Highlights
This study contributes to a European evidence base for effective interventions for homeless people.
It is the first RCT conducted in Dutch shelter services; this is uncommon outside the United States.
In this sample, recurrent homelessness was rare 9 months after moving from a shelter to housing.
Beneficial effects of CTI on mental health seem to be independent of health care system or context.
Keywords: Homelessness, Intervention, Housing, Family support, Psychological distress, Randomized controlled trial
Abstract
To help create an evidence base in Europe for effective interventions that improve the well‐being of homeless people, we tested whether critical time intervention (CTI), a time‐limited intervention developed to support vulnerable people during times of transition, is effective outside the United States. For this multicenter, parallel‐group randomized controlled trial, 183 adults who were moving from shelters in the Netherlands to supported or independent housing were allocated to CTI or care‐as‐usual. The primary outcome was number of days rehoused, which was assessed by interviewing participants four times during a 9‐month follow‐up. Outcomes were analyzed with three‐level mixed‐effects models. The primary outcome did not differ between groups. CTI had a significant effect on family support and, for people experiencing less social support, psychological distress. Groups did not differ significantly on social support, fulfillment of care needs, quality of life, self‐esteem, excessive alcohol use, or cannabis use. Because few participants were homeless at 9 months, more research is needed to establish whether CTI can prevent long‐term recurrent homelessness. Given recent emphasis on informal support in public services and positive effects of CTI on family support and psychological distress, CTI is a fitting intervention for Dutch shelter services.
Introduction
Making the transition from a homeless shelter to community living can be challenging. A study among first‐time New York City shelter residents showed that 24% of those who obtained housing experienced recurrent homelessness during the 18‐month follow‐up period (McQuistion, Gorroochurn, Hsu & Caton, 2014). Because shelter services are terminated and relationships with fellow residents difficult to maintain, people experience discontinuity of support after shelter discharge (Herman, Conover, Felix, Nakagawa & Mills, 2007). Having less informal support is associated with a higher risk of becoming homeless (Kingree, Stephens, Braithwaite & Griffin, 1999) and longer duration of homelessness (Caton et al., 2005). Because individuals who experience one or two short homeless episodes (of less than a year) have better clinical outcomes than individuals experiencing longer or multiple episodes (Fazel, Geddes & Kushel, 2014), it is important to prevent recurrent homelessness.
Critical time intervention (CTI) is a time‐limited, strength‐based intervention for vulnerable people, which bridges the gap between services during times of transition. The CTI worker provides practical and emotional support and helps to develop and strengthen links with community resources, creating a network that will continue to provide support long after CTI has ended. In the United States, CTI has been found effective in preventing recurrent homelessness and rehospitalization and reducing psychiatric symptoms and substance use among people at risk of homelessness (Herman et al., 2011; Kasprow & Rosenheck, 2007; Susser et al., 1997). These previous studies added CTI to usual services, which generally consisted of discharge planning and referral services and access to a range of community‐based services, but did not compare its effectiveness to other case management approaches. Furthermore, little is known about the effectiveness of this intervention—as well as of other case management models implemented in European shelter services—outside the United States (De Vet et al., 2013), where health care systems and social context may differ substantially. By evaluating CTI in a randomized controlled trial in the Netherlands, we may show that effects are independent of a particular health care system or social context. We might expect findings here to be different from previous studies, because shelter services during and after discharge are usually provided in the Netherlands with a higher intensity than in the United States (Herman et al., 2007). In the experimental condition of the present study, usual services were exchanged for CTI instead of adding CTI to those services. Many of the control group participants received some type of case management services after discharge. Nonetheless, potential benefits are to be expected, because CTI has a systematic approach to providing support. The CTI model focuses particularly on strengthening the social and professional support system and, at the same time, provides clients with the guidance necessary to navigate the complex system of social services and health care in the Netherlands. The time‐limited nature of the intervention, which was terminated at 9 months in the present study, gives the CTI workers and clients a sense of urgency that helps them to focus on those life areas most important for clients’ long‐term stability. Furthermore, CTI helps to alleviate the stress that is coupled with a transition such as moving from a shelter to community living, because clients receive practical support with a very high intensity during the first phase of the intervention, which lasted until 3 months after discharge.
Based on the findings of previous CTI studies and the intervention's theoretical mechanism of effect, our hypotheses are that: (a) CTI is more effective than care‐as‐usual for clients moving from shelters to supported or independent housing with regard to increasing the number of days rehoused (primary outcome); (b) CTI improves family support, social support, and fulfillment of care needs (intermediate outcomes); and (c) CTI has a positive effect on quality of life, psychological distress, self‐esteem, excessive alcohol use, and cannabis use (secondary outcomes).
Method
Design and Participants
This multicenter, parallel‐group study was conducted by the Netherlands Center for Social Care Research (Impuls) and is registered with the Netherlands Trial Registry (NTR3425). The trial complied with the approval criteria of an accredited Medical Research Ethics Committee (aMREC) and was exempted from formal review by the local aMREC (CMO Region Arnhem‐Nijmegen: registration number 2010/247). Between December 1, 2010 and December 1, 2012 (the scheduled date of closure), 183 clients were recruited in 18 shelters of nine shelter organizations that participated in the Academic Collaborative Center for Shelter and Recovery in 2009. Shelters were selected for recruitment based on their even distribution over the Netherlands and provision of residential services (see Appendix S1 available online).
One staff member at each shelter assessed clients. Clients were eligible if they (a) were aged 18 years or over, (b) had stayed at the shelter for <14 months, (c) knew when they were going to exit the shelter or had received priority status for social housing, and (d) were moving to housing for which they would have to pay rent without supervision or daily supportive services. Clients were excluded if they were moving to an area where none of the participating organizations provided services.
Randomization and Masking
Randomization was stratified by shelter and balanced within blocks of four. A list of random numbers was computer generated by a member of the research team (RV) and concealed in a secure digital file until assignment. Shelter staff supplied contact details of eligible clients, with their consent, to the research team. The research assistant who enrolled clients into the study scheduled an appointment for the baseline interview. Clients, shelter staff, and this research assistant did not have any foreknowledge of condition assignment. After the baseline interview, one of the researchers (RV or DL) ascertained the allocated condition and notified shelter staff. Clients provided informed consent before the baseline interview and remained blind until they met their CTI worker or case manager for the first time. Condition assignment was withheld from data collectors. However, some of them did become aware of the allocated condition during follow‐up, because participants would sometimes spontaneously disclose this information during an interview.
