Abstract
Objectives
Chronic low back pain (CLBP) is a common health problem with challenges for providing satisfactory care. This study was undertaken to identify opportunities to improve key aspects of physicians’ communications with CLBP-affected patients.
Methods
A series of 3 focus groups, each with 7 to 11 patients with CLBP, were recruited from primary care settings and grouped by risk level of reduced function resulting from back pain, to elicit perspectives about interactions with their primary care physicians. Analysis of focus group transcripts used an iterative process based on a thematic approach and a priori concepts.
Results
A total of 28 patients participated in the focus groups. Patient comments about communicating with physicians around CLBP fit into themes of listening and empathy, validating pain experiences, conducting effective CLBP assessment, providing clear diagnosis and information, and collaboratively working on treatment. Patients shared that physicians can foster positive interactions with CLBP-affected patients by sharing personal experiences of chronic pain, being truthful about not having all the answers and being clear about how patients can benefit from referrals, reviewing the patient’s previous treatments before beginning conversations about treatment options, providing follow-up instructions, giving patients a diagnosis beyond “chronic pain,” and explaining the role of imaging in their care.
Conclusion
This study provides specific steps that physicians in the US can take to improve physician-patient interactions during primary care visits pertaining to CLBP. The findings could inform physician training, development of educational materials for patients, and future research.
INTRODUCTION
Chronic low back pain (CLBP) is a common and costly health problem in primary care. A study reviewing North Carolina data between 1996 and 2013 found that personal health care expenditures for low back pain in 2013 were greater than $86 billion.1 Globally, low back pain causes more disability than any other condition.2 Providing care for patients with CLBP is challenging, with few tools for diagnosing and treating it. The structural cause of the pain is often not identifiable,3 and treatment options may not be effective.4,5
With these challenges, it is not surprising that many patients are dissatisfied with care provided for their CLBP.6,7 Physicians tend to take a biomedical approach to problems such as CLBP that involve psychological and social factors. The physician’s adherence to a strictly biomedical model can frustrate patients and result in visits that do not meet their needs. Research has found that patients with CLBP expect physicians to offer diagnostic tests, a diagnosis, information on prognosis, prescription medicines, and referrals.8 Predictors of patient satisfaction with health care include feeling that one is treated with respect, listened to, and taken seriously.9,10 Patient dissatisfaction is associated with feeling disrespected or distrusted by the physician and feeling that the physician dismissed symptoms as trivial or suspected drug seeking.
The quality of physician-patient communication is associated with patient satisfaction,11 patient adherence to treatment plans,12 and positive health outcomes.13 Furthermore, the way physicians communicate with CLBP-affected patients can influence beliefs about their condition. Physician communication that is correctly interpreted can affect the patients’ ability to understand the source and meaning of symptoms and prognostic expectations, whereas misinterpreted messages can result in amplified vigilance, guilt about not adhering to treatment plans, or frustration when plans fail.14
Improving physician-patient interactions regarding chronic pain has the potential to enhance the care experience of patients with CLBP. The aim of this article was to identify strategies to improve physician-patient communication surrounding CLBP and to shed light on opportunities for physicians to communicate with patients in ways that patients find supportive. Our findings help address knowledge gaps about communication and personalization of visits, specific characteristics of physician-patient interactions that make patients feel respected, and perspectives of US patients about communicating about back pain.
METHODS
Three focus groups were conducted in preparation for a larger project evaluating a risk-stratification strategy for improving CLBP treatment in primary care. The analysis assessed differences in care experiences and perspectives of physician communication, if any, between patients with differing levels of biopsychosocial factors.15 Our methods were consistent with rigorous criteria in qualitative research, as documented by the consolidated criteria for reporting qualitative research (COREQ) checklist for interview and focus groups.16 The study design and materials were reviewed and approved by the institutional review board of Kaiser Permanente (KP) Washington Health Research Institute, Seattle, WA.
