaneous integrated boost (SIB) with a single fraction dose of 2.2 Gy leading to a cumulative dose of 66 Gy. SIB dose prescription was reduced to 60 and 64.5 Gy in two patients due to OAR constraint infringing large macroscopic tumor volumes. The following OAR were contoured for clinical and investigational purposes: Stomach, small bowel loops, peritoneal cavity, spleen, kidneys, liver and spinal canal. Treatment planning and adherence to normal tissue constraints were based on peritoneal cavity while small bowel loops and spleen were retrospectively delineated and evaluated. Delineation was consensually performed by the same experienced radiation oncologist/radiologist (PW, SZ). 24 patients received simultaneous chemotherapy with either capecitabine (21 patients received 825 mg/m2 bi-daily, 2 patients received dose reduction, n = 23) or gemcitabine (600 mg/mq weekly, n = 1). All but one patient received > 90% of fractions by tomotherapy and the remaining one or two fractions by volumetric arc therapy, in the latter one only 15 fractions were delivered as planned and the remaining 15 fractions had to be re-planned on volumetric arc radiotherapy (VMAT) due to temporary breakdown of tomotherapy.
Toxicity was scored on a weekly basis based on Common Terminology Criteria for Adverse Events (CTCAE), version 4.0. Acute toxicity was defined as occurring during and up to 3 months after completion of radiotherapy (RT). Late toxicity was defined as occurring > 3 months after RT completion. Before and during the last week of or immediately after radiotherapy levels of serological tumor markers CEA and CA-19-9 were registered along with differential blood counts (the corresponding values are labeled with the suffixes preRT and postRT). For patients with normal Bilirubin levels percentual change of CA-19-9 during therapy was calculated as follows:
Follow-up visits were usually performed at least each three months after terminating RT. Commonly follow-up included CT scans of the upper abdomen and lung and/ or abdominal sonography. In case of clinical uncertainties patients were referred for whole body FDG-PET-CT. Loco-regional tumor response at the first follow-up visit, 3 months after terminating RT was evaluated using response evaluation criteria in solid tumors (RECIST), version 1.1.
Dose-volume and imaging analyses
Tomotherapy treatment plans of patients receiving > 90% fractions on tomotherapy were imported into ARIA® treatment planning software (Varian, Palo Alto, CA, USA) and dose volume histograms (DVH) for all target volumes and OAR were calculated and exported for further analysis. Maximal, median and average dose was calculated for all OAR, furthermore volumes receiving 5 to 60 Gy were calculated in 5 Gy steps for the following OAR: Small bowel loops (volume in ml), stomach (in % of total volume) and spleen (in % of total volume).
In case of local recurrence during follow-up, imaging of local recurrence (CT or FDG-PET-CT) was rigidly co-registered to the treatment plan. After delineation of local recurrence the spatial distribution of recurrence concerning RT dose was performed. Since size of recurrences differed substantially, the volume of recurrence was iso-volumteric reduced to an origin of recurrence volume measuring 4–5 ml. Dose parameters to this volume and to the whole recurrence volume were analysed to distinguish between in field recurrences, marginal recurrences and out of field recurrences.
Statistical analyses
All statistical analyses were performed using IBM® SPSS®, version 24 (IBM Corporation, Armonk, NY, USA). Correlation of acute and late toxicity with DVH was performed using non-parametric Spearman analysis. CTCAE scores of acute gastro-intestinal toxicities (nausea, vomiting, diarrhea, constipation, anorexia, dehydration, abdominal pain, hemorrhage, dyspepsia, gastro-esophageal reflux) were additionally summed up as combined gastro-intestinal toxicity.
Oncological endpoints of the study were local control (LC), overall survival (OS), occurrence of distant metastasis (DM, only for patients without metastases prior to RT) and progression free survival (PFS). The impact of potential prognostic and clinical variables on the endpoints were evaluated using the univariate Cox-regression model, corresponding survival curves were estimated by the Kaplan-Meier method, starting on the first day of radiotherapy.
Results
Median patient age was 66 years (range: 45 to 77 years). In case of local recurrent disease after radical surgery median time between surgery and start of radiotherapy was 541 days (range: 43 to 2297 days). Table 1 summarizes patient characteristics.
Table 1. Patient characteristics.
| Gender | |
| Male | 19 |
| Female | 9 |
| Tumor location | |
| Pancreas head | 19 |
| Pancreas body | 7 |
| Pancreas tail | 2 |
| Initial UICC stage | |
| I | 2 |
| IIA | 6 |
| IIB | 6 |
| III | 9 |
| IV | 5 |
| Tumor markers (median value and range) | |
| Initial CA-19-9 (U/ml) | 215 (0.5–4926) |
| Initial CEA (ng/ml) | 2.85 (1.1–12.9) |
| CA-19-9 (U/ml) before radiotherapy | 122.7 (9.4–3474) |
| CEA before radiotherapy | 4.1 (0.9–57.2) |
| CA-19-9 (U/ml) after radiotherapy | 85 (0.5–5146) |
| CEA after radiotherapy | 3.85 (1.1–49.5) |
| Prior neoadjuvant Chemotherapy | |
| None | 26 |
| Gemcitabine/ Nab-Paclitaxel | 2 |
| Prior palliative Chemotherapy | |
| None | 6 |
| FOLFIRINOX | 13 |
| Gemcitabine/ Nab-Paclitaxel | 9 |
| Prior surgery | |
| Pylorus preserving Pancreatico-duodenectomy | 9 |
| Whipple procedure | 2 |
| Distal Pancreatectomy | 2 |
| R0 resection | 7 |
| R1 resection | 5 |
| R2 resection | 1 |
| none | 15 |
Treatment was well tolerated in most patients. Ten of 28 patients presented acute toxicities > grade 2, most frequently weight loss was observed. One patient succumbed to gastrointestinal bleeding two weeks after end of treatment. This patient already presented severe anemia and fatigue before initiation of radiotherapy, probably due to undetected bloody oozing. Another patient developed controllable mild gastrointestinal bleeding during mid-treatment which was most probably tumor related. Table 2 summarizes the observed toxicities of RT. Evaluation of DVH revealed a weak correlation of intestine volume receiving ≥ 50 Gy and nausea (R = 0.403; p = 0.034). Also a significant correlation between anemia and various DVH parameters of the stomach (Average dose, median dose, V10%, 20%, 30%, 40%) was observed (R between 0.398 and 0.434; p between 0.024 and 0.04). Table 3 shows stomach and small intestine volumes receiving 10, 20, 30 and 40 Gy in individual patients and average values.
