Abstract
Background
Describing the morphologic features of the thoracic pedicle in patients with adolescent idiopathic scoliosis is necessary for placement of pedicle screws. Previous studies showed inadequate reliability owing to small sample size and heterogeneity of the patients surveyed.
Questions/Purposes
To use CT scans (1) to describe the morphologic features of 2718 thoracic pedicles from 60 female patients with Lenke Type 1 adolescent idiopathic scoliosis and 60 age-, sex-, and height-matched controls; and (2) to classify the pedicles in three types based on pedicle width and analyze the distribution of each type.
Methods
A total of 2718 pedicles from 60 female patients with Lenke Type 1 adolescent idiopathic scoliosis and 60 matched female controls were analyzed via CT. All patients surveyed were diagnosed with adolescent idiopathic scoliosis, Lenke Type 1, at the First Affiliated Hospital of Sun Yat-sen University, and all underwent pedicle screw fixation between January 2008 and December 2013 with preoperative radiographs and CT images on file. We routinely obtained CT scans before these procedures; all patients who underwent surgery during that period had CT scans, and all were available for analysis here. Control subjects had CT scans for other clinical indications and had no abnormal findings of the spine. The control subjects were chosen to match patients in terms of age (15 ± 2.6 years versus 15 ± 2.6 years) and sex. Height of the two groups also was matched (154 ± 9 cm versus 155 ± 10 cm; mean difference, −1.06 cm; 95% CI, −1.24 to −0.81 cm; p < 0.001). Pedicle width and length were measured from T1 to T12. The thoracic spine was classified in four regions: apical vertebra in the structural curve (AV-SC), nonapical vertebra in the structural curve (NAV-SC), apical vertebra in the nonstructural curve (AV-NSC), and nonapical vertebra in the nonstructural curve (NAV-NSC). Pedicles were classified in three types: pedicle width less than 2 mm as Type I, 2 mm to 4 mm as Type II, and greater than 4 mm as Type III. Types I and II were defined as dysplastic pedicles. Paired t test, independent samples t test, one-way ANOVA, followed by Bonferroni’s post hoc test and chi-square or Fisher’s exact tests were used for statistical comparisons between patients and controls, as appropriate.
Results
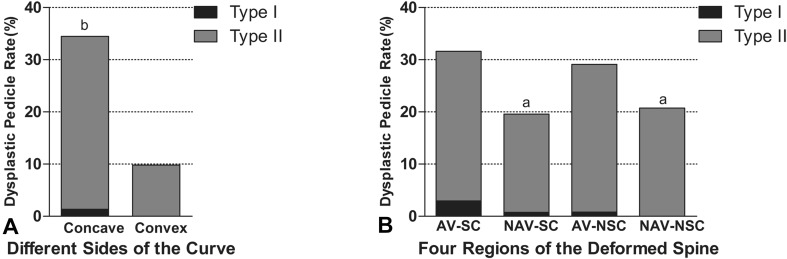
No difference was found between pedicle width on the convex side (PWv) and in controls (PWn), but pedicle width on the concave side (PWc) (4.99 ± 1.87 mm) was found to be narrower than PWv (6 ± 1.66 mm) and PWn (6 ± 1.45 mm). The variation degree of pedicle width (VDPW) was greatest in the AV-SC region (34% ± 37%), in comparison to AV-NSC (20% ± 25%) (mean difference, 14%; 95% CI, 1.15%–27%; p = 0.025), NAV-SC (17% ± 30%) (mean difference, 17%; 95% CI, 7%–27%; p < 0.001), and NAV-NSC (11% ± 24%) (mean difference, 24%; 95% CI, 13%–34%; p < 0.001). Dysplastic pedicles appeared more in patients with adolescent idiopathic scoliosis (22%; 293 of 1322) compared with controls (13%; 178 of 1396) (odds ratio [OR] = 0.51; 95% CI, 0.42–0.63; p < 0.001). In patients with adolescent idiopathic scoliosis, they commonly occurred on the concave side 34% (228 of 661) and on the AV-SC region (32%; 43 of 136).
Conclusions
Pedicle width on the concave side was narrower than pedicle width on the convex side and pedicle width in healthy control subjects. The apical vertebra in the structural curve was the most variegated region of the curve with the highest prevalence of dysplastic pedicles.
Clinical Relevance
Our study can help surgeons perform preoperative assessments in females with adolescent idiopathic scoliosis, and with preoperative and intraoperative management for difficult pedicle screw placement. In particular, our results suggest that surgeons should exercise increased vigilance when selecting pedicle screw dimensions, especially in the concave aspect of the mid-thoracic curve, to avoid cortical breeches. Future studies should evaluate other Lenke types of adolescent idiopathic scoliosis, and males with adolescent idiopathic scoliosis.
Introduction
Adolescent idiopathic scoliosis is the most-common spinal deformity, which affects 1% to 3% of children 10 to 16 years old [13, 21]. It is a complex, three-dimensional deformity of the spine with lateral deviation in the coronal plane, alternation of the kyphosis or lordosis in the sagittal plane, and rotation of the vertebrae in the axial plane. Lenke et al. [17] presented a widely accepted system for classification of adolescent idiopathic scoliosis that helps in defining the vertebrae to be included in an arthrodesis preoperatively, and they highlighted the distinction of structural and nonstructural curves. Among the six Lenke types of scoliosis, Type 1 is the most common, the curve of which is located mainly in the thoracic spine [17]. Transpedicle screw fixation is the mainstay of surgery for adolescent idiopathic scoliosis, allows for segmental instrumentation in multiple vertebrae across a multilevel fusion area, and provides strong pullout strength and desired deformity correction [8, 16, 18, 19]. Despite its advantages, it remains controversial when used in the thoracic levels owing to the relatively small pedicle dimensions and wide variation in morphologic features of the pedicles [6, 32]. Screw misplacement may reduce pullout strength or lead to severe complications involving the nearby visceral, vascular, and neurologic structures [5, 10, 23, 26]. Numerous anatomic studies regarding the unique characteristics of thoracic pedicles have been conducted, however, some of these studies involved adults [33, 34], and a couple focused on morphologic features of the thoracic pedicle in the immature spine [28, 37]. In addition, controversy persists because some studies involve small sample sizes and heterogeneous populations [28, 29]. Thus, the safety and feasibility of using pedicle screws in the immature spine remain questionable, and morphologic data in an adolescent population are needed to build a complete database for the thoracic pedicle in the immature spine. Krag et al. [14] and Misenhimer et al. [24] reported good correlation between CT-based and true morphometric measurements of pedicles in cadavers. Gstoettner et al. [7] found substantial intra- and interobserver reliability of CT scans. However, to the best of our knowledge, numerous studies investigating morphologic features of the pedicle only focused on comparison between the concave and convex sides of scoliosis, which provides limited information regarding the deformed spine [2–4, 11, 15, 31, 35]. Thus, we conducted a morphologic study of the thoracic pedicle in 60 female patients with Lenke Type 1 adolescent idiopathic scoliosis using CT scans, and 60 age-, sex-, and height-matched controls were included. The thoracic spine was subdivided in four regions, which would allow for investigation of segmental differences in the thoracic spine, with the ability to discern and isolate important differences.
