Abstract
Context
Atypical defecation habits are common and distressing for children and families and can have a major impact on quality of life. Often, no underlying factor can be identified, and the defecation disorder is considered functional. Current interventions are not successful for up to 50% of children. We suggest this high failure rate may be caused by lack of consistency in descriptors of behavioral indicators for functional defecation problems. Most investigations and descriptors focus on general behavior. There are fewer reports concerning defecation-specific behaviors.
Objective
To develop a thorough inventory of defecation-specific behaviors, providing a more informed foundation for assessment and intervention.
Design
A systematic review of six common databases was performed following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses recommendations. Reference lists of retained articles were screened for additional studies.
Main Outcome Measures
Content analysis was used to classify defecation-specific behaviors into 17 categories.
Results
Our search yielded 2677 articles; 98 peer-reviewed publications were retained for full-text review, and 67 articles were included in the final qualitative synthesis. Although there is inconsistency in reported diagnostic criteria, stool withholding and manifesting pain on defecation are the most commonly reported defecation-specific behaviors. In the studies that included children with autism or attention-deficit/hyperactivity disorder, the defecation-specific behaviors were not unique to the diagnostic group.
Conclusion
Consistent use of established diagnostic criteria, along with use of behaviors identified through this review, lay a foundation for more effective interventions.
INTRODUCTION
Atypical defecation habits are a common and distressing condition for children and families and can have a major impact on quality of life.1,2 Given that they can be so impactful, appropriate and clear identification of problematic defecation behaviors is crucial. Research looking at behaviors associated with functional defecation concerns has taken 2 approaches. The most frequent has been to examine general behavioral concerns; considerably less common has been research concentrating on defecation-specific behaviors. However, both general and defecation-specific behavioral concerns are thought to play an important role in the development and in the persistence of constipation.3 A deeper understanding of the behaviors reflective of actual toileting and defecation problems could provide greater insight into the unique manifestations of functional defecation disorders and thus a better foundation for treatment. Because approximately 25% to 50% of children do not fully recover from functional defecation disorders despite medical management and therapeutic strategies,3,4 reconsidering our understanding of these disorders is imperative.
When referring to gastrointestinal disorders, the term functional is used to describe conditions that cannot be linked to a single discrete underlying biological etiology and are the result of the interaction between psychosocial factors and altered gut physiology via the brain-gut axis.5 The Rome Foundation diagnostic criteria are considered a gold standard for identification of functional gastrointestinal disorders.4,5 In the case of childhood functional defecation disorders, the clinical manifestations typically result from an interaction of physiologic, social, and behavioral processes.1,2 As such, once organic pathology has been ruled out, clinicians are often faced with myriad simultaneous and interdependent behaviors that cannot be easily teased apart, described, or classified. For example, the clinician must evaluate the impact of the caregiver’s behavior on the child’s gastrointestinal tract processes (eg, punishment for involuntary fecal incontinence, unrealistic expectations), the child’s response to the caregiver (eg, stubbornness, toileting refusal), the impact of gastrointestinal processes on the child’s behavior (eg, painful defecation), and the impact of the child’s behavior on the gastrointestinal processes (eg, voluntary stool withholding). Enhancing our understanding of these specific behavioral elements could help optimize outcomes.
The behaviors of children with atypical toileting habits is a longstanding subject of study and continues to be a central issue of debate.6 Most reports focus on otherwise healthy children and general behavior using measures such as the Child Behavior Checklist.7 Although most studies indicate a higher incidence of general behavioral issues in these children,8–14 others fail to find this difference.15–17
Several reports exist concerning the elevated incidence of defecation issues in children with a diagnosis of autism spectrum disorder (ASD)18–20 or attention-deficit/hyperactivity disorder (ADHD),21,22 but studies addressing the behaviors of children with these comorbidities are scarce. A few studies have specifically looked at the general behavior of children with autism and toileting issues. For instance, Peeters et al23 report an association between mixed bowel symptoms and rigid-compulsive behaviors in children with ASD. Other studies point to a relationship between maladaptive behaviors and gastrointestinal issues in this population.24,25 Studies dealing with the behavioral characteristics of children with ADHD and toileting issues were not found.
There are few reports concerning the defecation-specific behaviors of children with constipation, fecal incontinence, and/or stool toileting refusal. One older study compared children with encopresis and asymptomatic siblings and nonsiblings.26 Using an automated telephone survey system, caregivers reported that children with encopresis voluntarily went to the toilet the same number of times each day as did controls. However, caregivers also reported a significantly greater amount of pain associated with defecation among children with encopresis. Cox et al27 provided some early guidance for distinguishing between defecation-specific behaviors and generic behavioral concerns (eg, noncompliant to toileting instructions vs generally noncompliant) in children with encopresis using the Virginia Encopresis-Constipation Apperception Test. On the basis of this tool, both children with encopresis and their mothers reported more bowel-specific problems, but not more generic behavior problems, compared with controls.27 Burket et al9 added the dimension of stubbornness to the study of behavior in children with defecation issues, and differentiated between specific and generic toileting stubbornness. Together these studies suggest that general behavior concerns and bowel-related behavior concerns can be differentiated and that bowel-related concerns may be more useful in defining the problem.
Concomitantly with consideration of behavior and stubbornness, research has also focused on physical factors, such as pain, as contributing to functional defecation issues. Pain on defecation as well as stool withholding to avoid pain have been identified as problematic in children with chronic functional constipation and fecal incontinence; these behaviors also differentiate children with and without functional defecation disorders. Dehghani et al28 identified painful defecation and stool withholding behavior in almost all of the 222 children with constipation studied. Kammacher Guerreiro et al29 came to similar conclusions in a retrospective study of 270 children with functional constipation, reporting that among the most frequent complaints were pain during defecation and stool retention. Borowitz and colleagues26 found that defecation-related pain was also common in children with encopresis.
Despite these insights, no review and synthesis of the reported defecation-specific behaviors and other concerns associated with functional defecation disorders could be found in the literature, making it challenging to comprehensively characterize these children and to clearly delineate behaviors indicating a need for specific intervention. Importantly, although toileting concerns have been identified in children with ASD and ADHD, it is unclear whether these are specific to the diagnosis or consistent with behaviors seen in children without these additional diagnoses. The aim of this review was to develop a thorough inventory of reported defecation-specific behaviors and to document their frequency, providing a more informed foundation for assessment and intervention. Although there is a large body of literature addressing behavioral treatment approaches for children with defecation issues,30–33 a thorough summary of this literature is beyond the scope of this review.
The objectives, inclusion criteria, and methods of analysis for this review were specified in advance and documented in a protocol registered with the PROSPERO database (registration number CRD42016039436).
METHODS
Answers to the following questions were sought: In children with functional defecation issues (constipation, fecal incontinence, encopresis, stool toileting refusal), which defecation-specific behaviors have been identified, and to what extent? Considering the descriptive nature of the inquiry, the PEO (population, exposure, outcome) model for systematic review was used to formulate the research question.34 The elements of the PEO question are as follows: 1) population: children age 0 to 18 years; 2) exposure: functional defecation issues (constipation, fecal incontinence, encopresis, stool toileting refusal); and 3) outcome or themes: defecation-specific behaviors.