Table 2. Observed acute radiation induced toxicities.
| Nausea | |
| Grade 0 | 7 |
| Grade 1 | 15 |
| Grade 2 | 5 |
| Grade 3 | 1 |
| Vomiting | |
| Grade 0 | 24 |
| Grade 1 | 4 |
| Diarrhea | |
| Grade 0 | 12 |
| Grade 1 | 12 |
| Grade 2 | 4 |
| Constipation | |
| Grade 0 | 26 |
| Grade 1 | 1 |
| Grade 2 | 1 |
| Anorexia | |
| Grade 0 | 7 |
| Grade 1 | 7 |
| Grade 2 | 6 |
| ≥ Grade 3 | 8 |
| Dehydration | |
| Grade 0 | 24 |
| Grade 1 | 1 |
| Grade 2 | 3 |
| Abdominal pain | |
| Grade 0 | 14 |
| Grade 1 | 5 |
| Grade 2 | 7 |
| Grade 3 | 2 |
| Gastrointestinal bleeding | |
| Grade 0 | 26 |
| ≥ Grade 3 | 2 |
| Dyspepsia | |
| Grade 0 | 26 |
| Grade 1 | 1 |
| Grade 2 | 1 |
| Gastroesophageal reflux | |
| Grade 0 | 26 |
| Grade 2 | 2 |
| Fatigue | |
| Grade 0 | 8 |
| Grade 1 | 6 |
| Grade 2 | 10 |
| Grade 3 | 3 |
| n.a. | 1 |
| Hematologic toxicity | |
| Grade 0 | 24 |
| Grade 1 | 3 |
| n.a. | 1 |
Toxicities scored according to CTCAE 4.0
Table 3. Stomach and small bowel dose volume histograms.
| Pat. | Stomach | bowel loops | ||||||
|---|---|---|---|---|---|---|---|---|
| V10 (%) | V20 (%) | V30 (%) | V40 (%) | V10 (ml) | V20 (ml) | V30 (ml) | V40 (ml) | |
| 1 | 97 | 80 | 66 | 58 | 820 | 368 | 149 | 69 |
| 2 | 28 | 21 | 12 | 5 | 661 | 212 | 96 | 32 |
| 3 | 45 | 24 | 5 | 1 | 531 | 327 | 92 | 31 |
| 4 | 81 | 47 | 14 | 4 | 816 | 414 | 147 | 61 |
| 5 | 83 | 71 | 57 | 39 | 721 | 544 | 289 | 79 |
| 6 | 62 | 52 | 28 | 2 | 743 | 320 | 146 | 60 |
| 7 | 16 | 10 | 6 | 2 | 1200 | 445 | 130 | 39 |
| 8 | 31 | 13 | 4 | 1 | 648 | 310 | 100 | 19 |
| 9 | 60 | 26 | 8 | 3 | 505 | 391 | 281 | 135 |
| 10 | 61 | 14 | 4 | 1 | 972 | 330 | 188 | 104 |
| 11 | 38 | 20 | 1 | 0 | 780 | 516 | 287 | 166 |
| 12 | 38 | 29 | 17 | 5 | 924 | 631 | 179 | 62 |
| 13 | 14 | 12 | 11 | 9 | 780 | 409 | 169 | 60 |
| 14 | 34 | 24 | 4 | 0 | 660 | 402 | 142 | 44 |
| 15 | 73 | 46 | 27 | 11 | 1026 | 616 | 240 | 105 |
| 16 | 64 | 37 | 14 | 5 | 642 | 356 | 129 | 32 |
| 17 | 91 | 84 | 72 | 45 | 606 | 392 | 167 | 83 |
| 18 | 37 | 8 | 1 | 0 | 477 | 196 | 56 | 10 |
| 19 | 53 | 32 | 7 | 1 | 248 | 144 | 77 | 31 |
| 20 | 55 | 41 | 11 | 1 | 604 | 302 | 91 | 23 |
| 21 | 100 | 75 | 36 | 16 | 2153 | 814 | 305 | 121 |
| 22 | 18 | 5 | 1 | 0 | 1218 | 525 | 102 | 23 |
| 23 | 57 | 32 | 11 | 2 | 736 | 261 | 77 | 18 |
| 24 | 19 | 13 | 7 | 2 | 803 | 425 | 171 | 47 |
| 25 | 39 | 21 | 10 | 1 | 711 | 251 | 79 | 43 |
| 26 | 50 | 34 | 15 | 2 | 485 | 158 | 33 | 3 |
| 27 | 54 | 27 | 9 | 1 | 723 | 310 | 109 | 26 |
| 28 | 98 | 73 | 46 | 23 | 287 | 114 | 40 | 11 |
| Avg. | 53% | 35% | 18% | 9% | 767 ml | 374 ml | 145 ml | 55 ml |
Volumes of the stomach (in %) and of bowel loops (in ml) receiving 10, 20, 30 and 40 Gy (V10, V20, V30, V40) in individual patients (Pat.) and on average (Avg.).