The aim of our study was to quantify the important diameters and provide a thorough description of the variations of the thoracic pedicle in a homogeneous cohort. Specifically, we attempted, using CT scans (1) to describe the morphologic features of 2718 thoracic pedicles from 60 female patients with Lenke Type 1 adolescent idiopathic scoliosis and 60 age-, sex-, and height-matched controls, and (2) to classify the pedicles in three types based on pedicle width to help surgeons plan for difficult screw placement.
Patients and Methods
Patient Demographic Data
This study involved 60 female patients with adolescent idiopathic scoliosis classified as Lenke Type 1 according to the Lenke classification. The patients were recruited from the First Affiliated Hospital of Sun Yat-sen University and all underwent pedicle screw fixation between January 2008 and December 2013. We only included female subjects in the adolescent idiopathic scoliosis and control groups to guarantee homogeneity and size of samples at the same time. Criteria for patient selection were: (1) all patients with adolescent idiopathic scoliosis who were carefully screened to ensure that their scoliosis was idiopathic and classified as Lenke Type 1; and (2) preoperative radiographs and CT images were available on file. Exclusion criteria were: (1) proven or even suspected congenital, muscular, neurologic, or hormonal causes of scoliosis; and (2) clinical history of any condition that may have affected vertebral growth (eg, history of cancer, vertebral abnormalities, muscular abnormalities, or neurologic conditions). We routinely obtained CT scans before these procedures; all patients who underwent surgery during that period had CT scans, and all were available for analysis here. Applying these criteria, there were 60 female patients with a mean age of 15 ± 2.6 years (range, 12–18 years), classified as having Lenke Type 1 adolescent idiopathic scoliosis. The mean Cobb angle of the main curve was 53° ± 13° (range, 40°–96°), and the mean height of the patients with adolescent idiopathic scoliosis was 154 cm ± 9 cm.
Criteria for control selection were: (1) sex, age- and height- matched subjects; and (2) had clinical indications for CT (such as pneumonia) but no abnormal findings of the skeletal system on CT as assessed by a radiologist. Radiographs and family history also were used to exclude the possibility of adolescent idiopathic scoliosis. In the control group, 60 age- and height-matched female subjects were included (Table 1). We did not collect weight information of the studied subjects, therefore BMI data are unavailable.
Table 1.
Demographic data of the patients and control subjects
| Demographic | Patients with adolescent idiopathic scoliosis | Control subjects | p Value |
|---|---|---|---|
| Age (years) | 15 ± 2.6; range, 12–18 | 15 ± 2.6; range, 12–18 | p < 0.001 |
| Height (cm) | 154 ± 9 | 155 ± 10 | p < 0.001 |
| Cobb’s angle (°) | 53 ± 13; range, 40–96 | Not available | – |
| Number of pedicles | 1322 | 1396 | – |
A total of 1322 pedicles from the patients with adolescent idiopathic scoliosis and 1396 pedicles from the controls were evaluated.
Ethical Statement
The medical ethical committee for clinical research and animal trials of the First Affiliated Hospital of Sun Yat-sen University approved the design and performance for this investigation.
Vertebrae Classification in Patients with Adolescent Idiopathic Scoliosis
Standard whole-spine radiographs in AP, lateral, and bending position views were used. Cobb angle was measured, and according to the Lenke classification, the thoracic vertebrae of the patients were classified in four regions: apical vertebra in the structural curve (AV-SC), nonapical vertebra in the structural curve (NAV-SC), apical vertebra in the nonstructural curve (AV-NSC), and nonapical vertebra in the nonstructural curve (NAV-NSC) (Table 2). Apical vertebra is defined as the vertebra farthest from the center sacral vertical line. If the intervertebral disc was located in the farthest position, we collected the data from the upper and lower vertebrae at the same time, which brings two apical vertebrae in one apical region.
Table 2.
Abbreviations and descriptions
| Abbreviations | Description |
|---|---|
| PW | Pedicle width |
| PWc | Pedicle width on the concave side |
| PWv | Pedicle width on the convex side |
| PWn | Pedicle width in normal controls |
| PL | Pedicle length |
| PLc | Pedicle length on the concave side |
| PLv | Pedicle length on the convex side |
| PLn | Pedicle length in normal controls |
| AV-SC | Apical vertebra in the structural curve |
| NAV-SC | Nonapical vertebra in the structural curve |
| AV-NSC | Apical vertebra in the nonstructural curve |
| NAV-NSC | Nonapical vertebra in the nonstructural curve |
| VDPW | Variation degree of pedicle width |
| VDPL | Variation degree of pedicle length |
Measurement of Morphologic Features of the Pedicle
A total of 1322 pedicles in patients with adolescent idiopathic scoliosis and 1396 in controls were measured from T1 to T12 vertebrae by three orthopaedic surgeons (BG, WG, CC). Three patients (total of 72 pedicles) and three controls (total of 72 pedicles) then were selected at random and the 144 pedicles were measured three times by three different observers (BG, WG, CC) to calculate interobserver reliability and by one observer (BG) two times to calculate intraobserver reliability. The CT scans were performed on a 64-slice scanner for each subject, at 120 kV, less than 200 mA, with a slice thickness of 0.5 mm, and with a resultant average radiation burden less than 10 mGy (Toshiba Aquilion® 64-slice; Toshiba Medical Systems Corporation, Otawara-shi, Japan). All images were measured and analyzed by picture archiving and communication systems (PACS; Anke High-tech Co, Ltd, Shenzhen, China). CT slices in the axial plane were obtained using multidetector scanning without angulation of the gantry. The images in both groups (adolescent idiopathic scoliosis and control subjects) were reformatted on a workstation with appropriate angulation so that the pedicles could be seen in-plane without distortion. Pedicle diameter was measured on axial slices through the thinnest portion of the pedicle using reformatted slices closest to the middle of the pedicle in the craniocaudad dimension. The parameters measured in the current study for each subject included pedicle width and pedicle length. The measurement method is described below [29, 36]. The guideline was defined as the straight-line perpendicular to the axis of the vertebra that passed through the anterior tip of the vertebral canal. Pedicle length was defined as the distance along the line through the axis of the pedicle from its intersection with the guideline to its intersection with the line through the axis of the lamina. Pedicle width was defined as the shortest distance along the perpendicular to the line through the axis of the pedicle (Fig. 1). For patients with adolescent idiopathic scoliosis, pedicle width on the convex side is provided as PWv and on the concave side as PWc. In controls, pedicle width is given as PWn. In the same way, pedicle length on the convex side is provided as PLv and on the concave side as PLc. Pedicle length in the controls is cited as PLn. Based on pedicle width, the pedicles were classified as three types: pedicle width less than 2 mm as Type I, 2 mm to 4 mm as Type II, and greater than 4 mm as Type III. Types I and II were defined as dysplastic pedicles [31]. To evaluate the unbalanced development of the deformed pedicles between the convex and concave sides in patients with adolescent idiopathic scoliosis, variation degree of pedicle width (VDPW) and variation degree of pedicle length (VDPL) were calculated as follows: VDPW (%) = Σ[(PWv − PWc)/{(PWv + PWc)/2}]/number of vertebrae involved in the region × 100%; VDPL (%)= Σ[(PLv − PLc)/{(PLv + PLc)/2}]/number of vertebrae involved in the region × 100%.
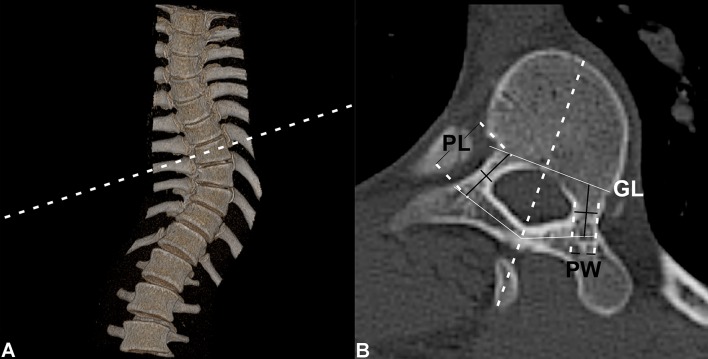
Fig. 1A–B.
Measurement parameters are presented in these illustrations. (A) The dashed line represents the appropriate angulation on a reformatted workstation for obtaining the transverse CT image for each vertebra displaying both pedicles. (B) The dashed line represents the axis of the vertebra; the guideline was defined as the straight-line perpendicular to the axis of the vertebra that passed through the anterior tip of the vertebral canal. Pedicle length was defined as the distance along the line through the axis of the pedicle from its intersection with the guide line to its intersection with the line through the axis of the lamina. Pedicle width was defined as the shortest distance along the perpendicular to the line through the axis of the pedicle. Pedicle length and pedicle width were recorded bilaterally. PL = pedicle length; PW = pedicle width; GL = guideline.
Statistical Analysis
Comparison of the convex and concave sides of the spines of patients with adolescent idiopathic scoliosis was performed using a paired t-test. The independent samples t test was conducted to compare the parameters between patients with adolescent idiopathic scoliosis and controls. Parameters among the four different regions in the patients were compared using one-way ANOVA followed by Bonferroni’s post hoc test. Comparison of the prevalence and distribution of the dysplastic pedicles was performed using chi-square or Fisher’s exact tests when appropriate. Statistical analyses were conducted using SPSS Version 20.0 (IBM Corporation, Armonk, NY, USA). A two-sided probability less than 0.05 was considered statistically significant. Interobserver reliability was evaluated using interclass correlation coefficients (ICC). A Bland-Altman assessment for agreement was used to compare the intraobserver reliability. A range of agreement was defined as mean bias ± 2 SD.
Intra- and Interobserver Reliability
Pedicle width (ICC = 0.997; p < 0.001) and pedicle length (ICC = 0.995; p < 0.001) showed substantial interobserver reliability. Bland-Altman plots showed minimal biases between two repeated measurements (bias ± SD, 0.02 ± 0.12; 95% CI, −0.22 to 0.26).
Results
Morphology
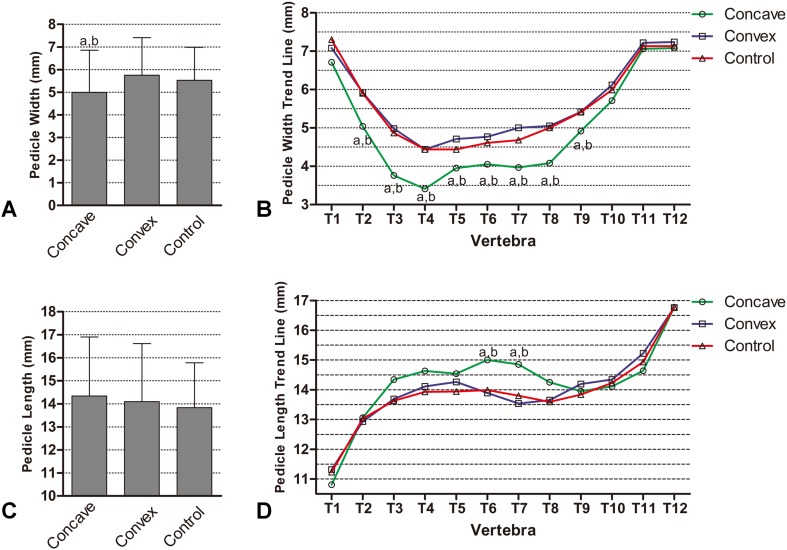
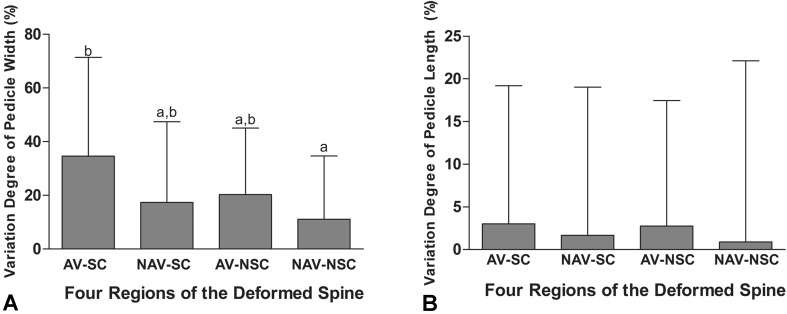
The main differences in morphologic features of the spine between patients with adolescent idiopathic scoliosis and controls were that PWc was narrower than PWv in patients with adolescent idiopathic scoliosis and no difference was found between PWv and PWn. In the patients and the controls, pedicle width showed decreasing dimensions from T1 to T4 followed by increasing dimensions from T5 to T12. The relatively narrow pedicles were located between T3 and T8, and the narrowest was in T4 (PWc 3.41 ± 0.98 mm, PWv 4.44 ± 0.88 mm, and PWn 4.46 ± 0.89 mm, respectively) (Table 3). Overall, no difference was found between PWv (6 ± 1.66 mm) and PWn (6 ± 1.45 mm), and PWc (4.99 ± 1.87 mm) was found to be narrower than PWv (6 ± 1.66 mm) (mean difference, −0.77; 95% CI, −0.94 to −0.59; p < 0.001) and narrower than PWn (6 ± 1.45 mm) (mean difference, −0.54; 95% CI, −0.69 to −0.39; p < 0.001) () (Fig. 2A). Consistently, few differences were found between PWv and PWn in most of the levels (except T5 and T7), and PWc was the narrowest in most of the vertebrae (except T1, T11, and T12) (Fig. 2B) (Table 3). Pedicle length showed increasing dimensions from T1 to T12, and generally there were few differences among PLv (14 ± 2.52 mm), PLn (14 ± 1.95 mm), and PLc (14 ± 2.56 mm) (Fig. 2C). However, in T6 and T7, PLc was found to be the longest among the three groups. Specifically, T6 PLc (15 ± 2.46 mm) was longer than PLv (14 ± 1.90 mm) (mean difference, 1.11; 95% CI, 0.27–1.94; p = 0.005), and T6 PLc (15 ± 2.46 mm) was longer than PLn (14 ± 1.47 mm) (mean difference, 0.99; 95% CI, 0.27–1.71; p = 0.003) (Fig. 2D) (Table 3). For pedicle width, we found that the unbalanced development is most severe in AV-SC. The VDPW in AV-SC (34% ± 37%) was the highest among the four regions. VDPW in AV-SC (34% ± 37%) was higher than in AV-NSC (20% ± 25%) (mean difference, 14%; 95% CI, 1.15%–27%; p = 0.025), NAV-SC (17% ± 30%) (mean difference, 17%; 95% CI, 7%–27%; p < 0.001), and NAV-NSC (11% ± 24%) (mean difference, 24%; 95% CI, 13%–34%; p < 0.001) (Fig. 3A). There was no difference for VDPW in AV-NSC (20% ± 25%) or in NAV-SC (17% ± 30%) (mean difference, 2.99%; 95% CI, −8% to 14%; p = 1.000), and the VDPW in NAV-NSC (11% ± 24%) was the lowest among the four regions. VDPW in NAV-NSC (11% ± 24%) was lower than in AV-SC (34% ± 37%) (mean difference, −24%; 95% CI, −34% to −13%; p < 0.001), AV-NSC (20% ± 25%) (mean difference, −9%; 95% CI, −8% to 14%; p = 0.049), and NAV-SC (17% ± 30%) (mean difference, 17%; 95% CI, 7%–27%; p = 0.019). No difference was found for VDPL among AV-SC (3.01% ± 16%), NAV-SC (1.67% ± 17%), AV-NSC (2.75% ± 15%), and NAV-NSC (0.89% ± 21%) (Fig. 3B).
Table 3.
Pedicle parameters in patients and controls
| Level | PWc (mm) | PWv (mm) | PWn (mm) | PLc (mm) | PLv (mm) | PLn (mm) |
|---|---|---|---|---|---|---|
| T1 | 7 ± 1.25 | 7 ± 1.09 | 7 ± 1.01 | 11 ± 2.34 | 11 ± 2.17 | 11 ± 1.57 |
| T2 | 5 ± 1.24*,† | 6 ± 0.91 | 6 ± 1.02 | 13 ± 1.92 | 13 ± 1.75 | 13 ± 1.71 |
| T3 | 3.76 ± 1.37*,† | 4.98 ± 1.03 | 4.89 ± 0.83 | 14 ± 2.25 | 14 ± 1.87 | 14 ± 1.73 |
| T4 | 3.41 ± 0.98*,† | 4.44 ± 0.88 | 4.46 ± 0.89 | 15 ± 2.43 | 14 ± 2.18 | 14 ± 1.38 |
| T5 | 3.95 ± 1.05*,† | 4.71±1.01 | 4.44 ± 0.75 | 15 ± 1.90 | 14 ± 1.98 | 14 ± 1.40 |
| T6 | 4.05 ± 1.05*,† | 4.77 ± 1.01 | 4.61 ± 0.79 | 15 ± 2.46*,† | 14 ± 1.90 | 14 ± 1.47 |
| T7 | 3.97 ± 1.10*,† | 5 ± 0.88 | 4.68 ± 0.80 | 15 ± 2.32*,† | 14 ± 1.62 | 14 ± 1.36 |
| T8 | 4.08 ± 1.11*,† | 5 ± 1.04 | 4.99 ± 0.91 | 14 ± 2.17 | 14 ± 1.92 | 14 ± 1.49 |
| T9 | 4.92 ± 1.45*,† | 5 ± 1.05 | 5 ± 0.90 | 14 ± 2.34 | 14 ± 2.15 | 14 ± 1.70 |
| T10 | 6 ± 1.62 | 6 ± 1.43 | 6 ± 1.00 | 14 ± 2.24 | 14 ± 2.44 | 14 ± 1.67 |
| T11 | 7 ± 2.04 | 7 ± 1.81 | 7 ± 1.73 | 15 ± 2.42 | 15± 3.14 | 15 ± 1.74 |
| T12 | 7 ± 1.61 | 7 ± 1.83 | 7 ± 1.57 | 17± 2.56 | 16 ± 2.55 | 17 ± 1.83 |
PWc = pedicle width on the concave side; PWv = pedicle width on the convex side; PWn = pedicle width in controls; PLc = pedicle length on the concave side; PLv = pedicle length on the convex side; PLn = pedicle length in controls; *p < 0.05 versus PWn (PLn) group; †p < 0.05 versus PWv (PLv) group.
Fig. 2A–D.
(A) A comparison is shown for pedicle width on the concave and convex sides of the curve in patients with adolescent idiopathic scoliosis and in controls. (B) The changing patterns are shown for pedicle width on the concave and convex sides of each thoracic vertebra. (C) A comparison of pedicle length on the concave and convex sides of the curve is shown for patients with adolescent idiopathic scoliosis and for controls. (D) The changing patterns of pedicle length on the concave and convex sides of each thoracic vertebra are shown. ap < 0.05 versus control group; bp < 0.05 versus convex group.
Fig. 3A–B.
Variation of the (A) degree of pedicle width and (B) pedicle length among four different regions of the thoracic spine are shown. ap < 0.05 versus the AV-SC group; bp < 0.05 versus the NAV-NSC group. AV-SC = apical vertebra in the structural curve; NAV-SC = nonapical vertebra in the structural curve; AV-NSC = apical vertebra in the nonstructural curve; NAV-NSC = nonapical vertebra in the nonstructural curve VDPW = variation degree of pedicle width; VDPL = variation degree of pedicle length.
Pedicle Classification
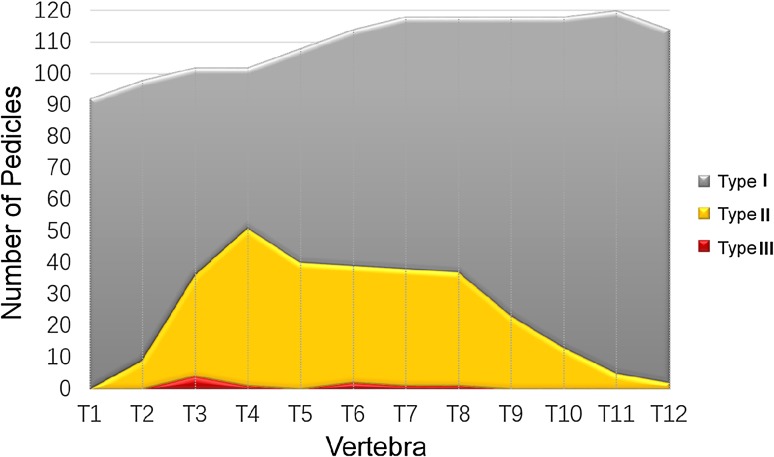
There were more dysplastic pedicles (Types I and II) in patients with adolescent idiopathic scoliosis (22%; 293 of 1322) than there were in control subjects (13%; 178 of 1396) (odds ratio [OR], 0.51; 95% CI, 0.42–0.63; p < 0.001). In patients with adolescent idiopathic scoliosis, 1% (nine of 1322) of pedicles could be classified as Type I, 21% (284 of 1322) as Type II, and 78% (1029 of 1322) as Type III (Table 4). Thus, a total of 22% (293 of 1322) of the thoracic pedicles in patients with Lenke Type 1 adolescent idiopathic scoliosis were dysplastic, and 82% (241 of 293) of the dysplastic pedicles were located in T3 to T8 (Fig. 4) (Table 5). On the concave side, dysplastic pedicles accounted for 34% (228 of 661), which is higher than that on the convex side (10%; 65 of 661) (OR, 4.83; 95% CI, 3.57–6.53; p < 0.001) (Fig. 5A). Further, 32% (43 of 136) of pedicles in AV-SC are dysplastic, and 29% are dysplastic in NAV-SC (35 of 120). There were few differences between AV-SC and AV-NSC. However the rate of dysplastic pedicles in AV-SC (32%; 43 of 136) was higher than in NAV-SC (20%; 105 of 536) (OR, 1.90; 95% CI, 1.25–2.89; p = 0.004) and in NAV-NSC (21%; 110 of 530) (OR, 1.77; 95% CI, 1.16–2.68; p = 0.009) (Fig. 5B).
Table 4.
Distribution of the three types of pedicles
| Variable | Type I | Type II | Type III | Total |
|---|---|---|---|---|
| Total number of controls without deformity | 0 | 178 (13%) | 1218 (87%) | 1396 |
| Total number of patients with adolescent idiopathic scoliosis | 9 (1%) | 284 (21%) | 1029 (78%) | 1322 |
| Distribution on concave/convex sides | ||||
| Concave side | 9 (1%) | 219 (33%) | 433 (66%) | 661 |
| Convex side | 0 | 65 (10%) | 596 (90%) | 661 |
| Distribution on four regions | ||||
| AV-SC | 4 (3%) | 39 (29%) | 93 (68%) | 136 |
| NAV-SC | 4 (1%) | 101 (19%) | 431 (80%) | 536 |
| AV-NSC | 1 (1%) | 34 (28%) | 85 (71%) | 120 |
| NAV-NSC | 0 | 110 (21%) | 420 (79%) | 530 |
AV-SC = apical vertebra in the structural curve; NAV-SC = nonapical vertebra in the structural curve; AV-NSC = apical vertebra in the nonstructural curve; NAV-NSC = nonapical vertebra in the nonstructural curve.
Fig. 4.
The distribution of pedicles, defined as Types I through III, in each thoracic vertebra of the adolescent idiopathic scoliosis spine is shown.
Table 5.
Distribution on 12 levels of thoracic vertebra in patients with adolescent idiopathic scoliosis
| Type | T1 | T2 | T3 | T4 | T5 | T6 | T7 | T8 | T9 | T10 | T11 | T12 | Total |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 4 | 1 | 2 | 1 | 1 | 9 | |||||||
| 2 | 9 | 32 | 50 | 40 | 37 | 37 | 36 | 23 | 13 | 5 | 2 | 284 | |
| 3 | 92 | 89 | 66 | 51 | 68 | 75 | 80 | 81 | 95 | 105 | 115 | 112 | 1029 |
Fig. 5A–B.
(A) The distribution of dysplastic pedicles on the concave and convex sides of the curvature and (B) in the four regions of the thoracic spine are shown. ap < 0.05 versus the AV-SC group; bp < 0.05 versus the convex group. AV-SC = apical vertebra in the structural curve; NAV-SC = nonapical vertebra in the structural curve; AV-NSC = apical vertebra in the nonstructural curve; NAV-NSC = nonapical vertebra in the nonstructural curve.
Discussion
Pedicle screw instrumentation has become a popular and widely accepted surgical technique for treatment of patients with adolescent idiopathic scoliosis [1, 16, 18, 20, 25]. Although some newly developed navigation techniques may help surgeons place pedicle screws more safely, their use remains limited owing to the poor practicability and universality [15]. Therefore, it is important that spinal surgeons have clear knowledge of the morphometric anatomy of pedicles, especially in deformed spines, to guarantee the safest pedicle screw placement. Using CT scans, we conducted a morphologic study of thoracic pedicles in 60 female patients with Lenke Type 1 adolescent idiopathic scoliosis and 60 sex-, age-, and height-matched controls, which provided a more-accurate assessment than previously published studies because of our large sample size and sample homogeneity [4, 12].
Although there were innovative aspects of this work, our study has some limitations. We included only female subjects in the adolescent idiopathic scoliosis and control groups to improve homogeneity. This means that our results cannot necessarily be applied to males; however, most patients with adolescent idiopathic scoliosis are female. In the same way, it would have been ideal if we could repeat the same measurements in all other patients with Lenke-type adolescent idiopathic scoliosis and observe if there were any differences in morphologic features of the pedicle among individuals with different Lenke curve types. However, it was difficult to do so in the current study owing to the limited number of other patients with Lenke curve types in our patient cohort. The entire program was conducted at one Asian hospital, which again limits generalizability to other geographic locations and socioeconomic demographics that may have variable access to early nonoperative interventions to limit curve progression and potential subsequent morphologic changes.
In addition, we chose age as a surrogate factor to represent skeletal maturity, even though Risser stage [22, 27, 30] is a more-accurate reflection of skeletal development. This choice was driven by practical concerns; we were unable to obtain the additional radiographs (AP view of the pelvis) to calculate the Risser stage for patients in the control group. Unfortunately, we did not collect weight information of the studied subjects, therefore BMI could not be used to match controls with patients with adolescent idiopathic scoliosis. Additionally we did not stratify data by curve severity or progression, which is a limitation of our study. The reason for this was that all subjects in the adolescent idiopathic scoliosis group eventually underwent instrumented reconstruction, suggesting that all included subjects had an advanced and severe deformity at the time of imaging, therefore there would not have been enough patients with adolescent idiopathic scoliosis with milder curves to stratify in this way. Although this does not affect the utility of our data to improve the understanding of morphologic features for surgical planning, it does limit the use of this information to patients with more-advanced adolescent idiopathic scoliosis.
Pedicle width is widely accepted as the limiting factor in screw-caliber selection owing to its smaller size compared with other diameters of the pedicle [12, 31]. Similar to previous studies [2, 4, 9, 31, 37], we found PWc to be narrower than PWv. In addition, our results showed that there was no difference between PWv and PWn, indicating that the concave side is the dysplastic side of the curve, while the pedicles on the convex side seem to be normal. Pedicle width showed decreasing dimensions from T1 to T4 followed by increasing dimensions from T5 to T12 in patients with adolescent idiopathic scoliosis and the controls. The relatively small pedicles were located between T3 and T8, and T4 was the narrowest. Based on the Lenke classification, we further classified the thoracic vertebrae of patients with adolescent idiopathic scoliosis into four regions (AV-SC, NAV-SC, AV-NSC, and NAV-NSC) in the hopes of better defining the characteristics of each region. We found that the unbalanced development of pedicle width was most severe in AV-SC, as VDPW in AV-SC is the highest among the four regions. Consistently, dysplastic pedicles were observed mostly in AV-SC, indicating that AV-SC is the most severely deformed region of the thoracic spine and the AV-SC region might be the origin of the adolescent idiopathic scoliosis curvature.
Furthermore, based on pedicle width, pedicles were classified as three types: pedicle width less than 2 mm as Type I, 2 mm to 4 mm as Type II, and greater than 4 mm as Type III. Types I and II were defined as dysplastic pedicles [31]. The prevalence and distribution of dysplastic pedicles were evaluated in patients with adolescent idiopathic scoliosis. A total of 22% (293 of 1322) of the pedicles in the patients were dysplastic. The pedicles on the concave side had a greater chance of being dysplastic (34.49%; 228 of 661) than those on the convex side (10%; 65 of 661). Dysplastic pedicles were observed with an obviously high rate of 82% in T3 to T8 (241 of 293), which highlights the risk of perforations during surgery and insertion of pedicle screws at the T3 to T8 level, especially in surgeries involving T4.
We found that pedicle width on the concave side was narrower than on the convex side, and that morphologic features of the pedicle on the convex side were relatively normal in patients with adolescent idiopathic scoliosis compared with the controls. In patients and controls, pedicle width showed decreasing dimensions from T1 to T4 followed by increasing dimensions from T5 to T12. The relatively narrow pedicles were located between T3 and T8, and the narrowest was in T4. Pedicle length showed increasing dimensions from T1 to T12, and generally there were few differences between the concave and convex sides, or between patients with adolescent idiopathic scoliosis and controls, in terms of pedicle length. We also found that the AV-SC had the greatest variation degree with highest dysplastic pedicle occurrence rate. The variation degree tended to decrease progressively following the order of AV-SC, AV-NSC, NAV-SC, and NAV-NSC. In other words, apical > nonapical, structural curve > nonstructural curve. Our study can help surgeons perform preoperative assessments in females with adolescent idiopathic scoliosis, and with preoperative and intraoperative management for difficult pedicle screw placement. In particular, our results suggest that surgeons should exercise increased vigilance when selecting pedicle screw dimensions, especially in the concave aspect of the mid-thoracic curve, to avoid cortical breeches. Future studies should evaluate morphologic features of the pedicle in other patients with Lenke types of adolescent idiopathic scoliosis, and in cohorts including males and females, to improve generalizability.
Acknowledgment
We thank Jinxin Zhang MD, Xuan Du MM, and Xiaohan Liu MM, (Department of Medical Statistics and Epidemiology, School of Public Health, Sun Yat-sen University) for their help with the statistical analysis.
Footnotes
Funding for this study was received from the National Natural Science Foundation of China (PS) No. 81371908; (CX) No. 81472039; (PS) No. 81572091; and (WG) No. 81601898 and the China Postdoctoral Science Foundation (No. 2017M613177).
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research ® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
The Institutional Research Ethical Committee of the First Affiliated Hospital of Sun Yat-sen University approved the human protocol for this investigation, and each author certifies that all investigations were conducted in conformity with ethical principles of research.
This work was performed at the Department of Orthopaedic Surgery, Guangdong Provincial Key Laboratory of Orthopedics and Traumatology, the First Affiliated Hospital of Sun Yat-sen University, Guangzhou, China.
An erratum to this article is available at https://doi.org/10.1007/s11999-017-5484-5.
References
- 1.Boos N, Webb JK. Pedicle screw fixation in spinal disorders: a European view. Eur Spine J. 1997;6:2–18. doi: 10.1007/BF01676569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Catan H, Buluc L, Anik Y, Ayyildiz E, Sarlak AY. Pedicle morphology of the thoracic spine in preadolescent idiopathic scoliosis: magnetic resonance supported analysis. Eur Spine J. 2007;16:1203–1208. doi: 10.1007/s00586-006-0281-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chadha M, Balain B, Maini L, Dhaon BK. Pedicle morphology of the lower thoracic, lumbar, and S1 vertebrae: an Indian perspective. Spine (Phila Pa 1976). 2003;28:744–749. [PubMed]
- 4.Davis CM, Grant CA, Pearcy MJ, Askin GN, Labrom RD, Izatt MT, Adam CJ, Little JP. Is there asymmetry between the concave and convex pedicles in adolescent idiopathic scoliosis? A CT investigation. Clin Orthop Relat Res. 2017;475:884–893. doi: 10.1007/s11999-016-5188-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Di Silvestre M, Parisini P, Lolli F, Bakaloudis G. Complications of thoracic pedicle screws in scoliosis treatment. Spine (Phila Pa 1976). 2007;32:1655–1661. [DOI] [PubMed]
- 6.Ebraheim NA, Xu R, Ahmad M, Yeasting RA. Projection of the thoracic pedicle and its morphometric analysis. Spine (Phila Pa 1976). 1997;22:233–238. [DOI] [PubMed]
- 7.Gstoettner M, Lechner R, Glodny B, Thaler M, Bach CM. Inter- and intraobserver reliability assessment of computed tomographic 3D measurement of pedicles in scoliosis and size matching with pedicle screws. Eur Spine J. 2011;20:1771–1779. doi: 10.1007/s00586-011-1908-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hamill CL, Lenke LG, Bridwell KH, Chapman MP, Blanke K, Baldus C. The use of pedicle screw fixation to improve correction in the lumbar spine of patients with idiopathic scoliosis: is it warranted? Spine (Phila Pa 1976). 1996;21:1241–1249. [DOI] [PubMed]
- 9.Hassan E, Liau KM, Ariffin I, Halim Yusof A. Internal morphometry of thoracic pedicles in the immature spine. Spine (Phila Pa 1976). 2010;35:1253–1256. [DOI] [PubMed]
- 10.Hicks JM, Singla A, Shen FH, Arlet V. Complications of pedicle screw fixation in scoliosis surgery: a systematic review. Spine (Phila Pa 1976). 2010;35:E465–470. [DOI] [PubMed]
- 11.Hou S, Hu R, Shi Y. Pedicle morphology of the lower thoracic and lumbar spine in a Chinese population. Spine (Phila Pa 1976). 1993;18:1850–1855. [DOI] [PubMed]
- 12.Hu X, Siemionow KB, Lieberman IH. Thoracic and lumbar vertebrae morphology in Lenke type 1 female adolescent idiopathic scoliosis patients. Int J Spine Surg. 2014 Dec 1;8. doi: 10.14444/1030. Available at: https://www.ncbi.nlm.nih.gov/pubmed/25694922. Accessed July 7, 2017. [DOI] [PMC free article] [PubMed]
- 13.Kesling KL, Reinker KA. Scoliosis in twins: a meta-analysis of the literature and report of six cases. Spine (Phila Pa 1976). 1997;22:2009–2014; discussion 2015. [DOI] [PubMed]
- 14.Krag MH, Weaver DL, Beynnon BD, Haugh LD. Morphometry of the thoracic and lumbar spine related to transpedicular screw placement for surgical spinal fixation. Spine (Phila Pa 1976). 1988;13:27–32. [DOI] [PubMed]
- 15.Kuraishi S, Takahashi J, Hirabayashi H, Hashidate H, Ogihara N, Mukaiyama K, Kato H. Pedicle morphology using computed tomography-based navigation system in adolescent idiopathic scoliosis. J Spinal Disord Tech. 2013;26:22–28. doi: 10.1097/BSD.0b013e31823162ef. [DOI] [PubMed] [Google Scholar]
- 16.Lehman RA Jr, Lenke LG, Keeler KA, Kim YJ, Buchowski JM, Cheh G, Kuhns CA, Bridwell KH. Operative treatment of adolescent idiopathic scoliosis with posterior pedicle screw-only constructs: minimum three-year follow-up of one hundred fourteen cases. Spine (Phila Pa 1976). 2008;33:1598–1604. [DOI] [PubMed]