Critical Time Intervention
Participants allocated to the experimental condition received CTI, which was delivered in three phases of 3 months: transition to the community (phase 1), try‐out (phase 2), and transfer of care (phase 3). The intervention's components are described elsewhere (Lako et al., 2013) and summarized in Table 1. In each organization, two or three case managers were drawn from community service teams to deliver the intervention. These case managers needed to have a bachelor's degree in social work or a related field in order to qualify. They completed three 1‐day training sessions before the start of the trial, provided by the research team (JW and RV) and experienced trainers, to become familiar with the intervention's theoretical and procedural aspects and to acquire essential skills for CTI practice. With the goal of enhancing model fidelity, a community of practice was created consisting of CTI workers, researchers, trainers, and experts to gain and share knowledge and experiences during half‐day follow‐up training sessions—(bi)monthly during the first year and quarterly during the second year of study. Furthermore, CTI workers had biweekly face‐to‐face supervision with an internal coach, who was responsible for ensuring sufficient organizational support and monitoring model fidelity. Each participating organization selected one of their staff members to become the internal coach based on a profile of the coach's role and tasks, which was provided by the research team. Coaches received a 1‐day training session at the start of the trial and four half‐day follow‐up training sessions during the study period. The recommended caseload for a CTI worker was 16 clients, considering that these clients would be distributed evenly across the different phases of the intervention.
Table 1.
Components of critical time intervention (CTI) in each phase
| Phase | Pre‐CTI | Phase 1: Transition to the community | Phase 2: Try‐out | Phase 3: Transfer of care |
|---|---|---|---|---|
| Timing | Between assignment and discharge | Between discharge and 3 months after discharge | Between 3 and 6 months after discharge | Between 6 and 9 months after discharge |
| Responsibilities of CTI worker | Build a relationship |
|
|
|
| Materialsa |
Required:
Optional:
|
Required:
|
Required:
Optional: Strengths assessment |
Required:
|
| Intensity | At least two or three meetings with client before discharge, with no more than a month between each meeting (10 h in total) | Average of 3 h per week (36 h in total) | Average of 2 h per week (24 h in total) | Average of 30 min to 1 h per week (6–12 h in total) |
Because the degree of fidelity to the CTI model (i.e., whether the intervention was delivered as intended) may influence its effectiveness (Bond, Evans, Salyers, Williams & Kim, 2000), we conducted a fidelity assessment for a representative subsample of 35 cases randomly allocated to CTI (de Vet et al., 2017). The fidelity of the intervention was assessed using the CTI fidelity scale, a quantitative tool developed by Conover and Herman (2007). The items of the CTI fidelity scale are rated on a 5‐point scale ranging from 1 (not implemented) to 5 (ideally implemented). The overall fidelity score, which was computed by combining item‐level ratings (Conover, 2012), was based on compliance fidelity, which is the degree to which providers implemented the key elements of the CTI model (eight items), and chart quality, which measures how well the intervention was documented (four items). The intervention in this study obtained an overall fidelity score of 3, which indicates that CTI was fairly implemented according to the CTI fidelity scale manual (Conover, 2012; de Vet et al., 2017). Eight of the 12 items received a score of 3 or higher, which indicates that these components had been sufficiently implemented: in most cases, the intervention was time‐limited, with a follow‐up of 9 months (±2 weeks), and focused on a maximum of three intervention areas. Furthermore, most clients were engaged early by their CTI worker, who worked according to outreach principles, and were linked to community support resources during the first phase of the intervention. Additionally, the quality of the intake assessment and progress notes was sufficient in the majority of client charts. Four other components, however, appeared to be less adequately applied in practice. Generally, the three phases of the intervention did not last exactly 3 months, CTI workers would have contact with their clients during the last phase more often than their monitoring role prescribed (i.e., more than once every 3 weeks), and in the clients’ personal recovery plans, which contain information about phase planning, and their closing notes, prescribed elements were often omitted (de Vet et al., 2017). The fidelity assessment's findings will be taken into consideration in the discussion.
Care‐as‐Usual
Participants allocated to the control condition received care‐as‐usual from the same shelter organizations that provided CTI to participants in the experimental group. These shelter organizations generally provided services after discharge, although type, approach, intensity, and duration differed greatly depending on the organization, clients’ needs, and available funds. Clients with complex service needs would receive case management services after discharge from all except one organization. Most organizations employed a strength‐based approach. Case managers’ average caseloads ranged between 10 and 30 clients. Average intensity ranged from less than an hour to 3 hours weekly for an average duration of 12 weeks to about 2.5 years. Clients with less complex service needs were offered home visits or telephone calls with their shelter case manager, shelter walk‐in hours, or referral to other services.
As indicated by the CTI workers in a focus group (de Vet et al., 2017), the CTI model contrasts significantly from the usual case management services offered by the participating organizations at the time of the study in six ways. 1. CTI was designed to bridge the gap between services during critical times in the lives of vulnerable people. To ease the transition, CTI workers would engage clients early, by getting to know the client before discharge and meeting with the client and his or her shelter case manager to complete an Intake Form together. In usual services, case managers in shelters and community teams would rarely have contact during or after the discharge process. 2. At discharge, it was generally unclear how long usual services would be continued and, as a result, case managers were used to helping clients by taking over and completing tasks for them. The time‐limited nature of CTI, on the other hand, helped CTI workers to share the responsibility with their clients. Instead of taking over, they would assist their clients with enlisting help from key figures in their support networks to complete tasks and reach their goals. 3. Compared to usual services, the structure of CTI allowed CTI workers to spend more time with their clients immediately after the transition to housing, which is often a critical time when clients need the most support. 4. The decreasing intensity of CTI also meant that, up to 9 months, CTI workers would continue monitoring and kept making attempts to contact clients, while usual services would be terminated automatically in case of several “no shows.” 5. CTI workers would focus on up to three areas of intervention that were most important for the long‐term stability of their clients, while case managers were often encouraged to set goals with their clients in all life areas. And, 6. CTI workers would map out the social and professional support network of their clients with tools provided by the research team and organize a joint meeting with key figures from this network at the beginning and end of the intervention, which was rarely done in usual services.