Dose volume parameters of the spleen showed the highest correlation with several toxicities (vomiting, anorexia, dehydration, hematologic toxicity, fatigue, combined gastro-intestinal toxicity) wit R-values between 0.392 and 0.561 (all p-values significant), Table 4 shows observed toxicities and spleen dose-volume parameters. No significant correlations between patient characteristics, clinical parameters or PTV volumes and toxicity were observed. S1 Table lists individual DVH parameters for selected OAR. Higher grade (> grade 2) late toxicity was only observed in one patient, who presented substantial weight loss. However this patient suffered from local and systemic relapse, therefore an association of these symptoms with radiation therapy is doubtful.
Table 4. Dose volume parameters of the spleen (individual maximal, average and median dose and spleen volumes receiving 10 to 40 Gy) and correlation to acute toxicities.
| Toxicity | Spleen DMax | Spleen DMean | Spleen DMedian | Spleen V10 | Spleen V20 | Spleen V30 | Spleen V40 | |
|---|---|---|---|---|---|---|---|---|
| Vomiting | R | 0.242 | 0.061 | 0.000 | 0.166 | 0.076 | 0.219 | 0.45 |
| p | 0.244 | 0.774 | 1.000 | 0.427 | 0.712 | 0.292 | 0.024 | |
| Diarrhea | R | 0.344 | .440 | .419 | .445 | 0.270 | .430 | 0.338 |
| p | 0.100 | 0.031 | 0.042 | 0.029 | 0.192 | 0.036 | 0.106 | |
| Anorexia/Loss of Appetite | R | 0.561 | 0.387 | 0.326 | 0.437 | 0.447 | 0.299 | 0.312 |
| p | 0.004 | 0.056 | 0.112 | 0.029 | 0.022 | 0.147 | 0.129 | |
| Hematologic toxicity | R | 0.173 | 0.446 | 0.446 | 0.391 | 0.258 | 0.351 | 0.154 |
| p | 0.419 | 0.029 | 0.029 | 0.059 | 0.214 | 0.092 | 0.472 | |
| Combined GI | R | 0.498 | 0.437 | 0.379 | 0.458 | 0.392 | 0.331 | 0.526 |
| p | 0.011 | 0.029 | 0.062 | 0.021 | 0.048 | 0.106 | 0.007 | |
| Fatigue | R | 0.152 | -0.025 | -0.043 | -0.073 | 0.146 | 0.259 | 0.408 |
| p | 0.478 | 0.906 | 0.843 | 0.735 | 0.487 | 0.221 | 0.048 |
DMax = Maximal splenic dose, DMean = Average splenic dose, DMedian = median splenic dose. V10 –V40 = splenic volumes (in % of the whole organ) receiving 10 to 40 Gy radiation dose. R = correlation coefficient, p = p-value, significant p-values < 0.05 in bold,.
Local response evaluation three months after completing RT was available for 24 patients and revealed stable disease in 14 cases, partial remission in 9 cases and one case of progressive disease.
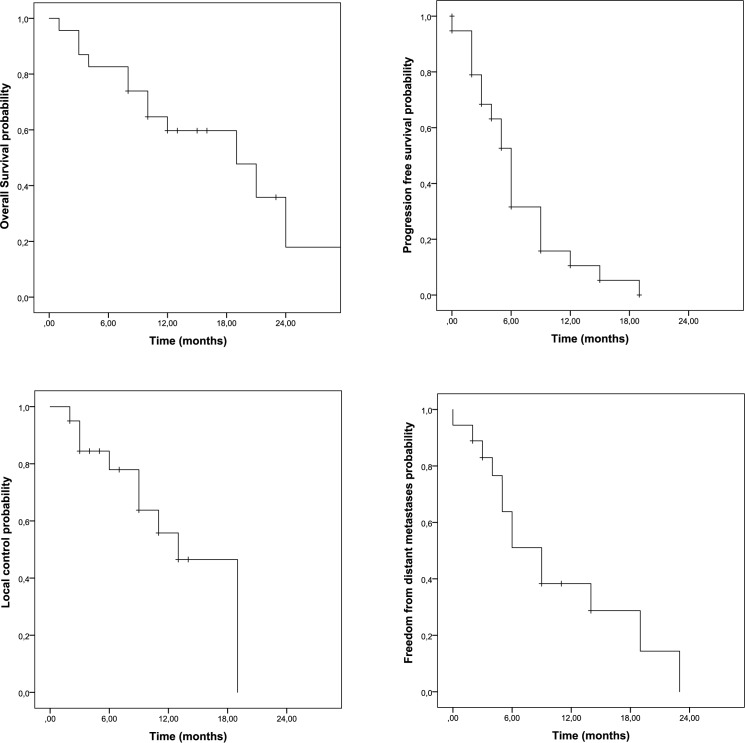
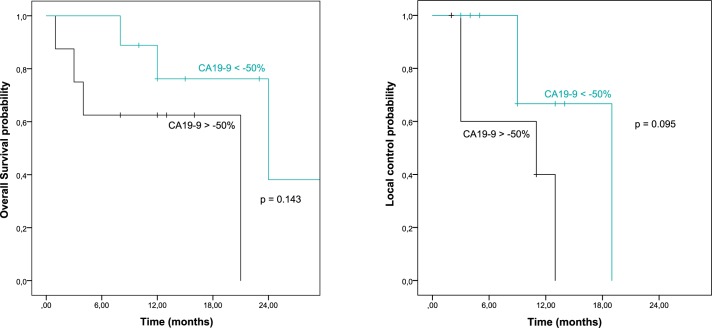
With an average follow-up time of 14 months in surviving patients, median OS time was 19 months, median time to local recurrence was 13 months. Fig 1 depicts the Kaplan-Meier curves for OS, PFS, LC and DM. In univariate analysis only the ΔCA-19-9 response during RCT was significantly associated with outcome (OS, p = 0.049; LC, p = 0.029;). All other factors, including age, tumor location, distant metastases prior to RT and splenic dose parameters did not show any association with OS. Results of univariate analyses are summarized in S2 Table. Dichotomization of ΔCA-19-9 (decrease of 50% or more versus decrease of less than 50% or increase during RCT) revealed a trend for better local control in patients with more pronounced CA-19-9 responses (p = 0.095) as shown in Fig 2.
