Abstract
Objective
Lister's tubercle is used as a standard anatomical landmark in hand surgery and arthroscopy procedures. In this study, we aimed to evaluate and propose a classification for anatomical variants of Lister's tubercle.
Materials and Methods
Between September 2011 and July 2014, 360 MRI examinations for wrists performed using 1.5T scanners in a single institution were retrospectively evaluated. The prevalence of anatomical variants of Lister's tubercle based on the heights and morphology of its radial and ulnar peaks was assessed. These were classified into three distinct types: radial peak larger than ulnar peak (Type 1), similar radial and ulnar peaks (Type 2) and ulnar peak larger than radial peak (Type 3). Each type was further divided into 2 subtypes (A and B) based on the morphology of the peaks.
Results
The proportions of Type 1, Type 2, and Type 3 variants in the study population were 69.2, 21.4, and 9.5%, respectively. For the subtypes, the Type 1A variant was the most common (41.4%) and conformed to the classical appearance of Lister's tubercle; whereas, Type 3A and 3B variants were rare configurations (6.4% and 3.1%, respectively) wherein the extensor pollicis longus tendon coursed along the radial aspect of Lister's tubercle.
Conclusion
Anatomical variations of Lister's tubercle have potential clinical implications for certain pathological conditions and pre-procedural planning. The proposed classification system facilitates a better understanding of these anatomical variations and easier identification of at-risk and rare variants.
Keywords: Lister's tubercle, Extensor pollicis longus, MR imaging, Anatomy
INTRODUCTION
The prominent bony tubercle over the dorsal aspect of the distal radius, known as Lister's tubercle, functions as a pulley for the extensor pollicis longus (EPL) tendon before the tendon pivots and turns obliquely to insert onto the distal phalanx of the thumb (1). As a palpable structure, Lister's tubercle has been used as an anatomical landmark for localizing the first dorsal extensor compartment (2), posterior interosseous nerve (3), superficial branch of the radial nerve (4) and dorsal radiotriquetral ligament (5). It is also used as a surgical landmark in wrist arthrography injections and arthroscopy (6,7), dorsal wrist capsulotomy (8), hand microsurgery (9,10,11), radioscapholunate arthrodesis (11), Kirschner wire placement, and internal fixation of Colles fractures (12,13).
Because of its proximity to carpal structures and overlapping bony densities, conventional radiology does not provide a detailed outline of Lister's tubercle or its relationship to the adjacent tendon structures.
Despite the importance of Lister's tubercle in modern surgical procedures and its close spatial relationship with the EPL tendon, few reports have described the variations of Lister's tubercle and its relationship with the EPL tendon. Pichler et al. (14) reported the height variations of Lister's tubercle on computed tomography (CT) and Ağır et al. (15) described its variable location along the dorsal radius using cadaveric radii. To our best knowledge, currently, there is no literature describing variations in anatomical morphology of Lister's tubercle and its relationship with the course of the EPL tendon in the third dorsal extensor compartment.
In this study, we aimed to evaluate MR wrist studies to determine the incidence and describe the morphological variants of Lister's tubercle. We proposed a classification system of these variants and its relationship with the EPL tendon, along with a review of existing literature with respect to potential relevance in clinical conditions and surgical procedures.
MATERIALS AND METHODS
Institution Review Board
This was a retrospective study of all MRI wrist studies performed in the radiology department from a single institution over a 3 year period between September 2011 and July 2014. Institutional Review Board waiver was obtained prior to the study.
Patients
The cases were collated through a search of the hospital's radiology information system (Carestream Health Vue RIS/PACS). A total of 380 MRI wrist studies for various clinical indications were performed during the study period. All MRI wrist studies performed on patients aged ≥ 18 years were included in the study. Exclusion criteria were: evidence of acute or prior fracture of the distal radius near or at Lister's tubercle, acute osteomyelitis, prior surgery of the distal radius, underlying bone marrow disorder, and suboptimal studies due to technical factors. In patients who underwent bilateral wrist MRI, only the left wrist MRI was included for assessment to optimize representation of the number of left and right wrists included in the study population.
