Abstract
Candida spp. adhere to medical devices, such as catheters, forming drug-tolerant biofilms that resist killing by the immune system. Little is known about how C. glabrata, an emerging pathogen, resists attack by phagocytes. Here we show that upon encounter with planktonic (non-biofilm) C. glabrata, human neutrophils initially phagocytose the yeast and subsequently release neutrophil extracellular traps (NETs), complexes of DNA, histones, and proteins capable of inhibiting fungal growth and dissemination. When exposed to C. glabrata biofilms, neutrophils also release NETs, but significantly fewer than in response to planktonic cells. Impaired killing of biofilm parallels the decrease in NET production. Compared to biofilm, neutrophils generate higher levels of reactive oxygen species (ROS) when presented with planktonic organisms, and pharmacologic inhibition of NADPH-oxidase partially impairs NET production. In contrast, inhibition of phagocytosis nearly completely blocks NET release to both biofilm and planktonic organisms. Imaging of the host response to C. glabrata in a rat vascular model of infection supports a role for NET release in vivo. Taken together, these findings show that C. glabrata triggers NET release. The diminished NET response to C. glabrata biofilms likely contributes to the resilience of these structured communities to host defenses.
Introduction
The most common nosocomial fungal pathogen, Candida, causes disseminated, invasive disease with mortality near 35%1–3. Patients treated with immunosuppressive medications, receiving antibiotics, or residing in intensive care units are at particularly high risk for infection4. In addition, indispensable medical devices, such as vascular catheters, allow Candida to form resilient, surface-associated biofilm communities that tolerate antifungal drugs and resist host defenses5–10. Nearly 80% of patients with invasive candidiasis have implanted medical devices2. The fungal biofilms associated with these devices are notoriously difficult to eradicate clinically, and studies are just beginning to shed light on how they survive immune attack5–13. C. albicans has served as the model pathogen for the majority of these investigations.
Neutrophils are a critical first line of defense against fungal pathogens, including Candida 2,14–18. In response to planktonic, or non-biofilm C. albicans, they release neutrophil extracellular traps (NETs), which are webs of DNA, histones, and proteins with antifungal activity19–22. These structures can prevent pathogen dissemination and kill organisms too large to be phagocytosed19,20. However, a recent investigation revealed that neutrophils fail to release NETs in response to biofilms produced by C. albicans 12. This explains, in part, why neutrophils are ineffective at controlling C. albicans device-associated biofilm infections. The impaired neutrophil function was linked to the biofilm matrix, the fungal-produced extracellular material that coheres cells within the biofilm and protects them from external insults12,23. The composition of this material varies significantly among Candida spp. and it remains a mystery if other species employ this mechanism to resist killing by neutrophils24–27.
Historically, C. albicans has accounted for the majority of invasive candidiasis. However, there has been a global shift and emergence of non-albicans Candida spp., which now account for 55% of disease3. Of these, C. glabrata is frequently the most prevalent, particularly in Europe and North America18,28. This emerging pathogen poses obstacles to treatment, including increased intrinsic resistance to commonly used antifungals, such as azoles, and the rapid emergence of drug resistance during treatment4,29. The mortality for invasive C. glabrata infection is astonishingly high, even greater than that for C. albicans 18,30.
Like C. albicans, C. glabrata forms biofilms on medical devices and mucosal surfaces6,31,32. However, C. glabrata and C. albicans vary genetically and morphologically29,33. The genome of C. albicans is diploid, whereas C. glabrata is haploid and phylogenetically closer to Saccharomyces cerevisiae, or baker’s yeast. C. glabrata grows strictly as a relatively small yeast (1–4 µm), while C. albicans produces larger yeast forms (4–7 µm), as well as filamentous forms (pseudohyphae and hyphae), which serve as the more potent stimuli for NET formation20,34. In the current study, we investigate the neutrophil response to C. glabrata during planktonic and biofilm growth and identify stark differences compared to C. albicans.
Results
Neutrophils release NETs in response to planktonic C. glabrata
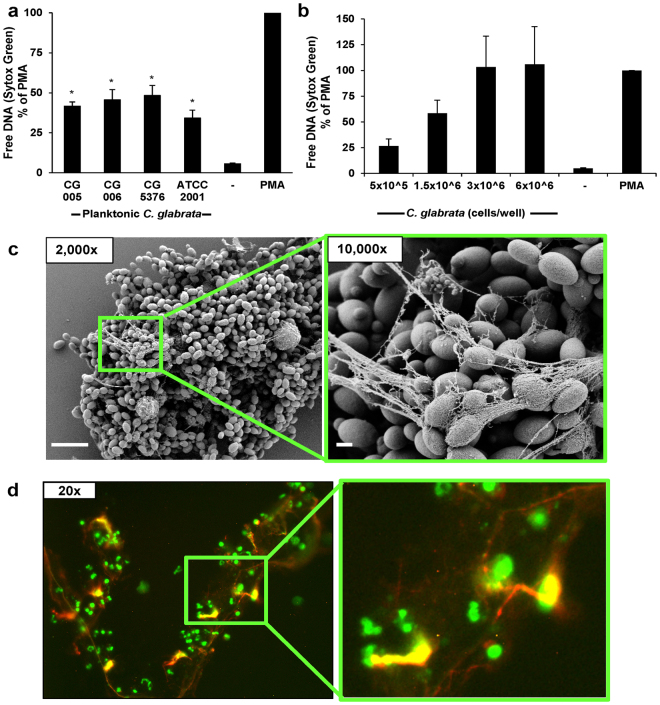
Prior investigations have demonstrated NET release to hyphal, but not yeast forms of C. albicans 20. As C. glabrata does not filament to form hyphae, our initial experiments examined the neutrophil response to planktonic C. glabrata with the inclusion of strains collected from the bloodstream, vagina, and gastrointestinal tract of patients35,36. To estimate NET release, we utilized Sytox Green, a cell-impermeable dye that fluoresces upon DNA binding12,37. After co-culture with human neutrophils for 4 h, each C. glabrata strain triggered fluorescence, consistent with the production of NETs (Fig. 1a). At a concentration of 1.5 × 106 cells/well, each strain elicited similar fluorescence. These values ranged from approximately 35–50% of the levels measured for the positive control, phorbol myristate acetate (PMA), a potent stimulus for NET production38. Given the similarity among the neutrophil responses to the strains, we selected a single strain (CG 006) for additional planktonic studies. We next examined the neutrophil response to a variety of C. glabrata concentrations, representing E:T ranging from 2:5 to 1:30. With increasing C. glabrata concentrations, free DNA increased to the levels of the positive control (PMA) (Fig. 1b).
Figure 1.
Planktonic C. glabrata induce release of NETs. (a) Human neutrophils were exposed to four strains of planktonic C. glabrata (1.5 × 106 cells/well) for 4 h. NET release was estimated by Sytox Green detection of free DNA. Results were normalized for the positive control, PMA, and data from 5 experiments performed in triplicate were combined. Neutrophil responses to Candida were analyzed by ANOVA with pairwise comparison to the untreated neutrophil control, *P < 0.05, SEM shown. (b) Various concentrations of planktonic C. glabrata (CG 006) were co-cultured with human neutrophils for 4 h and NET release was estimated using Sytox Green. Results were normalized for the positive control, PMA, and data from 5 experiments performed in triplicate were combined, SEM shown. (c) Neutrophil interactions with planktonic C. glabrata at 4 h were imaged with scanning electron microscopy. Measurement bars represent 10 µm and 1 µm for 2,000x and 10,000x images, respectively. (d) Following co-culture with C. glabrata for 4 h, the neutrophil response was visualized by immunofluorescence using an anti-citrullinated H4 antibody (red) and Sytox Green staining of DNA (green).
To determine if the Sytox Green staining of free DNA represented NET release, we visualized neutrophil-Candida interactions by scanning electron microscopy (Fig. 1c). After a 4 h co-culture, we observed fibrillary material extruding from neutrophils and web-like structures coating the planktonic C. glabrata, consistent with the release of NETs. To further evaluate for NET formation, we utilized immunofluorescence labeling of citrullinated histones, a modification frequently present in NETs39 (Fig. 1d and Supplementary Fig. 1). Fluorescent microscopy revealed citrullinated histones (red) co-localizing to the extracellular DNA associated with the neutrophils (green). In this assay, the neutrophils also stained by Sytox Green, due to the membrane permeabilization required for sample processing. Together, these studies reveal extrusion of NETs in response to planktonic C. glabrata.