Fig 1. Kaplan-Meier curves showing overall survival and progression free survival probability (above) and freedom from local recurrence or distant metastases rate (below).
Fig 2. Dichotomization of patients regarding CA-19-9 plasma marker response and association with overall survival and local control probability.
Sectional imaging information of patients with local recurrences was available in 8 of 11 cases. 5 patients developed in field recurrences, 2 patients marginal recurrences and one patient developed a lymphnode recurrence outside the RT field. Table 5 shows doses to the recurrent tumor volumes and corresponding GTV volumes.
Table 5. Recurrence patterns.
| GTV volume | Median dose | Median dose | Minimal dose | Time to failure* | Failure |
|---|---|---|---|---|---|
| recurrence | OOR | OOR | |||
| 31.4 | 43.6 | 44.2 | 30.0 | 13 | marginal |
| 123.3 | 65.0 | 65.8 | 39.1 | 4 | in field |
| 45.3 | 6.3 | 8.3 | 1.6 | 9 | out of field |
| 350.0 | 64.9 | 66.4 | 64.0 | 2 | in field |
| 33.5 | 65.2 | 66.7 | 61.6 | 11 | in field |
| 40.5 | 58.8 | 65.8 | 39.9 | 9 | in field |
| 57.1 | 36.1 | 38.0 | 26.5 | 13 | marginal |
| 65.2 | 57.0 | 57.5 | 51.6 | 3 | In field |
GTV volume = irradiated gross tumor volume in ml. OOR = origin of recurrence (isovolumetric shrunk recurrence volume). All doses in Gray.
*given in months, measured from start of radiotherapy.
Discussion
Here we report our first experience with daily image guided dose-escalated RT for LAPC. Compared to the 47 dose escalated patients described by Krishnan and colleagues the median OS observed in our study was similar (17.8 months versus 19 months in our study) although 25% (7 of 28) of the patients described here presented with distant metastases. Additionally no clear correlation between classical OAR DVH and toxicity was found, in contrast several significant associations of spleen DVHs and acute toxicities were observed. Furthermore CA-19-9 response during RCT could be identified as a potential novel biomarker to select patients that most likely benefit from focal dose-escalated RT.
Regarding outcome after high-dose radiotherapy similar results were reported by Chung and colleagues: In a retrospective analysis of 152 patients receiving radiochemotherapy with 61 Gy or more the median overall survival time was 21.9 months [17]. In a phase-I/II dose escalation trial Ben-Josef and colleagues reported a median overall survival time of 14.8 months with most patients of the study receiving 55 Gy prescribed dose [18]. Another Phase-II study with induction chemotherapy followed by radiochemotherapy up to 59.4 Gy total radiation dose reported a median overall survival time of 14 months in unresectable patients [19]. Despite further dose escalation, permanent local tumor control is still unsatisfactory with in-field recurrences in most cases. Obviously, the radiation dosage is still too low. Considering the described advantage of dose escalation [14,17] a further increase of dose might be required to warrant local control. Therefore, uncertainties causing geographical misses must be minimized to enable further dose escalation and improve dose coverage while adjacent OARs are still sufficiently spared. One error source could be intra-fractional variation due to respiratory motion [20,21]. GTV was delineated using FDG-PET whenever available. Due to the long acquisition time PET imaging contains some information on respiratory motion, however even 3D PET underestimates respiratory motion as a recent publication on 4D PET for pancreatic cancer showed [22]. In our study we instructed the patients to breathe shallow during planning CT as well as during dose delivery. The instantaneous equilibrium position of the tumor was adjusted via MCVT exploiting soft tissue contrast and stents in situ as far as possible. Further evaluation based on 4D-CT and methods to determine and minimize intrafractional displacements are required.