A total of 360 MRI wrist studies in 360 patients were included in the final assessment, of which, 174 were left wrist and 186 were right wrist MRI studies in 284 men and 76 women, with a mean age of 32.1 years (age range, 18–88 years). Clinical indications for MRI included suspected triangular fibrocartilage complex tear or injury (39.7%), wrist pain (24.7%), scaphoid fracture (8.0%), scapholunate instability or ligament injury (6.9%), and other miscellaneous conditions (19.6%).
MRI Examination
The MRI studies were performed on two identical 1.5T MR scanners using 16-channel wrist coils (Magnetom Aera; Siemens Healthcare, Erlangen, Germany). All patients were positioned supine in the MRI scanner with the wrist held at the patient's side in pronation. Axial intermediateweighted fast spin echo images were performed as part of the MRI examinations and used for subsequent evaluation in this study. The axial images of the wrist were acquired perpendicular to the longitudinal length of the radius. MRI scan parameters were as follows: repetition time (TR) 3000 ms, echo time (TE) 30 ms, echo train length (ETL) 6, flip angle 150°, matrix 512 × 320, slice thickness 3 mm, no interslice gap, and receiver bandwidth 120 Hz/pixel.
Image Analysis
The axial MRI images were evaluated for morphological anatomical variants of Lister's tubercle as well as their relationship with the course of the EPL tendon. Two observers (with 14 years and 2 years of experience in musculoskeletal radiology) initially performed the evaluations separately and then in consensus.
Lister's tubercle was comprised of two distinct bony peaks: the radial and ulnar peaks. Based on observational analysis of these peaks, a classification system was formulated following several iterations of refinement and fine-tuning. We described three primary variants of Lister's tubercle based on the relative sizes of the radial and ulnar peaks, each with two sub-classifications based on the morphology of these peaks.
RESULTS
Several anatomical variants of Lister's tubercle were identified in this study. A total of 360 MR wrists were evaluated, which included 284 MR wrists from male patients (139 left wrist and 145 right wrist studies) and 76 MR wrists from female patients (35 left wrist and 41 right wrist studies). Differences in variations between sexes were not evaluated due to the smaller number of female patients in our study. The findings and prevalence of each anatomical variant are summarised in Table 1.
Table 1. Distribution of Morphological Variants of Lister's Tubercle in Study Population.
| Morphology | Number | Incidence (%) |
|---|---|---|
| Type 1 | 249 | 69.2 |
| Type 1A | 149 | 41.4 |
| Type 1B | 100 | 27.8 |
| Type 2 | 77 | 21.4 |
| Type 2A | 40 | 11.1 |
| Type 2B | 37 | 10.3 |
| Type 3 | 34 | 9.4 |
| Type 3A | 23 | 6.4 |
| Type 3B | 11 | 3.1 |
| Total | 360 | 100.0 |
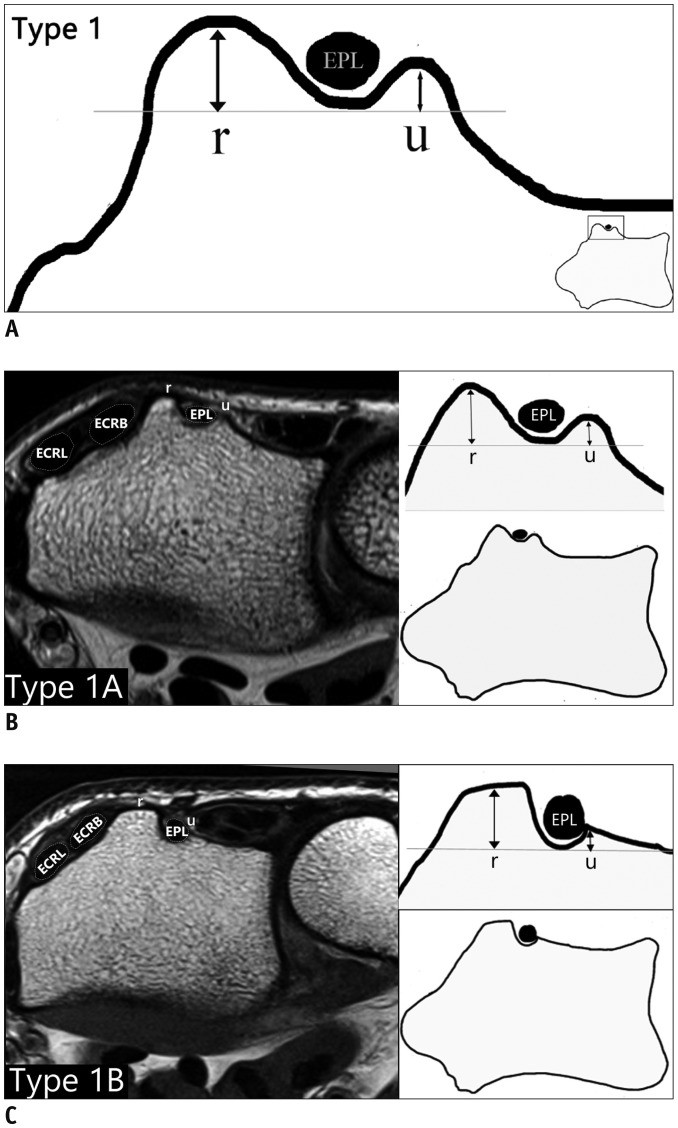
The Type 1 variant of Lister's tubercle describes a configuration wherein the radial peak is larger than the ulnar peak (Fig. 1A). The EPL tendon courses between the radial and ulnar peaks. This variant was found in 69.2% of all cases and was further classified into Types 1A and 1B subtypes based on the morphology of the peaks.
