Dear Editor,
I am Dr. Pitipol Choopong, from the Department of Ophthal-mology, Siriraj Hospital, Mahidol University, Bangkok, Thailand. I write to present a case of successful treatment of retinal neovascularization (NV) from tuberculous retinal vasculitis using intravitreal bevacizumab prior to and after laser photocoagulation.
Ocular tuberculosis, a reactivation of latent tuberculous infection, has a broad range of clinical manifestations. The clinical appearance may occur in the eye, around the eye, or on its surface[1]. Among these, involvements of the posterior part of the eye, including retinal vasculitis, choroidal tubercles and choroidal tuberculoma are the most common[2]. Tuberculous retinal vasculitis treatment comprises of a 9 to 12mo course of anti-tuberculosis therapy (ATT) with or without concomitant systemic corticosteroids[3]–[4]. However, despite prompt ATT, ocular complications such as retinal vascular occlusion followed by retinal NV, vitreous hemorrhage, and neovascular glaucoma may occur. The main treatment for these complications is laser photocoagulation of the ischemic retina to induce involution of NV, but recurrent vitreous hemorrhages usually preclude the view of retina and delay the successful laser therapy[5]–[6]. Intravitreal injection of anti-vascular endothelial growth factor (anti-VEGF) temporarily reduces the number of NV and vitreous bleedings. It showed benefits in the treatment of retinal NV from various ocular diseases such as diabetes mellitus, retinal vein occlusion, and uveitis but there was limited evidence for those related to tuberculous retinal vasculitis[7]–[11]. We here reported a case of retinal NV caused by tuberculous retinal vasculitis that was successfully treated with laser photocoagulation together with intravitreal bevacizumab injections.
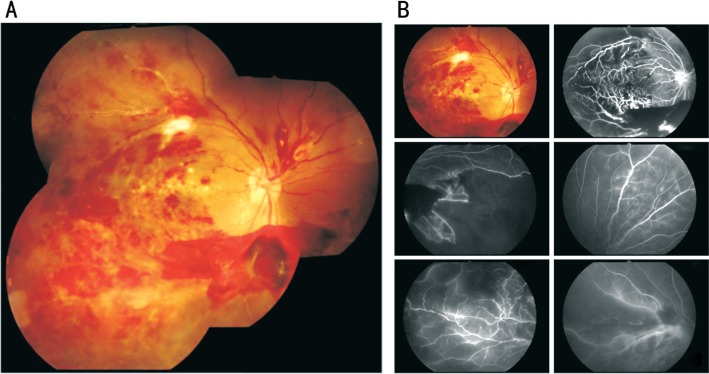
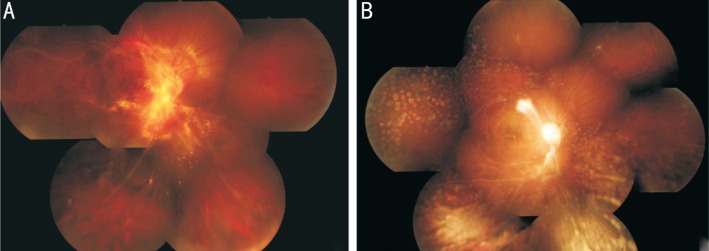
A 29-year-old Thai male presented with progressive loss of vision in his right eye for one month. The best-corrected visual acuity was 6/60 in the right eye and 6/6 in the left eye. Tonometry was normal in both eyes, and slit-lamp examination revealed mild vitreous cells in the right eye without other significant findings. Retinal vasculitis and branch retinal vein occlusion, which occurred mostly in temporal half of the right fundus, were seen by fundoscopic examination. Fluorescein angiography demonstrated multiple large areas of capillaries dropout in the temporal side of the macula and peripheral retinal area. Early and late vascular leakage was also observed throughout the retina (Figure 1). Fundoscopic examination and angiography of the left eye appeared normal. Complete blood count, chest X-ray, ESR, TPHA, VDRL, anti-HIV, ANA, anti-dsDNA, and rheumatoid factor tests were within the normal limits. Interestingly, tuberculin skin test demonstrated highly positive result, with a 19-mm wheal. The diagnosis of presumed tuberculous retinal vasculitis was made. The patient was treated with the standard 4-drug ATT including isoniazid (I), rifampicin (R), pyrazinamide (Z), and ethambutol (E). Retinal vasculitis began to resolve within two weeks after the initiation of therapy. However, two months later, retinal and optic disc NV with vitreous hemorrhage and secondary glaucoma due to peripheral anterior synechiae developed (Figure 2). Intravitreal bevacizumab 1.25 mg/0.05 mL injection was given to the patient two weeks before segmental retinal photocoagulation. The retinal NV resolved considerably in one month after treatments. Trabeculectomy with mitomycin C was performed later to control the intraocular pressure. The patient responded well to a 9mo ATT course (2IRZE/7IR). Unfortunately, he had retinal NV and vitreous hemorrhage recurred two months after the cessation of ATT (seven months after the first injection). We administered the second injection of intravitreal bevacizumab without additional photocoagulation. At last, vitreous hemorrhage and retinal NV completely regressed within two weeks, and there was no recurrence within a 12mo period of follow-up (Figure 2).