If further dose escalation in the upper abdomen is indispensible, small bowel and in particular the duodenum are limiting the magnitude and coverage of tumor dose. Published data on OAR constraints and toxicity show a large heterogeneity. For pancreatic cancer Kelly described a correlation of V55Gy within the duodenum and gastro-intestinal toxicity [23], however in a small cohort of patients treated with hypofractionated stereotactic RT duodenal DVHs only correlated to histomorphological alterations but not to clinical scored toxicity [24]. The best available data on small intestine constraints from QUANTEC recommends that the dose to the small bowel receiving ≥ 45 Gy should not exceed 200 ml, if the entire peritoneal space is delineated. This constraint was always adhered to for treatment planning. For delineation of small bowel loops QUANTEC recommends that the dose to the small bowel receiving ≥ 15 Gy should not exceed 120ml. Retrospective additional delineation of small bowel loops showed excessive doses compared to the latter QUANTEC constraints, as shown in Table 3, with relatively good tolerability. The DVH-values of intestine in our study were not associated with relevant intestinal acute toxicity. Furthermore addition of chemotherapy or previous surgery is known for an additional, though in its magnitude unknown, contribution to toxicity [25]. Type of surgery and anastomosis may have an additional effect on radiation toxicity. However surgical procedures were relatively homogeneous as most patients received pylorus preserving pancreaticoduodenectomy and a recent Cochrane analysis showed that postoperative comorbidities do not differ dramatically between classical Whipple procedure and pylorus preserving surgery [26].
In all patients higher volumes of the intestine were exposed to 30 Gy and 20 Gy (Table 3). However, QUANTEC data is mainly based on DVH analyses of rectal and cervical cancer patients. Explicit DVH data for irradiation of pancreatic cancers is sparse. Jin and colleagues analysed DVHs of 20 patients treated for pancreatic cancers and found similar, comparatively low rates of higher grade toxicity. Additionally an advantage of VMAT compared to 3D conformal RT or intensity modulated RT (IMRT) regarding acute toxicities was described by several groups [27,28]. These findings are in contrast to the Phase-I/II study on radiation dose escalation reported by Ben-Josef and colleagues: They observed an increase of dose limiting toxicities with radiation doses higher than 55 Gy [18]. However no information on daily image guidance was reported, which may be an important difference to our and other studies who reported the tolerability of higher radiation doses. The missing correlation of small bowel dose volume parameters and acute toxicity when using modern RT techniques was also described by another group who investigated preoperative RCT for rectal cancer [29].
Besides the absent association of classical OAR dosimetric factors and toxicity, we found instead several associations between DVH parameters of the spleen and toxicity. Traditionally the spleen is an ignored organ in RT, although with the onset of radio-immunotherapy it currently raised some interest. Trip found dose-dependend volumetric long-term alterations of the spleen in patients treated for gastric cancers [30]. In irradiated pancreatic cancer patients splenic DVH parameters were associated with development of severe lymphopenia after RT, the latter one being prognostic for patient survival [31]. No information about a correlation of splenic DVHs and other than hematologic toxicities were reported in that publication. No association of splenic dose parameters and oncological outcome parameters (LC, OS, DM) was observed in our study upon univariate testing. The explanation for the observed association between splenic DVH-parameters and toxicity remains unresolved and it is unlikely that all observed side effects are attributable to the spleen doses. The spleen might most likely be a surrogate organ to quantify the dose exposure specifically to the upper abdomen, which is correlated with general complaints such as anorexia and fatigue. Even when patients are carefully instructed about timing of ingestion, stomach dose volume parameters still fluctuate largely, which may be an explanation why no strong correlations were observed when evaluationg DVH parameters of the stomach. Splenic DVH parameters should be further evaluated and validated.
Pre-therapeutic CA-19-9 levels are known prognostic factors for OS and PFS in patients treated with RCT for LAPC, however the role of pre-therapeutic levels in case of radical surgery is controversial [32–34]. In this cohort of patients we were not able to confirm a prognostic role of initial CA-19-9, however patients described here had relatively high CA-19-9 levels as only 4 of 22 patients would have belonged to the favourable prognostic group with CA-19-9 lower or equal 90 U/ml described by Vainshtein [32]. However individual CA-19-9 decrease was found to be significantly associated with OS and LC. Our findings are in line with another publication: Koom and colleagues identified CA-19-9 decrease of less than 40% as a strong negative prognostic factor for patients undergoing RCT for pancreatic cancer [35], however the latter study measured the second CA-19-9 value one to three months after RT, while our study measured CA-19-9 values during the last week or immediately after radiotherapy, when therapeutic alterations of the treatment regime would still be potentially feasible.
Our study has several limitations: First of all its retrospective nature, although patients were treated within an internal standardized protocol and all consecutive patients were evaluated. Second the heterogeneity of patients: Patients with distant metastases as well as patients with non-resectable or local recurrent cancer were included. However, the latter two groups are very similar regarding prognosis and presence of distant metastases prior to RT was not associated with inferior outcome upon univariate testing. Another limitation regards the relatively low patient number, therefore no multivariate analysis was performed to avoid statistical overfitting, furthermore our findings should be seen as hypothesis generating. In this regard high-dose daily image-guided normo-fractionated RCT for LAPC seems to be relatively safe, while established OAR restrictions were not associated with acute toxicity. Our findings indicate that the spleen should potentially be included as an OAR for high-dose RT of the upper abdomen. Furthermore, CA-19-9 response during irradiation might be useful for treatment stratification. Last but not least the low LC rate observed in our study indicates that RT in this setting needs further intensification: Either by the use of novel systemic agents [36,37], by the addition of hyperthermia to RCT [38], and particularly by selectively increasing the radiation dose to morphological defined high-risk regions, which requires improved image guidance and compensation of organ motion during dose delivery. The proof of principle that high radiation doses within a small volume are well tolerable could also be used for future trials in unresectable or borderline resectable pancreatic cancer. Instead of boosting the whole macroscopic tumor, a boost to infiltrated vessels might be better tolerated and consecutive surgery could substantially improve local control [39,40].