- 17.Lenke LG, Betz RR, Clements D, Merola A, Haher T, Lowe T, Newton P, Bridwell KH, Blanke K. Curve prevalence of a new classification of operative adolescent idiopathic scoliosis: does classification correlate with treatment? Spine (Phila Pa 1976). 2002;27:604–611. [DOI] [PubMed]
- 18.Lenke LG, Kuklo TR, Ondra S, Polly DW Jr. Rationale behind the current state-of-the-art treatment of scoliosis (in the pedicle screw era). Spine (Phila Pa 1976). 2008;33:1051–1054. [DOI] [PubMed]
- 19.Liljenqvist UR, Allkemper T, Hackenberg L, Link TM, Steinbeck J, Halm HF. Analysis of vertebral morphology in idiopathic scoliosis with use of magnetic resonance imaging and multiplanar reconstruction. J Bone Joint Surg Am. 2002;84:359–368. doi: 10.2106/00004623-200203000-00005. [DOI] [PubMed] [Google Scholar]
- 20.Liljenqvist UR, Halm HF, Link TM. Pedicle screw instrumentation of the thoracic spine in idiopathic scoliosis. Spine (Phila Pa 1976). 1997;22:2239–2245. [DOI] [PubMed]
- 21.Lonstein JE. Adolescent idiopathic scoliosis. Lancet. 1994;344:1407–1412. doi: 10.1016/S0140-6736(94)90572-X. [DOI] [PubMed] [Google Scholar]
- 22.Lonstein JE, Carlson JM. The prediction of curve progression in untreated idiopathic scoliosis during growth. J Bone Joint Surg Am. 1984;66:1061–1071. doi: 10.2106/00004623-198466070-00013. [DOI] [PubMed] [Google Scholar]
- 23.Mac-Thiong JM, Parent S, Poitras B, Joncas J, Hubert L. Neurological outcome and management of pedicle screws misplaced totally within the spinal canal. Spine (Phila Pa 1976). 2013;38:229–237. [DOI] [PubMed]
- 24.Misenhimer GR, Peek RD, Wiltse LL, Rothman SL, Widell EH Jr. Anatomic analysis of pedicle cortical and cancellous diameter as related to screw size. Spine (Phila Pa 1976). 1989;14:367–372. [DOI] [PubMed]
- 25.Modi HN, Suh SW, Fernandez H, Yang JH, Song HR. Accuracy and safety of pedicle screw placement in neuromuscular scoliosis with free-hand technique. Eur Spine J. 2008;17:1686–1696. doi: 10.1007/s00586-008-0795-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mueller TL, Miller NH, Baulesh DM, Hastings LH, Chang FM, Georgopoulos G, Benefield EM, Pan Z, Erickson MA. The safety of spinal pedicle screws in children ages 1 to 12. Spine J. 2013;13:894–901. doi: 10.1016/j.spinee.2012.10.040. [DOI] [PubMed] [Google Scholar]
- 27.Nault ML, Parent S, Phan P, Roy-Beaudry M, Labelle H, Rivard M. A modified Risser grading system predicts the curve acceleration phase of female adolescent idiopathic scoliosis. J Bone Joint Surg Am. 2010;92:1073–1081. doi: 10.2106/JBJS.H.01759. [DOI] [PubMed] [Google Scholar]
- 28.O’Brien MF, Lenke LG, Mardjetko S, Lowe TG, Kong Y, Eck K, Smith D. Pedicle morphology in thoracic adolescent idiopathic scoliosis: is pedicle fixation an anatomically viable technique? Spine (Phila Pa 1976). 2000;25:2285–2293. [DOI] [PubMed]
- 29.Rajwani T, Bagnall KM, Lambert R, Videman T, Kautz J, Moreau M, Mahood J, Raso VJ, Bhargava R. Using magnetic resonance imaging to characterize pedicle asymmetry in both normal patients and patients with adolescent idiopathic scoliosis. Spine (Phila Pa 1976). 2004;29:E145–152. [DOI] [PubMed]
- 30.Risser JC, Ferguson AB. Scoliosis: its prognosis. J Bone Joint Surg. 1936;18:667–670. [Google Scholar]
- 31.Sarwahi V, Sugarman EP, Wollowick AL, Amaral TD, Lo Y, Thornhill B. Prevalence, distribution, and surgical relevance of abnormal pedicles in spines with adolescent idiopathic scoliosis vs. no deformity: a CT-based study. J Bone Joint Surg Am. 2014;96:e92. doi: 10.2106/JBJS.M.01058. [DOI] [PubMed] [Google Scholar]
- 32.Vaccaro AR, Rizzolo SJ, Allardyce TJ, Ramsey M, Salvo J, Balderston RA, Cotler JM. Placement of pedicle screws in the thoracic spine. Part I: Morphometric analysis of the thoracic vertebrae. J Bone Joint Surg Am. 1995;77:1193–1199. doi: 10.2106/00004623-199508000-00008. [DOI] [PubMed] [Google Scholar]
- 33.Yu CC, Bajwa NS, Toy JO, Ahn UM, Ahn NU. Pedicle morphometry of upper thoracic vertebrae: an anatomic study of 503 cadaveric specimens. Spine (Phila Pa 1976). 2014;39:E1201–1209. [DOI] [PubMed]
- 34.Yu CC, Yuh RT, Bajwa NS, Toy JO, Ahn UM, Ahn NU. Lower thoracic pedicle morphometry: male, taller, and heavier specimens have bigger pedicles. Spine (Phila Pa 1976). 2015;40:E323–331. [DOI] [PubMed]
- 35.Zheng C, Huang Q, Hu Y, Wang X, Chen W. Computed tomographic morphometry of thoracic pedicles: safety pedicle parameter measurement of the Chinese immature thoracic spine. Int Orthop. 2009;33:1663–1668. doi: 10.1007/s00264-008-0675-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zhuang Z, Xie Z, Ding S, Chen Y, Luo J, Wang X, Kong K. Evaluation of thoracic pedicle morphometry in a Chinese population using 3D reformatted CT. Clin Anat. 2012;25:461–467. doi: 10.1002/ca.21265. [DOI] [PubMed] [Google Scholar]
- 37.Zindrick MR, Knight GW, Sartori MJ, Carnevale TJ, Patwardhan AG, Lorenz MA. Pedicle morphology of the immature thoracolumbar spine. Spine (Phila Pa 1976). 2000;25:2726–2735. [DOI] [PubMed]