Search Strategy
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement35,36 was used to guide the systematic review. An electronic database search of the Cumulative Index to Nursing & Allied Health Literature (CINAHL), Embase, PsycINFO, MEDLINE, The Cochrane Library, and Scopus was conducted to retrieve relevant articles for the literature review. Key terms used for the advanced search were: behavior, behaviour, constipation, fecal incontinence, faecal incontinence, elimination disorder*, dysfunctional elimination syndrome, encopresis, toileting, stool toileting refusal, soiling, and defecation. The table of contents of all issues of the Journal of Pediatric Gastroenterology and Nutrition was also reviewed using the same terms. The search strategy and the chosen keywords were developed and revised by the first (IBB) and second (DB) authors; DB is an experienced librarian.
Data Selection
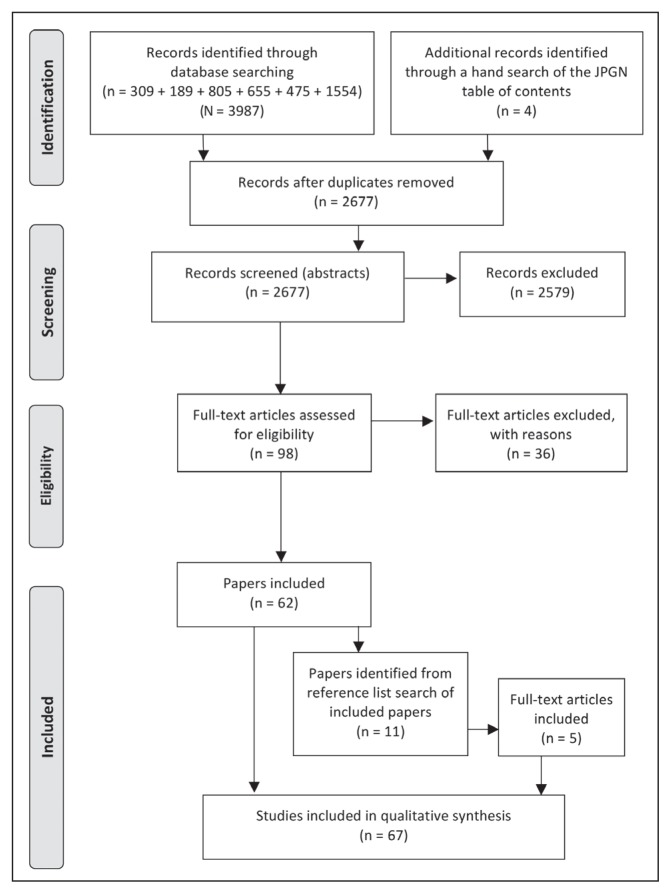
Included articles met the following criteria: Addressed functional (not organic) defecation issues; described defecation-specific (not generic) behavioral concerns; focused on children ages 0 to 18 years; were published in English, Spanish, or French with an English abstract (IBB is fluent in these languages); appeared in a peer-reviewed journal; and were at any level of evidence. Given that the incidence of defecation issues is higher in children with ASD18–20 and/or ADHD,21,22 studies that included children with these diagnoses were also included in the review, but studies focused on children with other diagnoses were not. Given that no other review of this type has been identified, the search included all articles since the inception date of each database through August 2016. Articles were excluded if they addressed organic defecation issues, focused on generic behaviors, included subjects older than age 18 years, were review articles, or discussed the same study sample as another previous publication. Reference lists of included studies were reviewed for relevant publications. Table 1 illustrates an example of the search strategy, and Figure 1 illustrates the PRISMA flow diagram of searched results.
Table 1.
MEDLINE search strategy, August 6, 2016
| Number | Search terms | Results |
|---|---|---|
| 1 | Constipation | 20,452 |
| 2 | Fecal incontinence | 9493 |
| 3 | Faecal incontinence | 1578 |
| 4 | Elimination disorder* | 66 |
| 5 | Dysfunctional elimination syndrome | 46 |
| 6 | Encopresis | 793 |
| 7 | Toileting | 687 |
| 8 | Stool toileting refusal | 15 |
| 9 | Soiling | 1426 |
| 10 | Defecation | 9591 |
| 11 | 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 | 36,433 |
| 12 | Behaviour | 139,611 |
| 13 | Behavior | 833,960 |
| 14 | 12 or 13 | 934,250 |
| 15 | 11 and 14 | 2516 |
| 16 | Limit 15 to humans | 1555 |
| 17 | Limit 16 to “all child (0 to 18 years)” | 707 |
| 18 | Limit 17 to (English or French or Spanish) | 655 |
Figure 1.
PRISMA 2009 flow diagram for all sources searched (August 2016).
JPGN = Journal of Pediatric Gastroenterology and Nutrition; PRISMA = Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
The first two authors identified search terms and strategy; the first author performed the initial comprehensive literature search and filtered for duplicates. After duplicates were removed, IBB and the third author (SJL) screened each study title and abstract for potential relevance. When disagreement was identified between reviewers, the full text of the article was retrieved; disagreements were again considered and discussed until consensus was reached. If disagreements had persisted, a third reviewer would have been consulted to determine final inclusion, but this was not necessary. The reviewers kept a log of all reviewed abstracts with reasons for inclusion or exclusion of articles. The full text of articles included in the final selection was reviewed by the first author. A data extraction table was used to organize the information extracted from each of the selected citations (see Table 2, available online at: www.thepermanentejournal.org/files/2017/17-047-Table2.pdf).
Data Analysis
The descriptive nature of this inquiry supports using conventional content analysis.37,38 This approach made it possible to distill words into content-specific categories and enabled us to identify and to categorize the behaviors. Engaging in content analysis enabled the investigators to immerse themselves in the data and develop categories; here we used the process of abstraction to develop mutually exclusive categories of defecation-specific behaviors. The PDF (portable document format) files of the eligible studies were imported into qualitative data analysis software (NVivo, version 11; QSR International Pty Ltd, Doncaster, Victoria, Australia) to facilitate this analysis. No preconceived categories were established. The categories emerged from the data through repeated reading of the narrative descriptions of behavior, with the link to toileting and defecation driving the creation of the final classifications.
RESULTS
Our search yielded 3991 citations. After eliminating duplicates, we screened titles, abstracts, and keywords of 2677 citations. We excluded 2579 citations that did not match our research question; largely these citations focused on hygiene behavior relative to toileting and stool disposal in developing countries. DB was consulted on the possibility of narrowing the search; however, this would have involved the risk of missing citations relevant to the research question and was therefore dismissed. Ninety-eight peer-reviewed publications were retained for full-text review. After full-text review, 36 articles were excluded as follows: Behaviors not defecation specific (n = 21), sample/study is described in another publication (n = 5), concomitant diagnosis other than ASD or ADHD (n = 6), subjects outside the age range (n = 1), defecation issues are not functional (n = 1), article is a review (n = 1), and article is not peer reviewed (n = 1). From the reference lists of the resulting 62 articles, 5 additional articles were identified. A total of 67 articles published between 1953 and 2016, representing 18 countries worldwide, were included in the final content analysis.
Because most of the citations belonged to observational studies, the Joanna Briggs Institute (JBI) evidence ranking system was chosen.39 The JBI is a nonprofit research organization at the University of Adelaide in Australia whose approach to evidence-based health care considers the feasibility, appropriateness, meaningfulness, and effectiveness of health care practices. This system offers detailed subcategories for observational studies, differentiating it from other systems, which are less specific for this type of research. For example, the JBI system categorizes observational analytic designs (Level 3) and observational descriptive studies (Level 4) into a total of 9 subcategories. According to the JBI system, 7 citations were Level 1 studies,40–46 3 were Level 2 studies,27,47,48 12 were classified at Level 3,15,24,49–58 35 belonged to Level 4,9,26,28,59–90 and 10 were expert opinions classified at Level 5.91–100 (Details of subcategories can be found in Table 2, available online at: www.thepermanentejournal.org/files/2017/17-047-Table2.pdf.)