Supporting information
(DOCX)
95% CI = 95 percent confidence interval. Local recurrence = local recurrent versus initially local advanced pancreatic cancer. Distant metastases = distant metastasis before radiotherapy.
(DOCX)
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
The authors received no specific funding for this work.
References
- 1.Neoptolemos JP, Stocken DD, Friess H, Bassi C, Dunn JA, Hickey H, et al. A randomized trial of chemoradiotherapy and chemotherapy after resection of pancreatic cancer. N Engl J Med. 2004;350: 1200–1210. doi: 10.1056/NEJMoa032295 [DOI] [PubMed] [Google Scholar]
- 2.Oettle H, Post S, Neuhaus P, Gellert K, Langrehr J, Ridwelski K, et al. Adjuvant chemotherapy with gemcitabine vs observation in patients undergoing curative-intent resection of pancreatic cancer: a randomized controlled trial. JAMA. 2007;297: 267–277. doi: 10.1001/jama.297.3.267 [DOI] [PubMed] [Google Scholar]
- 3.Huguet F, Mukherjee S, Javle M. Locally advanced pancreatic cancer: the role of definitive chemoradiotherapy. Clin Oncol (R Coll Radiol). 2014;26: 560–568. doi: 10.1016/j.clon.2014.06.002 [DOI] [PubMed] [Google Scholar]
- 4.Sperti C, Pasquali C, Piccoli A, Pedrazzoli S. Recurrence after resection for ductal adenocarcinoma of the pancreas. World J Surg. 1997;21: 195–200. [DOI] [PubMed] [Google Scholar]
- 5.Sperti C, Moletta L, Merigliano S. Multimodality treatment of recurrent pancreatic cancer: Mith or reality? World J Gastrointest Oncol. 2015;7: 375–382. doi: 10.4251/wjgo.v7.i12.375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Thomas RM, Truty MJ, Nogueras-Gonzalez GM, Fleming JB, Vauthey J-N, Pisters PWT, et al. Selective reoperation for locally recurrent or metastatic pancreatic ductal adenocarcinoma following primary pancreatic resection. J Gastrointest Surg. 2012;16: 1696–1704. doi: 10.1007/s11605-012-1912-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Klaassen DJ, MacIntyre JM, Catton GE, Engstrom PF, Moertel CG. Treatment of locally unresectable cancer of the stomach and pancreas: a randomized comparison of 5-fluorouracil alone with radiation plus concurrent and maintenance 5-fluorouracil—an Eastern Cooperative Oncology Group study. J Clin Oncol. 1985;3: 373–378. doi: 10.1200/JCO.1985.3.3.373 [DOI] [PubMed] [Google Scholar]
- 8.Hammel P, Huguet F, van Laethem J-L, Goldstein D, Glimelius B, Artru P, et al. Effect of Chemoradiotherapy vs Chemotherapy on Survival in Patients With Locally Advanced Pancreatic Cancer Controlled After 4 Months of Gemcitabine With or Without Erlotinib: The LAP07 Randomized Clinical Trial. JAMA. 2016;315: 1844–1853. doi: 10.1001/jama.2016.4324 [DOI] [PubMed] [Google Scholar]
- 9.Chauffert B, Mornex F, Bonnetain F, Rougier P, Mariette C, Bouché O, et al. Phase III trial comparing intensive induction chemoradiotherapy (60 Gy, infusional 5-FU and intermittent cisplatin) followed by maintenance gemcitabine with gemcitabine alone for locally advanced unresectable pancreatic cancer. Definitive results of the 2000–01 FFCD/SFRO study. Ann Oncol. 2008;19: 1592–1599. doi: 10.1093/annonc/mdn281 [DOI] [PubMed] [Google Scholar]
- 10.Huguet F, André T, Hammel P, Artru P, Balosso J, Selle F, et al. Impact of chemoradiotherapy after disease control with chemotherapy in locally advanced pancreatic adenocarcinoma in GERCOR phase II and III studies. J Clin Oncol. 2007;25: 326–331. doi: 10.1200/JCO.2006.07.5663 [DOI] [PubMed] [Google Scholar]
- 11.Krishnan S, Rana V, Janjan NA, Varadhachary GR, Abbruzzese JL, Das P, et al. Induction chemotherapy selects patients with locally advanced, unresectable pancreatic cancer for optimal benefit from consolidative chemoradiation therapy. Cancer. 2007;110: 47–55. doi: 10.1002/cncr.22735 [DOI] [PubMed] [Google Scholar]
- 12.Loehrer PJ, Feng Y, Cardenes H, Wagner L, Brell JM, Cella D, et al. Gemcitabine alone versus gemcitabine plus radiotherapy in patients with locally advanced pancreatic cancer: an Eastern Cooperative Oncology Group trial. J Clin Oncol. 2011;29: 4105–4112. doi: 10.1200/JCO.2011.34.8904 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rutter CE, Park HS, Corso CD, Lester-Coll NH, Mancini BR, Yeboa DN, et al. Addition of radiotherapy to adjuvant chemotherapy is associated with improved overall survival in resected pancreatic adenocarcinoma: An analysis of the National Cancer Data Base. Cancer. 2015;121: 4141–4149. doi: 10.1002/cncr.29652 [DOI] [PubMed] [Google Scholar]