Planktonic C. glabrata induce rapid NETosis
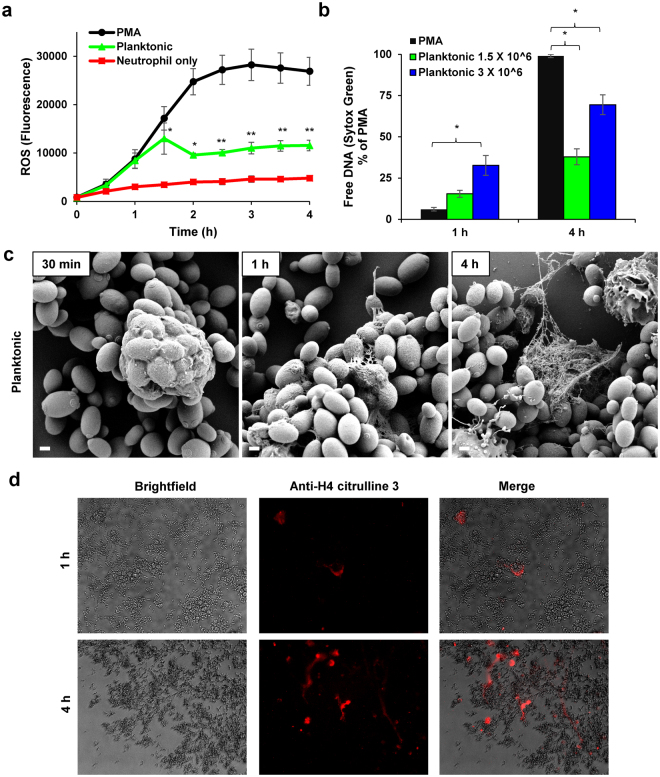
Prior investigations have demonstrated NET release to pathogens through distinct pathways, which vary in their timing of release, capacity for microbial killing, dependence on reactive oxygen species (ROS), and involvement of histone citrullination34,38–43. To further characterize NET release in response to planktonic C. glabrata, we performed several complementary experiments. We first considered the involvement of ROS in NET release and analyzed the generation of ROS by neutrophils pre-stained with a free radical sensor (CM-H2DCFDA). Over the course of 90 min, the ROS production in response to C. glabrata mirrored that of PMA, a strong inducer of ROS-dependent NETosis (Fig. 2a)44. Of note, the pattern of ROS production in response to C. glabrata and PMA differed after 90 min, with ROS production plateauing for C. glabrata, but continuing to rise for PMA, ultimately reaching 2-fold higher levels. These findings suggest that NET release to planktonic C. glabrata may involve ROS-dependent pathways.
Figure 2.
Mechanism of NET release to planktonic C. glabrata. (a) Production of ROS in response to C. glabrata (CG 006 at 3 × 106 cells/well) was measured by fluorescence after neutrophils were pre-stained with oxidative stress indicator CM-DCF and co-cultured with C. glabrata over 4 h. The mean and SEM of 4 experiments performed in triplicate on 4 occasions are shown. Data for each time point were analyzed by ANOVA (*P < 0.05), with pairwise comparisons using the Holm-Sidak method (**P < 0.05 for C. glabrata v. PMA). (b) Neutrophils were co-cultured with planktonic C. glabrata for various time points and NET production was estimated by Sytox Green. Results were normalized to the positive control, PMA, and data from 4 experiments performed in triplicate were combined, SEM shown. Data for each time point were analyzed by ANOVA (*P < 0.05 for pairwise comparison by Holm-Sidak). (c) The neutrophil response to planktonic C. glabrata was imaged with scanning electron microscopy at various time points over 4 h. Measurement bars represent 1 µm for 10,000x images. (d) Following co-culture with C. glabrata for 1 h or 4 h, samples were immunolabeled with an anti-citrullinated H4 antibody and a fluorescently labeled (DyLight) secondary antibody and examined with brightfield microscopy and fluorescent (565/620 nm) microscopy.
Our next experiments examined the timing of NET release to planktonic C. glabrata. In contrast to NETs produced through ROS-dependent pathways, those formed independent of ROS are termed “rapid” NETs for their earlier release40,41. Therefore, to further explore NET release to C. glabrata, we examined the kinetics of NET formation using a Sytox Green assay. PMA, an inducer of the ROS-dependent pathway, did not generate NETs at the early (1 h) time point, with free DNA levels similar to neutrophil-only controls (Figs 1a,b and 2b). However, at the later time point (4 h), PMA induced free DNA levels over 10-fold higher. In contrast, co-culture with C. glabrata (1.5 × 106 cells/well) induced a more rapid rise of free DNA, but the levels reached less than 40% of the PMA-treated cells (Fig. 2b). The pattern of NET release to a higher concentration of C. glabrata (3 × 106 cells/well) paralleled that of the lower concentration, augmenting the more rapid NET release. At 1 h, free DNA levels had already reached approximately half of the total observed in response to C. glabrata at 4 h. The early elevation of free DNA in response to C. glabrata suggests the involvement of rapid NETosis.
We further analyzed neutrophil interactions with planktonic C. glabrata over time with scanning electron microscopy (Fig. 2c). After a 30 min co-culture, neutrophils had phagocytosed numerous yeast cells, often multiple per neutrophil. At 1 h, fibrillar material was beginning to extrude from many of the neutrophils. After a 4 h co-culture, webs of material encased the groups of C. glabrata, consistent with the release of NETs. Immunofluorescent imaging for citrullinated histones mirrored the scanning electron microscopy findings of early NET formation. Citrullination of histones was observed within the first hour of co-culture with C. glabrata and increased over the course of the 4 h experiment (Fig. 2d). High levels of histone citrullination during NETosis have also been linked with a more rapid release of NETs, suggesting the involvement of a similar pathway in response to C. glabrata 42.
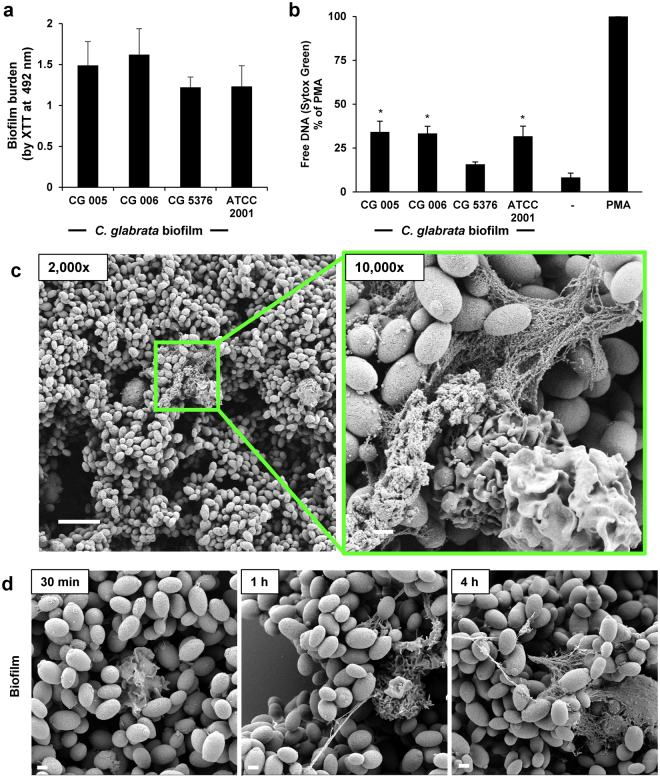
C. glabrata biofilms induce NETs
During biofilm growth, C. albicans fails to elicit the release of NETs, promoting survival upon neutrophil attack12. Our next studies asked if C. glabrata employs a similar strategy to impair neutrophil function. As C. glabrata lacks the capacity for the generation of hyphal or pseudohyphal forms, biofilms formed on coverslips and imaged by scanning electron microscopy revealed mats of adherent yeast (Supplementary Fig. 2). In a microtiter plate model, each of the four clinical isolates similarly formed biofilms with viable burden estimated by XTT metabolic activity after 24 h of growth (Fig. 3a). The biofilm viable burdens were equivalent to planktonic cultures of approximately 3 × 106 to 6 × 106 cells/well (Supplementary Fig. 3). To examine the biofilm-neutrophil interactions, we exposed neutrophils to biofilms for 4 h and measured free DNA with a Sytox Green assay (Fig. 3b). Each of the isolates elicited free DNA, with levels reaching approximately 20–40% of the PMA positive control, consistent with NET release. Using a coverslip model of biofilm formation, we next imaged biofilm-neutrophil interactions by scanning electron microscopy. Following an adherence period and 24 h growth period, C. glabrata formed a dense biofilm on the coverslip, consisting of clusters of adherent ovoid yeast (Supplementary Fig. 2). After a 4 h co-culture, web-like structures were seen protruding from many of the neutrophils, indicating NET formation (Fig. 3c). Like the neutrophil response to planktonic C. glabrata (Fig. 2), NET release appeared to progress over the 4 h time course (Fig. 3d).