Figure 1. Fundus photograph and fluorescein angiogram of tuberculous retinal vasculitis in the right eye.
A: Retinal perivascular infiltration with branch retinal vein occlusion occurred mostly in temporal half area; B: Fluorescein angiogram demonstrated multiple large areas of capillaries dropout in the temporal side of the macula and peripheral retinal area. Early and late vascular leakage was also observed throughout the retina.
Figure 2. Fundus photographs of tuberculous retinal vasculitis in the right eye over treatment period.
A: Retinal and optic disc NV and vitreous hemorrhage occurred 2mo after treatment despite the resolution of retinal vasculitis; B: Complete regression of retinal NV after the second intravitreal bevacizumab injection was observed and there was no recurrence within a 12mo period.
Tuberculous retinal vasculitis could result from either direct invasion of Mycobacterium tuberculosis or a hypersensitivity reaction to tuberculous protein[12]. It is a major risk for developing retinal vascular occlusion, ischemia and infarction. These ischemic vascular complications induce massive production of the VEGF and upregulation of their receptors (VEGFR). The ligation of VEGF on VEGFR induces endothelial cell proliferation, angiogenesis, and increased microvascular permeability which in turn leads to vascular leakage and NV. These also results in adverse effects including macular edema, retinal hemorrhage, vitreous hemorrhage, retinal detachment and permanent visual loss[6],[13].
According to the recommendation of American Thoracic Society, Center for Disease Control, and Infectious Disease Society of America for Extrapulmonary TB, standard 4-drug ATT is given initially for 2mo (2IRZE), followed by 2-drug regimen for 4-7mo (4-7IR)[14]. In our patient, ATT, as a major therapy, proved to be efficacious in controlling retinal vasculitis as well as preventing recurrent inflammatory episodes without concomitant corticosteroids. However, it did not show an effect on prevention or resolution of retinal and optic disc NV. Instead, photocoagulation and intravitreal bevacizumab resolved this complication. Many studies have demonstrated the effectiveness of anti-VEGF to treat NV and its sequelae in various inflammatory diseases[9],[15]–[19]. Intravitreal bevacizumab was very helpful in our circumstance as it rapidly cleared vitreous hemorrhage and reduced the severity of retinal NV. It promoted better retinal evaluation and reduced the waiting time before laser photocoagulation. However, retinal NV may recur despite adequate photocoagulation due to residual VEGF-VEGFR ligation. In our case, an additional intravitreal bevacizumab could regress the blood vessels without the need of supplementary laser. Although intravitreal bevacizumab demonstrated benefits in our case, two previous case reports failed to see the efficacy[10]–[11]. While our case had branch retinal vein occlusion, both previous cases associated with central retinal vein occlusion. The larger extent of venous obstruction could cause more severe retinal ischemia and massive expression of VEGF, resulting in poor response to anti-VEGF. Besides, photocoagulation was not performed in the early state of both cases. Therefore, it should be noted that photocoagulation is still mandatory for the treatment of retinal NV from tuberculous retinal vasculitis, anti-VEGF only temporarily facilitate vitreous clearing and minimize NV. The appropriate numbers and interval of injection cannot exactly be determined since it should depend on the severity of underlying inflammation and the extent of a retinal vascular shut down. In the future, we suggest performing more controlled studies to observe safety and efficacy of intravitreal anti-VEGF in tuberculous retinal vasculitis.
In conclusion, tuberculous retinal vasculitis causes many complications such as retinal ischemia and NV. The main treatment is ATT with or without corticosteroids. Intravitreal injection of anti-VEGF, as an adjunct to standard anti-tuberculous treatment and retinal photocoagulation, seems to be effective in clearance of vitreous hemorrhage and reduction retinal and optic disc NV.
Acknowledgments
The authors wish to acknowledge Miss Wilawan Sanpan for manuscript preparation before submission.
Conflicts of Interest: Sriboonnark T, None; Boonsopon S, None; Tesavibul N, None; Leeamornsiri S, None; Choopong P, None.