Defecation behaviors were described as part of the characterization of the samples in multiple studies.a An additional 18 studies, specifically aimed at identifying clinical features of children with functional defecation issues, described toileting-specific behaviors as part of the results section of the article.b The remaining 12 articles included the description of toileting and defecation behaviors as expert clinical observations91–100 or in the discussion section of the article.64,70
Toileting and Defecation Behaviors
Narrative descriptions of reported defecation behaviors were classified by IBB into preliminary categories using common themes. Credibility and dependability of these themes were established through discussion between IBB and SJL. This iterative process allowed us to refine categories and create groupings that would fully capture the subtle differences in the behaviors described in the literature.37 For example, some children are described as always refusing to sit on the toilet, whereas others manifest refusal of the toilet only for defecation, and some refuse to use the toilet only when outside their home; each of these variations of toilet refusal was categorized separately. Another example of this effort relates to resisting the urge to defecate. Stool withholding is often mentioned as a common behavior; however, some authors additionally describe retentive posturing and movement as a means to avoid defecation. As such, stool withholding alone and retentive efforts accompanied by specific postures or movements have been categorized separately.
Furthermore, to offer an accurate summary of the narrative description of children’s behavior, we chose to consider as part of the behavioral categories all types of responses and manifestations of psychological or emotional distress, such as fear or anxiety. This decision was based on the following definition of behavior: “anything that an organism does involving action and response to stimulation; the response of an individual, group, or species to its environment.”101
A total of 17 behavioral categories were established, with defecation-related manifestations of pain and stool withholding behavior being the most frequently reported defecation-specific behaviors in children with functional defecation disorders. Different types of toilet refusal behaviors are also frequently reported. Table 3 shows the number of articles that reference each of the 17 established behavioral categories.
Table 3.
Defecation-specific behaviors identified in the literature
| Behavior | Number of articles referencing/describing the behavior |
|---|---|
| Manifests pain or fear of pain on defecation or urge to defecate | 40 |
| Withholds stool/avoidance of defecation/resists the urge to defecate | 39 |
| Refuses to defecate in toilet (accepts to urinate in toilet)/stool toileting refusal | 16 |
| Refuses to sit on toilet/manifests fear or anxiety in relation to sitting on toilet (in all contexts, even at home) | 16 |
| Retentive posturing/moves in a particular way when urge to defecate | 12 |
| Asks for/waits for/prefers a diaper or pull-up to defecate | 11 |
| Refuses/is reluctant to use school toilet or to use a variety of toilets (accepts toilet at home) | 9 |
| Hides to defecate or on urge to defecate, refuses to defecate in presence of others | 9 |
| Straining/prolonged time needed to have a bowel movement | 9 |
| Denies incontinence/hides soiled underwear | 6 |
| Does not manifest sensation of urge to defecate/denies or ignores urge to defecate | 6 |
| Defecates in a specific place other than toilet after being toilet trained | 5 |
| Not upset by soiling/does not notice incontinence | 4 |
| Manifests fear/resistance of wiping after a bowel movement/soiling | 3 |
| Manifests fear of flushing toilet | 2 |
| Manifests aversion to smell of feces | 1 |
| Manifests fear of feces | 1 |
Clear classifications based on defecation diagnosis could not be made; a review of the retained publications shows that the identified categories of defecation behaviors are seen across studies and do not appear to be exclusive to any particular gastrointestinal diagnosis or defecation disorder. Thus, we could not explore the relationship between specific defecation disorders and defecation-specific behaviors because 1) diversity of diagnostic criteria across studies makes it difficult to clearly classify articles according to specific defecation disorders and 2) several articles refer to samples that group together children with different defecation issues or with more than one diagnosis.
Concomitant Diagnosis of Autism Spectrum Disorder
Among the articles retained from the systematic review, six articles include children with a diagnosis of autism.24,65,70,76,83,84 The behaviors of these children are similar to those of children with defecation issues without any concomitant diagnosis; manifestations of pain in relation to defecation, stool withholding behavior, and all variants of toilet refusal are common. Table 4 shows the number of articles describing children with autism that reference the established behavioral categories.
Table 4.
Number of articles that document toileting and defecation-specific behaviors in children with defecation disorders and a concomitant diagnosis of autism spectrum disorder (ASD) or attention-deficit/hyperactivity disorder (ADHD).
| Defecation-specific behaviors | Number of references | |
|---|---|---|
| ASD | ADHD | |
| Pain | 2 | 2 |
| Withhold | 3 | 2 |
| Refuse toilet | 3 | 0 |
| Stool toileting refusal | 1 | 0 |
| Posture | 0 | 0 |
| Diaper | 2 | 0 |
| Hide | 2 | 0 |
| Refuse school toilet | 2 | 0 |
| Straining | 0 | 0 |
| Deny fecal incontinence | 0 | 0 |
| Deny urge | 0 | 1 |
| Not feel fecal incontinence | 0 | 0 |
| Place | 2 | 0 |
| Wiping | 1 | 0 |
| Flushing | 1 | 0 |
| Smell | 0 | 0 |
| Fear feces | 0 | 0 |
Concomitant Diagnosis of Attention-Deficit/Hyperactivity Disorder
Among the articles retained from the systematic review, four included children with a diagnosis of ADHD.26,53,70,82 Once again, manifestations of pain in relation to defecation and stool withholding behavior are the most commonly reported defecation-specific behaviors. Table 4 shows the number of articles describing children with ADHD that reference the established behavioral categories.
DISCUSSION
To our knowledge, this is the first systematic review concerning defecation-specific behavior in children with functional defecation issues. Our search strategy included three languages (English, French, Spanish), six databases from their inception through 2016, the table of contents of the Journal of Pediatric Gastroenterology and Nutrition, and the reference lists of all included articles. Content analysis was used to determine behavioral categories, which were determined to be both credible and dependable.
The key findings of this study were: The identification of 17 unique categories of defecation-specific behaviors and delineation of the frequency of reporting for each. Our findings support and extend previous work in this area.9,26,27 These categories can now provide researchers and clinicians with a foundation for a clearer identification of, and differentiation between, functional defecation disorders. To date, there has been no consensus on how to assess, classify, or address these behaviors. Given that current long-term success rates using conventional treatment regimens remain limited,3,4 there is an urgent need for consistency in the description of defecation-specific concerns to enable optimal classification and lay the foundation for focused interventions. We suggest that the descriptors identified in this review are a place to begin.
These findings move us beyond simply identifying a defecation-related behavior in broad, superficial terms, in a way that parallels previous research,51,63 which guided clarification of fecal soiling. We now consider retentive and nonretentive fecal incontinence as very different conditions that require different treatment approaches. Such may be the case with other defecation-related behaviors, which once clarified and described in greater detail, could lead to better treatment.
Further analysis of each of the identified defecation-specific behavioral categories in this review may be needed to broaden our comprehension of the psychoemotional factors related to the observable behaviors common to children with functional defecation disorders. For instance, a behavior such as stool toileting refusal is not unique to a specific defecation disorder and is often described as a disorder in itself15,52,73,99 or in association with other concomitant diagnosesc or temperamental characteristics.9,80 The most frequently reported associations with this common childhood behavior are constipation and painful defecation.d However, encopresis,44,45,51,83,92,98 sensory overresponsivity,59,76,84 anxiety,89,95,99 difficult temperament,9,80 autism,65,76,83 and oppositional defiant disorder86 have also been linked to stool toileting refusal. Differentiating subgroups in the group with this common behavior may be necessary to provide clearer direction for treatment.