Fig. 1. Type 1 variant on diagrams and axial MR images.
A. Schematic of Type 1 variant. B. Type 1A variant (classical configuration of Lister's tubercle). C. Type 1B variant wherein radial (r) peak is dominant with box-like configuration and ulnar peak (u) is small. ECRB = extensor carpi radialis brevis, ECRL = extensor carpi radialis longus, EPL = extensor pollicis longus
The Type 1A variant represents the classical appearance of Lister's tubercle, wherein both radial and ulnar peaks are discrete and well-formed, with the radial peak having a triangular configuration (Fig. 1B). The Type 1B variant comprises a dominant radial peak with a broad box-like configuration and a plateaued top. Its ulnar peak is small and rudimentary, defined as such when the peak surrounds or encases less than one half of the height of the EPL tendon (Fig. 1C). In this configuration, the resultant groove for the EPL tendon is relatively deep. The Type 1A configuration was the most common variant with an overall incidence of 41.4%; whereas, the Type 1B variant showed an overall incidence of 27.8%.
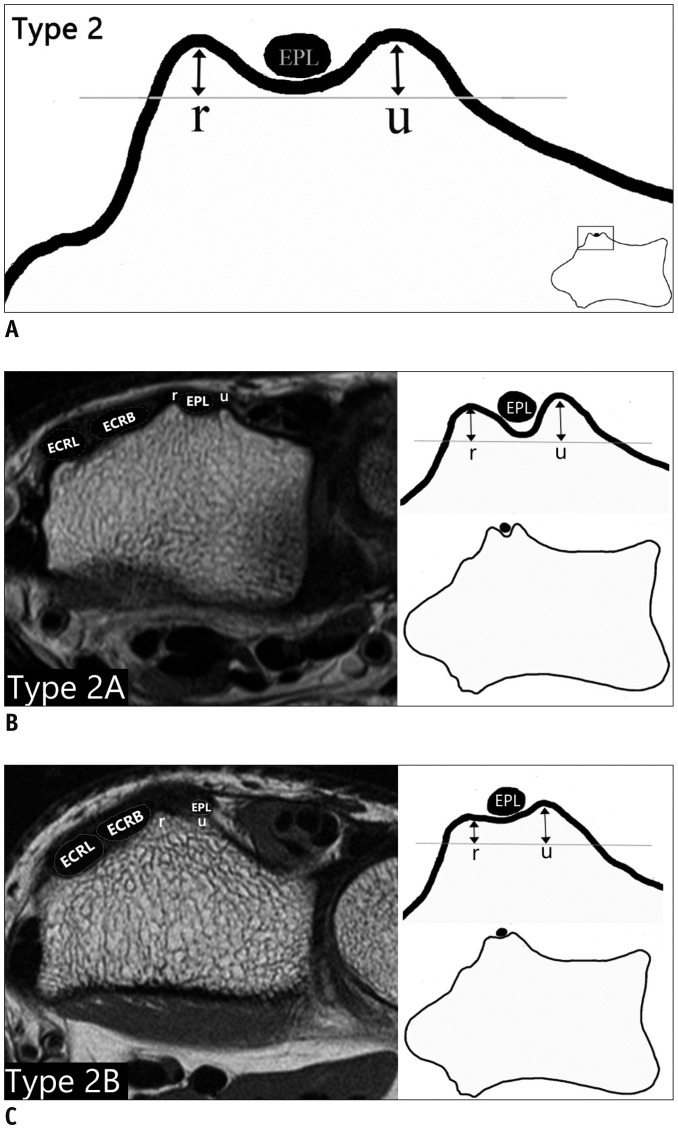
In the Type 2 variant, the radial and ulnar peaks of Lister's tubercle are of similar or approximately equal heights and sizes (Fig. 2A). This variant was found in 21.4% of all cases and might be further divided into Types 2A and 2B based on the morphology of the peaks.