These differences between services correspond to several of the 14 key components of CTI, which can be found in the CTI fidelity scale manual (Conover, 2012) and Appendix S2 (available online). To assess treatment differentiation (i.e., whether conditions differed in the intended manner), six of these key components of CTI were translated into process measures and administered at 3, 6, and 9 months (see Table 2).
Table 2.
Translation of key components of CTI into process measures
| Key component | Description | Process measure(s) |
|---|---|---|
| A time‐limited, 9‐month intervention | The CTI worker should still be in touch with the client and be providing intervention up to the time of the 9‐month postdischarge due date. | Did you receive support services from the shelter organization since the last interview? |
| Decreasing intensity of services | CTI involves intensive outreach during Phase 1, then gradually decreases in intensity until Phase 3 when CTI is about monitoring. | How often did you meet your CTI worker/case manager in the past 3 months? |
| How often did you talk to your CTI worker/case manager on the phone in the past 3 months? | ||
| In vivo (i.e., community‐based) needs assessment and provision of services | Preferably, the CTI worker should not provide shelter‐based standard case management in addition to CTI. | Is your CTI worker/case manager the same person who provided services to you in the shelter? Or is this someone else? (3‐month follow‐up only) |
| The CTI worker should visit the client where he/she is living or receiving community services. | Where did you usually meet your CTI worker/case manager? | |
| Early establishment of community linkages | The CTI worker should meet at least once a month with the client before discharge. | Did you already meet or talk to your CTI worker/case manager during shelter stay? (3‐month follow‐up only) |
| Strengthening of community linkages through negotiation and mediation | The CTI worker should encourage communication between the client and community linkages. | Do you receive help from other professionals or agencies to achieve your goals? |
| Maintaining contact with clients with histories of transience, in order to minimize drop‐outs | The CTI worker should have provided at least 7 months of active postdischarge intervention. | How often did you meet your CTI worker/case manager in the past 3 months? |
| How often did you talk to your CTI worker/case manager on the phone in the past 3 months? |
Descriptions of the key components were derived from the CTI fidelity scale (Conover & Herman, 2007).
To reduce the risk of contamination between conditions, participants in the control group would not receive any services from the CTI workers. Case managers from the participating organizations who would be providing care‐as‐usual to control participants were not informed about CTI's theoretical and procedural aspects and could not participate in any of the pretrial or follow‐up training sessions during which CTI workers acquired the skills essential for CTI practice. Furthermore, CTI cases were not discussed in general team meetings, but in separate supervision meetings between the CTI workers and their coach. Frequently (e.g., during the follow‐up training sessions), the research team urged CTI workers, coaches, and other staff members involved in the study to refrain from sharing any knowledge or tools specific to CTI with other colleagues during the data collection period.
Measurements
Participants were interviewed at baseline and 3, 6, and 9 months afterward. During the face‐to‐face baseline and 9‐month follow‐up interview, all measures were administered. The primary outcome was also assessed by telephone at 3 and 6 months. Participants’ sociodemographic characteristics were obtained at baseline. Research assistants administered the interviews. These data collectors received training from the research team and were selected using stringent criteria: they had to have relevant academic or vocational degrees and be able to create a positive rapport with participants. Preferably, they had experience working with vulnerable people. Several multilingual research assistants were recruited and, if necessary, the interviews were conducted with the aid of an interpreter. For completing the interviews, participants received a financial incentive, which increased over time from €15 at baseline to €30 at 9‐month follow‐up.
The primary outcome was number of days rehoused, defined as living in conventional independent housing (i.e., property or legal (sub)tenancy) or accommodation permanently provided by relatives, friends, or acquaintances. To assess participants’ residential histories, we used the Residential Follow‐Back Calendar (New Hampshire Dartmouth Psychiatric Research Center, 1995).
Intermediate outcomes, which are directly targeted by CTI, were family support, social support, and unmet care needs. Family and social support were measured using the average score on a 5‐point scale of five items from the RAND Course of Homelessness Study (Burnam & Koegel, 1989). These items inquired how often relatives or friends and acquaintances would be available to provide practical and emotional support. Scales demonstrated adequate reliability (Cronbach's α = .93–.94 across time points for family support and α = .90–.92 for social support). To assess whether participants had unmet care needs, we asked whether they wanted and/or received help in six life areas (i.e., housing and daily life, finances and daily activities, physical health, mental health, safety and protection against violence, and social relationships) using adapted items from the short‐form quality of life and care (Wennink & Van Wijngaarden, 2004). Participants who indicated they wanted but did not receive help in one or more areas were considered to have unmet care needs.
Secondary outcomes were quality of life, psychological distress, self‐esteem, excessive alcohol use, and cannabis use. Quality of life was assessed using a two‐item average score on a 7‐point scale, from Lehman's Brief Quality of Life Interview (Lehman, 1983): α = .67–.87. The Global Severity Index, an average score of the 53‐item Brief Symptom Inventory (Derogatis, 1975), was used to measure psychological distress: α = .96. Self‐esteem was evaluated using the sum score of the 10‐item Rosenberg Self‐Esteem Scale (Rosenberg, 1965): α = .85–.90. Whether participants had used alcohol excessively (i.e., five or more drinks a day) or cannabis in the past 30 days was assessed with the European Addiction Severity Index (McLellan et al., 1992). Details about these measures have been published in the protocol (Lako et al., 2013), which outlined another four outcomes that we decided to omit from this report before statistical analysis began (see Appendix S3, available online).
Statistical Analysis
Based on the first CTI trial in the United States (Susser et al., 1997), the target sample size was 109 participants per group to detect a difference of 15% in participants who became homeless, with 80% power, 5% two‐sided significance level, and intraclass correlation coefficient of .05. During data cleaning, it became apparent that none of the participants were homeless at the end of follow‐up. We chose to use the number of days rehoused instead as our primary outcome, because this continuous measure might have more power to detect between‐group differences in housing stability.