Selection and Recruitment of Participants
Focus groups were assembled to inform understanding of patient experiences in seeking treatment of CLBP. Patients were eligible if they had recently seen their primary care physician regarding CLBP, were from the central Puget Sound region of Washington State whose physician worked at one of KP’s owned and operated clinics, were aged 18 years or older, and had a visit to a primary care physician in the previous week that resulted in a diagnosis code for nonspecified back pain. Study staff sent recruitment letters using patient information extracted from our administrative data system. Patients were excluded if they had diagnoses indicating specific reasons for back pain or had conditions that affected their ability to provide informed consent.
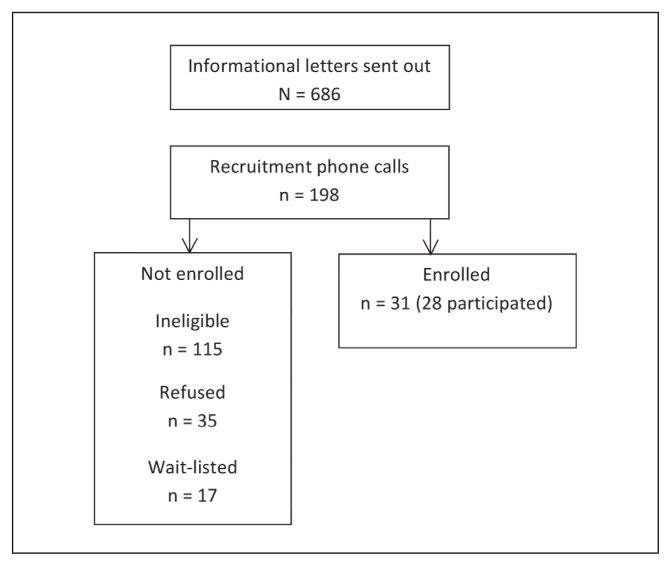
Potential participants were mailed an invitation letter two weeks after their visit for CLBP. The research team then contacted potential participants by telephone to determine eligibility. If the patient was eligible and willing to participate, the STarT Back Tool,15 which recommends treatments on the basis of patient scores from a nine-item questionnaire, was administered. The tool categorizes patients by risk scores of the impact of pain on their physical and psychosocial functioning. High risk includes a risk of impaired psychosocial functioning, medium risk involves the risk of pain or dysfunction but no clinically significant psychosocial impairment, and low risk is less severe pain and no psychosocial risk. Potential participants were asked if they were willing and able to participate in focus groups and were recruited into these groups by their risk group. The recruitment process and sample sizes for each step are shown in Figure 1.
Figure 1.
Focus group for patients with chronic low back pain: Recruitment process and sample sizes.
Focus Groups
Two qualitative researchers conducted 2-hour focus groups. The discussion guide was designed to elicit rich descriptions of the individual experiences of patients seeking treatment of CLBP, their interactions with physicians, and other issues germane to the larger research study (see Appendix, available at: www.thepermanentejournal.org/files/2017/16-177-Appendix.pdf). Three groups, one for each risk group, had a maximum of 12 participants each. Each participant received $100 for participating; a light meal was served during the focus group. A court reporter transcribed the discussions; transcripts were imported into qualitative analysis software (ATLAS.ti Version 6.2 for Microsoft Windows, Berlin, Germany). All participants provided informed consent.
Analysis
The analysis team consisted of two project team members (SE and CH), who conducted or were present at all three focus groups. Using an iterative process based on a thematic analysis approach, the primary coder (SE) developed a code list on the basis of emergent themes that surfaced during transcript review and a priori concepts of interest. These concepts included patients’ views of their interaction with their physicians; physician evaluation of their back pain; treatments they discussed or received; and expectations and factors related to patients feeling empowered, encouraged, and clear about next steps. This code list was reviewed and revised by the secondary coder (CH). Both analysts then coded one transcript using a draft code list and compared their coding. Codes were added and revised, and definitions were clarified on the basis of differences. After the process was repeated with a second transcript, the team believed that the code list captured the emergent issues raised by respondents. The final transcript was coded by the primary coder, who also reviewed the other transcripts to ensure consistency.
The analysis team discussed key themes of interest with other project members, prioritizing codes related to communication between physicians and patients about their CLBP. Prioritization was based on the overall frequency of the codes and issues of most importance to the field from the perspective of our research team. We did not observe substantive differences among patients in different risk groups for this subset of codes, so results are presented for all groups.
To create a coding memo, the primary coder extracted data by code and reviewed the data for subthemes and insights. The coding memo went through iterations with feedback from the secondary coder. Other team members provided feedback on a near-final version of the coding memo. The final version was used to structure the findings.
RESULTS
Participant characteristics are summarized in Table 1 by risk group. Here we present findings from our coding memo in an order that corresponds to common stages of an office visit: Listening to concerns, and validation, assessment, diagnosis, and development of treatment plan.
Table 1.
Focus group participants’ characteristics by risk groupa
| Characteristic | High (n = 10) | Medium (n = 11) | Low (n = 7) |
|---|---|---|---|
| Average age, years (range) | 58 (36–79) | 56 (25–82) | 52 (26–84) |
| Sex, no. (%) | |||
| Men | 5 (50) | 8 (73) | 4 (57) |
| Women | 5 (50) | 3 (27) | 3 (43) |
| Race, no. (%) | |||
| White | 6 (60) | 8 (73) | 4 (57) |
| Black | 2 (20) | 2 (18) | 2 (29) |
| Asian | 1 (10) | 1 (9) | 1 (14) |
| Unknown | 1 (10) | 0 (0) | 0 (0) |
Risk group: Low, medium, or high risk for persistent, disabling, chronic lower back pain in primary care settings.
Listening and Showing Empathy
Patients wished for an empathetic encounter with their physician—a visit that emphasized careful listening, getting to know the patient, and discovering what is important to them in their care and recovery. Patients described wanting their physician to try to know them and understand how pain uniquely affects their lives. Patients talked about how they did not think the physician cared about their unique experience when they felt they were rushed out of an office, or when they were not being closely listened to.
We had a doctor that we liked … and often we had to sit there and wait. But you know why we waited? Because he listened to each person, and we knew that when he came in, he was going to take his time with us. —Low-risk patient
Patients responded very well to physicians who connected with them by sharing their personal experiences with chronic pain. Patients described a belief that physicians who had not experienced chronic pain were unlikely to understand the patient’s condition or be able to truly empathize with their situation.
[M]y doctor actually had a back injury, so I think she was more sympathetic. —Medium-risk patient
Validating Pain Experience and Belief that the Pain is Real
Patients shared a desire for physicians to validate their pain experience by imparting an understanding that the way each patient experiences and relates to pain was unique. Patients thought that physicians invalidated them, or did not believe the “realness” of their pain when they were viewed as “opioid seekers”; when a physician indicated that their pain was not as strong as the patient reported; when the physician suggested the patient “buck up”; or when the patient felt put in a “box” or category of other patients. One focus group participant noted that pain is not visible so physicians might not acknowledge it. Another described a physician who was helpful about diabetes but minimized the impact of back pain.
It’s too bad you don’t have something where you can poke a button, and it shows that you’re having pain, because pain doesn’t show. And I’m not sure that all doctors believe in it ... . It very much hurt that the doctor doesn’t believe that you have all this pain. And maybe he’s never had pain like that. —High-risk patient
Performing Effective Assessment of Chronic Low Back Pain
Patients had opinions about the thoroughness or effectiveness of the back pain assessment done in their office visit. The concept of an effective assessment from the patient perspective included investigative necessities such as a physical examination or ordering an x-ray or magnetic resonance image. Patients believed that their visit was incomplete when physicians did not perform a physical examination of the affected areas, including touching/palpating painful areas. They also complained about physicians who did not ask them enough questions about their history of back pain or factors contributing to it.
I’m very frustrated. They hardly even touch you. —High-risk patient
Patients believed that imaging is critical for a definitive diagnosis. They were often dissatisfied when physicians did not order diagnostic tests. Evidence-based guidelines recommend not ordering imaging early in an episode of back pain. However, if imaging is ordered later in the course of treatment, patients may see this as a failure to provide a thorough assessment at the outset.
Finally one day, I went to her in tears, something is going on, and this is two years later. So finally she did an MRI [magnetic resonance image], and the results came back, and the doctor said, “Oh, there’s one of your disks that [is] degenerating.” —Low-risk patient
Providing a Clear Diagnosis and Information about Chronic Low Back Pain
Patients wanted physicians to give clear and specific diagnoses with information about what can be done to minimize future damage. They wanted to know when urgent care may be needed. Although the term chronic pain appears to be commonly used when talking with patients, it did not seem to help them understand their condition, in part because patients may view the term as a medical symptom rather than a diagnosis.
When I asked that question [about diagnosis], they said “Well, your condition is that you have CLBP.” Well, yes, I know that. But what is it called? I know it’s pain, I mean, do I have a slipped disk, a crushed disk? I want to know what caused it. And that’s been since 2005; we’re now [in] 2013. —High-risk patient
Patients worried that their CLBP could be an indication of more serious underlying problems such as kidney disease. In addition to wanting a clear diagnosis and a good sense of the problem, patients sought detailed information about their CLBP, including biological explanations of the cause and how the recommended treatment addresses it.
I like to know a lot of details, like a lot of details. [Quoting doctor] “Well, this is what could be happening, and this is what might help it. And physical therapy, I think that would loosen this up, and break up this particular tissue, or this is going to help.”—Low-risk patient
Patients had an awareness and frustration with the difficulty of treating back pain. They recognized that physicians do not have all the answers and realized the difficulty of treating back pain; some appreciated when physicians acknowledged that lack of certainty of how best to help a patient. Patients expressed that they liked when physicians were clear about the limits of their knowledge about CLBP and referred them to other physicians with more specialized knowledge.
I would have more respect for the doctor [if s/he were] to say, “I’m not qualified or experienced in that. Let me send you to this person that I know.” —Medium-risk patient
Although patients appreciated physician referrals or recommendations to see physical therapists, they were dismayed if they thought that physicians referred them out of frustration or because they did not want to spend time addressing their needs.
I felt kind of shoved aside. “Do the physical therapy. Here, get out of my office” kind of thing. —Medium-risk patient
Working with the Patient to Develop a Treatment Plan
Patients had experience with a variety of evidence-based and complementary and alternative treatments of back pain. In general, patients were willing to try anything a physician thought could help relieve pain and were eager for their physician to offer options. Patients reported positive experiences with primary care physicians who reviewed and inquired about previous treatments before offering other options. There was a sense that this inquiry into treatment history made for a more effective and thoughtful plan for the future.
She asked me, “What treatments have you done before for your back?” So that was important because she wanted to get my history. [She asked me,] “How have you responded to pain meds?” I said, “I don’t respond well to them, and I need to be able to function to take care of my daughter.” —Medium-risk patient
Patients wanted physicians to offer timely treatment of immediate pain relief and follow-up therapy. Patients were frustrated when they perceived physicians to not take steps to address immediate pain that severely limited function. They expressed the need to be assertive, or “steer” the physician toward a type of treatment or opportunity for follow-up. They identified a critical element of the treatment plan being clarity around when a patient should follow up with his/her physician, or when it might be appropriate to seek urgent or emergency care.
What I prefer to hear from my doctor is in many cases that you are going to get better, or if this happens, then you’re probably in that bucket, and if this happens, then you should call me and we should take care of it. When this happens, do that. As opposed to [patient speaking for doctor], “Oh, we’re hoping it will float in that direction, let’s see what happens.” —Low-risk patient
DISCUSSION
Our results highlight key aspects of care that are important to patients with CLBP and extend previous research from different health care contexts in other developed countries. A qualitative study from Australia looked at the partnership in care between physicians and patients and found that listening and demonstrating empathy was critical to the patient feeling part of a partnership. A mixed-methods study from Norway observed consultations between back pain specialists and patients and highlighted the importance that patients believe they are taken seriously. Also, a qualitative study from New Zealand found a clinician’s language and messaging had an impact on attitudes and beliefs of people with CLBP.9,14,17 Our study participants emphasized that physicians must let patients know that they believe their pain is real. Patients seek legitimization, yet may interpret some comments from physicians as implying that their pain is unimportant.18 Themes from our focus groups suggest that an effective approach to CLBP care emphasizes empathy, builds a shared understanding of what CLBP is, and includes a discussion of previous treatments. Incorporating these specific elements into care may help patients feel heard and validate their experience of pain.
Similar to other studies, our patients with CLBP wanted a specific diagnosis other than “chronic pain,” and they wanted an explanation for their pain.18–20 Patients who seek a diagnosis and do not receive one may believe their physician did not take their concerns seriously. To further help patients understand their condition, physicians should consider discussing pain concepts such as the following: 1) gate control theory,20 which offers a biological explanation of pain, including how nonpain sensory input “closes a gate” to relieve pain and why emotions influence pain perception; 2) pain centralization to help patients understand that the location of pain is not necessarily connected with a physical place in the body; and 3) pain central sensitization to explain how after an injury, the nervous system can enter into a persistent reactive state that continues even after an injury has healed.20 Explanations of chronic pain can be brief and still build understanding between the patient and physician. Having a deeper understanding of chronic pain may increase adherence to treatment plans that require active participation.
Our results confirmed that patients often expect and demand imaging; some believe that identifying the cause of pain through imaging is required to guide treatment options. This desire for imaging is challenging for physicians, who may feel forced to accommodate these demands.21,22 Similar to patient dissatisfaction with not receiving a diagnosis, we found that patients may think that physicians are not taking them seriously if they refuse to order imaging without an explanation. Talking a patient through the examination process may be a key strategy for overcoming patient wishes for imaging. A discussion point can include that imaging is not usually recommended early in an episode of back pain.4,23 One reason is that imaging rarely identifies a clear structural cause for CLBP because of the high frequency of incidental imaging findings.24 These nonrelevant findings can lead to harm such as misdiagnosis and inappropriate treatment. Physician-patient discussions should include articulating how and why serious diagnoses are ruled out and sharing the rationale for final conclusions. A patient request for imaging can be an educational opportunity and help the patient understand that the physician is fully considering the patient’s condition.25 These results highlight the importance of the development of a mutual treatment plan, including consideration of the treatments that a patient has already tried.
Patients with CLBP shared that if physicians were unable to explain the source of their pain, they nonetheless appreciated when physicians acknowledged their lack of understanding and referred them to others with more specialized knowledge. However, referral must be done thoughtfully to avoid making patients feel dismissed.10 Referrals were most appreciated when patients understood why the physician chose to refer the patient (ie, by explaining what they believe the referral may accomplish) and letting the patient know when it would be important to return for another visit and how the physician will follow-up with the patient.
A primary limitation of this study was the potential for self-selection bias. Compared with other patients with CLBP, participants may have been more concerned with the CLBP care they received or could have had more issues with their physician. All patients were from KP Washington, an integrated health care delivery system, and may have had experiences that are not generalizable to a fee-for-service setting. Nonetheless, our finding that patients reported common perspectives, regardless of their level of back-pain risk, suggests that our conclusions are applicable for a range of patients with CLBP.
CONCLUSION
This study adds new insights on aspects of physician-patient interactions around CLBP during primary care visits in the US. We learned that physicians can gain trust and foster a positive interaction with patients experiencing CLBP in the following ways: 1) listening and showing empathy, for example, sharing personal experiences of their own chronic pain; 2) admitting they do not have all the answers and being clear about how patients can benefit from referrals; 3) reviewing previous treatments before beginning a conversation about treatment options; 4) including follow-up instructions and letting patients know when it would be important to return for a visit; and 5) giving patients an explanation of their diagnosis beyond the label of “chronic pain,” with an explanation for why imaging is needed or not needed. Findings from this current research have implications for training of physicians, developing educational materials, and planning future research.
Acknowledgments
This research was funded by the Patient-Centered Outcomes Research Institute, Washington, DC (Project no. 398), and the National Center for Complementary and Integrative Health, Bethesda, MD (Grant no. 1R21AT007326). We wish to thank all of the patients who participated in our focus groups.
Kathleen Louden, ELS, of Louden Health Communications provided editorial assistance.
Footnotes
Disclosure Statement
The author(s) have no conflicts of interest to disclose.
References
- 1.Freburger JK, Holmes GM, Agans RP, et al. The rising prevalence of chronic low back pain. Arch Intern Med. 2009 Feb 9;169(3):251–8. doi: 10.1001/archinternmed.2008.543. DOI: https://doi.org/10.1001/archinternmed.2008.543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hoy D, Bain C, Williams G, et al. A systematic review of the global prevalence of low back pain. Arthritis Rheum. 2012 Jun;64(6):2028–37. doi: 10.1002/art.34347. DOI: https://doi.org/10.1002/art.34347. [DOI] [PubMed] [Google Scholar]
- 3.Croft PR, Dunn KM, Raspe H. Course and prognosis of back pain in primary care: The epidemiological perspective. Pain. 2006 May;122(1–2):1–3. doi: 10.1016/j.pain.2006.01.023. DOI: https://doi.org/10.1016/j.pain.2006.01.023. [DOI] [PubMed] [Google Scholar]
- 4.Chou R, Deyo RA, Jarvik JG. Appropriate use of lumbar imaging for evaluation of low back pain. Radiol Clin North Am. 2012 Jul;50(4):569–85. doi: 10.1016/j.rcl.2012.04.005. DOI: https://doi.org/10.1016/j.rcl.2012.04.005. [DOI] [PubMed] [Google Scholar]
- 5.Chou R, Huffman LH American Pain Society; American College of Physicians. Medications for acute and chronic low back pain: A review of the evidence for an American Pain Society/American College of Physicians clinical practice guideline. Ann Intern Med. 2007 Oct 2;147(7):505–14. doi: 10.7326/0003-4819-147-7-200710020-00008. DOI: https://doi.org/10.7326/0003-4819-147-7-200710020-00008. [DOI] [PubMed] [Google Scholar]
- 6.Corbett M, Foster NE, Ong BN. Living with low back pain—stories of hope and despair. Soc Sci Med. 2007 Oct;65(8):1584–94. doi: 10.1016/j.socscimed.2007.06.008. DOI: https://doi.org/10.1016/j.socscimed.2007.06.008. [DOI] [PubMed] [Google Scholar]
- 7.Silvis WL, Lakke SE, Stegeman P, et al. Groningen Spine Study Group. Can patients with low back pain be satisfied with less than expected? Spine (Phila Pa 1976) 2016 Oct 15;41(20):1606–12. doi: 10.1097/BRS.0000000000001592. DOI: https://doi.org/10.1097/brs.0000000000001592. [DOI] [PubMed] [Google Scholar]
- 8.Azoulay L, Ehrmann-Feldman D, Truchon M, Rossignol M. Effects of patient-clinician disagreement in occupational low back pain: A pilot study. Disabil Rehabil. 2005 Jul 22;27(14):817–23. doi: 10.1080/09638280400018684. DOI: https://doi.org/10.1080/09638280400018684. [DOI] [PubMed] [Google Scholar]
- 9.Laerum E, Indahl A, Skouen JS. What is “the good back-consultation”? A combined qualitative and quantitative study of chronic low back pain patients’ interaction with and perceptions of consultations with specialists. J Rehabil Med. 2006 Jul;38(4):255–62. doi: 10.1080/16501970600613461. DOI: https://doi.org/10.1080/16501970600613461. [DOI] [PubMed] [Google Scholar]
- 10.Upshur CC, Bacigalupe G, Luckmann R. “They don’t want anything to do with you”: Patient views of primary care management of chronic pain”. Pain Med. 2010 Dec;11(12):1791–8. doi: 10.1111/j.1526-4637.2010.00960.x. DOI: https://doi.org/10.1111/j.1526-4637.2010.00960.x. [DOI] [PubMed] [Google Scholar]
- 11.Clever SL, Jin L, Levinson W, Meltzer DO. Does doctor-patient communication affect patient satisfaction with hospital care? Results of an analysis with a novel instrumental variable. Health Serv Res. 2008 Oct;43(5 Pt 1):1505–19. doi: 10.1111/j.1475-6773.2008.00849.x. DOI: https://doi.org/10.1111/j.1475-6773.2008.00849.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zolnierek KB, Dimatteo MR. Physician communication and patient adherence to treatment: A meta-analysis. Med Care. 2009 Aug;47(8):826–34. doi: 10.1097/MLR.0b013e31819a5acc. DOI: https://doi.org/10.1097/mlr.0b013e31819a5acc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Michie S, Miles J, Weinman J. Patient-centredness in chronic illness: What is it and does it matter? Patient Educ Couns. 2003 Nov;51(3):197–206. doi: 10.1016/s0738-3991(02)00194-5. DOI: https://doi.org/10.1016/s0738-3991(02)00194-5. [DOI] [PubMed] [Google Scholar]
- 14.Darlow B, Dowell A, Baxter GD, Mathieson F, Perry M, Dean S. The enduring impact of what clinicians say to people with low back pain. Ann Fam Med. 2013 Nov-Dec;11(6):527–34. doi: 10.1370/afm.1518. DOI: https://doi.org/10.1370/afm.1518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hill JC, Whitehurst DG, Lewis M, et al. Comparison of stratified primary care management for low back pain with current best practice (STarT Back): A randomised controlled trial. Lancet. 2011 Oct 29;378(9802):1560–71. doi: 10.1016/S0140-6736(11)60937-9. DOI: https://doi.org/10.1016/S0140-6736(11)60937-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007 Dec;19(6):349–57. doi: 10.1093/intqhc/mzm042. DOI: https://doi.org/10.1093/intqhc/mzm042. [DOI] [PubMed] [Google Scholar]
- 17.Slade SC, Molloy E, Keating JL. ‘Listen to me, tell me’: A qualitative study of partnership in care for people with non-specific chronic low back pain. Clin Rehabil. 2009 Mar;23(3):270–80. doi: 10.1177/0269215508100468. DOI: https://doi.org/10.1177/0269215508100468. [DOI] [PubMed] [Google Scholar]
- 18.Newton BJ, Southall JL, Raphael JH, Ashford RL, LeMarchand K. A narrative review of the impact of disbelief in chronic pain. Pain Manag Nurs. 2013 Sep;14(3):161–71. doi: 10.1016/j.pmn.2010.09.001. DOI: https://doi.org/10.1016/j.pmn.2010.09.001. [DOI] [PubMed] [Google Scholar]
- 19.Melzack R, Wall PD. Pain mechanisms: A new theory. Science. 1965 Nov 19;150(3699):971–9. doi: 10.1126/science.150.3699.971. DOI: https://doi.org/10.1016/s1082-3174(96)80062-6. [DOI] [PubMed] [Google Scholar]
- 20.Woolf CJ. Central sensitization: Implications for the diagnosis and treatment of pain. Pain. 2011 Mar;152(3 Suppl):S2–15. doi: 10.1016/j.pain.2010.09.030. DOI: https://doi.org/10.1016/j.pain.2010.09.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chenot JF, Scherer M, Becker A, et al. Acceptance and perceived barriers of implementing a guideline for managing low back in general practice. Implement Sci. 2008 Feb 7;3:7. doi: 10.1186/1748-5908-3-7. DOI: https://doi.org/10.1186/1748-5908-3-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Schers H, Wensing M, Huijsmans Z, van Tulder M, Grol R. Implementation barriers for general practice guidelines on low back pain: A qualitative study. Spine (Phila Pa 1976) 2001 Aug 1;26(15):E348–53. doi: 10.1097/00007632-200108010-00013. DOI: https://doi.org/10.1097/00007632-200108010-00013. [DOI] [PubMed] [Google Scholar]
- 23.Jarvik JG, Gold LS, Comstock BA, et al. Association of early imaging for back pain with clinical outcomes in older adults. JAMA. 2015 Mar 17;313(11):1143–53. doi: 10.1001/jama.2015.1871. DOI: https://doi.org/10.1001/jama.2015.1871. [DOI] [PubMed] [Google Scholar]
- 24.Balagué F, Mannion AF, Pellisé F, Cedraschi C. Non-specific low back pain. Lancet. 2012 Feb 4;379(9814):482–91. doi: 10.1016/S0140-6736(11)60610-7. DOI: https://doi.org/10.1016/s0140-6736(11)60610-7. [DOI] [PubMed] [Google Scholar]
- 25.Balderson BHK, Lin EHB, Von Korff M. The management of pain-related fear in primary care. In: Asmundson GJG, Vlaeyen JWS, Crombez G, editors. Understanding and treating fear of pain. Oxford, UK: Oxford University Press; 2004. pp. 267–9. [Google Scholar]