Fig. 2. Type 2 variant on diagrams and axial MR images.
A. Schematic of Type 2 variant. B. Type 2A variant wherein both radial (r) and ulnar (u) peaks are discrete and equal in height. C. Type 2B variant wherein both radial (r) and ulnar (u) peaks are equal in height but rudimentary and difficult to visualize.
In the Type 2A variant, both radial and ulnar peaks are discrete and approximately equal in size to the EPL tendon situated along the groove formed between these two peaks (Fig. 2B). This differs from the Type 2B variant wherein both radial and ulnar peaks are equal in size but small and not well formed. In this latter variant, both peaks may be found elevated on a broad bony shelf, between which the EPL tendon courses (Fig. 2C). Both Types 2A and 2B variants were uncommon and found in 11.1% and 10.3% of all cases, respectively.
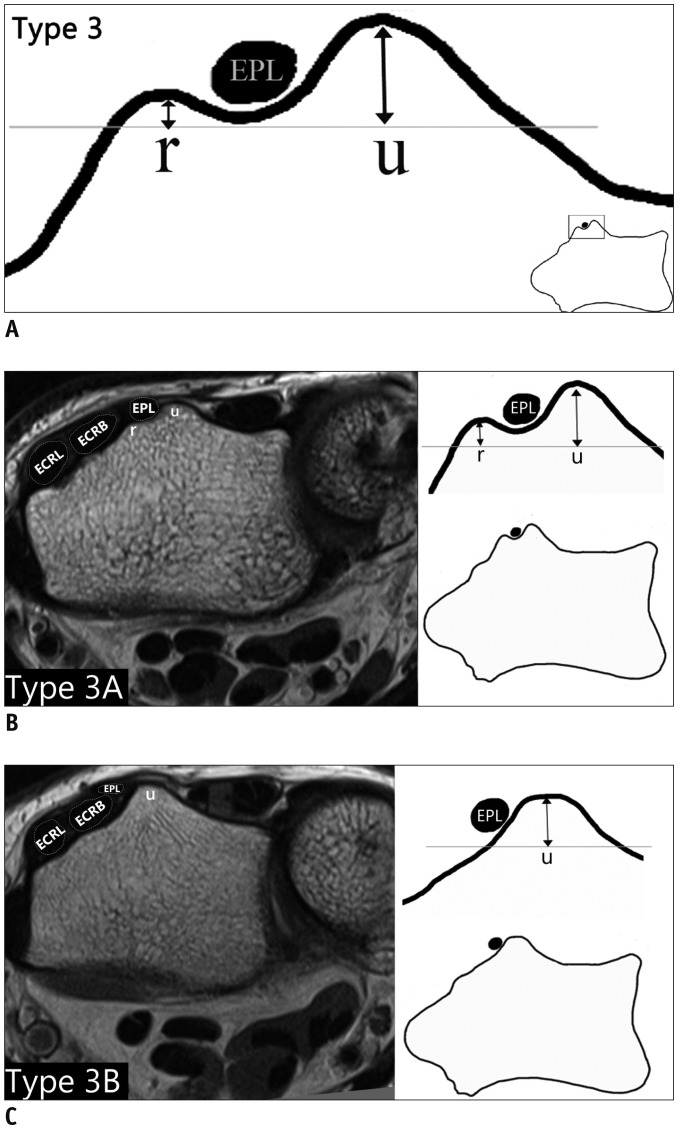
In the Type 3 variant, the radial peak of Lister's tubercle is smaller than its ulnar counterpart (Fig. 3A). This variant was uncommon with an incidence of 9.5%, and could be sub-classified into Types 3A and 3B variants based on the morphology of the peaks.
Fig. 3. Type 3 variant on diagrams and axial MR images.
A. Schematic of Type 3 variant. B. Type 3A variant wherein the ulnar (u) peak is dominant and taller than radial (r) peak. C. Type 3B variant wherein ulnar (u) peak is dominant with absent radial (r) peak. In these variants, EPL tendon appears to cross radial to palpated Lister's tubercle.
In the Type 3A variant, the ulnar peak is higher and larger with a small yet distinct radial peak (Fig. 3B). In contrast, the Type 3B variant shows a broad dominant ulnar peak without an appreciable radial peak (Fig. 3C). In both Types 3A and 3B variants, the EPL tendon courses between the radial and ulnar peaks, and as the dominant ulnar peak forms the palpable bony prominence of Lister's tubercle, the EPL tendon appears to cross radial to the clinically palpated Lister's tubercle. The Type 3A variant was rare in our study population with an incidence of 6.4%, while the Type 3B variant was the rarest configuration with an overall incidence of 3.1%.
DISCUSSION
The bony dorsal tubercle along the distal radius known as Lister's tubercle has not been clearly described. The earliest reference anatomy textbooks (16,17) described Lister's tubercle as the bony landmark wherein the EPL tendon crosses to the ulna or over it.
Ağır et al. (15) studied 27 cadaver radii and showed that the position of Lister's tubercle along the dorsal surface of the distal radius varies between the radial styloid process and ulnar notch. Their study suggested possible implications in volar plate fixation as dorsal screw penetration may occur in some variants. In our study, we showed that differences in Lister's tubercle were not limited to its position but to its morphology as well.
Clement et al. (18) performed a morphometric analysis of Lister's tubercle using 100 cadaver radii by measuring the height of Lister's tubercle and depth of the EPL groove. The increased height of Lister's tubercle and a deep EPL groove in certain individuals could potentially obscure the field of view of surgeons during volar plate fixation. Greater differences in heights of the radial and ulnar peaks are possibly associated with an increase in the perceived height of Lister's tubercle. These characteristics are seen in Type 1B (with a box-like radial peak and rudimentary ulnar peak) and Type 3B (with non-existent radial peak and dominant ulnar peak) variants. However, further studies on the two groups are required to confirm this hypothesis.
Pichler et al. (14) were the first to analyse the size of Lister's tubercle and the length of the EPL groove through CT and three-dimensional (3D) analysis of 30 forearms; their study results indicated considerable variation. The study likewise suggested that increased height of Lister's tubercle and a deep EPL groove may increase the risk of dorsal screw penetration and lead to EPL rupture.
Extensor pollicis longus tendon rupture after distal radius fracture is a rare complication following volar pate fixation, occurring in 0.07l–0.88% of cases and usually presenting within 3 months after injury (9). Several studies (19,20,21,22,23,24) have identified the level of Lister's tubercle as the site of EPL rupture, which may go unrecognized (21). The proposed etiologies include the marginal blood supply to Lister's tubercle (19,22,23) and dorsal screw penetration from volar plate fixation (20, 21). The EPL is poorly vascularized at this segment (24,25), withstanding intrinsic high tensile stresses as the tendon angulates radially towards the thumb. Ferreres el al. (26) suggested that hyperextension of the wrist impacts the base of the third metacarpal against Lister's tubercle, and can result in EPL rupture at this level.
Identifying anatomical variants of Lister's tubercle has potential clinical significance in planning a surgical strategy for volar plate fixation. Benson et al. (19) evaluated commercially available volar plates and reported that the screw holes in some models direct the drill bit into the third extensor compartment, which could be a factor in dorsal cortical penetration of the distal radius during volar plate fixation. Using our proposed classification system, at-risk variants include a deep EPL groove resulting in decreased drilling depth (Type 2A variant), as well as dominant radial and ulnar peaks that may obscure fluoroscopic visualisation in the lateral projection (Types 1B and 3B variants). If volar plating is to be considered, a 3D CT study of the wrist might be considered to identify at-risk variants. Our classification system is applicable to CT as well as MR imaging. These may lead to shorter screws for use in specific holes (19); and intra-operative pronation views (20), or dorsal tangential view (21) to visualise the ulnar aspect of the dorsal cortex and avoid inadvertent penetration.
The clinical significance of understanding anatomical variants of Lister's tubercle is also applicable in wrist injections and arthroscopic procedures. Corticosteroid injection for de Quervain's disease is a common nonoperative treatment with a high success rate (27). Lister's tubercle can be used as a bony landmark together with the scaphoid tubercle to guide injection into the first dorsal compartment (2). However, in Type 3 variants wherein the palpated bony tubercle is the ulnar peak and the third dorsal compartment lies radially, the marking of the first dorsal compartment may be more ulnar than its actual location. In the radiocarpal joint, the injection site for MR arthrography and the introduction site for insertion of the 3-4 portal for arthroscopy are localised to just distal to Lister's tubercle (6,7). The Type 2B variant has indistinct peaks with the EPL coursing over it, making it difficult to palpate the tubercle and likely to cause difficulty in precise injection and portal insertion.
In our study, we identified a small percentage of variants (9.5%) wherein the ulnar peak is dominant and the EPL tendon crosses radial to the palpable Lister's tubercle (Types 3A and 3B). It is likely that this variant was represented previously in a case report by Nishijo et al. (28), who described intra-operative findings of the EPL coursing radial to Lister's tubercle in a young Asian female. The patient was initially diagnosed with de Quervain's tenosynovitis with an inflamed EPL tendon. A CT of the wrist also showed a shallow Lister's tubercle (corresponding to Type 3B variant based on our classification). As such, the identification of Type 3 variants, wherein the EPL appears to course radial to the palpated Lister's tubercle may also influence the clinical diagnosis. The authors also showed a possible association with a duplicated EPL tendon; however, this was not observed in our study population.
We also attempted to apply our classification system of Lister's tubercle in other studies. De Maeseneer et al. (29) retrospectively studied EPL tears using ultrasound and correlated the findings with cadaveric dissections; the sonographic and cadaveric images of Lister's tubercle demonstrated a Type 2B configuration with the EPL tendon coursing over the top of the tubercle. Another case report by Perugia et al. (30) described MR imaging in a patient with a sports-related EPL rupture. Their findings were indicative of a Lister's tubercle divided into two similar sized plateaus at its distal aspect, corresponding to a Type 2 configuration. These two studies collectively suggest that the Type 2 configuration of Lister's tubercle may present an increased risk of EPL rupture due to inherent microinstability, potentially predisposing to chronic inflammation. However, further studies are needed to evaluate this hypothesis.
Although Clement et al. (18) and Pichler et al. (14) highlighted the variations of Lister's tubercle on cadaveric radii and CT respectively, the need for exact measurements of Lister's height or EPL groove may be too laborious for routine clinical use by reporting radiologists in a busy institution; whereas, an easy qualitative classification would be more practical. MRI is superior to CT in the assessment of tendons and soft tissue structures around the wrist without the use of ionizing radiation. The requirement for dedicated CT studies with higher spatial resolution to increase measurement precision may not be feasible or necessary.
Therefore, we proposed a new anatomical classification system for Lister's tubercle based on qualitative assessment of the size and morphology of its radial and ulnar peaks. This classification is both simple to remember and easy to apply, eliminating the need for point measurements and can be readily applied to both CT and MR images.
Our study had a few limitations. This was a retrospective analysis of MRIs performed in patients presenting with various wrist complaints and might not be a true representative population. However, we included as many patients as possible and excluded patients with pathology adjacent to Lister's tubercle from the analysis. As the primary objective of the study was to develop an anatomical classification system, it was derived following several iterations by both observers largely working together and as such inter-observer agreement of the proposed classification was not measured. The inter-observer agreement should be assessed in future studies. In addition, imaging-anatomic correlation of the Lister's tubercle variants were not available, but no significant discrepancy is likely.
In conclusion, this study, we identified and described several anatomical variations of Lister's tubercle. The study may have clinical implications for certain pathological conditions and pre-procedural planning. The proposed classification system allows for an understanding of these anatomical variations, and easier identification of at-risk and rare variants.
References
- 1.Saffar P, Fakhoury B. [Secondary repair of the extensor pollicis longus] Ann Chir Main. 1987;6:225–229. doi: 10.1016/s0753-9053(87)80064-9. [DOI] [PubMed] [Google Scholar]
- 2.Hazani R, Engineer NJ, Cooney D, Wilhelmi BJ. Anatomic landmarks for the first dorsal compartment. Eplasty. 2008;8:e53. [PMC free article] [PubMed] [Google Scholar]
- 3.Smith J, Rizzo M, Finnoff JT, Sayeed YA, Michaud J, Martinoli C. Sonographic appearance of the posterior interosseous nerve at the wrist. J Ultrasound Med. 2011;30:1233–1239. doi: 10.7863/jum.2011.30.9.1233. [DOI] [PubMed] [Google Scholar]
- 4.Ikiz ZA, Uçerler H. Anatomic characteristics and clinical importance of the superficial branch of the radial nerve. Surg Radiol Anat. 2004;26:453–458. doi: 10.1007/s00276-004-0256-9. [DOI] [PubMed] [Google Scholar]
- 5.Smith DK. Dorsal carpal ligaments of the wrist: normal appearance on multiplanar reconstructions of threedimensional Fourier transform MR imaging. AJR Am J Roentgenol. 1993;161:119–125. doi: 10.2214/ajr.161.1.8517289. [DOI] [PubMed] [Google Scholar]
- 6.Lohman M, Vasenius J, Nieminen O. Ultrasound guidance for puncture and injection in the radiocarpal joint. Acta Radiol. 2007;48:744–747. doi: 10.1080/02841850701422146. [DOI] [PubMed] [Google Scholar]
- 7.Slutsky DJ. Wrist arthroscopy. In: Wolfe SW, Hotchkiss RN, Pederson WC, Kozin SH, editors. Green's operative hand surgery. 6th ed. Philadelphia: Elsevier; 2011. pp. 709–741. [Google Scholar]
- 8.Berger RA. A method of defining palpable landmarks for the ligament-splitting dorsal wrist capsulotomy. J Hand Surg Am. 2007;32:1291–1295. doi: 10.1016/j.jhsa.2007.07.023. [DOI] [PubMed] [Google Scholar]
- 9.Barbieri CH, Mazzer N. Triradiate skin incision for dorsal approach to the wrist. J Hand Surg Br. 1996;21:21–23. doi: 10.1016/s0266-7681(96)80006-4. [DOI] [PubMed] [Google Scholar]
- 10.Samarakoon LB, Lakmal KC, Thillainathan S, Bataduwaarachchi VR, Anthony DJ, Jayasekara RW. Anatomical relations of the superficial sensory branches of the radial nerve: a cadaveric study with clinical implications. Patient Saf Surg. 2011;5:28. doi: 10.1186/1754-9493-5-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Galvis EJ, Kumar KK, Özyurekoglu T. Radioscapholunate arthrodesis using low-profile dorsal pi plate. Tech Hand Up Extrem Surg. 2013;17:80–83. doi: 10.1097/BTH.0b013e318280e9cc. [DOI] [PubMed] [Google Scholar]
- 12.Espen D. [Fixation of fractures of the distal radius using the “nail-plate”] Oper Orthop Traumatol. 2009;21:459–471. doi: 10.1007/s00064-009-1912-3. [DOI] [PubMed] [Google Scholar]
- 13.Hochwald NL, Levine R, Tornetta P., 3rd The risks of Kirschner wire placement in the distal radius: a comparison of techniques. J Hand Surg Am. 1997;22:580–584. doi: 10.1016/S0363-5023(97)80112-8. [DOI] [PubMed] [Google Scholar]
- 14.Pichler W, Windisch G, Schaffler G, Rienmüller R, Grechenig W. Computer tomography aided 3D analysis of the distal dorsal radius surface and the effects on volar plate osteosynthesis. J Hand Surg Eur Vol. 2009;34:598–602. doi: 10.1177/1753193409101471. [DOI] [PubMed] [Google Scholar]
- 15.Ağr I, Aytekin MN, Küçükdurmaz F, Gökhan S, Cavus¸ UY. Anatomical localization of Lister’s tubercle and its clinical and surgical importance. Open Orthop J. 2014;8:74–77. doi: 10.2174/1874325001408010074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kaplan EB. Anatomical variations of the forearm and hand. In: Tubiana R, editor. The hand. Philadelphia: W. B. Saunders; 1981. pp. 361–374. [Google Scholar]
- 17.Valentin P. Extrinsic muscles of the hand and wrist: an introduction. In: Tubiana R, editor. The hand. Philadelphia: WB Saunders; 1981. p. 243. [Google Scholar]
- 18.Clement H, Pichler W, Nelson D, Hausleitner L, Tesch NP, Grechenig W. Morphometric analysis of Lister’s tubercle and its consequences on volar plate fixation of distal radius fractures. J Hand Surg Am. 2008;33:1716–1719. doi: 10.1016/j.jhsa.2008.08.012. [DOI] [PubMed] [Google Scholar]
- 19.Benson EC, DeCarvalho A, Mikola EA, Veitch JM, Moneim MS. Two potential causes of EPL rupture after distal radius volar plate fixation. Clin Orthop Relat Res. 2006;451:218–222. doi: 10.1097/01.blo.0000223998.02765.0d. [DOI] [PubMed] [Google Scholar]
- 20.Maschke SD, Evans PJ, Schub D, Drake R, Lawton JN. Radiographic evaluation of dorsal screw penetration after volar fixed-angle plating of the distal radius: a cadaveric study. Hand (N Y) 2007;2:144–150. doi: 10.1007/s11552-007-9038-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ozer K, Toker S. Dorsal tangential view of the wrist to detect screw penetration to the dorsal cortex of the distal radius after volar fixed-angle plating. Hand (N Y) 2011;6:190–193. doi: 10.1007/s11552-010-9316-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lamas C, Llusà M, Méndez A, Proubasta I, Carrera A, Forcada P. Intraosseous vascularity of the distal radius: anatomy and clinical implications in distal radius fractures. Hand (N Y) 2009;4:418–423. doi: 10.1007/s11552-009-9204-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shima H, Ohno K, Michi K, Egawa K, Takiguchi R. An anatomical study on the forearm vascular system. J Craniomaxillofac Surg. 1996;24:293–299. doi: 10.1016/s1010-5182(96)80062-x. [DOI] [PubMed] [Google Scholar]
- 24.Lanzetta M, Howard M, Conolly WB. Post-traumatic triggering of extensor pollicis longus at the dorsal radial tubercle. J Hand Surg Br. 1995;20:398–401. doi: 10.1016/s0266-7681(05)80102-0. [DOI] [PubMed] [Google Scholar]
- 25.Stahl S, Wolff TW. Delayed rupture of the extensor pollicis longus tendon after nonunion of a fracture of the dorsal radial tubercle. J Hand Surg Am. 1988;13:338–341. doi: 10.1016/s0363-5023(88)80004-2. [DOI] [PubMed] [Google Scholar]
- 26.Ferreres A, Llusá M, García-Elías M, Lluch A. A possible mechanism of direct injury to the EPL tendon at Lister's tubercle during falls with the wrist fully extended. J Hand Surg Eur Vol. 2008;33:149–151. doi: 10.1177/1753193407087575. [DOI] [PubMed] [Google Scholar]
- 27.Rowland P, Phelan N, Gardiner S, Linton KN, Galvin R. The effectiveness of corticosteroid injection for de Quervain’s stenosing tenosynovitis (DQST): A Systematic Review and meta-analysis. Open Orthop J. 2015;9:437–444. doi: 10.2174/1874325001509010437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nishijo K, Kotani H, Miki T, Senzoku F, Ueo T. Unusual course of the extensor pollicis longus tendon associated with tenosynovitis, presenting as de Quervain disease--a case report. Acta Orthop Scand. 2000;71:426–428. doi: 10.1080/000164700317393484. [DOI] [PubMed] [Google Scholar]
- 29.De Maeseneer M, Marcelis S, Osteaux M, Jager T, Machiels F, Van Roy P. Sonography of a rupture of the tendon of the extensor pollicis longus muscle: initial clinical experience and correlation with findings at cadaveric dissection. AJR Am J Roentgenol. 2005;184:175–179. doi: 10.2214/ajr.184.1.01840175. [DOI] [PubMed] [Google Scholar]
- 30.Perugia D, Ciurluini M, Ferretti A. Spontaneous rupture of the extensor pollicis longus tendon in a young goalkeeper: a case report. Scand J Med Sci Sports. 2009;19:257–259. doi: 10.1111/j.1600-0838.2008.00779.x. [DOI] [PubMed] [Google Scholar]