- 14.Krishnan S, Chadha AS, Suh Y, Chen H-C, Rao A, Das P, et al. Focal Radiation Therapy Dose Escalation Improves Overall Survival in Locally Advanced Pancreatic Cancer Patients Receiving Induction Chemotherapy and Consolidative Chemoradiation. Int J Radiat Oncol Biol Phys. 2016;94: 755–765. doi: 10.1016/j.ijrobp.2015.12.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sinn M, Ganeshan R, Graf R, Pelzer U, Stieler JM, Striefler JK, et al. Intensity-modulated and image-guided radiotherapy in patients with locally advanced inoperable pancreatic cancer after preradiation chemotherapy. ScientificWorldJournal. 2014;2014: 452089 doi: 10.1155/2014/452089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sun W, Leong CN, Zhang Z, Lu JJ. Proposing the lymphatic target volume for elective radiation therapy for pancreatic cancer: a pooled analysis of clinical evidence. Radiat Oncol. 2010;5: 28 doi: 10.1186/1748-717X-5-28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chung SY, Chang JS, Lee BM, Kim KH, Lee KJ, Seong J. Dose escalation in locally advanced pancreatic cancer patients receiving chemoradiotherapy. Radiotherapy and Oncology. 2017; doi: 10.1016/j.radonc.2017.04.010 [DOI] [PubMed] [Google Scholar]
- 18.Ben-Josef E, Schipper M, Francis IR, Hadley S, Ten-Haken R, Lawrence T, et al. A phase I/II trial of intensity modulated radiation (IMRT) dose escalation with concurrent fixed-dose rate gemcitabine (FDR-G) in patients with unresectable pancreatic cancer. Int J Radiat Oncol Biol Phys. 2012;84: 1166–1171. doi: 10.1016/j.ijrobp.2012.02.051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fiore M, Ramella S, Valeri S, Caputo D, Floreno B, Trecca P, et al. Phase II study of induction chemotherapy followed by chemoradiotherapy in patients with borderline resectable and unresectable locally advanced pancreatic cancer. Sci Rep. 2017;7: 45845 doi: 10.1038/srep45845 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Akimoto M, Nakamura M, Nakamura A, Mukumoto N, Kishi T, Goto Y, et al. Inter- and intrafractional variation in the three-dimensional positions of pancreatic tumors due to respiration under real-time monitoring. International Journal of Radiation Oncology*Biology*Physics. 2017; doi: 10.1016/j.ijrobp.2017.03.042 [DOI] [PubMed] [Google Scholar]
- 21.Lens E, Gurney-Champion OJ, Tekelenburg DR, van Kesteren Z, Parkes MJ, van Tienhoven G, et al. Abdominal organ motion during inhalation and exhalation breath-holds: pancreatic motion at different lung volumes compared. Radiother Oncol. 2016;121: 268–275. doi: 10.1016/j.radonc.2016.09.012 [DOI] [PubMed] [Google Scholar]
- 22.Kishi T, Matsuo Y, Nakamura A, Nakamoto Y, Itasaka S, Mizowaki T, et al. Comparative evaluation of respiratory-gated and ungated FDG-PET for target volume definition in radiotherapy treatment planning for pancreatic cancer. Radiother Oncol. 2016;120: 217–221. doi: 10.1016/j.radonc.2016.07.012 [DOI] [PubMed] [Google Scholar]
- 23.Kelly P, Das P, Pinnix CC, Beddar S, Briere T, Pham M, et al. Duodenal toxicity after fractionated chemoradiation for unresectable pancreatic cancer. Int J Radiat Oncol Biol Phys. 2013;85: e143–149. doi: 10.1016/j.ijrobp.2012.09.035 [DOI] [PubMed] [Google Scholar]
- 24.Verma V, Lazenby AJ, Zheng D, Bhirud AR, Ly QP, Are C, et al. Dosimetric parameters correlate with duodenal histopathologic damage after stereotactic body radiotherapy for pancreatic cancer: Secondary analysis of a prospective clinical trial. Radiother Oncol. 2017;122: 464–469. doi: 10.1016/j.radonc.2016.12.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kavanagh BD, Pan CC, Dawson LA, Das SK, Li XA, Ten Haken RK, et al. Radiation dose-volume effects in the stomach and small bowel. Int J Radiat Oncol Biol Phys. 2010;76: S101–107. doi: 10.1016/j.ijrobp.2009.05.071 [DOI] [PubMed] [Google Scholar]
- 26.Hüttner FJ, Fitzmaurice C, Schwarzer G, Seiler CM, Antes G, Büchler MW, et al. Pylorus-preserving pancreaticoduodenectomy (pp Whipple) versus pancreaticoduodenectomy (classic Whipple) for surgical treatment of periampullary and pancreatic carcinoma. Cochrane Database Syst Rev. 2016;2: CD006053 doi: 10.1002/14651858.CD006053.pub6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jin L, Wang R, Jiang S, Yue J, Liu T, Dou X, et al. Dosimetric and clinical toxicity comparison of critical organ preservation with three-dimensional conformal radiotherapy, intensity-modulated radiotherapy, and RapidArc for the treatment of locally advanced cancer of the pancreatic head. Curr Oncol. 