Diagnostic Criteria
In addition to inviting researchers to deepen our understanding of common toileting behaviors in children with functional defecation issues, this review also summons a reflection on diagnostic criteria. The Rome Foundation’s diagnostic criteria are the most frequently cited in this review,e but others such as the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders (DSM) criteria for encopresis47,63,76,91,99 or the North American Society for Pediatric Gastroenterology, Hepatology and Nutrition description of constipation50 are also cited. However, it is noteworthy that most articles in this review (n = 52) do not reference any standardized diagnostic criteria. In many cases, researchers develop their own questionnaires and/or criteria using definitions found in the literature. This variability in diagnostic criteria makes it difficult to comprehensively appraise the research. Future studies should aim to use internationally accepted diagnostic criteria, such as Rome IV, for diagnosis, and develop surveys or questionnaires that tap into the 17 defecation-specific behaviors identified in this study to clarify the link between specific behaviors and functional defecation disorders.
It is also necessary to consider a deeper understanding of toileting behavior in relation to diagnosis. For example, the DSM-V criteria for encopresis, the second most frequently cited diagnostic criterion in this review, includes the repeated passage of feces into inappropriate places, either voluntarily or involuntarily. Considering this definition more closely, if a child voluntarily chooses to defecate in an unorthodox place, can we consider this child to have the same diagnosis as the child who involuntarily defecates in his clothing? If a child feels the urge to defecate, momentarily withholds stool, voluntarily goes to a specific place, although it may not be a socially acceptable one, and then proceeds to defecate, does s/he not possess all the elements of continence? The only problem is where the child chooses to defecate. The questions might be why is the child not able to accept the socially acceptable place, what are the features of this chosen place that the child is seeking, and what features of the socially acceptable place is he avoiding? On the other hand, the child who involuntarily defecates in his clothing shows none of the elements of continence. Considering voluntary and involuntary defecation together, simply because it is not in the toilet, does not make sense as we strive to ameliorate our understanding of functional defecation disorders.
Limitations
Although we saw including all levels of evidence as essential to answering the question posed in this review, the inclusion of weaker study designs may be seen as a limitation. However, given the intent of this investigation to produce a broad inventory of defecation-specific behaviors associated with functional defecation concerns, the broad inclusion of literature was appropriate. A second limitation is the restriction of diagnostic conditions to ASD and ADHD. However, defecation concerns are highly common in these two high-frequency diagnostic groups, making this choice logical. We acknowledge that conventional content analysis, a qualitative data analysis method, is open to subjectivity and represents a third limitation of this review. However, we have endeavored to establish rigor through the use of qualitative software and establishment of credibility and dependability of data. Finally, we are aware that a simple tally does not represent an in-depth analysis of results; however, given that the goal of this review was to develop an inventory of defecation-specific behaviors, this method provides a valid means by which to report our results.
CONCLUSION
Our review delineated 17 unique behaviors that have been identified as characterizing functional defecation concerns. We also identified a lack of consensus, fueled partly by the differences in diagnostic criteria but also in relation to assessment and classification of defecation-specific behaviors. Furthermore, this review found that defecation-specific behaviors overlap across functional defecation disorders and, on the basis of the limited evidence available, that the defecation behaviors of children with autism or ADHD are not unique to their diagnostic group. Moving forward, we suggest that we look at defecation-specific behaviors, rather than more general behaviors, in defining issues specifically related to defecation concerns. This work provides some guidelines for characterization that go beyond that of current diagnostic guidelines or existing assessment tools in looking at the context of behaviors.
Acknowledgment
Kathleen Louden, ELS, of Louden Health Communications provided editorial assistance.
Footnotes
Disclosure Statement
The author(s) have no conflicts of interest to disclose.
Author Contributions
Isabelle Beaudry-Bellefeuille conducted the systematic review and wrote the manuscript.
Debbie Booth assisted Isabelle Beaudry-Bellefeuille in the literature search.
Shelly J Lane reviewed all included abstracts and reviewed and edited each draft of the manuscript.
References
- 1.Afzal NA, Tighe MP, Thomson MA. Constipation in children. Ital J Pediatr. 2011 Jun 13;37:28. doi: 10.1186/1824-7288-37-28. DOI: https://doi.org/10.1186/1824-7288-37-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Freeman KA, Riley A, Duke DC, Fu R. Systematic review and meta-analysis of behavioral interventions for fecal incontinence with constipation. J Pediatr Psychol. 2014 Sep;39(8):887–902. doi: 10.1093/jpepsy/jsu039. DOI: https://doi.org/10.1093/jpepsy/jsu039. [DOI] [PubMed] [Google Scholar]
- 3.Bongers ME, van Wijk MP, Reitsma JB, Benninga MA. Long-term prognosis for childhood constipation: Clinical outcomes in adulthood. Pediatrics. 2010 Jul;126(1):e156–62. doi: 10.1542/peds.2009-1009. DOI: https://doi.org/10.1542/peds.2009-1009. [DOI] [PubMed] [Google Scholar]
- 4.Pijpers MA, Bongers ME, Benninga MA, Berger MY. Functional constipation in children: A systematic review on prognosis and predictive factors. J Pediatr Gastroenterol Nutr. 2010 Mar;50(3):256–68. doi: 10.1097/MPG.0b013e3181afcdc3. DOI: https://doi.org/10.1097/mpg.0b013e3181afcdc3. [DOI] [PubMed] [Google Scholar]