Statistical analyses were performed using IBM SPSS Statistics for Windows 20.0 (IBM Corp., 2011). The effect of CTI was assessed by intention‐to‐treat using three‐level mixed‐effects models, with observation points nested within participants and participants nested within service providers. Because case managers mostly provided services to only one client taking part in the study (see Appendix S4, available online), we adjusted for clustering within organizations instead of within CTI workers and case managers, as specified in the protocol (Lako et al., 2013).
As prespecified, sociodemographic characteristics and baseline measurements of other outcomes were considered potential covariates. We assessed relationship strength between these variables and follow‐up measurements of outcomes using Pearson's r, φ, or η (depending on type of variable). Excluding the baseline and follow‐up measurements of the same outcomes, none of the potential covariates correlated strongly (>.5). If variables correlated intermediately (.1 < x ≤ .5), we assessed covariate imbalance to identify covariates. Because intermediate outcomes could potentially mediate the relationship between condition and other outcomes, we also added interaction effects if family support, social support, or unmet care needs were identified as a covariate.
Results
Of 1,144 clients assessed, 513 (45%) people met the selection criteria (Fig. 1). Of those eligible, 183 (36%) were assigned to CTI or care‐as‐usual. Participants were significantly older than nonparticipants, mean difference = 5.34 years, p < .001, 95% CI [3.24, 7.44]. We found no significant differences regarding country of birth and gender. Four participants were not included in the primary outcome analysis, because three refused participation after randomization and one participant's residential history data were missing at every follow‐up. As dictated by the intention‐to‐treat principle, all other participants were included in the analysis and retained in the group to which they had been allocated, including the four individuals who were assigned to care‐as‐usual but received services from a CTI worker and the 12 participants who were allocated to CTI and deviated from the protocol.
Figure 1.
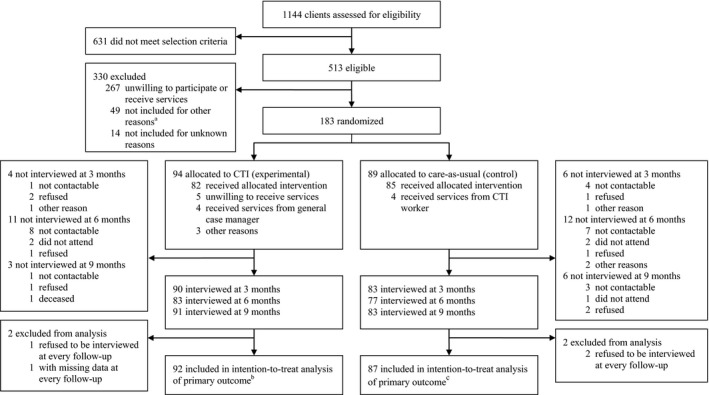
Participant flowchart following Journal Article Reporting Standards (JARS) guidelines. CTI, critical time intervention. aMostly because these clients could not be reached within the predetermined time frame of 2 weeks after discharge. bFor the experimental group, n ranges between 91 and 94 in the intention‐to‐treat analyses of intermediary and secondary outcomes. cFor the control group, n ranges between 88 and 89 in the intention‐to‐treat analyses of intermediary and secondary outcomes.
Table 3 shows participants’ baseline characteristics. The experimental group contained significantly more women and there was a trend toward participants in the CTI group being married or in a civil partnership more often compared to the control group; groups were balanced concerning other sociodemographic characteristics. Outcomes did not show any significant between‐group differences at baseline, although there was a trend toward control participants experiencing less social support than participants in the experimental group.
Table 3.
Baseline characteristics of participants in critical time intervention (CTI) and control (care‐as‐usual) group
| Characteristic | CTI (n = 94) | Control (n = 89) | Test statistica (p value) |
|---|---|---|---|
| Gender (female) | 51 (54%) | 34 (38%) | 4.74 (.03) |
| Age (years) | 41.42 (11.27) | 39.72 (11.87) | −0.99 (.32) |
| Migration background | |||
| Dutch native | 63 (67%) | 60 (67%) | 0.16 (.92) |
| First‐generation migrant | 21 (22%) | 21 (24%) | |
| Second‐generation migrant | 10 (11%) | 8 (9%) | |
| Married or in civil partnership | 16 (17%) | 7 (8%) | 3.49 (.06) |
| One or more children | 69 (73%) | 58 (65%) | 1.46 (.23) |
| One or more minor childrenb | 40 (45%) | 40 (49%) | 0.25 (.62) |
| One or more minor children staying with participantc | 26 (29%) | 15 (19%) | 2.52 (.11) |
| Education level | |||
| Low education level | 60 (64%) | 55 (62%) | 3.30 (.19) |
| Intermediate education level | 26 (28%) | 19 (21%) | |
| High education level | 8 (9%) | 15 (17%) | |
| History of literal homelessness | 62 (66%) | 52 (58%) | 1.10 (.29) |
| Family supportd | 2.94 (1.44) | 2.97 (1.32) | 0.14 (.89) |
| Social supporte | 3.41 (1.09) | 3.10 (1.12) | −1.86 (.06) |
| Unmet care needs in one or more life areasf | 64 (74%) | 62 (71%) | 0.21 (.65) |
| General quality of life | 4.75 (1.16) | 4.78 (1.35) | 0.14 (.89) |
| BSI global severity indexg | 0.59 (0.53) | 0.59 (0.55) | −0.02 (.98) |
| RSES scoreh | 31.51 (5.64) | 31.10 (5.57) | −0.49 (.63) |
| Excessive alcohol use in past 30 daysi | 18 (21%) | 17 (20%) | 0.04 (.85) |
| Cannabis use in past 30 daysj | 12 (14%) | 16 (20%) | 1.00 (.32) |
Data are n (%) or M (SD). BSI, Brief Symptom Inventory; RSES, Rosenberg Self‐Esteem Scale.
aStatistical differences in gender, migration background, marital and parental status, education level, homelessness history, unmet care needs, excessive alcohol use, and cannabis use were calculated using a chi‐square test; differences in age, family support, social support, quality of life, BSI index, and RSES score were calculated using an independent samples t test.
bMinors are children younger than 18 years old; n = 89 in CTI group and n = 82 in control group.
c n = 90 in CTI group and n = 81 in control group.
d n = 88 per group.
e n = 89 in CTI group and n = 88 in control group.
f n = 87 in CTI group and n = 88 in control group.
g n = 89 in CTI group and n = 87 in control group.
h n = 90 in CTI group and n = 89 in control group.
i n = 86 per group.
j n = 87 in CTI group and n = 82 in control group.