2016;23: e41–48. doi: 10.3747/co.23.2771 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lee KJ, Yoon HI, Chung MJ, Park JY, Bang S, Park S-W, et al. A Comparison of Gastrointestinal Toxicities between Intensity-Modulated Radiotherapy and Three-Dimensional Conformal Radiotherapy for Pancreatic Cancer. Gut Liver. 2016;10: 303–309. doi: 10.5009/gnl15186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Xu B, Guo Y, Chen Y, Lu H, Tang T, Yue Z, et al. Is the irradiated small bowel volume still a predictor for acute lower gastrointestinal toxicity during preoperative concurrent chemo-radiotherapy for rectal cancer when using intensity-modulated radiation therapy? Radiat Oncol. 2015;10: 257 doi: 10.1186/s13014-015-0566-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Trip AK, Sikorska K, van Sandick JW, Heeg M, Cats A, Boot H, et al. Radiation-induced dose-dependent changes of the spleen following postoperative chemoradiotherapy for gastric cancer. Radiother Oncol. 2015;116: 239–244. doi: 10.1016/j.radonc.2015.07.036 [DOI] [PubMed] [Google Scholar]
- 31.Chadha AS, Liu G, Chen H-C, Das P, Minsky BD, Mahmood U, et al. Does unintentional splenic radiation predict severe lymphopenia following pancreatic cancer radiotherapy? International Journal of Radiation Oncology*Biology*Physics. 2016; doi: 10.1016/j.ijrobp.2016.10.046 [DOI] [PubMed] [Google Scholar]
- 32.Vainshtein JM, Schipper M, Zalupski MM, Lawrence TS, Abrams R, Francis IR, et al. Prognostic significance of carbohydrate antigen 19–9 in unresectable locally advanced pancreatic cancer treated with dose-escalated intensity modulated radiation therapy and concurrent full-dose gemcitabine: analysis of a prospective phase 1/2 dose escalation study. Int J Radiat Oncol Biol Phys. 2013;86: 96–101. doi: 10.1016/j.ijrobp.2012.11.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Micke O, Bruns F, Kurowski R, Horst E, deVries AF, Hausler JW, et al. Predictive value of carbohydrate antigen 19–9 in pancreatic cancer treated with radiochemotherapy. Int J Radiat Oncol Biol Phys. 2003;57: 90–97. [DOI] [PubMed] [Google Scholar]
- 34.Park JK, Paik WH, Ryu JK, Kim Y-T, Kim YJ, Kim J, et al. Clinical Significance and Revisiting the Meaning of CA 19–9 Blood Level Before and After the Treatment of Pancreatic Ductal Adenocarcinoma: Analysis of 1,446 Patients from the Pancreatic Cancer Cohort in a Single Institution. Alg?l H, editor. PLoS ONE. 2013;8: e78977 doi: 10.1371/journal.pone.0078977 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Koom WS, Seong J, Kim YB, Pyun HO, Song SY. CA 19–9 as a predictor for response and survival in advanced pancreatic cancer patients treated with chemoradiotherapy. Int J Radiat Oncol Biol Phys. 2009;73: 1148–1154. doi: 10.1016/j.ijrobp.2008.06.1483 [DOI] [PubMed] [Google Scholar]
- 36.Uesaka K, Boku N, Fukutomi A, Okamura Y, Konishi M, Matsumoto I, et al. Adjuvant chemotherapy of S-1 versus gemcitabine for resected pancreatic cancer: a phase 3, open-label, randomised, non-inferiority trial (JASPAC 01). Lancet. 2016;388: 248–257. doi: 10.1016/S0140-6736(16)30583-9 [DOI] [PubMed] [Google Scholar]
- 37.Chadha AS, Skinner HD, Gunther JR, Munsell MF, Das P, Minsky BD, et al. Phase I Trial of Consolidative Radiotherapy with Concurrent Bevacizumab, Erlotinib and Capecitabine for Unresectable Pancreatic Cancer. Lesinski G, editor. PLOS ONE. 2016;11: e0156910 doi: 10.1371/journal.pone.0156910 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Maluta S, Schaffer M, Pioli F, Dall’oglio S, Pasetto S, Schaffer PM, et al. Regional hyperthermia combined with chemoradiotherapy in primary or recurrent locally advanced pancreatic cancer : an open-label comparative cohort trial. Strahlenther Onkol. 2011;187: 619–625. doi: 10.1007/s00066-011-2226-6 [DOI] [PubMed] [Google Scholar]
- 39.Wang LS, Shaikh T, Handorf EA, Hoffman JP, Cohen SJ, Meyer JE. Dose escalation with a vessel boost in pancreatic adenocarcinoma treated with neoadjuvant chemoradiation. Pract Radiat Oncol. 2015;5: e457–463. doi: 10.1016/j.prro.2015.04.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bahra M, Pratschke J, Klein F, Neuhaus P, Boas-Knoop S, Puhl G, et al. Cytoreductive Surgery for Pancreatic Cancer Improves Overall Outcome of Gemcitabine-Based Chemotherapy. Pancreas. 2015;44: 930–936. doi: 10.1097/MPA.0000000000000365 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
95% CI = 95 percent confidence interval. Local recurrence = local recurrent versus initially local advanced pancreatic cancer. Distant metastases = distant metastasis before radiotherapy.
(DOCX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.