- 5.Drossman DA. The functional gastrointestinal disorders and the Rome III process. Gastroenterology. 2006 Apr;130(5):1377–90. doi: 10.1053/j.gastro.2006.03.008. DOI: https://doi.org/10.1053/j.gastro.2006.03.008. [DOI] [PubMed] [Google Scholar]
- 6.Rajindrajith S, Devanarayana NM, Crispus Perera BJ, Benninga MA. Childhood constipation as an emerging public health problem. World J Gastroenterol. 2016 Aug 14;22(30):6864–75. doi: 10.3748/wjg.v22.i30.6864. DOI: https://doi.org/10.3748/wjg.v22.i30.6864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Achenbach TM. Manual for the child behavior checklist/4–18 and 1991 profile. Burlington, VT: University of Vermont, Department of Psychiatry; 1991. [Google Scholar]
- 8.Benninga MA, Voskuijl WP, Akkerhuis GW, Taminiau JA, Büller HA. Colonic transit times and behaviour profiles in children with defecation disorders. Arch Dis Child. 2004 Jan;89(1):13–6. [PMC free article] [PubMed] [Google Scholar]
- 9.Burket RC, Cox DJ, Tam AP, et al. Does “stubbornness” have a role in pediatric constipation? J Dev Behav Pediatr. 2006 Apr;27(2):106–11. doi: 10.1097/00004703-200604000-00004. DOI: https://doi.org/10.1097/00004703-200604000-00004. [DOI] [PubMed] [Google Scholar]
- 10.Demir T, Yavuz M, Doğangün B, et al. Behavioral problems of encopretic children and their familial characteristics. Turk Pediatri Ars. 2012 Mar;47(1):35–9. DOI: https://doi.org/10.4274/tpa.582. [Google Scholar]
- 11.Holman KS. Parent and child functioning in a community sample of children with constipation [dissertation] [Internet] Milwaukee, WI: University of Wisconsin-Milwaukee, ProQuest Dissertations Publishing; 2012. [cited 2016 Aug 15]. Available from: http://gradworks.umi.com/35/20/3520627.html. [Password protected] [Google Scholar]
- 12.Joinson C, Heron J, Butler U, von Gontard A Avon Longitudinal Study of Parents and Children Study Team. Psychological differences between children with and without soiling problems. Pediatrics. 2006 May;117(5):1575–84. doi: 10.1542/peds.2005-1773. DOI: https://doi.org/10.1542/peds.2005-1773. [DOI] [PubMed] [Google Scholar]
- 13.van Dijk M, Benninga MA, Grootenhuis MA, Last BF. Prevalence and associated clinical characteristics of behavior problems in constipated children. Pediatrics. 2010 Feb;125(2):e309–17. doi: 10.1542/peds.2008-3055. DOI: https://doi.org/10.1542/peds.2008-3055. [DOI] [PubMed] [Google Scholar]
- 14.Young MH, Brennen LC, Baker RD, Baker SS. Functional encopresis: Symptom reduction and behavioural improvement. J Dev Behav Pediatr. 1995 Aug;16(4):226–32. DOI: https://doi.org/10.1097/00004703-199508000-00003. [PubMed] [Google Scholar]
- 15.Blum NJ, Taubman B, Osborne ML. Behavioral characteristics of children with stool toileting refusal. Pediatrics. 1997 Jan;99(1):50–3. doi: 10.1542/peds.99.1.50. DOI: https://doi.org/10.1542/peds.99.1.50. [DOI] [PubMed] [Google Scholar]
- 16.Friman PC, Mathews JR, Finney JW, Christophersen ER, Leibowitz JM. Do encopretic children have clinically significant behavior problems? Pediatrics. 1988 Sep;82(3 Pt 2):407–9. [PubMed] [Google Scholar]
- 17.Ozokutan BH, Zoroglu S, Ceylan H, Ozkan KU. Psychological evaluation of children with idiopathic constipation and their parents. Pediatr Int. 2005 Jun;47(3):311–5. doi: 10.1111/j.1442-200x.2005.02061.x. DOI: https://doi.org/10.1111/j.1442-200x.2005.02061.x. [DOI] [PubMed] [Google Scholar]
- 18.Kang V, Wagner GC, Ming X. Gastrointestinal dysfunction in children with autism spectrum disorders. Autism Res. 2014 Aug;7(4):501–6. doi: 10.1002/aur.1386. DOI: https://doi.org/10.1002/aur.1386. [DOI] [PubMed] [Google Scholar]
- 19.Maskey M, Warnell F, Parr JR, Le Couteur A, McConachie H. Emotional and behavioural problems in children with autism spectrum disorder. J Autism Dev Disord. 2013 Apr;43(4):851–9. doi: 10.1007/s10803-012-1622-9. DOI: https://doi.org/10.1007/s10803-012-1622-9. [DOI] [PubMed] [Google Scholar]
- 20.McElhanon B, McCracken C, Karpen S, Sharp WG. Gastrointestinal symptoms in autism spectrum disorder: A meta-analysis. Pediatrics. 2014 May;133(5):872–83. doi: 10.1542/peds.2013-3995. DOI: https://doi.org/10.1542/peds.2013-3995. [DOI] [PubMed] [Google Scholar]
- 21.McKeown C, Hisle-Gorman E, Eide M, Gorman GH, Nylund CM. Association of constipation and fecal incontinence with attention-deficit/hyperactivity disorder. Pediatrics. 2013 Nov;132(5):e1210–5. doi: 10.1542/peds.2013-1580. DOI: https://doi.org/10.1542/peds.2013-1580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Johnston BD, Wright JA. Attentional dysfunction in children with encopresis. J Dev Behav Pediatr. 1993 Dec;14(6):381–5. DOI: https://doi.org/10.1097/00004703-199312010-00004. [PubMed] [Google Scholar]
- 23.Peeters B, Noens I, Philips EM, Kuppens S, Benninga MA. Autism spectrum disorders in children with functional defecation disorders. J Pediatr. 2013 Sep;163(3):873–8. doi: 10.1016/j.jpeds.2013.02.028. DOI: https://doi.org/10.1016/j.jpeds.2013.02.028. [DOI] [PubMed] [Google Scholar]
- 24.Chaidez V, Hansen RL, Hertz-Picciotto I. Gastrointestinal problems in children with autism, developmental delays or typical development. J Autism Dev Disord. 2014 May;44(5):1117–27. doi: 10.1007/s10803-013-1973-x. DOI: https://doi.org/10.1007/s10803-013-1973-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nikolov RN, Bearss KE, Lettinga J, et al. Gastrointestinal symptoms in a sample of children with pervasive developmental disorders. J Autism Dev Disord. 2009 Mar;39(3):405–13. doi: 10.1007/s10803-008-0637-8. DOI: https://doi.org/10.1007/s10803-008-0637-8. [DOI] [PubMed] [Google Scholar]
- 26.Borowitz SM, Cox DJ, Sutphen JL. Differences in toileting habits between children with chronic encopresis, asymptomatic siblings, and asymptomatic nonsiblings. J Dev Behav Pediatr. 1999 Jun;20(3):145–9. doi: 10.1097/00004703-199906000-00002. DOI: https://doi.org/10.1097/00004703-199906000-00002. [DOI] [PubMed] [Google Scholar]
- 27.Cox DJ, Ritterband LM, Quillian W, et al. Assessment of behavioral mechanisms maintaining encopresis: Virginia Encopresis-Constipation Apperception Test. J Pediatr Psychol. 2003 Sep;28(6):375–82. doi: 10.1093/jpepsy/jsg027. DOI: https://doi.org/10.1093/jpepsy/jsg027. [DOI] [PubMed] [Google Scholar]
- 28.Dehghani SM, Kulouee N, Honar N, Imanieh MH, Haghighat M, Javaherizadeh H. Clinical manifestations among children with chronic functional constipation. Middle East J Dig Dis. 2015 Jan;7(1):31–5. [PMC free article] [PubMed] [Google Scholar]