Process Measures
At the 3‐month follow‐up, nearly all participants indicated they received services from a shelter organization after discharge (Table 4). Consistent with the model, which prescribes that CTI workers remain in touch with clients until 9 months postdischarge, participants allocated to CTI continued to receive services throughout the follow‐up (92% at 6 months and 83% at 9 months), while the proportion of control participants receiving services dropped to 73% and 59%, respectively.
Table 4.
Process measure results at 3‐, 6‐, and 9‐month follow‐up
| Process measure | 3‐month follow‐up | 6‐month follow‐up | 9‐month follow‐up | |||
|---|---|---|---|---|---|---|
| CTI (n = 94) | Control (n = 89) | CTI (n = 94) | Control (n = 89) | CTI (n = 94) | Control (n = 89) | |
| All participants | ||||||
| Services from CTI worker/case manager | n = 90 | n = 79 | n = 83 | n = 77 | n = 90 | n = 81 |
| Participant received services since last interview | 86 (96%) | 71 (90%) | 76 (92%) | 56 (73%) | 75 (83%) | 48 (59%) |
| Frequency of face‐to‐face contacta | n = 88 | n = 78 | n = 82 | n = 77 | n = 83 | n = 80 |
| Not at all | 7 (8%) | 10 (13%) | 9 (11%) | 21 (27%) | 16 (19%) | 35 (44%) |
| Less than once a month | 6 (7%) | 5 (6%) | 2 (2%) | 4 (5%) | 7 (8%) | 2 (3%) |
| At least once a month | 21 (24%) | 14 (18%) | 38 (46%) | 24 (31%) | 36 (43%) | 22 (28%) |
| At least once a week | 54 (61%) | 49 (63%) | 33 (40%) | 28 (36%) | 24 (29%) | 21 (26%) |
| Frequency of telephone contacta | n = 88 | n = 78 | n = 82 | n = 77 | n = 83 | n = 80 |
| Not at all | 20 (23%) | 18 (23%) | 16 (20%) | 30 (39%) | 24 (29%) | 45 (56%) |
| Less than once a month | 22 (25%) | 14 (18%) | 18 (22%) | 11 (14%) | 18 (22%) | 9 (11%) |
| At least once a month | 28 (32%) | 31 (40%) | 30 (37%) | 26 (34%) | 29 (35%) | 17 (21%) |
| At least once a week | 18 (20%) | 15 (19%) | 18 (22%) | 10 (13%) | 12 (14%) | 9 (11%) |
| Participants who received services only | ||||||
| Most frequent location of face‐to‐face contact | n = 81 | n = 68 | n = 73 | n = 56 | n = 67 | n = 45 |
| Participant's house | 78 (96%) | 56 (82%) | 67 (92%) | 45 (80%) | 60 (90%) | 39 (87%) |
| CTI worker's/case manager's office | 1 (1%) | 6 (9%) | 3 (4%) | 8 (14%) | 7 (10%) | 2 (4%) |
| House of someone from social network | 0 (0%) | 0 (0%) | 2 (3%) | 0 (0%) | 0 (0%) | 0 (0%) |
| Another professional's office or agency | 1 (1%) | 0 (0%) | 0 (0%) | 1 (2%) | 0 (0%) | 2 (4%) |
| Shelter | 1 (1%) | 6 (9%) | 1 (1%) | 2 (4%) | 0 (0%) | 2 (4%) |
| Help from other professionals and service agencies | n = 83 | n = 70 | n = 74 | n = 56 | n = 65 | n = 47 |
| Never | 21 (25%) | 21 (30%) | 12 (16%) | 7 (13%) | 6 (9%) | 13 (28%) |
| Sometimes | 13 (16%) | 17 (24%) | 16 (22%) | 18 (32%) | 13 (20%) | 13 (28%) |
| Often | 22 (27%) | 16 (23%) | 28 (38%) | 19 (34%) | 28 (43%) | 7 (15%) |
| Always | 27 (33%) | 16 (23%) | 18 (24%) | 12 (21%) | 18 (28%) | 14 (30%) |
CTI, critical time intervention.
aContact between participant and CTI worker/case manager in past 3 months.
Because CTI involves intensive outreach in phase 1, we expected participants to mostly meet their CTI worker on a weekly basis during the first 3 months, which the majority did (61%). For some of them, CTI workers were successful in gradually decreasing the intervention's intensity until phase 3, when CTI is about monitoring: half of CTI participants reported meeting their CTI worker at least, or less than, once a month at 6 and 9 months (48% and 51%), compared to a third of control participants (36% and 31%). But, contrary to our expectations, a substantial minority (29%) in the experimental group still reported weekly meetings at the end of follow‐up. A similar proportion of control participants also received services that frequently (26%).
Critical time intervention should be delivered where clients live or receive community services. Most participants indicated that face‐to‐face contacts generally took place at their residence, although CTI workers visited clients at home more often than case managers at 3 months (96% compared to 82%) and 6 months (92% compared to 80%). Also, a larger proportion of CTI participants received help from other professionals often or always, especially at 9 months (71% compared to 45% of controls), indicating that CTI workers successfully involved other agencies as intended by protocol.
Outcomes Measures
Groups did not significantly differ regarding the number of days rehoused at any follow‐up (Table 5). Concerning intermediate outcomes, participants allocated to CTI reported increased family support during follow‐up compared to controls, adjusted mean difference = .36, p = .037, 95% CI [0.02, 0.71], but no additional social support. The proportion of participants with unmet care needs decreased at a similar rate in both groups. For the secondary outcomes, differences were small and nonsignificant, although there was a trend for psychological distress toward participants allocated to CTI experiencing less distress than controls, adjusted mean difference = −.14, p = .065, 95% CI [−0.29, 0.01].
Table 5.