REFERENCES
- 1.Shakarchi FI. Ocular tuberculosis: current perspectives. Clin Ophthalmol. 2015;9:2223–2227. doi: 10.2147/OPTH.S65254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gupta V, Gupta A, Rao NA. Intraocular tuberculosis--an update. Surv Ophthalmol. 2007;52(6):561–587. doi: 10.1016/j.survophthal.2007.08.015. [DOI] [PubMed] [Google Scholar]
- 3.Ang M, Hedayatfar A, Wong W, Chee SP. Duration of anti-tubercular therapy in uveitis associated with latent tuberculosis: a case-control study. Br J Ophthalmol. 2012;96(3):332–336. doi: 10.1136/bjophthalmol-2011-300209. [DOI] [PubMed] [Google Scholar]
- 4.Agrawal R, Gupta B, Gonzalez-Lopez JJ, Rahman F, Phatak S, Triantafyllopoulou I, Addison PKF, Westcott M, Pavesio CE. The role of anti-tubercular therapy in patients with presumed ocular tuberculosis. Ocul Immunol Inflamm. 2015;23(1):40–46. doi: 10.3109/09273948.2014.986584. [DOI] [PubMed] [Google Scholar]
- 5.El-Asrar AM, Al-Kharashi SA. Full panretinal photocoagulation and early vitrectomy improve prognosis of retinal vasculitis associated with tuberculoprotein hypersensitivity (Eales' disease) Br J Ophthalmol. 2002;86(11):1248–1251. doi: 10.1136/bjo.86.11.1248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Al-Mezaine HS, Al-Muammar A, Kangave D, Abu El-Asrar AM. Clinical and optical coherence tomographic findings and outcome of treatment in patients with presumed tuberculous uveitis. Int Ophthalmol. 2008;28(6):413–423. doi: 10.1007/s10792-007-9170-6. [DOI] [PubMed] [Google Scholar]
- 7.Ciulla TA, Rosenfeld PJ. Anti-vascular endothelial growth factor therapy for neovascular ocular diseases other than age-related macular degeneration. Curr Opin Ophthalmol. 2009;20(3):166–174. doi: 10.1097/ICU.0b013e328329d173. [DOI] [PubMed] [Google Scholar]
- 8.Zhou AY, Zhou CJ, Yao J, Quan YL, Ren BC, Wang JM. Panretinal photocoagulation versus panretinal photocoagulation plus intravitreal bevacizumab for high-risk proliferative diabetic retinopathy. Int J Ophthalmol. 2016;9(12):1772–1778. doi: 10.18240/ijo.2016.12.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gunther JB, Altaweel MM. Bevacizumab (Avastin) for the treatment of ocular disease. Surv Ophthalmol. 2009;54(3):372–400. doi: 10.1016/j.survophthal.2009.02.004. [DOI] [PubMed] [Google Scholar]
- 10.Yuksel E, Ozdek S. Unusual presentation of ocular tuberculosis: multiple chorioretinitis, retinal vasculitis and ischaemic central retinal vein occlusion. Clin Exp Optom. 2013;96(4):428–429. doi: 10.1111/cxo.12008. [DOI] [PubMed] [Google Scholar]
- 11.Taguchi M, Sakurai Y, Kanda T, Takeuchi M. Anti-VEGF therapy for central retinal vein occlusion caused by tuberculosis-associated uveitis: a case report. Int Med Case Rep J. 2017;10:139–141. doi: 10.2147/IMCRJ.S128885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gupta V, Shoughy SS, Mahajan S, Khairallah M, Rosenbaum JT, Curi A, Tabbara KF. Clinics of ocular tuberculosis. Ocul Immunol Inflamm. 2015;23(1):14–24. doi: 10.3109/09273948.2014.986582. [DOI] [PubMed] [Google Scholar]
- 13.Talat L, Lightman S, Tomkins-Netzer O. Ischemic retinal vasculitis and its management. J Ophthalmol. 2014;2014:197675. doi: 10.1155/2014/197675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.American Thoracic Society, CDC, Infectious diseases society of america Treatment of tuberculosis. MMWR Recomm Rep. 2003;52(RR-11):1–77. [PubMed] [Google Scholar]
- 15.Mansour AM, Mackensen F, Arevalo JF, Ziemssen F, Mahendradas P, Mehio-Sibai A, Hrisomalos N, Lai TY, Dodwell D, Chan WM, Ness T, Banker AS, Pai SA, Berrocal MH, Tohme R, Heiligenhaus A, Bashshur ZF, Khairallah M, Salem KM, Hrisomalos FN, Wood MH, Heriot W, Adan A, Kumar A, Lim L, Hall A, Becker M. Intravitreal bevacizumab in inflammatory ocular neovascularization. Am J Ophthalmol. 2008;146(3):410–416. doi: 10.1016/j.ajo.2008.05.024. [DOI] [PubMed] [Google Scholar]
- 16.Mansour AM, Mackensen F, Mahendradas P, Khairallah M, Lai TY, Bashshur Z. Five-year visual results of intravitreal bevacizumab in refractory inflammatory ocular neovascularization. Clin Ophthalmol. 2012;6:1233–1237. doi: 10.2147/OPTH.S34294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gulati N, Forooghian F, Lieberman R, Jabs DA. Vascular endothelial growth factor inhibition in uveitis: a systematic review. Br J Ophthalmol. 2011;95(2):162–165. doi: 10.1136/bjo.2009.177279. [DOI] [PubMed] [Google Scholar]
- 18.Ishijima K, Namba K, Ohno S, Mochizuki K, Ishida S. Intravitreal injection of bevacizumab in a case of occlusive retinal vasculitis accompanied by syphilitic intraocular inflammation. Case Rep Ophthalmol. 2012;3(3):434–437. doi: 10.1159/000346046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wong R, Gupta B, Stanford MR, Laidlaw DA. Intravitreal bevacizumab to facilitate vitrectomy in idiopathic ischaemic retinal vasculitis. Int Ophthalmol. 2010;30(4):415–419. doi: 10.1007/s10792-009-9329-4. [DOI] [PubMed] [Google Scholar]