- 29.Kammacher Guerreiro M, Bettinville A, Herzog D. Fecal overflow often affects children with chronic constipation that appears after the age of 2 years. Clin Pediatr (Phila) 2014 Aug;53(9):885–9. doi: 10.1177/0009922814535659. DOI: https://doi.org/10.1177/0009922814535659. [DOI] [PubMed] [Google Scholar]
- 30.Brazzelli M, Griffiths PV, Cody JD, Tappin D. Behavioural and cognitive interventions with or without other treatments for the management of faecal incontinence in children. Cochrane Database Syst Rev. 2011 Dec 7;(12):CD002240. doi: 10.1002/14651858.CD002240.pub4. DOI: https://doi.org/10.1002/14651858.cd002240.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Levine MD, Bakow H. Children with encopresis: A study of treatment outcome. Pediatrics. 1976 Dec;58(6):845–52. [PubMed] [Google Scholar]
- 32.Stark LJ, Owens-Stively J, Spirito A, Lewis A, Guevremont D. Group behavioral treatment of retentive encopresis. J Pediatr Psychol. 1990 Oct;15(5):659–71. doi: 10.1093/jpepsy/15.5.659. DOI: https://doi.org/10.1093/jpepsy/15.5.659. [DOI] [PubMed] [Google Scholar]
- 33.Houts AC, Mellon MW, Whelan JP. Use of dietary fiber and stimulus control to treat retentive encopresis: A multiple-baseline investigation. J Pediatr Psychol. 1988 Sep;13(3):435–45. doi: 10.1093/jpepsy/13.3.435. DOI: https://doi.org/10.1093/jpepsy/13.3.435. [DOI] [PubMed] [Google Scholar]
- 34.Bettany-Saltikov J. How to do a systematic literature review in nursing: A step-by-step guide. Maidenhead, Berkshire, England: Open University Press/McGraw-Hill Education; 2012. [Google Scholar]
- 35.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. PLoS Med. 2009 Jul 21;6(7):e1000100. doi: 10.1371/journal.pmed.1000100. DOI: https://doi.org/10.1371/journal.pmed.1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Moher D, Liberati A, Tetzlaff J, Altman DG PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009 Jul 21;6(7):e1000097. doi: 10.1371/journal.pmed.1000097. DOI: https://doi.org/10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Graneheim UH, Lundman B. Qualitative content analysis in nursing research: Concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today. 2004 Feb;24(2):105–12. doi: 10.1016/j.nedt.2003.10.001. DOI: https://doi.org/10.1016/j.nedt.2003.10.001. [DOI] [PubMed] [Google Scholar]
- 38.Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005 Nov;15(9):1277–88. doi: 10.1177/1049732305276687. DOI: https://doi.org/10.1177/1049732305276687. [DOI] [PubMed] [Google Scholar]
- 39.The Joanna Briggs Institute. New JBI levels of evidence [Internet] Adelaide, South Australia, Australia: The University of Australia; p. 2014. [cited 2016 Jul 13]. Available from: http://joannabriggs.org/assets/docs/approach/JBI-Levels-of-evidence_2014.pdf. [Google Scholar]
- 40.Berg I, Forsythe I, Holt P, Watts J. A controlled trial of “Senokot” in faecal soiling treated by behavioural methods. J Child Psychol Psychiatry. 1983 Oct;24(4):543–9. doi: 10.1111/j.1469-7610.1983.tb00131.x. DOI: https://doi.org/10.1111/j.1469-7610.1983.tb00131.x. [DOI] [PubMed] [Google Scholar]
- 41.Borowitz SM, Cox DJ, Sutphen JL, Kovatchev B. Treatment of childhood encopresis: A randomized trial comparing three treatment protocols. J Pediatr Gastroenterol Nutr. 2002 Apr;34(4):378–84. doi: 10.1097/00005176-200204000-00012. DOI: https://doi.org/10.1097/00005176-200204000-00012. [DOI] [PubMed] [Google Scholar]
- 42.Cox DJ, Sutphen J, Borowitz S, Kovatchev B, Ling W. Contribution of behavior therapy and biofeedback to laxative therapy in the treatment of pediatric encopresis. Ann Behav Med. 1998 Spring;20(2):70–6. doi: 10.1007/BF02884451. DOI: https://doi.org/10.1007/bf02884451. [DOI] [PubMed] [Google Scholar]
- 43.Keshtgar AS, Ward HC, Clayden GS, Sanei A. Role of anal dilatation in treatment of idiopathic constipation in children: Long-term follow-up of a double-blind randomized controlled study. Pediatr Surg Int. 2005 Feb;21(2):100–5. doi: 10.1007/s00383-004-1336-y. DOI: https://doi.org/10.1007/s00383-004-1336-y. [DOI] [PubMed] [Google Scholar]
- 44.Nolan T, Debelle G, Oberklaid F, Coffey C. Randomised trial of laxatives in treatment of childhood encopresis. Lancet. 1991 Aug 31;338(8766):523–7. doi: 10.1016/0140-6736(91)91097-e. DOI: https://doi.org/10.1016/0140-6736(91)91097-e. [DOI] [PubMed] [Google Scholar]
- 45.Sprague-McRae JM, Lamb W, Homer D. Encopresis: A study of treatment alternatives and historical and behavioral characteristics. Nurse Pract. 1993 Oct;18(10):52–3. 56–63. doi: 10.1097/00006205-199310000-00009. DOI: https://doi.org/10.1097/00006205-199310000-00009. [DOI] [PubMed] [Google Scholar]
- 46.van Dijk M, Bongers ME, de Vries GJ, Grootenhuis MA, Last BF, Benninga MA. Behavioral therapy for childhood constipation: A randomized, controlled trial. Pediatrics. 2008 May;121(5):e1334–41. doi: 10.1542/peds.2007-2402. DOI: https://doi.org/10.1542/peds.2007-2402. [DOI] [PubMed] [Google Scholar]
- 47.Amendola S, De Angelis P, Dall’oglio L, Di Abriola GF, Di Lorenzo M. Combined approach to functional constipation in children. J Pediatr Surg. 2003 May;38(5):819–23. doi: 10.1016/jpsu.2003.50174. DOI: https://doi.org/10.1016/jpsu.2003.50174. [DOI] [PubMed] [Google Scholar]
- 48.Anthony EJ. An experimental approach to the psychopathology of childhood: Encopresis. Br J Med Psychol. 1957 Sep 6;30(3):146–75. doi: 10.1111/j.2044-8341.1957.tb01194.x. DOI: https://doi.org/10.1111/j.2044-8341.1957.tb01194.x. [DOI] [PubMed] [Google Scholar]
- 49.Firestone Baum C, John A, Srinivasan K, et al. Colon manometry proves that perception of the urge to defecate is present in children with functional constipation who deny sensation. J Pediatr Gastroenterol Nutr. 2013 Jan;56(1):19–22. doi: 10.1097/MPG.0b013e31826f2740. DOI: https://doi.org/10.1097/mpg.0b013e31826f2740. [DOI] [PubMed] [Google Scholar]
- 50.Ismail N, Ratchford I, Proudfoot C, Gibbs J. Impact of a nurse-led clinic for chronic constipation in children. J Child Health Care. 2011 Sep;15(3):221–9. doi: 10.1177/1367493511406568. DOI: https://doi.org/10.1177/1367493511406568. [DOI] [PubMed] [Google Scholar]
- 51.Landman GB, Levine MD, Rappaport L. A study of treatment resistance among children referred for encopresis. Clin Pediatr (Phila) 1984 Aug;23(8):449–52. doi: 10.1177/000992288402300808. DOI: https://doi.org/10.1177/000992288402300808. [DOI] [PubMed] [Google Scholar]
- 52.Luxem MC, Christophersen ER, Purvis PC, Baer DM. Behavioral-medical treatment of pediatric toileting refusal. J Dev Behav Pediatr. 1997 Feb;18(1):34–41. doi: 10.1097/00004703-199702000-00007. DOI: https://doi.org/10.1097/00004703-199702000-00007. [DOI] [PubMed] [Google Scholar]
- 53.Misra S, Lee A, Gensel K. Chronic constipation in overweight children. JPEN J Parenter Enteral Nutr. 2006 Mar-Apr;30(2):81–4. doi: 10.1177/014860710603000281. DOI: https://doi.org/10.1177/014860710603000281. [DOI] [PubMed] [Google Scholar]
- 54.Poenaru D, Roblin N, Bird M, et al. The Pediatric Bowel Management Clinic: Initial results of a multidisciplinary approach to functional constipation in children. J Pediatr Surg. 1997 Jun;32(6):843–8. doi: 10.1016/s0022-3468(97)90633-3. DOI: https://doi.org/10.1016/s0022-3468(97)90633-3. [DOI] [PubMed] [Google Scholar]
- 55.Taubman B. Toilet training and toileting refusal for stool only: A prospective study. Pediatrics. 1997 Jan;99(1):54–8. doi: 10.1542/peds.99.1.54. DOI: https://doi.org/10.1542/peds.99.1.54. [DOI] [PubMed] [Google Scholar]
- 56.Taubman B, Blum NJ, Nemeth N. Children who hide while defecating before they have completed toilet training: A prospective study. Arch Pediatr Adolesc Med. 2003 Dec;157(12):1190–2. doi: 10.1001/archpedi.157.12.1190. DOI: https://doi.org/10.1001/archpedi.157.12.1190. [DOI] [PubMed] [Google Scholar]
- 57.Taubman B, Buzby M. Overflow encopresis and stool toileting refusal during toilet training: A prospective study on the effect of therapeutic efficacy. J Pediatr. 1997 Nov;131(5):768–71. doi: 10.1016/s0022-3476(97)70112-4. DOI: https://doi.org/10.1016/s0022-3476(97)70112-4. [DOI] [PubMed] [Google Scholar]
- 58.Turner-Bowker DM, Lindner E, Mareya S, et al. Development and content validity of a pediatric functional constipation daily diary. Value Health. 2015 May;18(3):A28. DOI: https://doi.org/10.1016/j.jval.2015.03.169. [Google Scholar]
- 59.Beaudry IB, Schaaf RC, Polo ER. Occupational therapy based on Ayres Sensory Integration in the treatment of retentive fecal incontinence in a 3-year-old boy. Am J Occup Ther. 2013 Sep-Oct;67(5):601–6. doi: 10.5014/ajot.2013.008086. DOI: https://doi.org/10.5014/ajot.2013.008086. [DOI] [PubMed] [Google Scholar]
- 60.Bellman M. Studies on encopresis. Acta Paediatr Scand. 1966;(Suppl 170):121–32. [PubMed] [Google Scholar]
- 61.Benninga MA, Büller HA, Heymans HS, Tytgat GN, Taminiau JA. Is encopresis always the result of constipation? Arch Dis Child. 1994 Sep;71(3):186–93. doi: 10.1136/adc.71.3.186. DOI: https://doi.org/10.1136/adc.71.3.186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Chang SH, Park KY, Kang SK, et al. Prevalence, clinical characteristics, and management of functional constipation at pediatric gastroenterology clinics. J Korean Med Sci. 2013 Sep;28(9):1356–61. doi: 10.3346/jkms.2013.28.9.1356. DOI: https://doi.org/10.3346/jkms.2013.28.9.1356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Clément C. [Toilet training and psychological dyschezia: Behavioral therapy in young children]. Journal de Thérapie Comportementale et Cognitive. 2014 Jun;24(2):47–52. [Article in French] DOI: https://doi.org/10.1016/j.jtcc.2014.04.001. [Google Scholar]
- 64.Corday RJ. Toilet training and “the terrible two’s.” Comments on the prevention and management of behavior problems at this age. Clin Pediatr (Phila) 1967 Jan;6(1):41–6. doi: 10.1177/000992286700600112. DOI: https://doi.org/10.1177/000992286700600112. [DOI] [PubMed] [Google Scholar]
- 65.Dalrymple NJ, Ruble LA. Toilet training and behaviors of people with autism: Parent views. J Autism Dev Disord. 1992 Jun;22(2):265–75. doi: 10.1007/BF01058155. DOI: https://doi.org/10.1007/bf01058155. [DOI] [PubMed] [Google Scholar]
- 66.Feinberg L, Mahajan L, Steffen R. The constipated child: Is there a correlation between symptoms and manometric findings? J Pediatr Gastroenterol Nutr. 2008 Nov;47(5):607–11. doi: 10.1097/mpg.0b013e3181684c94. DOI: https://doi.org/10.1097/mpg.0b013e3181684c94. [DOI] [PubMed] [Google Scholar]
- 67.Inan M, Aydiner CY, Tokuc B, et al. Factors associated with childhood constipation. J Paediatr Child Health. 2007 Oct;43(10):700–6. doi: 10.1111/j.1440-1754.2007.01165.x. DOI: https://doi.org/10.1111/j.1440-1754.2007.01165.x. [DOI] [PubMed] [Google Scholar]
- 68.Khanna V, Poddar U, Yachha SK. Etiology and clinical spectrum of constipation in Indian children. Indian Pediatr. 2010 Dec;47(12):1025–30. doi: 10.1007/s13312-010-0175-2. DOI: https://doi.org/10.1007/s13312-010-0175-2. [DOI] [PubMed] [Google Scholar]
- 69.Kocaay P, Eğrıtaş O, Dalgiç B. Normal defecation pattern, frequency of constipation and factors related to constipation in Turkish children 0–6 years old. Turk J Gastroenterol. 2011 Aug;22(4):369–75. doi: 10.4318/tjg.2011.0238. DOI: https://doi.org/10.4318/tjg.2011.0238. [DOI] [PubMed] [Google Scholar]
- 70.Malowitz S, Green M, Karpinski A, Rosenberg A, Hyman PE. Age of onset of functional constipation. J Pediatr Gastroenterol Nutr. 2016 Apr;62(4):600–2. doi: 10.1097/MPG.0000000000001011. DOI: https://doi.org/10.1097/mpg.0000000000001011. [DOI] [PubMed] [Google Scholar]
- 71.Niemczyk J, Equit M, El Khatib D, von Gontard A. Toilet refusal syndrome in preschool children: Do different subtypes exist? J Pediatr Gastroenterol Nutr. 2014 Mar;58(3):303–6. doi: 10.1097/MPG.0000000000000204. DOI: https://doi.org/10.1097/mpg.0000000000000204. [DOI] [PubMed] [Google Scholar]
- 72.Olness K. Autohypnosis in functional megacolon in children. Am J Clin Hypn. 1976 Jul;19(1):28–32. doi: 10.1080/00029157.1976.10403828. DOI: https://doi.org/10.1080/00029157.1976.10403828. [DOI] [PubMed] [Google Scholar]
- 73.Papenfus HA. Encopresis in the school aged child. J Sch Nurs. 1998 Feb;14(1):26–31. [PubMed] [Google Scholar]
- 74.Partin JC, Hamill SK, Fischel JE, Partin JS. Painful defecation and fecal soiling in children. Pediatrics. 1992 Jun;89(6 Pt 1):1007–9. [PubMed] [Google Scholar]
- 75.Phillips GT, Smith JE. The behavioural treatment of faeces retention: An expanded case study. Behav Cogn Psychother. 1986 Apr;14(2):124–36. DOI: https://doi.org/10.1017/s0141347300014555. [Google Scholar]
- 76.Radford J, Anderson M. Encopresis in children on the autistic spectrum. Early Child Development and Care. 2003;173(4):375–82. DOI: https://doi.org/10.1080/0300443032000079069. [Google Scholar]
- 77.Rajindrajith S, Devanarayana NM, Benninga MA. Determinants of healthcare consultation behavior in children with chronic constipation: A school based survey [abstract]. Proceedings of the Fifth European Paediatric Motility Meeting. J Pediatr Gastroenterol Nutr. 2011 Dec;53(Suppl 2):S82–3. DOI: https://doi.org/10.1097/MPG.0b013e31823cadc6. [Google Scholar]
- 78.Rajindrajith S, Devanarayana NM, Benninga MA. Constipation and constipation-predominant irritable bowel syndrome: A comparative study using Rome III criteria. J Pediatr Gastroenterol Nutr. 2017 May;64(5):679–84. doi: 10.1097/MPG.0000000000001332. DOI: https://doi.org/10.1097/MPG.0000000000001332. [DOI] [PubMed] [Google Scholar]
- 79.Rugolotto S, Sun M, Boucke L, Calò DG, Tatò L. Toilet training started during the first year of life: A report on elimination signals, stool toileting refusal and completion age. Minerva Pediatr. 2008 Feb;60(1):27–35. [PubMed] [Google Scholar]
- 80.Schonwald A, Sherritt L, Stadtler A, Bridgemohan C. Factors associated with difficult toilet training. Pediatrics. 2004 Jun;113(6):1753–7. doi: 10.1542/peds.113.6.1753. DOI: https://doi.org/10.1542/peds.113.6.1753. [DOI] [PubMed] [Google Scholar]
- 81.Segall A. Report of a constipated child with fecal withholding. Am J Orthopsychiatry. 1957 Oct;27(4):823–9. doi: 10.1111/j.1939-0025.1957.tb05549.x. DOI: https://doi.org/10.1111/j.1939-0025.1957.tb05549.x. [DOI] [PubMed] [Google Scholar]
- 82.Silverman AH, Mugie SM, Di Lorenzo C, et al. Current presentation and management of childhood constipation [abstract]. Proceedings of Digestive Disease Week 2013. Gastroenterology. 2013 May;144(5 Suppl 1):S397. DOI: https://doi.org/10.1016/S0016-5085(13)61462-6. [Google Scholar]
- 83.Smith L, Smith P, Lee SK. Behavioural treatment of urinary incontinence and encopresis in children with learning disabilities: Transfer of stimulus control. Dev Med Child Neurol. 2000 Apr;42(4):276–9. doi: 10.1017/s0012162200000475. DOI: https://doi.org/10.1111/j.1469-8749.2000.tb00085.x. [DOI] [PubMed] [Google Scholar]
- 84.Stadtler AC, Burke P. A group treatment approach to failure to toilet train: The case of Max. Clin Excell Nurse Pract. 1998 Mar;2(2):83–7. [PubMed] [Google Scholar]
- 85.Velasco-Benitez CA, Orsagh-Yentis D, Koppen IJ, Di Lorenzo C, Saps M. First multicity study on the prevalence of functional constipation in Latin American children 2–4 years of age [abstract]. Proceedings of Digestive Disease Week 2016. Gastroenterology. 2016 Apr;150(4 Suppl 1):S935. DOI: https://doi.org/10.1016/s0016-5085(16)33166-3. [Google Scholar]
- 86.von Gontard A, Niemczyk J, Thomé-Granz S, Nowack J, Moritz AM, Equit M. Incontinence and parent-reported oppositional defiant disorder symptoms in young children—a population-based study. Pediatr Nephrol. 2015 Jul;30(7):1147–55. doi: 10.1007/s00467-014-3040-z. DOI: https://doi.org/10.1007/s00467-014-3040-z. [DOI] [PubMed] [Google Scholar]
- 87.Warson SR, Caldwell MR, Warinner A, Kirk AJ, Jenson RA. The dynamics of encopresis. Am J Orthopsychiatry. 1954 Apr;24(2):402–15. doi: 10.1111/j.1939-0025.1954.tb02028.x. DOI: https://doi.org/10.1111/j.1939-0025.1954.tb02028.x. [DOI] [PubMed] [Google Scholar]
- 88.Wells J. Adult agendas and children’s experience—a response to secondary victimization. Child Abuse Rev. 1992 Apr;1(1):52–5. DOI: https://doi.org/10.1002/car.2380010109. [Google Scholar]
- 89.West AF, Steinhardt K. Containing anxiety in the management of constipation. Arch Dis Child. 2003 Dec;88(12):1038–9. doi: 10.1136/adc.88.12.1038. DOI: https://doi.org/10.1136/adc.88.12.1038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Yong D, Beattie RM. Normal bowel habit and prevalence of constipation in primary-school children. Ambulatory Child Health. 1998;4(3):277–82. [Google Scholar]
- 91.Böige N, Missonnier S, Bellaïche M, Foucaud P. [Psychosomatic approach to encopresis]. Archives de Pédiatrie. 1999 Dec;6(12):1331–7. doi: 10.1016/s0929-693x(00)88898-3. [Article in French] DOI: https://doi.org/10.1016/s0929-693x(00)88898-3. [DOI] [PubMed] [Google Scholar]
- 92.Christophersen ER. Toileting problems in children. Pediatr Ann. 1991 May;20(5):240–4. doi: 10.3928/0090-4481-19910501-07. DOI: https://doi.org/10.3928/0090-4481-19910501-07. [DOI] [PubMed] [Google Scholar]
- 93.Day AS. Constipation in infants and children. Med Today. 2003 Jan;4(1):24–31. [Google Scholar]
- 94.Dowling T, Nightingale S. Constipation in infants and children. Med Today. 2013 Jul;14(7):71–3. [Google Scholar]
- 95.Fleisher DR. Understanding toilet training difficulties. Pediatrics. 2004 Jun;113(6):1809–10. doi: 10.1542/peds.113.6.1809. DOI: https://doi.org/10.1542/peds.113.6.1809. [DOI] [PubMed] [Google Scholar]
- 96.Griffin GC, Roberts SD, Graham G. How to resolve stool retention in a child. Underwear soiling is not a behavior problem. Postgrad Med. 1999 Jan;105(1):159–61. 165–6, 172–3. doi: 10.3810/pgm.1999.01.506. DOI: https://doi.org/10.3810/pgm.1999.01.506. [DOI] [PubMed] [Google Scholar]
- 97.Jacob H, Grodzinski B, Fertleman C. Fifteen-minute consultation: Problems in the healthy child-toilet training. Arch Dis Child Educ Pract Ed. 2016 Jun;101(3):119–23. doi: 10.1136/archdischild-2015-308973. DOI: https://doi.org/10.1136/archdischild-2015-308973. [DOI] [PubMed] [Google Scholar]
- 98.Kuhn BR, Marcus BA, Pitner SL. Treatment guidelines for primary nonretentive encopresis and stool toileting refusal. Am Fam Physician. 1999 Apr 15;59(8):2171–8. 2184–6. [PubMed] [Google Scholar]
- 99.Loening-Baucke V. Toilet tales: Stool toileting refusal, encopresis, and fecal incontinence. J Wound Ostomy Continence Nurs. 1998 Nov;25(6):304–13. doi: 10.1016/s1071-5754(98)90028-6. DOI: https://doi.org/10.1097/00152192-199811000-00008. [DOI] [PubMed] [Google Scholar]
- 100.Shaikh N. Time to get on the potty: Are constipation and stool toileting refusal causing delayed toilet training? J Pediatr. 2004 Jul;145(1):12–3. doi: 10.1016/j.jpeds.2004.04.037. DOI: https://doi.org/10.1016/j.jpeds.2004.04.037. [DOI] [PubMed] [Google Scholar]
- 101.Behavior [Internet] Springfield, MA: Merriam-Webster Inc; c2017. [cited 2016 Oct 17]. Available from: www.merriam-webster.com/dictionary/behavior. [Google Scholar]