Estimated impact of critical time intervention (CTI) on primary outcome at 3‐, 6‐, and 9‐month follow‐up and intermediate and secondary outcomes at 9‐month follow‐up
| CTI (n = 94) | Control (n = 89) | Adjusted mean difference or OR [95% CI]a | |||
|---|---|---|---|---|---|
| n | M (SD) or n (%) | n | M (SD) or n (%) | ||
| Primary outcome at 3‐, 6‐, and 9‐month follow‐up | |||||
| Days rehoused | |||||
| 3‐month follow‐upb | 89 | 78.21 (35.98) | 80 | 82.95 (32.21) | |
| 6‐month follow‐up | 82 | 84.33 (33.03) | 75 | 82.23 (34.81) | 7.48 [−3.69, 18.64] |
| 9‐month follow‐up | 80 | 87.16 (40.19) | 82 | 95.45 (53.27) | 0.16 [−10.91, 11.23] |
| Intermediate outcomes at 9‐month follow‐up | |||||
| Family support | 84 | 3.41 (1.27) | 79 | 3.00 (1.37) | 0.36 [0.02, 0.71]* |
| Social support | 87 | 3.39 (1.15) | 77 | 3.33 (1.03) | −0.27 [−0.62, 0.08] |
| Unmet care needs | 86 | 47 (55%) | 77 | 43 (56%) | 0.82 [0.33, 2.05] |
| Secondary outcomes at 9‐month follow‐up | |||||
| General quality of life | 90 | 5.26 (1.27) | 83 | 5.08 (1.32) | 0.21 [−0.19, 0.60] |
| BSI global severity index | 85 | 0.44 (0.44) | 77 | 0.57 (0.62) | −0.14 [−0.29, 0.01]c , † |
| RSES score | 87 | 32.11 (4.72) | 80 | 31.23 (4.87) | 0.71 [−0.73, 2.14] |
| Excessive alcohol use | 87 | 19 (22%) | 80 | 21 (26%) | 0.71 [0.24, 2.09] |
| Cannabis use | 87 | 13 (15%) | 80 | 18 (23%) | 0.89 [0.26, 3.05] |
OR, odds ratio; CI, confidence interval; BSI, Brief Symptom Inventory; RSES, Rosenberg Self‐Esteem Scale.
aIntention‐to‐treat analysis for primary outcome adjusted for days between follow‐up assessments and organization. Intention‐to‐treat analyses for intermediary and secondary outcomes adjusted for baseline scores/proportions and organization.
bThe 3‐month follow‐up measurement of this outcome was used as a reference category.
cWhen social support was added to the model as a covariate, the interaction between time, condition, and social support was statistically significant, estimated difference in intervention effect = .19, p = .013, 95% CI [0.04, 0.34].
† p < .10; *p < .05
Variables identified as covariates were gender for excessive alcohol use and cannabis use and social support for psychological distress and unmet care needs. Adjustment for covariates had no discernible effect, except for psychological distress. CTI had an added differential effect on psychological distress for participants experiencing less social support, estimated difference in intervention effect = .19, p = .013, 95% CI [0.04, 0.34].
Discussion
For people moving from homeless shelters to community living, CTI had a significant effect on family support and, for people with less social support, on psychological distress, but was not more effective than care‐as‐usual regarding the primary outcome, number of days rehoused. The finding that CTI improved family support is important in the light of recent changes in European social policies, which nowadays tend to promote reliance on informal support resources instead of public services (Grootegoed & van Dijk, 2012). Although costs associated with CTI and usual services were not assessed in the present study, it could be fruitful to conduct such an assessment in the future and investigate whether CTI is a cost‐effective alternative to care‐as‐usual. Although more participants allocated to CTI were still receiving services at 9 months, service frequency was relatively lower among them compared to those receiving services in the control group. Moreover, CTI ends after 9 months while care‐as‐usual could continue up to 2.5 years. A cost‐effectiveness evaluation with a follow‐up that extends beyond CTI's service delivery period of 9 months should be conducted to test this hypothesis.
Similar to the findings concerning psychological distress in this study, other trials have found positive effects of CTI on different measures of symptom severity. This strengthens the evidence that CTI is beneficial to vulnerable people's mental health (Herman et al., 2000; Kasprow & Rosenheck, 2007; Shinn, Samuels, Fischer, Thompkins & Fowler, 2015). The finding that CTI had an effect specifically for those with less social support raises questions about the intervention's effective elements. One explanation is that clients experiencing less social support benefit more from improved family support regarding their mental health. Future research into which CTI components facilitate favorable outcomes for certain subpopulations should be able to demonstrate this.
The lack of effect on number of days rehoused can be explained by the fact that recurrent homelessness was rare in both conditions, which could be explained by a number of factors. One pertains to differences between the United States and the Netherlands in health care systems and social context. The intensity of care‐as‐usual in the Netherlands was quite high during the study period, with about a quarter of participants continuing to receive services frequently throughout follow‐up, whereas in the United States such follow‐up services were not typically available (Herman et al., 2007). Beside high‐intensity service provision, the Netherlands has an extensive social housing system, with one in three households residing in social housing. The process from rent arrear to eviction can take longer than 6 months (Stenberg, van Doorn & Gerull, 2011) and, even after the court has issued an eviction order, social housing associations manage to prevent evictions in 7 of 10 cases (Boerebach, 2013), making the short‐term risk of recurrent homelessness negligible.
Another explanation could be that the between‐group difference in the primary outcome would have been more pronounced if CTI had been delivered with higher model fidelity. A fidelity assessment showed that, with an overall fidelity score of 3 of 5, CTI was fairly implemented in a representative subsample of 35 participants and research has shown that more faithfully implemented evidence‐based practices produce better outcomes (Cuddeback et al., 2013; Fukui et al., 2012). However, this explanation is unlikely given there was little room left for improvement on this outcome in both conditions. During the 9‐month follow‐up, the risk for loss of housing was so small in our sample that improving fidelity of the experimental intervention to the CTI model, which could theoretically lead to an improvement of the intervention's effectiveness, would not have produced better results for CTI compared to care‐as‐usual on the primary outcome. However, if CTI had been delivered with higher fidelity to the model, more effects of CTI may have been obtained with regard to the intermediary and secondary outcomes, because those outcomes could be improved.