Figure 3.
Biofilms formed by C. glabrata elicit NET release. (a) The biofilm-forming capacity of C. glabrata isolates was estimated by XTT assay after 24 h of growth. Assays were performed in triplicate on 3 days and representative data is shown with SD. (b) C. glabrata biofilms (24 h) were co-cultured with human neutrophils and NET release was estimated by Sytox Green detection of free DNA. Results were normalized to the positive control, PMA, and data from 5 experiments performed in triplicate were combined. Neutrophil responses to Candida were analyzed by ANOVA with pairwise comparison to the untreated neutrophil control, *P < 0.05, SEM shown. (c) Neutrophil interactions with C. glabrata at 4 h were imaged with scanning electron microscopy. Measurement bars represent 10 µm and 1 µm for 2,000x and 10,000x images, respectively. (d) The neutrophil response to C. glabrata biofilms was imaged with scanning electron microscopy at various time points over 4 h. Measurement bars represent 1 µm for 10,000x images.
C. glabrata biofilms resist neutrophil killing by modulating NET release
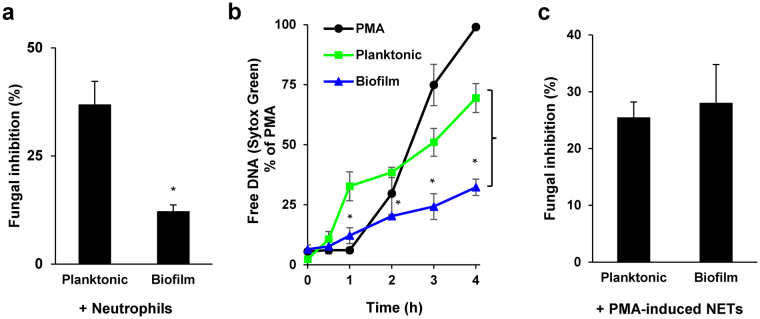
Prior investigations have demonstrated that biofilms formed by C. albicans and C. parapsilosis resist neutrophil killing9,11,12,45. To investigate a similar survival advantage for C. glabrata biofilms, we utilized a killing assay which measures fungal inhibition by neutrophils with an XTT assay12. The activity of neutrophils against biofilms was compared to a similar burden of planktonic organisms (3 × 106 cells/well), as estimated for CG 006 (Supplementary Fig. 3)12. A 4 h exposure to neutrophils reduced the viable burden of biofilm by 12% (Fig. 4a). Time course analysis revealed impaired killing by neutrophils after as little as 6 h of biofilm growth (Supplementary Fig. 4). In contrast, inhibition of planktonic C. glabrata was 3-fold higher (36%). These results suggest that biofilm formation by C. glabrata is a protective mechanism to evade killing by neutrophils.
Figure 4.
Comparison of neutrophil responses to C. glabrata during biofilm and planktonic growth. (a) Planktonic and biofilm C. glabrata were co-cultured with human neutrophils at an effector:target ratio of 1:2 for 4 h and fungal inhibition was estimated by an XTT assay. Results were normalized to the no neutrophil controls, and data from 3 experiments performed in triplicate were combined. Statistical significance was determined using a two-tailed Student’s t-test assuming unequal variances, *P < 0.05, SEM shown. (b) Neutrophils were co-cultured with C. glabrata for 4 h and NET release was estimated by Sytox Green staining of free DNA at various time points. Results were normalized for the positive control, PMA, and data from 4 experiments performed in triplicate were combined. The statistical significance for NET release to biofilm and planktonic C. glabrata were analyzed for each time point using a two-tailed Student’s t-test assuming unequal variances, *P < 0.05, SEM shown. (c) NETs were induced by incubation with PMA for 1.5 h prior to addition to C. glabrata. After 10 min, fungal inhibition was estimated by an XTT assay. Results were normalized to the no neutrophil controls, and data from 4 experiments performed in triplicate were combined. Statistical significance was determined using a two-tailed Student’s t-test assuming unequal variances, *P < 0.05, SEM shown.
One mechanism to account for the resistance of C. glabrata biofilms to neutrophil killing is a diminished or delayed production of NETs. Utilizing Sytox Green assays as a measure of NET release, we compared the neutrophil response to biofilm and planktonic C. glabrata. By 1 h, a significantly higher level of NET formation was observed in response to planktonic C. glabrata, with free DNA levels approximately 35% of the maximum observed for the PMA control (Fig. 4b). The levels continued to rise over time, ultimately reaching near 70% of the control, consistent with a rapid and robust production of NETs. In contrast, NETs were released more slowly in response to biofilms, with free DNA levels near the baseline at 1 h, less than one third of the levels measured for planktonic organisms. After 4 h, the NET response to biofilm was less than half of that observed in response to planktonic organisms. This time course analysis indicates that delayed and impaired NET release is a potential mechanism of innate immune evasion for C. glabrata biofilms.
We next asked if production of NETs is a successful neutrophil strategy to combat C. glabrata during planktonic or biofilm growth. To address this question, we induced NETs by PMA treatment of neutrophils for 1.5 h. Following application to C. glabrata, we measured fungal inhibition with an XTT metabolic assay. A 10 min exposure to PMA-induced NETs similarly inhibited both biofilm and planktonic C. glabrata by approximately 25% (Fig. 4c). These findings show that NETs exhibit antifungal activity against C. glabrata. Similar inhibition of the biofilm and planktonic C. glabrata indicates that the biofilm mode of growth does not provide resistance to killing by NETs. Instead, dampened or delayed triggering of NETs appears to account for the resistance of C. glabrata biofilms to neutrophil killing.
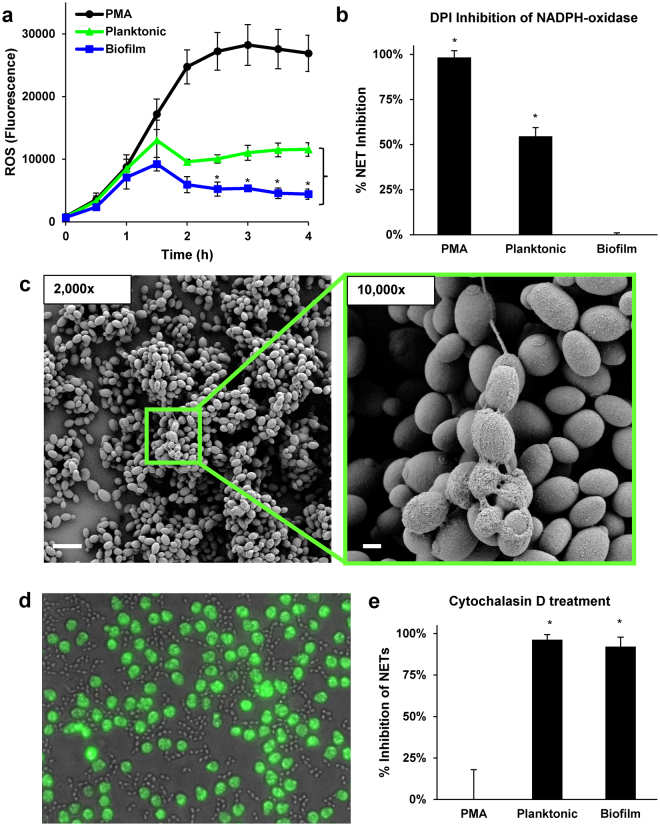
The mechanisms of NET release for biofilm and planktonic C. glabrata
The difference in triggering of NETs by planktonic and biofilm C. glabrata prompted exploration of the mechanism unpinning NET release to this pathogen. Prior investigations examining NET formation in response to C. albicans have identified the involvement of both ROS-dependent and -independent pathways34,40,46,47. The generation of ROS by neutrophils exposed to planktonic C. glabrata suggested the involvement of a ROS-dependent pathway of NET induction (Fig. 2a). A comparison of the neutrophil response to C. glabrata demonstrated heightened ROS production to planktonic cells in comparison to biofilm, which generated levels near the baseline (Fig. 5a). However, ROS levels were significantly lower upon exposure to C. glabrata, when compared to PMA treatment. To test the dependence of NET release on ROS, we utilized DPI (diphenylene iodonium), a pharmacological inhibitor of NADPH oxidase38. Similar to prior investigations, PMA-induction of NETs, which is ROS-dependent, was abolished by treatment with DPI38 (Fig. 5b). In contrast, DPI treatment decreased NET production in response to planktonic C. glabrata by approximately 50%, consistent with only a partial dependence on ROS (Fig. 5b). As expected, inhibition of NADPH-oxidase had no impact on biofilm-induced NETs, as C. glabrata biofilms elicited minimal ROS, a phenomenon previously described for biofilms formed by C. albicans 12. These findings suggests the involvement of an alternative, ROS-independent pathway triggering NETs in response to C. glabrata.
Figure 5.
Mechanism of NET induction by planktonic and biofilm C. glabrata. (a) Production of ROS in response to C. glabrata was measured by fluorescence after neutrophils were pre-stained with oxidative stress indicator CM-H2DCFDA and co-cultured with C. glabrata over 4 h. The mean and SEM of 4 experiments performed in triplicate is shown. The statistical significance neutrophil production of ROS in response to biofilm and planktonic C. glabrata were calculated for each time point using a two-tailed Student’s t-test assuming unequal variances, *P < 0.05, SEM shown. (b) Neutrophils were treated with DPI to inhibit NADPH-oxidase and the release of NETs in response to C. glabrata was measured by Sytox Green. The percent of the total free DNA (untreated) reduced by DPI-treatment for each condition is shown. Data represent 5 experiments performed in triplicate. Statistical significance was determined using a Student’s t-test compared to no inhibition, *P < 0.05, SEM shown. (c) Neutrophil-C. glabrata interactions after 4 h were imaged with scanning electron microscopy. (d) Calcein AM-labeled neutrophils (green) were treated with cytochalasin D to inhibit phagocytosis and added to planktonic C. glabrata. Neutrophil interactions were imaged at 1 h (40x). (e) Neutrophils were treated with cytochalasin D to inhibit phagocytosis and the release of NETs in response to C. glabrata was measured by Sytox Green. The percent of the total free DNA (untreated) reduced by DPI treatment for each condition is shown. Data represent 5 experiments performed in triplicate. Statistical significance was determined using a Student’s t-test compared to no inhibition, *P < 0.05, SEM shown.
To gain insight into alternative pathways promoting NET release, we utilized time-lapse imaging to visualize neutrophil-C. glabrata interactions. Imaging of early neutrophil interactions (30–60 min) revealed the rapid engulfment of C. glabrata by neutrophils pre-stained with Calcein AM (green), often of many yeast per cell (Supplementary Video 1). The ingestion of numerous yeast per phagocyte is similar to prior observations of macrophage-C. glabrata interactions48,49. The findings also corroborate our scanning electron microscopy imaging studies at 30 min, which illustrate the acquisition of numerous yeast per neutrophil (Fig. 2c). For examination of later interactions (2.5–3 h) we included the free DNA stain, propidium iodide (red)12. After 2.5 h, many of the neutrophils appeared viable, retaining the Calcein AM stain and excluding propidium iodide (Supplementary Video 2 and Supplementary Fig. 5). However, a subset of the neutrophils had lost this viability staining and exhibited propidium iodide staining, often displaying a slight halo, suggesting NET release. Time-lapse imaging revealed continued phagocytosis of C. glabrata. Nearly all of the C. glabrata remained viable, marked by exclusion of propidium iodide, with the exception of several propidium iodide-stained groups of C. glabrata. Interestingly, these appeared to be extruded from neutrophils, remaining adherent by only a tether. On several occasions, the bundles of yeast moved in concert with the associated neutrophil during migration (Supplementary Video 3). A similar release of inviable C. glabrata has previously been described for neutrophils and termed “dumping”50. However, in our studies, the propidium iodide staining of the C. glabrata groups was more diffuse than would be expected for individual inviable cells, prompting the question of NET encasement accounting for the fluorescence. By scanning electron microscopy, we identified comparable groups of encased C. glabrata with a single fibrillary extension (Fig. 5c). The web-like covering of these cell groups was consistent with the release of NETs.
We next questioned a role for phagocytosis in the pathway triggering NET release to C. glabrata. To determine if phagocytosis was a prerequisite for NET release, we pre-treated neutrophils with cytochalasin D, which impaired the phagocytosis of C. glabrata (Fig. 5d and Supplementary Video 4). While cytochalasin D treatment had no impact on PMA-induced NET release, it eliminated NET formation in response to both planktonic and biofilm C. glabrata (Fig. 5e). Together, the findings show that C. glabrata induces NET release through a phagocytosis-dependent pathway distinct from the mechanism of PMA-induction.
Neutrophil response to C. glabrata in vivo
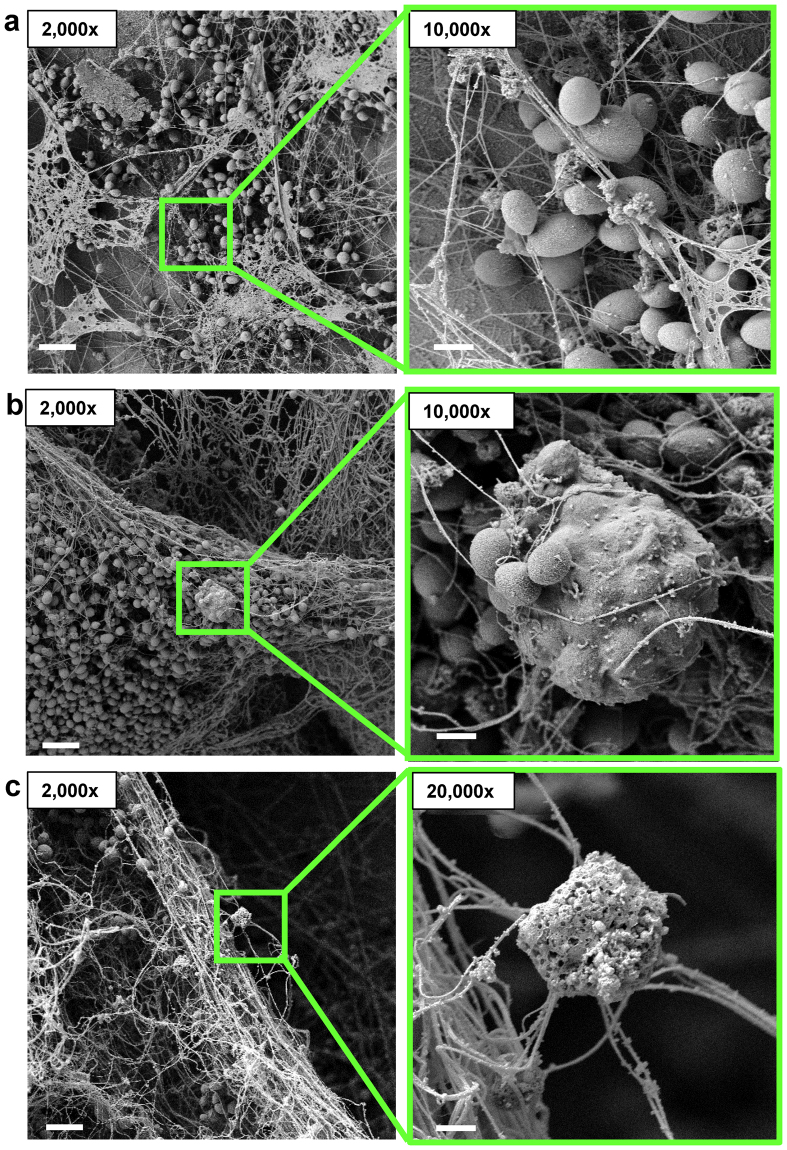
To investigate the neutrophil response to C. glabrata in vivo, we selected a rat venous catheter model of infection35,51,52. In this model, C. glabrata grows adherent to the luminal surface of a vascular catheter, allowing for the imaging of host-Candida interactions upon catheter removal and processing35. After 48 h, imaging of the catheters by scanning electron microscopy revealed a heterogeneous biofilm of adherent yeast cells encased in extracellular material and thread-like structures coating the biofilm (Fig. 6a). Host cells, including leukocytes, were observed to be interacting with C. glabrata. Several of them had engulfed numerous yeast (Fig. 6b), mimicking the initial neutrophil-C. glabrata interactions observed in vitro (Fig. 2c and Supplementary Video 1). Other cells were extending fibrils consistent with NET release (Fig. 6c). Unlike time course experiments in vitro, the in vivo model provides a continuous supply of neutrophils, likely accounting for the multiple interactions observed at a single time point. These findings corroborate our in vitro studies and support a role for NET release in response to C. glabrata during infection.
Figure 6.
C. glabrata appears to induce the formation of NETs in vivo. (a,b,c) C. glabrata was inoculated in the lumen of rat jugular catheters. After 48 h, catheters were harvested and host-fungal interactions on the luminal catheter surface were observed by scanning electron microscopy. Measurement bars represent 10 µm and 1 µm for 2,000x and 10,000x images, respectively.
Discussion
Recent investigations have shed light on the importance of NET release for control of candidiasis and other invasive fungal infections22,53–56. This neutrophil effector mechanism delivers antimicrobial proteins and peptides while preventing dissemination of infection19,21. NET-associated calprotectin has been shown to be critical for the killing of C. albicans in vitro and for the clearance of candidiasis in murine models of infection22. As the larger size of the hyphae produced by C. albicans precludes phagocytosis by neutrophils, NET-mediated fungal killing is thought to be crucial for control of invasive candidiasis20.
We have shown that C. glabrata induces the release of NETs. The process involves the phagocytosis of yeast, often multiple per neutrophil, followed by the extrusion of DNA with citrullinated histones and neutrophil death. As C. glabrata does not form hyphae, this is a surprising finding. For C. albicans, hyphae appear to trigger a NET response more robust than yeast morphotypes20,34,40. While yeast forms of C. albicans have been shown to induce NETosis, these studies have primarily examined NET formation in the context of assay conditions promoting the induction of filamentous growth12,19. However, an investigation employing a yeast-locked mutant revealed neutrophil phagocytosis of yeast cells without the generation of NETs20. An additional study demonstrating diminished NET release to yeast during non-hyphal inducing assay conditions further supports the importance of filamentous growth to NET release against C. albicans 34. Therefore, the induction of NETs by the yeast forms of C. glabrata signifies a neutrophil response distinct from C. albicans and highlights the importance of examining individual species in host-pathogen interactions.
The current studies show that biofilms formed by C. glabrata resist killing by neutrophils (Fig. 4a). This mechanism of resistance to immune attack has been described for other Candida spp., including C. albicans and C. parapsilosis, with biofilms exhibiting 5-fold increase in resistance to neutrophil killing9,11,12,45. For C. albicans, biofilms drastically impair the release of NETs, permitting fungal survival, through a mechanism linked to production of an extracellular matrix12,57. The composition of the biofilm extracellular matrix, the material first encountered by immune cells, has been well described for C. albicans 58,59. Polysaccharides unique to the biofilm matrix and residing in a mannan-glucan complex have been linked to the impaired release of NETs12,59. Like C. albicans, C. glabrata biofilm formation involves production of an extracellular matrix rich in polysaccharides26,60. However, it is not known if these polysaccharides exist in a mannan-glucan complex similar to that observed for C. albicans. Therefore, it is somewhat surprising that biofilm formation by C. glabrata modified NET formation, suggesting an inhibitory pathway conserved among the Candida biofilms. However, in contrast to observations for C. albicans, the current investigation shows that C. glabrata biofilms permit a degree of NET release, although to a lesser extent than planktonic C. glabrata (Fig. 4b). Differences in extracellular matrix and/or biofilm architecture may underpin the altered NET release in response to C. albicans and C. glabrata biofilms.
It has become increasingly clear that multiple pathways are capable of triggering NET production and that these pathways vary with respect to their dependence on ROS, involvement of histone citrullination, and timing of NET release34,38–43. However, less is known about how activation of these specific pathways influences immunity and microbial killing. NET release triggered by planktonic C. glabrata exhibited features of both classical (ROS-dependent) and rapid (ROS-independent) pathways, similar to that observed for C. albicans 34,40,52–54. In contrast, NET formation in response to C. glabrata biofilm was delayed. It is interesting to speculate a role for delayed NET production as a microbial survival mechanism. Unlike biofilms formed by the fungal pathogen Aspergillus fumigatus, which resist killing by NETs, C. glabrata biofilms were susceptible to pre-formed NETs, similar to the pattern observed for C. albicans biofilms12,55. These results point to impairment of neutrophil function as a common feature of Candida biofilms to avoid neutrophil attack, conserved across species.
Methods
Organisms and inoculum
C. glabrata isolates CG 005, CG 006, CG 5376 and ATCC 2001 were used in this study. The previously described strains CG 5376 and ATCC 2001 were initially isolated from the bloodstream and gastrointestinal tract, respectively35,36. CG005 and CG006 strains are vaginal isolates newly described in this study and were obtained in accordance with relevant guidelines and regulations, including the Policy for the Protection of Human Subjects. Strain speciation was confirmed for all isolates by PCR, as previously described61. Strains were stored in 15% (vol/vol) glycerol stock at −80 °C and maintained on yeast extract-peptone-dextrose (YPD) medium + uridine (1% yeast extract, 2% peptone, 2% dextrose, and 80 μg/ml uridine) prior to experiments. Cultures were propagated overnight in YPD + uridine at 30 °C on an orbital shaker at 200 RPM. For studies using planktonic organisms, overnight cultures were inoculated in YPD + uridine broth and grown at 30 °C for 2 h on an orbital shaker at 200 RPM, washed twice with Dulbecco’s phosphate buffered saline (-calcium, -magnesium) (DPBS) (Hyclone Laboratories Inc., Logan, UT), and enumerated by hemocytometer.
Human neutrophil collection
Blood was obtained from study participants after informed consent through a protocol approved by the University of Wisconsin Internal Review Board (IRB) in accordance with relevant guidelines and regulations, including the Policy for the Protection of Human Subjects. Peripheral blood neutrophils were purified by negative antibody selection using the MACSxpress Neutrophil Isolation and MACSxpress Erythrocyte Depletion kits (Miltenyi Biotec Inc., Auburn, CA)12. Neutrophils were enumerated by hemocytometer and resuspended in RPMI 1640 (without phenol red) supplemented with 2% heat-inactivated fetal bovine serum (FBS) and supplemented with glutamine (0.3 mg/ml) for all experiments. Incubations were at 37 °C with 5% CO2.
In vitro microtiter plate biofilms and XTT assay
Biofilms were formed in 96-well plates as previously described12,62. Briefly, C. glabrata was resuspended in RPMI-MOPS at a concentration of 1.5 × 106 cell/ml and 200 µl was added to each well and plates were incubated for 24 h at 37 °C. Biofilm burden was estimated using an XTT (2,3-Bis-(2-Methoxy-4-Nitro-5-Sulfophenyl)-2H-Tetrazolium-5-Carboxanilide) assay as previously described, but with the electron-coupling agent menadione62. One hundred µl of the XTT working solution (0.75 mg/ml XTT in PBS with 10 µM menadione (from 10 mM stock in acetone)) was added to each well. After a 30 min incubation, samples were transferred to a Falcon 96 well U bottom plate and centrifuged for 3 minutes at 1,200 × g to pellet cells. Supernatants (110 µl) were collected and transferred to a 96-well flat bottom plate for absorption reading at 492 nm. To determine an equivalent burden of planktonic organisms, biofilm XTT values were compared to XTT values obtained for a dilution series of planktonic organisms. Results showed a burden of approximately 3 × 106 planktonic cells/well to be similar to the biofilm burden (Supplementary Fig. 1). Therefore, this number of planktonic cells was used in neutrophil co-culture experiments comparing their response to biofilm and planktonic cells.