A final consideration relates to the target population. Half of the clients assessed did not meet our criteria, mostly because they were not moving to community living. This might indicate that participating organizations employed a “staircase” approach, which requires individuals to prove housing readiness while transferring through shelters and transitional housing before they become eligible for housing (Pleace, 2012). The threshold for acquiring housing could be too high and, given the costs associated with this approach (Gulcur, Stefancic, Shinn, Tsemberis & Fischer, 2003), earlier discharge might be considered. If a “housing‐led” approach—providing access to permanent housing as the initial response to homelessness with flexible support services (Pleace, 2012)—would become the norm in Dutch shelter services, CTI could be effective in preventing recurrent homelessness for those excluded from the present study. In the United States, combining CTI with a housing‐led approach has been successful in helping people with complex needs and chronic homelessness to move to stable housing (Clark, Guenther & Mitchell, 2016).
Strengths and Limitations
The present study is the first randomized controlled trial to test an intervention for homeless people in Dutch shelter services (Rensen, van Arum & Engbersen, 2008), which is generally rare outside the United States (De Vet et al., 2013). Because participants with unstable residential histories are known to be difficult to follow‐up (Coen, Patrick & Shern, 1996), measures to minimize attrition were taken and, consequently, loss to follow‐up was limited to only 5%.
A limitation of the present study is the relatively short follow‐up, which does not allow drawing conclusions about CTI's long‐term effects. The rationale of CTI is that supports put in place during the intervention will have a long‐term positive impact that extends beyond service delivery. A trial of CTI provided after hospital discharge showed that it took over 12 months for risk of homelessness to differ in favor of the experimental group (Herman et al., 2011). More research is needed to establish whether CTI has long‐term effects on housing and other outcomes for people leaving shelters in the Netherlands.
Another limitation is that some of the data collectors had occasionally become aware of condition assignment. Although data collectors had been trained to ignore this knowledge in conducting their tracking and interviews, it could have affected data collected for these specific participants. However, the use of standardized instruments should limit this bias to a minimum.
Implications
Given recent emphasis on informal support in public services and significant effects on family support and, for those with less social support, on psychological distress in this trial, we conclude that CTI is a fitting intervention for Dutch shelter organizations. Although the differences in outcomes between the groups are limited, there are other advantages to using the CTI model in the Dutch context. CTI workers indicated they could enable a more smooth transition from shelter to housing by meeting with clients and their shelter case managers before discharge and help alleviate stress by spending more time with their clients immediately after the transition to housing. Because of the CTI model, they helped clients make better use of their social support network and felt they were more focused and structured in providing and coordinating support and could share responsibility for success with their clients (de Vet et al., 2017).
Very few participants in both groups were homeless at 9 months and, consequently, CTI did not have a short‐term effect on number of days rehoused. More research is needed to establish whether, given a longer follow‐up, CTI can prevent recurrent homelessness and is cost‐effective compared to care‐as‐usual in the Netherlands. If housing for this population in the Netherlands is relatively stable once it is obtained, then CTI, when implemented in this different underlying housing context, could be directed toward other life areas that are important for social inclusion and participation. As a result, different community sources for support, to which CTI workers can link their clients, will come into play and other linkages, such as with the social housing association from which clients are renting their living accommodations, may need less attention.
Supporting information
Acknowledgments
This study was funded by the Netherlands Organization for Health Research and Development (ZonMw) (101200002) and the Academic Collaborative Center for Shelter and Recovery. The study sponsor had no role in the study design, the collection, analysis, and interpretation of data, the writing of the report, or the decision to submit for publication. The corresponding author had full access to all study data and final responsibility for the decision to submit for publication. The authors declare that they have no potential conflicts of interest. We thank all practitioners and participants involved in this trial and Reinier Akkermans for his input on the data analysis.
References
- Boerebach, N. (2013, December 10). Prevention of evictions by social housing organisations in the Netherlands. Homeless in Europe, 12–13. Available from: http://www.feantsa.org/download/homeless_in_europe_winter20138095145355003545457.pdf [last accessed July 18 2017].
- Bond, G.R. , Evans, L. , Salyers, M.P. , Williams, J. , & Kim, H.W. (2000). Measurement of fidelity in psychiatric rehabilitation. Mental Health Services Research, 2, 75–87. [DOI] [PubMed] [Google Scholar]
- Burnam, M. , & Koegel, P. (1989). The course of homelessness among the seriously mentally ill. An NIMH‐funded proposal. Unpublished manuscript.
- Caton, C.L.M. , Dominguez, B. , Schanzer, B. , Hasin, D.S. , Shrout, P.E. , Felix, A. , & Hsu, E. (2005). Risk factors for long‐term homelessness: Findings from a longitudinal study of first‐time homeless single adults. American Journal of Public Health, 95, 1753–1759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark, C. , Guenther, C.C. , & Mitchell, J.N. (2016). Case management models in permanent supported housing programs for people with complex behavioral issues who are homeless. Journal of Dual Diagnosis, 12, 185–192. [DOI] [PubMed] [Google Scholar]
- Coen, A.S. , Patrick, D.C. , & Shern, D.L. (1996). Minimizing attrition in longitudinal studies of special populations: An integrated management approach. Evaluation and Program Planning, 19, 309–319. [Google Scholar]
- Conover, S. (2012). CTI fidelity scale manual. Unpublished manuscript, Department of Psychiatry, Columbia University, New York.
- Conover, S. , & Herman, D.B. (2007). CTI fidelity scale. Unpublished manuscript, Department of Epidemiology and the Center for Homelessness Prevention Studies, Columbia University Mailman School of Public Health, New York.