Biofilm coverslip model
For scanning electron microscopy imaging, a coverslip model of biofilm formation was utilized12,63. Briefly, C. glabrata resuspended in RPMI-MOPS at 1.5 × 106 cells/ml was added to poly-L-lysine coated coverslips (13 mm, Thermanox plastic for cell culture) and allowed to adhere for 30 min at 30 °C. After removal of media and non-adherent cells, 1 ml of RPMI-MOPS was added. Biofilms were propagated for 24 h at 37 °C and washed with DPBS. Neutrophils (5 × 105) were added to biofilm coverslips for 30 min, 1 h, or 4 h, washed gently with DPBS, and prepared for scanning electron microscopy, as described below. For studies utilizing planktonic organisms, a similar burden of planktonic organism was added to the coverslip prior to the addition of neutrophils.
Sytox Green assays
As an estimate of NET release, we adapted a Sytox Green assay for use with C. glabrata 12,37. C. glabrata biofilms were grown in wells of 96-well opaque plates, as described above, and neutrophils (2 × 105 cell/well) were added. Following a 4 h incubation, Sytox Green (Life Technologies, Eugene, OR) was added at a final concentration of 1 μM and fluorescence (excitation 500 nm/emission 528 nm) was measured in an automated plate reader. Experiments using planktonic cells were similarly performed by adding and allowing 3 × 106 cells/well to settle prior to the addition of neutrophils. DPI (10 μM) or Cytochalasin D (10 μg/ml) were included to inhibit ROS and phagocytosis, respectively. PMA (100 nM) was included as a positive control and used for normalization between donors. Background fluorescence for each condition was subtracted from total fluorescence values.
Measurement of ROS
For measurement of neutrophil ROS production, we utilized an oxidative stress assay, as previously described12. Briefly, neutrophils were pre-stained with CM-H2DCFDA (Life Technologies, Eugene, OR) in DPBS for 10 min at room temperature in the dark. Neutrophils (2 × 105 neutrophils/well) were added to C. glabrata biofilms growing in 96-well opaque plates or planktonic C. glabrata (3 × 106 cells/well). Fluorescence (excitation 495 nm; emission 527 nm) was recorded every 30 min for 4 h. Background fluorescence was determined for each C. glabrata condition and subtracted from total fluorescence values prior to data analysis. PMA (100 nM) was included as a positive control.
Fluorescent imaging
Time-lapse fluorescent imaging experiments were performed as previously described12. C. glabrata (5 µl at 3 × 107 cells/ml in DPBS) was added to 384 well plate (Corning 3985) containing 40 µl of media. Neutrophils were labeled with Calcein AM (ThermoFischer Scientific, Waltham, MA) at 0.5 μg/ml in DPBS for 10 min at room temperature in the dark, rinsed twice with DPBS and 5 µl was added to C. glabrata at a concentration of 2 × 105 cells/ml. For a subset of experiments, 2 µl of propidium iodide (80 µM) was added to wells 15 min prior to imaging and plates were reincubated. Images were obtained every 60 sec using brightfield and fluorescence (excitation 480 nm, emission 525 nm and excitation 565, emission 620) at 20x or 40x for 30 minutes on an inverted microscope (Nikon Eclipse TE300) equipped with a motorized stage (Ludl Electronic Products), charge-coupled device camera (CoolSNAP ES2), and MetaVue imaging software v6.2. Images and videos were compiled using ImageJ. Video is shown at 5 frames per second.
Immunofluorescent imaging
As a qualitative measure of NETs, immunofluorescent imaging for histone citrullination was performed. C. glabrata (100 µl at a concentration of 6 × 107 cells/ml) were added to a 4 well µ-Slide (Ibidi) with neutrophils (200 µl at a concentration of 2 × 106 cells/ml). After 4 h, mixtures were fixed with 4% formaldehyde in DPBS for an additional 2 h. Fixed co-cultures were treated with Sytox Green 1 µM in DPBS for 10 min, rinsed 3 × 5 min with DPBS, and incubated with antibody blocking buffer (2% w/v bovine serum albumin (BSA) and 0.02% v/v Tween 20 in DPBS) overnight at 4 °C. All steps were performed very gently to preserve NETs. Following rinsing with antibody binding buffer (0.1% BSA w/v and 0.005% v/v Tween 20 in DPBS), primary antibody (anti-histone H4, citrulline3) in antibody binding buffer at 1:500 was added for 2 h at room temperature39. Samples were rinsed gently 3 × 5 min and secondary antibody (goat-anti rabbit IgG Fc DyLight 594 conjugated) at 1:200 in antibody binding buffer was added for a 2 h incubation in the dark. Samples were rinsed 3 × 5 min with antibody binding buffer and brightfield and fluorescent (excitation 480 nm, emission 525 nm and excitation 565, emission 620) images were obtained using the 20x objective on an inverted microscope (Nikon Eclipse TE300) equipped with a charge-coupled device camera (CoolSNAP ES2) and MetaVue imaging software v6.2. Images were processed using ImageJ.
Killing assays
Briefly, an XTT (2,3-bis-(2-methoxy-4-nitro-5-sulfophenyl)-2H-tetrazolium-5-carboxanilide) metabolic assay was adapted to estimate C. glabrata viability following co-culture with neutrophils8,12. Following a 6, 12, or 24 h incubation period, biofilms grown in microtiter plates were washed with DPBS. In studies comparing the killing of 24 h biofilm and planktonic C. glabrata, biofilms were compared to planktonic cells at a concentration of 3 × 106 cells/well. Neutrophils were added to a final concentration of 1.5 × 106 cells/well (effector:target of 1:2). Following a 4 h co-incubation, an XTT assay was performed, as described above. To determine percent killing, values were compared to wells without neutrophils after subtraction of neutrophil generated XTT baseline absorbance, which was less than 5% of the total read. For killing assays with preformed, PMA-induced NETs, neutrophils at 1.5 × 107 cells/ml were incubated with or without 100 nM PMA for 90 min at 37 °C with gentle rotation. After 90 min, PMA-induced NETs or neutrophil controls were added to biofilms or planktonic cells, as above. After a 10 min incubation, an XTT assay was performed.
In vivo venous catheter biofilm model
All animal procedures were approved by the Institutional Animal Care and Use Committee at the University of Wisconsin according to the guidelines of the Animal Welfare Act, and The Institute of Laboratory Animal Resources Guide for the Care and Use of Laboratory Animals. Specific-pathogen-free rats (Harlan Sprague-Dawley, Indianapolis, Ind.) were used for all studies. A jugular vein rat central venous catheter biofilm infection model was used as previously described35,52. Briefly, 24 h following surgical jugular venous catheter insertion, C. glabrata at 106 cells/ml was instilled in the catheter lumen and flushed at 6 h. After a 48 h incubation, the catheters were harvested and collected for imaging by scanning electron microscopy, as described below.
Scanning electron microscopy
Rat vascular catheter and coverslips were processed and imaged by scanning electron microscopy, as previously described12,52. Briefly, after washing with DPBS, specimens were placed in fixative (4% formaldehyde, 1% glutaraldehyde, in PBS) overnight. After washing with PBS, they were treated with 1% osmium tetroxide and washed again with PBS. Samples were dehydrated through a series of ethanol washes followed by critical point drying and mounted on aluminum stubs with carbon conductive adhesive tabs. Following sputter coating with platinum, samples were imaged in a scanning electron microscope (LEO 1530) at 3 kV.
Statistics
Experiments were performed at least 3 times using neutrophils from different donors on different days. Statistical analyses were performed by Student’s t-test (two-tailed) or ANOVA with comparisons by the Holm-Sidak method using Sigma Stat or Excel software. Differences of P < 0.05 were considered significant.
Data availability
The data that support the findings of this study are available from the corresponding author upon request.
Electronic supplementary material
Acknowledgements
This work was supported by the National Institutes of Health (K08 AI108727) and the Burroughs Wellcome Fund (1012299). We thank David Andes for C. glabrata strains and assistance with animal studies. We are greatly appreciative of study volunteers for blood donation.
Author Contributions
C.J.J. and J.E.N. designed the experiments. C.J.J., J.F.K., A.R.H., and A.H. performed the experiments. C.J.J., J.F.K., and J.E.N. analyzed the data. C.J.J. and J.E.N. wrote the paper.
Competing Interests
The authors declare that they have no competing interests.
Footnotes
Electronic supplementary material
Supplementary information accompanies this paper at 10.1038/s41598-017-13588-6.
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Pfaller MA, Diekema DJ. Epidemiology of invasive candidiasis: a persistent public health problem. Clin Microbiol Rev. 2007;20:133–163. doi: 10.1128/CMR.00029-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Andes DR, et al. Impact of treatment strategy on outcomes in patients with candidemia and other forms of invasive candidiasis: a patient-level quantitative review of randomized trials. Clin Infect Dis. 2012;54:1110–1122. doi: 10.1093/cid/cis021. [DOI] [PubMed] [Google Scholar]
- 3.Horn DL, et al. Epidemiology and outcomes of candidemia in 2019 patients: data from the prospective antifungal therapy alliance registry. Clin Infect Dis. 2009;48:1695–1703. doi: 10.1086/599039. [DOI] [PubMed] [Google Scholar]
- 4.Pappas PG, et al. Clinical Practice Guideline for the Management of Candidiasis: 2016 Update by the Infectious Diseases Society of America. Clin Infect Dis. 2016;62:e1–e50. doi: 10.1093/cid/civ1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Donlan RM. Biofilm formation: a clinically relevant microbiological process. Clin Infect Dis. 2001;33:1387–1392. doi: 10.1086/322972. [DOI] [PubMed] [Google Scholar]
- 6.Kojic EM, Darouiche RO. Candida infections of medical devices. Clin Microbiol Rev. 2004;17:255–267. doi: 10.1128/CMR.17.2.255-267.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kumamoto CA, Vinces MD. Alternative Candida albicans lifestyles: growth on surfaces. Annu Rev Microbiol. 2005;59:113–133. doi: 10.1146/annurev.micro.59.030804.121034. [DOI] [PubMed] [Google Scholar]
- 8.Katragkou A, et al. Interactions between human phagocytes and Candida albicans biofilms alone and in combination with antifungal agents. J Infect Dis. 2010;201:1941–1949. doi: 10.1086/652783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Katragkou A, et al. Effects of interferon-gamma and granulocyte colony-stimulating factor on antifungal activity of human polymorphonuclear neutrophils against Candida albicans grown as biofilms or planktonic cells. Cytokine. 2011;55:330–334. doi: 10.1016/j.cyto.2011.05.007. [DOI] [PubMed] [Google Scholar]
- 10.Chandra J, et al. Biofilm formation by the fungal pathogen Candida albicans: development, architecture, and drug resistance. J Bacteriol. 2001;183:5385–5394. doi: 10.1128/JB.183.18.5385-5394.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Xie Z, et al. Candida albicans biofilms do not trigger reactive oxygen species and evade neutrophil killing. J Infect Dis. 2012;206:1936–1945. doi: 10.1093/infdis/jis607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Johnson CJ, et al. The extracellular matrix of Candida albicans biofilms impairs formation of neutrophil extracellular traps. PLoS Pathog. 2016;12:e1005884. doi: 10.1371/journal.ppat.1005884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ramage G, VandeWalle K, Bachmann SP, Wickes BL, Lopez-Ribot JL. In vitro pharmacodynamic properties of three antifungal agents against preformed Candida albicans biofilms determined by time-kill studies. Antimicrob Agents Chemother. 2002;46:3634–3636. doi: 10.1128/AAC.46.11.3634-3636.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shoham S, Levitz SM. The immune response to fungal infections. Br J Haematol. 2005;129:569–582. doi: 10.1111/j.1365-2141.2005.05397.x. [DOI] [PubMed] [Google Scholar]
- 15.Edwards JE, Jr., Lehrer RI, Stiehm ER, Fischer TJ, Young LS. Severe candidal infections: clinical perspective, immune defense mechanisms, and current concepts of therapy. Ann Intern Med. 1978;89:91–106. doi: 10.7326/0003-4819-89-1-91. [DOI] [PubMed] [Google Scholar]
- 16.Fidel PL., Jr. Immunity to Candida. Oral Dis. 2002;8(Suppl 2):69–75. doi: 10.1034/j.1601-0825.2002.00015.x. [DOI] [PubMed] [Google Scholar]
- 17.Erwig LP, Gow NA. Interactions of fungal pathogens with phagocytes. Nat Rev Microbiol. 2016;14:163–176. doi: 10.1038/nrmicro.2015.21. [DOI] [PubMed] [Google Scholar]
- 18.Andes DR, et al. The epidemiology and outcomes of invasive Candida infections among organ transplant recipients in the United States: results of the Transplant-Associated Infection Surveillance Network (TRANSNET) Transpl Infect Dis. 2016;18:921–931. doi: 10.1111/tid.12613. [DOI] [PubMed] [Google Scholar]
- 19.Urban CF, Reichard U, Brinkmann V, Zychlinsky A. Neutrophil extracellular traps capture and kill Candida albicans yeast and hyphal forms. Cell Microbiol. 2006;8:668–676. doi: 10.1111/j.1462-5822.2005.00659.x. [DOI] [PubMed] [Google Scholar]
- 20.Branzk N, et al. Neutrophils sense microbe size and selectively release neutrophil extracellular traps in response to large pathogens. Nat Immunol. 2014;15:1017–1025. doi: 10.1038/ni.2987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Brinkmann V, et al. Neutrophil extracellular traps kill bacteria. Science. 2004;303:1532–1535. doi: 10.1126/science.1092385. [DOI] [PubMed] [Google Scholar]
- 22.Urban CF, et al. Neutrophil extracellular traps contain calprotectin, a cytosolic protein complex involved in host defense against Candida albicans. PLoS Pathog. 2009;5:e1000639. doi: 10.1371/journal.ppat.1000639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hawser SP, Baillie GS, Douglas LJ. Production of extracellular matrix by Candida albicans biofilms. J Med Microbiol. 1998;47:253–256. doi: 10.1099/00222615-47-3-253. [DOI] [PubMed] [Google Scholar]
- 24.Martins M, et al. Presence of extracellular DNA in the Candida albicans biofilm matrix and its contribution to biofilms. Mycopathologia. 2010;169:323–331. doi: 10.1007/s11046-009-9264-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Al-Fattani MA, Douglas LJ. Biofilm matrix of Candida albicans and Candida tropicalis: chemical composition and role in drug resistance. J Med Microbiol. 2006;55:999–1008. doi: 10.1099/jmm.0.46569-0. [DOI] [PubMed] [Google Scholar]
- 26.Silva S, et al. Biofilms of non-Candida albicans Candida species: quantification, structure and matrix composition. Med Mycol. 2009;47:681–689. doi: 10.3109/13693780802549594. [DOI] [PubMed] [Google Scholar]
- 27.Kuhn DM, Chandra J, Mukherjee PK, Ghannoum MA. Comparison of biofilms formed by Candida albicans and Candida parapsilosis on bioprosthetic surfaces. Infect Immun. 2002;70:878–888. doi: 10.1128/IAI.70.2.878-888.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Leroy O, et al. Epidemiology, management, and risk factors for death of invasive Candida infections in critical care: a multicenter, prospective, observational study in France (2005–2006) Crit Care Med. 2009;37:1612–1618. doi: 10.1097/CCM.0b013e31819efac0. [DOI] [PubMed] [Google Scholar]
- 29.Glockner A, Cornely OA. Candida glabrata–unique features and challenges in the clinical management of invasive infections. Mycoses. 2015;58:445–450. doi: 10.1111/myc.12348. [DOI] [PubMed] [Google Scholar]
- 30.Lyon GM, Karatela S, Sunay S, Adiri Y, Candida Surveillance Study I. Antifungal susceptibility testing of Candida isolates from the Candida surveillance study. J Clin Microbiol. 2010;48:1270–1275. doi: 10.1128/JCM.02363-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hawser SP, Douglas LJ. Biofilm formation by Candida species on the surface of catheter materials in vitro. Infect Immun. 1994;62:915–921. doi: 10.1128/iai.62.3.915-921.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.d’Enfert C, Janbon G. Biofilm formation in Candida glabrata: What have we learnt from functional genomics approaches? FEMS Yeast Res. 2016;16:fov111. doi: 10.1093/femsyr/fov111. [DOI] [PubMed] [Google Scholar]
- 33.Brunke S, Hube B. Two unlike cousins: Candida albicans and C. glabrata infection strategies. Cell Microbiol. 2013;15:701–708. doi: 10.1111/cmi.12091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kenno S, Perito S, Mosci P, Vecchiarelli A, Monari C. Autophagy and Reactive Oxygen Species Are Involved in Neutrophil Extracellular Traps Release Induced by C. albicans Morphotypes. Front Microbiol. 2016;7:879. doi: 10.3389/fmicb.2016.00879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Nett J, Lincoln L, Marchillo K, Andes D. Beta -1,3 glucan as a test for central venous catheter biofilm infection. J Infect Dis. 2007;195:1705–1712. doi: 10.1086/517522. [DOI] [PubMed] [Google Scholar]
- 36.Koszul R, et al. The complete mitochondrial genome sequence of the pathogenic yeast Candida (Torulopsis) glabrata. FEBS Lett. 2003;534:39–48. doi: 10.1016/S0014-5793(02)03749-3. [DOI] [PubMed] [Google Scholar]
- 37.Brinkmann, V., Laube, B., Abu Abed, U., Goosmann, C. & Zychlinsky, A. Neutrophil extracellular traps: how to generate and visualize them. J Vis Exp (2010). [DOI] [PMC free article] [PubMed]
- 38.Fuchs TA, et al. Novel cell death program leads to neutrophil extracellular traps. J Cell Biol. 2007;176:231–241. doi: 10.1083/jcb.200606027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wang Y, et al. Histone hypercitrullination mediates chromatin decondensation and neutrophil extracellular trap formation. J Cell Biol. 2009;184:205–213. doi: 10.1083/jcb.200806072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Byrd AS, O’Brien XM, Johnson CM, Lavigne LM, Reichner JS. An extracellular matrix-based mechanism of rapid neutrophil extracellular trap formation in response to Candida albicans. J Immunol. 2013;190:4136–4148. doi: 10.4049/jimmunol.1202671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Pilsczek FH, et al. A novel mechanism of rapid nuclear neutrophil extracellular trap formation in response to Staphylococcus aureus. J Immunol. 2010;185:7413–7425. doi: 10.4049/jimmunol.1000675. [DOI] [PubMed] [Google Scholar]
- 42.Konig MF, Andrade F. A Critical Reappraisal of Neutrophil Extracellular Traps and NETosis Mimics Based on Differential Requirements for Protein Citrullination. Front Immunol. 2016;7:461. doi: 10.3389/fimmu.2016.00461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Malachowa N, Kobayashi SD, Freedman B, Dorward DW, DeLeo FR. Staphylococcus aureus leukotoxin GH promotes formation of neutrophil extracellular traps. J Immunol. 2013;191:6022–6029. doi: 10.4049/jimmunol.1301821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Remijsen Q, et al. Neutrophil extracellular trap cell death requires both autophagy and superoxide generation. Cell Res. 2011;21:290–304. doi: 10.1038/cr.2010.150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Katragkou A, Chatzimoschou A, Simitsopoulou M, Georgiadou E, Roilides E. Additive antifungal activity of anidulafungin and human neutrophils against Candida parapsilosis biofilms. J Antimicrob Chemother. 2011;66:588–591. doi: 10.1093/jac/dkq466. [DOI] [PubMed] [Google Scholar]
- 46.Byrd AS, et al. NETosis in Neonates: Evidence of a Reactive Oxygen Species-Independent Pathway in Response to Fungal Challenge. J Infect Dis. 2016;213:634–639. doi: 10.1093/infdis/jiv435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Metzler KD, Goosmann C, Lubojemska A, Zychlinsky A, Papayannopoulos V. A myeloperoxidase-containing complex regulates neutrophil elastase release and actin dynamics during NETosis. Cell Rep. 2014;8:883–896. doi: 10.1016/j.celrep.2014.06.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Dementhon K, El-Kirat-Chatel S, Noel T. Development of an in vitro model for the multi-parametric quantification of the cellular interactions between Candida yeasts and phagocytes. PLoS One. 2012;7:e32621. doi: 10.1371/journal.pone.0032621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Keppler-Ross S, Douglas L, Konopka JB, Dean N. Recognition of yeast by murine macrophages requires mannan but not glucan. Eukaryot Cell. 2010;9:1776–1787. doi: 10.1128/EC.00156-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Essig F, Hunniger K, Dietrich S, Figge MT, Kurzai O. Human neutrophils dump Candida glabrata after intracellular killing. Fungal Genet Biol. 2015;84:37–40. doi: 10.1016/j.fgb.2015.09.008. [DOI] [PubMed] [Google Scholar]
- 51.Nett JE, Marchillo K, Andes DR. Modeling of fungal biofilms using a rat central vein catheter. Methods Mol Biol. 2012;845:547–556. doi: 10.1007/978-1-61779-539-8_40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Andes D, et al. Development and characterization of an in vivo central venous catheter Candida albicans biofilm model. Infect Immun. 2004;72:6023–6031. doi: 10.1128/IAI.72.10.6023-6031.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Gratacap, R. L., Scherer, A. K., Seman, B. G. & Wheeler, R. T. Control of mucosal candidiasis in the zebrafish swimbladder depends on neutrophils that block filament invasion and drive extracellular trap production. Infect Immun (2017). [DOI] [PMC free article] [PubMed]
- 54.Bruns S, et al. Production of extracellular traps against Aspergillus fumigatus in vitro and in infected lung tissue is dependent on invading neutrophils and influenced by hydrophobin RodA. PLoS Pathog. 2010;6:e1000873. doi: 10.1371/journal.ppat.1000873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Lee MJ, et al. The fungal exopolysaccharide galactosaminogalactan mediates virulence by enhancing resistance to neutrophil extracellular traps. PLoS Pathog. 2015;11:e1005187. doi: 10.1371/journal.ppat.1005187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Bachiega TF, et al. Participation of dectin-1 receptor on NETs release against Paracoccidioides brasiliensis: Role on extracellular killing. Immunobiology. 2016;221:228–235. doi: 10.1016/j.imbio.2015.09.003. [DOI] [PubMed] [Google Scholar]
- 57.Kernien, J. F., Johnson, C. J. & Nett, J. E. Conserved Inhibition of neutrophil extracellular trap release by clinical Candida albicans biofilms. Journal of Fungi3 (2017). [DOI] [PMC free article] [PubMed]
- 58.Nett, J. E. The Host’s Reply to Candida Biofilm. Pathogens5 (2016). [DOI] [PMC free article] [PubMed]
- 59.Zarnowski R, et al. Novel entries in a fungal biofilm matrix encyclopedia. MBio. 2014;5:e01333–01314. doi: 10.1128/mBio.01333-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Monteiro DR, et al. Silver colloidal nanoparticles: effect on matrix composition and structure of Candida albicans and Candida glabrata biofilms. J Appl Microbiol. 2013;114:1175–1183. doi: 10.1111/jam.12102. [DOI] [PubMed] [Google Scholar]
- 61.Enache-Angoulvant A, et al. Rapid discrimination between Candida glabrata, Candida nivariensis, and Candida bracarensis by use of a singleplex PCR. J Clin Microbiol. 2011;49:3375–3379. doi: 10.1128/JCM.00688-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Nett JE, Cain MT, Crawford K, Andes DR. Optimizing a Candida biofilm microtiter plate model for measurement of antifungal susceptibility by tetrazolium salt assay. J Clin Microbiol. 2011;49:1426–1433. doi: 10.1128/JCM.02273-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Mitchell KF, et al. Community participation in biofilm matrix assembly and function. Proc Natl Acad Sci USA. 2015;112:4092–4097. doi: 10.1073/pnas.1421437112. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon request.