- Cuddeback, G.S. , Morrissey, J.P. , Domino, M.E. , Monroe‐DeVita, M. , Teague, G.B. , & Moser, L.L. (2013). Fidelity to recovery‐oriented ACT practices and consumer outcomes. Psychiatric Services, 64, 318–323. [DOI] [PubMed] [Google Scholar]
- de Vet, R. , Lako, D.A.M. , Beijersbergen, M.D. , van den Dries, L. , Conover, S. , van Hemert, A.M. , … & Wolf, J.R.L.M. (2017). Critical time intervention for people leaving shelters in the Netherlands: Assessing fidelity and exploring facilitators and barriers. Administration and Policy in Mental Health and Mental Health Services Research, 44, 67–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Vet, R. , van Luijtelaar, M.J.A. , Brilleslijper‐Kater, S.N. , Vanderplasschen, W. , Beijersbergen, M.D. , & Wolf, J.R.L.M. (2013). Effectiveness of case management for homeless persons: A systematic review. American Journal of Public Health, 103, e13–e26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derogatis, L. (1975). The Brief Symptom Inventory. Baltimore: Clinical Psychometric Research. [Google Scholar]
- Fazel, S. , Geddes, J.R. , & Kushel, M. (2014). The health of homeless people in high‐income countries: Descriptive epidemiology, health consequences, and clinical and policy recommendations. The Lancet, 384, 1529–1540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fukui, S. , Goscha, R. , Rapp, C.A. , Mabry, A. , Liddy, P. , & Marty, D. (2012). Strengths model case management fidelity scores and client outcomes. Psychiatric Services, 63, 708–710. [DOI] [PubMed] [Google Scholar]
- Grootegoed, E. , & van Dijk, D. (2012). The return of the family? Welfare state retrenchment and client autonomy in long‐term care. Journal of Social Policy, 41, 677–694. [Google Scholar]
- Gulcur, L. , Stefancic, A. , Shinn, M. , Tsemberis, S. , & Fischer, S.N. (2003). Housing, hospitalization, and cost outcomes for homeless individuals with psychiatric disabilities participating in continuum of care and housing first programmes. Journal of Community and Applied Social Psychology, 13, 171–186. [Google Scholar]
- Herman, D. , Conover, S. , Felix, A. , Nakagawa, A. , & Mills, D. (2007). Critical time intervention: An empirically supported model for preventing homelessness in high risk groups. The Journal of Primary Prevention, 28, 295–312. [DOI] [PubMed] [Google Scholar]
- Herman, D.B. , Conover, S. , Gorroochurn, P. , Hinterland, K. , Hoepner, L. , & Susser, E.S. (2011). Randomized trial of critical time intervention to prevent homelessness after hospital discharge. Psychiatric Services, 62, 713–719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herman, D. , Opler, L. , Felix, A. , Valencia, E. , Wyatt, R.J. , & Susser, E. (2000). A critical time intervention with mentally ill homeless men: Impact on psychiatric symptoms. The Journal of Nervous and Mental Disease, 188, 135–140. [DOI] [PubMed] [Google Scholar]
- IBM Corp . (2011). IBM SPSS statistics for windows, version 20.0. Armonk, NY: IBM Corp. [Google Scholar]
- Kasprow, W.J. , & Rosenheck, R.A. (2007). Outcomes of critical time intervention case management of homeless veterans after psychiatric hospitalization. Psychiatric Services, 58, 929–935. [DOI] [PubMed] [Google Scholar]
- Kingree, J.B. , Stephens, T. , Braithwaite, R. , & Griffin, J. (1999). Predictors of homelessness among participants in a substance abuse treatment program. American Journal of Orthopsychiatry, 69, 261–266. [DOI] [PubMed] [Google Scholar]
- Lako, D.A.M. , Beijersbergen, M.D. , Jonker, I.E. , de Vet, R. , Herman, D.B. , van Hemert, A.M. , & Wolf, J.R.L.M. (2017). The effectiveness of critical time intervention for abused women leaving women's shelters: A randomized controlled trial. Manuscript submitted for publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lako, D.A.M. , de Vet, R. , Beijersbergen, M.D. , Herman, D.B. , van Hemert, A.M. , & Wolf, J.R.L.M. (2013). The effectiveness of critical time intervention for abused women and homeless people leaving Dutch shelters: Study protocol of two randomised controlled trials. BMC Public Health, 13, 555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lehman, A.F. (1983). The well‐being of chronic mental patients. Archives of General Psychiatry, 40, 369–373. [DOI] [PubMed] [Google Scholar]
- McLellan, A.T. , Kushner, H. , Metzger, D. , Peters, R. , Smith, I. , Grissom, G. , … & Argeriou, M. (1992). The fifth edition of the addiction severity index. Journal of Substance Abuse Treatment, 9, 199–213. [DOI] [PubMed] [Google Scholar]
- McQuistion, H. , Gorroochurn, P. , Hsu, E. , & Caton, C.M. (2014). Risk factors associated with recurrent homelessness after a first homeless episode. Community Mental Health Journal, 50, 505–513. [DOI] [PubMed] [Google Scholar]
- New Hampshire Dartmouth Psychiatric Research Center (1995). Residential follow‐back calendar. Lebanon, NH: Dartmouth Medical School. [Google Scholar]
- Pleace, N. (2012). Housing first. European Observatory on Homelessness FEANTSA. Available from: http://www.feantsaresearch.org/download/housing_first_pleace3790695452176551843.pdf [last accessed July 18 2017].
- Rensen, P. , van Arum, S. , & Engbersen, R. (2008). Wat werkt? Een onderzoek naar de effectiviteit en de praktische bruikbaarheid van methoden in de vrouwenopvang, maatschappelijke opvang en opvang voor zwerfjongeren [What works? A study into the effectiveness and the practical usability of methods in women's shelters and shelters for homeless adults and youths]. Utrecht, Netherlands: Movisie.
- Rosenberg, M. (1965). Society and the adolescent self‐image. Princeton, NJ: Princeton University Press. [Google Scholar]
- Shinn, M. , Samuels, J. , Fischer, S.N. , Thompkins, A. , & Fowler, P.J. (2015). Longitudinal impact of a family critical time intervention on children in high‐risk families experiencing homelessness: A randomized trial. American Journal of Community Psychology, 56, 205–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stenberg, S.‐Å. , van Doorn, L. , & Gerull, S. (2011). Locked out in Europe: A comparative analysis of evictions due to rent arrears in Germany, the Netherlands and Sweden. European Journal of Homelessness, 5, 39–61. [Google Scholar]
- Susser, E. , Valencia, E. , Conover, S. , Felix, A. , Tsai, W.Y. , & Wyatt, R.J. (1997). Preventing recurrent homelessness among mentally ill men: A “critical time” intervention after discharge from a shelter. American Journal of Public Health, 87, 256–262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wennink, J. , & Van Wijngaarden, B. (2004). Quality of life and care (QoLC): Kwaliteit van leven en vervulling van zorgwensen [Quality of life and care (QoLC): Quality of life and fulfilment of care needs]. Utrecht, Netherlands: Trimbos‐Instituut. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials


